Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 11
Underweight and Its Associated Factors Among Children 6–59 Months of Age in Debre Tabor Town, Amhara Region of Ethiopia, 2019: A Community-Based Cross-Sectional Study
Authors Tibebu NS , Emiru TD , Tiruneh CM , Getu BD, Azanaw KA
Received 22 October 2020
Accepted for publication 24 November 2020
Published 27 November 2020 Volume 2020:11 Pages 469—476
DOI https://doi.org/10.2147/PHMT.S288071
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Nigusie Selomon Tibebu,1 Tigabu Dessie Emiru,1 Chalie Marew Tiruneh,1 Bisrat Dessie Getu,2 Kefyalew Amogne Azanaw2
1Department of Pediatrics and Child Health Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 2Department of Nursing, Debre Tabor Health Sciences College, Debre Tabor, Ethiopia
Correspondence: Nigusie Selomon Tibebu
Department of Pediatrics and Child Health Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
Email [email protected]
Introduction: Even-thought malnutrition is a double burden now time being; under-nutrition among under-five year’s children is a common public health problem, and it is one of the main reasons for the death of children in developing countries. Therefore, this study aimed to assess the prevalence and associated factors of underweight among children age 6– 59 months at Debre Tabor town Ethiopia, 2019.
Methods: A community-based cross-sectional study was conducted on an underweight using cluster and systematic random sampling. A sample of 608 participants completed a questionnaire designed for the study. The questionnaire was coded and entered into Epi info version 7.2.0.1 and exported to SPSS 20.0 for data analysis. Principal component analysis (PCA) was used to compute family wealth status. Bivariable and multivariable logistic regression analyses were done to see which independent variables have an association with the dependent variable, and a P value of less than 0.05 was considered as significant at 95% CI.
Results: The result revealed that underweight for children age 6– 59 months was 17.4% (95% CI: 14.5– 20.6%). Fathers who have primary education levels were 2.13 times more likely to have under-weighted children than those who have secondary and above education levels [adjusted odds ratio (AOR): 2.13; 95% CI: 1.19– 3.80]. Similarly, parents who have poor wealth status in their family 2.2 times more likely to have underweight children than those who have rich wealth status in their family [AOR: 2.2 (1.21– 4.09)]. However, on the sex of children being males were 1.8 times more likely to become underweight than females [AOR: 1.8 (1.14– 2.85)].
Conclusion: Among under-nutrition problems of children age 6– 59 months, underweight is still an important public health problem. Therefore, family education and family wealth status should be modified, and responsible bodies design further nutritional intervention programs.
Keywords: under-weight, children, Debre Tabor, Ethiopia
Introduction
Even-thought malnutrition is a double burden now time being, under-nutrition among under-5 year children is a common public health problem and it is one of the main reasons for the death of children in developing countries.1–3 Globally, there are 165 million stunted, 99 million underweighted, and 51 million wasted children.2–5
Demographic health survey of Pakistan (2012–2013) report confirmed that 29.4% of under-five children were underweight, on the other hand, mothers’ educational level, and child-size at birth were found the significant factors for being underweight.6
As a systematic review done in Sub-Saharan Africa (SSA) the overall (pooled) prevalence of underweight was not reported. However, low mother’s education, increasing child’s age, sex of child (male), wealth index (poor household), mother’s age (<20 years), source of drinking water, birth size (small), diarrheal morbidity, and low father’s education were the most significant factors for the occurrence of under-nutrition in the stated area.7
Weight-for-age is an overall indicator of a population’s nutritional health because children can be underweight for their age when they are stunted, wasted, or both. Therefore, weight-for-age is a composite index of weight-for-height and height-for-age and thus does not differentiate between acute malnutrition and chronic malnutrition.8
A community-based cross-sectional study was conducted in Ethiopia among children age 6–59 months and the result revealed that 15.8% of the child were underweight, adjacent to this maternal Education, family size, and diarrheal morbidity were the leading factors of children for the existence of under-weight.9
National demographic health survey of Ethiopia (EDHS 2016) report showed that 24% of all children were underweight, but good education level and household wealth can reduce the percentage of underweight of children in their life extent.8
As a study conducted in Gida Ayana and Aris Oromia, Ethiopia, the overall prevalence of underweight among children age 6–59 months was 19.2% and 49.2%, respectively. Besides, sex of child (male), numbers of children in the family (>one), breastfeeding, and diarrhea were showed a significant association for the direction of the survival of the problem.10,11
As the study allowed in an-other area of Oromia at Bishoftu town, the study revealed that 22.6% of children were underweight. However, the age of the child and numbers of the visit by health extension visits were determinant factors since, as the age of a child increases the risk of being underweight to be not increased.12
Materials and Methods
Study Area and Setting
This study was conducted at Debre Tabor town, Amhara regional state of Ethiopia. Debre Tabor town is the capital city of the South Gondar zone and has 6 kebeles with 36,285 households. The town had 84,382 general population, of them 19,898 was in a reproductive age (15–49) group, and from the total population 10,868 were children from age 6–59 months.
Study Design and Data Source
A community-based cross-sectional study was conducted among children age 6–59 months in randomly selected kebeles at Debre Tabor town and available during the data collection period were the study population.
Sample Size Determination and Sample Size Calculation
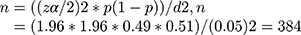
The sample size for this study was calculated using single population proportion formula considering the following assumption: according to a study done in Aris, Oromiya Ethiopia the prevalence of underweight among children age from 6 to 59 months was 49%. Based on this assumption the sample size was calculated as follow:
Where: n= the required sample size, z= standard score corresponding to 95% CI, p= prevalence of parental traditional medicine use for children, q= 1-p and d= the margin of error 5%. Therefore, 384*1.5=576 and 10% of none response rate 58 and total sample size are 634.
Sampling Procedure and Technique
Six kebeles were considered as a cluster and 50% of the clusters (three clusters) were selected randomly. To gate study participants for data collection, systematic random sampling technique was used. For households that had more than one eligible child, a lottery method was considered to select one child for the study.
Dependent Variable
- Underweight (below −2 SD) children age from 6 to 59 months
Independent Variables
- Socio-economic and Demographic variables (age, educational level, marital status, family wealth, and family size)
- Maternal Characteristics (ANC visits, family planning use, age at first birth, place of delivery)
- Childs’ Characteristics (sex of the child, birth order)
Operational Definition
Underweight
A child is defined as underweight if the weight-for-age Z-score is found to be below −2 SD of the median of the WHO standard curve.
Data Collection Tools and Procedures
Measurements
Anthropometric measurement was done. Child weight was measured by an electronic digital weight scale for children who were comfortable to be measured alone, but children who were unable to be measured alone; we were used mother-child weight combined measurement, and then the mother’s weight was measured to calculate the child’s weight through subtraction.
The weight measurement was recorded to the nearest 0.1 kg. The data were collected using a semi-structured interviewer-administered questionnaire. Either fathers or mothers of the children were interviewed but the priority was given to mothers because mothers are believed to be closer to their children than fathers.
When the mother would not available the father was interviewed and if not the guardian was interviewed. Semi-structured interviewer-administered questionnaires were adapted from previous researches done on similar topics and WHO stepwise surveillance (WHO STEPS) for child malnutrition. However, wealth status related questionnaire was adopted from EDHS (Ethiopian Demographic Health Survey, 2016). Pre-test (5% of the sample size) was done in non-selected clusters. The questionnaire was translated into Amharic, the national language of Ethiopia, and back-translated to English for its consistency.
The questionnaire had consisted of four parts (socio-demographic, maternal, child health-related characteristics), and wealth status of the family. The data was collected by three Diploma Nurses. The supervision was made by three master holder nurses. Before the data collection, one-day training was given to data collectors and supervisors.
Data Processing and Analysis
World Health Organization (WHO) Antro-version 3.2.2 software was used to generate the Z-score value of weight-for-age (WAZ) to compute underweight or to assess the nutritional status of the children by using the age of the child, sex of the child, the weight of the child and ID of the child. Principal component analysis (PCA) was used to compute family wealth status by fulfilling the assumptions of factor analysis, KMO value, and communality.
The data were cleaned, coded, and, entered into Epi info version 7.2.0.1 and transferred to SPSS version 20.0 for analysis. Descriptive and inferential statistics were used for presenting and analyzing the data, respectively. Descriptive statistics like frequency and percentage were done to summarize the data. And inferential statistics like odds ratio, binary logistic regression, and multiple logistic regression were used to determine the association between the dependent variable and different independent factors. Statistical significant variables (p <0.2) in the binary logistic regression analysis were entered for multivariable analysis and P-value less than 0.05 was considered as significant at 95% CI. Hosmer and Lemeshow goodness of fit test was checked.
Ethical Consideration
Ethical clearance was obtained from the school of the nursing ethical review committee on behalf of the University of Gondar review board. The verbal informed consent was acceptable and approved by Ethical review board on the behalf of the University of Gondar, and that this study was conducted under the declaration of Helsinki. A permission letter was obtained from the Debre Tabor town department of health. Participants were informed about voluntarism and that they can withdraw at any time of the study if they want not to respond. For those who were a volunteer to participate, verbal consents were obtained from the parent/legal guardian/for the children involved before the study begin. At the end of the interview, participants were informed about underweight and associated potential effects.
Results
Socio-Demographic Factors of the Study Participants
From a total of 634 proposed participants, 608 participants with a 95.9% response rate were included in the analysis. Among the total participants, 554 (91.1%) were married in their marital status and a half and above 55.9% were mothers have no formal education level.
Of the total participants of mothers, near to half, 54.4% had less than four antenatal care visits, and most of the mothers (97.2%) were gave birth in the health institutions. Almost half and above sex of the child were male (52.2%), and most of (93.4%) the participants were had less than or equal to four birth order in their family health-care status (Table 1)
 |
Table 1 Characteristics of Participants for Underweight Among Children Age from 6 to 59 Months in Debre Tabor Town Amhara Region of Ethiopia, 2019 |
Underweight Among Children Age from 6 to 59 Months in Debre Tabor Town Amhara Region of Ethiopia
From the total participants of the survey age from 6 to 59 months of children, 17.4% (95% CI 14.5%-20.6%) were found underweight (Figure 1)
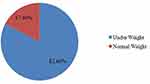 |
Figure 1 Prevalence of underweight among children age from 6–59 months in Debre Tabor town Amhara Region of Ethiopia, 2019. |
Factors Associated with Underweight Among Children Age from 6 to 59 Months in Debre Tabor Town Amhara Region of Ethiopia
Bivariable and multivariable logistic regression analysis were used to determine factors affecting the weight of children age from 6 to 59 months. The bivariable analysis showed that birth order, sex of the child, age of the mother at first birth, marital status of the participant, mothers’ educational level, fathers’ educational level, place of delivery, family planning use, and wealth of the family were associated with parental traditional medicine use for children considering p-value≤0.2. For adjusting potential confounders those variables which were significant at bivariable analysis were entered into multivariable logistic regression. The result revealed that the sex of the child, fathers’ educational level, and wealth status of the family were significantly associated with underweight for children age 6–59 months. However, the remaining listed above variables were not significant at p-value≤0.05 (Table 2).
 |
Table 2 Bivariate and Multivariable Logistic Regression Analyses for Underweight Among Children Age from 6 to 59 Months in Debre Tabor Town Amhara Region of Ethiopia, 2019 |
Fathers who have primary education levels were 2.13 times more likely to have underweight children than those who have secondary and above education levels [AOR: 2.13; 95% CI: 1.19–3.80]. Similarly, parents who have poor wealth status in their family 2.2 times more likely to have underweight child than those who have rich wealth status in their family [AOR: 2.2 (1.21–4.09)]. However, on the sex of child being male were 1.8 times more likely to become underweight than female [AOR: 1.8 (1.14–2.85)].
Discussion
Under-nutrition is a lack of proper nutrition, caused by not having enough food in the body, and expressed by non-specific nutritional problems like underweight.1
In this cross-sectional study, the prevalence of underweight among children age from 6 to 59 months was 17.4% (95% CI: 14.5–20.6%). It was higher when compares to a study done at Sodo, Ethiopia 14%,13 East Gojjam, Ethiopia from model house-holds 10%,14 and at Khyber Paktunkuwa 11.4%,15 Vietnam 8.4%.16 The possible reasons might be the number of mother to child for the participation in the study, and the period of the study.
On the other hand, this study was in line with the study done at Wonsho, Ethiopia 20.5%,17 Takusa Ethiopia 19.5%,18 Gidayana Ethiopia 19.2%,10 Howassa town Ethiopia 15.8%,9 and at the pooled prevalence of Sub-Saharan Africa 16.3%.19 However, this study was lower as evaluated to the study done at Bula-Hora, Ethiopia 29.2%,20 Dollo-Ado Somalia Ethiopia 47.7%,21 Afar Ethiopia 33.7%,22 a previous study of Ethiopia 25%,23 Lalibela Ethiopia 25.6%,24 Ethiopia (EDHS 2016) 24%,25 Bishofitu Ethiopia 22.6%,12 Tahtay Tigray Ethiopia 37.4%,26 EDHS-Tigray 23.9%,27 Shashemena Ethiopia 49.2%,11 Mai-Aini Eritrean refugee camp 33.4%,28 Khartoum Sudan 35%,29 Tigray region 33%,30 East Gojjam Ethiopia from non-model house-holds 52.5%,14 Nigeria,31 Pakistan 29.4%,6 Belahara VDC of Dhankuta district 27%,32 and Bangladesh 33%.33
The possible reasons might be due to different study periods in between the studies, and most studies were nationwide while this study was specific to one town.
In the present study fathers’ educational level was one of the predictors of underweight among children age 6–59 months. Fathers who have primary and below the level of education were 2 times more likely to have underweight children than those fathers’ who have secondary and above level of education in their educational status. The result is supported by the research done in Tigray region Ethiopia,27 Bangladesh,33 Khyber Pakhtunkhwa.15
An-other predictor of underweight for children age from 6 to 59 months was the sex of the child. Male children were 1.8 times more likely to have under-weight nutritional status than those female children. This finding is supported by a study done in EDHS Ethiopia (2016).25
Tigray region Ethiopia,27 Oromia region Ethiopia,10 Bula Hora Ethiopia,20 Somalia region Ethiopia,21 South Ethiopia,17 sub-Saharan Africa,7 Machakos country.34
Wealth status in the family has great importance for the occurrence of mal-nutrition typical under nutrition for children in developing countries. In this study families who have poor wealth status 2 times more likely to have under-weighted children than those families who have rich wealth status. Because, children who have poor family wealth status lack adequate nutrition’s in their house-hold, and this leads to a nutritional imbalance between demand and supply. This finding is supported by the study done in Tigray region Ethiopia,27 Sub-Saharan Africa,7 Bangladesh.33
Limitations of the Study
The present study has some limitations. It was focused on children characteristics rather than environmental factors, and also the study is cross-sectional it does not show a cause-effect relationship between underweight and associated factors.
Conclusion
Among under nutrition of children age 6–59 months underweight is still a significant public health problem. Significantly associated factors with underweight for children age from 6 to 59 months were the father’s educational level, sex of the child (male), and wealth status of the family.
These findings have great importance for different stokeholds that have responsibilities on the reduction of under-nutrition typically underweight, besides this, it is important for policymakers for nutrition and nutrition-related intervention programs.
Abbreviations
ANC, Ante Natal Care; AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; ETB, Ethiopian Birr; HH, House Holds; KM, Kilo Meter; PCA, Principal Component Analysis; SPSS, Statistical Package for Social Sciences; WHO, World Health Organization.
Data Sharing Statement
Data will be available upon request from the corresponding author.
Ethical Approval and Consent to Participate
Ethical clearance was obtained from the school of the nursing ethical review committee on behalf of the University of Gondar review board. The verbal informed consent was acceptable and approved by the Ethical review board on the behalf of University of Gondar, and that this study was conducted under the declaration of Helsinki.
A permission letter was obtained from the Debre Tabor town department of health. Participants were informed about voluntarism and that they can withdraw at any time of the study if they want not respond. For those who were a volunteer to participate, verbal-informed consent was obtained from the parent/legal guardian/for the children involved in this study. At the end of the interview, participants were informed about underweight and associated potential effects.
Acknowledgment
The authors would like to thank Amhara Regional Health Bureau for its financial support. Besides, we want to acknowledge data collectors and supervisors for their commitment to collect the data accurately.
Author Contributions
All authors made substantial contributions to conception, design, acquisition of data, or analysis and interpretation of data. And took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published, and agree to be accountable for all aspects of the work. All authors have read and approved the final manuscript.
Funding
This research didn’t receive any grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest.
References
1. Organization WH. Malnutrition. The Global Picture Geneva. World Health Organization; 2000.
2. United Nations Children’s Fund WHO, The World Bank. UNICEF-WHO-World Bank Joint Child Malnutrition Estimates. Geneva; Washington, DC; New York, NY: UNICEF; WHO; The World Bank; 2012.
3. Organization WH. World Health Statistics 2010. World Health Organization; 2010.
4. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–451. doi:10.1016/S0140-6736(13)60937-X
5. Organization WH. Nutrition in Universal Health Coverage. World Health Organization; 2019.
6. Khan S, Zaheer S, Safdar NF. Determinants of stunting, underweight and wasting among children< 5 years of age: evidence from 2012–2013 pakistan demographic and health survey. BMC Public Health. 2019;19(1):358.
7. Akombi BJ, Agho KE, Hall JJ, Wali N, Renzaho A, Merom D. Stunting, wasting and underweight in sub-Saharan Africa: a systematic review. Int J Environ Res Public Health. 2017;14(8):863. doi:10.3390/ijerph14080863
8. Demographic CE. Health Survey-2011. Central Statistical Agency Addis Ababa. Maryland, USA: Ethiopia ICF International Calverton; 2012:2016.
9. Darsene H, Geleto A, Gebeyehu A, Meseret S. Magnitude and predictors of undernutrition among children aged six to fifty nine months in Ethiopia: a cross sectional study. Arch Public Health. 2017;75(1):29. doi:10.1186/s13690-017-0198-4
10. Taye A, Wolde T, Seid A. Under-nutrition and related factors among children aged 6–59 months in Gida Ayana District, Oromiya region, West Ethiopia: a community based quantitative study. J Nutr Food Sci. 2016;6(5):1–12.
11. Kassa ZY, Behailu T, Mekonnen A, Teshome M, Yeshitila S. Malnutrition and associated factors among under five children (6–59 months) At Shashemene Referral Hospital, West Arsi Zone, Oromia, Ethiopia. Curr Pediatr Res. 2017.
12. Haile A. Prevalence of undernutrition and associated factors among children aged 6–59 months in Bishoftu Town, Oromia Region, Ethiopia. Food Proc Nutr Sci. 2020;1(1):8–24.
13. Tufa EG, Dake SK, Bekru ET, et al. Magnitude of wasting and underweight among children 6–59 months of age in Sodo Zuria District, South Ethiopia: a community based cross-sectional study. BMC Res Notes. 2018;11(1):790. doi:10.1186/s13104-018-3880-x
14. Zeray A, Kibret GD, Leshargie CT. Prevalence and associated factors of undernutrition among under-five children from model and non-model households in east Gojjam zone, Northwest Ethiopia: a comparative cross-sectional study. BMC Nutr. 2019;5(1):27. doi:10.1186/s40795-019-0290-y
15. Ali W, Ayub A, Hussain H. Prevalence and associated risk factors of under nutrition among children aged 6 to 59 months in internally displaced persons of Jalozai Camp, District Nowshera, Khyber Pakhtunkhwa. J Ayub Med Coll Abbottabad. 2015;27(3):556–559.
16. Huynh G, Huynh QHN, Nguyen NHT, Do QT, Van Tran K. Malnutrition among 6–59-month-old children at district 2 hospital, Ho Chi Minh City, Vietnam: prevalence and associated factors. Biomed Res Int. 2019;2019.
17. Gamecha R, Demissie T, Admasie A. The magnitude of nutritional underweight and associated factors among children aged 6–59 months in Wonsho Woreda, Sidama Zone Southern Ethiopia. Open Public Health J. 2017;10(1):7–16. doi:10.2174/1874944501610010007
18. Nigatu G, Woreta SA, Akalu TY, Yenit MK. Prevalence and associated factors of underweight among children 6–59 months of age in Takusa district, Northwest Ethiopia. Int J Equity Health. 2018;17(1):106. doi:10.1186/s12939-018-0816-y
19. Akombi BJ, Agho KE, Merom D, Renzaho AM, Hall JJ. Child malnutrition in sub-Saharan Africa: a meta-analysis of demographic and health surveys (2006–2016). PLoS One. 2017;12(5):e0177338. doi:10.1371/journal.pone.0177338
20. Asfaw M, Wondaferash M, Taha M, Dube L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public Health. 2015;15(1):41. doi:10.1186/s12889-015-1370-9
21. Demissie S, Worku A. Magnitude and factors associated with malnutrition in children 6–59 months of age in pastoral community of Dollo Ado district, Somali region, Ethiopia. Sci J Public Health. 2013;1(4):175–183. doi:10.11648/j.sjph.20130104.12
22. Hintsa S, Gereziher K. Determinants of underweight among 6–59 months old children in Berahle, Afar, North East Ethiopia: a case control study 2016. BMC Res Notes. 2019;12(1):753. doi:10.1186/s13104-019-4805-z
23. Tosheno D, Mehretie Adinew Y, Thangavel T, Bitew Workie S. Risk factors of underweight in children aged 6–59 months in Ethiopia. J Nutr Metab. 2017;2017:1–8. doi:10.1155/2017/6368746
24. Yalew B, Amsalu F, Bikes D. Prevalence and factors associated with stunting, underweight and wasting: a community based cross sectional study among children age 6–59 months at Lalibela Town, Northern Ethiopia. J Nutr Disord Ther. 2014;4(147):2161–0509.1000147. doi:10.4172/2161-0509.1000147
25. Fenta HM, Tesfaw LM, Derebe MA. Trends and determinants of underweight among under-five children in Ethiopia: data from EDHS. Int J Pediatr. 2020;2020.
26. Tamiru MW, Tolessa BE, Abera SF. Under nutrition and associated factors among under-five age children of Kunama ethnic groups in Tahtay Adiyabo Woreda, Tigray Regional State, Ethiopia: community based study. Int J Nutr Food Sci. 2015;4(3):277–288. doi:10.11648/j.ijnfs.20150403.15
27. Woldeamanuel BT, Tesfaye TT. Risk factors associated with under-five stunting, wasting, and underweight based on Ethiopian demographic health survey datasets in Tigray region, Ethiopia. J Nutr Metab. 2019;2019.
28. Kelati H, Mengiste B, Alemayehu T, Damtew B. Prevalence of acute malnutrition and its associated factors among children aged 6–59 months in Mai-Aini Eritrean refugees’ camp, Northern Ethiopia. J Nutr Food Sci. 2014;5(1):336.
29. Mohieldin A. The impact of feeding practices on prevalence of under nutrition among 6–59 months aged children in Khartoum. Sudan J Public Health. 2010;5(3):151–157.
30. Mulugeta A, Hagos F, Kruseman G, et al. Child malnutrition in Tigray, northern Ethiopia. East Afr Med J. 2010;87(6):248–254.
31. Akombi BJ, Agho KE, Merom D, Hall JJ, Renzaho AM. Multilevel analysis of factors associated with wasting and underweight among children under-five years in Nigeria. Nutrients. 2017;9(1):44. doi:10.3390/nu9010044
32. Gurung C, Sapkota V. Prevalence and predictors of underweight, stunting and wasting in under-five children. J Nepal Health Res Counc. 2009.
33. Das S, Gulshan J. Different forms of malnutrition among under five children in Bangladesh: a cross sectional study on prevalence and determinants. BMC Nutr. 2017;3(1):1. doi:10.1186/s40795-016-0122-2
34. Mutua RN, Keriko J, Mutai J. Factors associated with stunting, wasting and underweight among children aged 2–5 years in early childhood development and education centers in masinga sub county, machakos county. Eur J Health Sci. 2017;1(2):44–69. doi:10.47672/ejhs.232
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.