Back to Journals » Risk Management and Healthcare Policy » Volume 12
Understanding Healthcare Utilization In China Through The Andersen Behavioral Model: Review Of Evidence From The China Health And Nutrition Survey
Authors Zhang S, Chen Q , Zhang B
Received 7 June 2019
Accepted for publication 23 October 2019
Published 11 November 2019 Volume 2019:12 Pages 209—224
DOI https://doi.org/10.2147/RMHP.S218661
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kent Rondeau
Shu Zhang,1 Qihui Chen,2 Bo Zhang3
1Institute of Agricultural Economics and Development, Chinese Academy of Agricultural Sciences, Beijing, People’s Republic of China; 2Center for Food and Health Economic Research, College of Economics and Management, China Agricultural University, Beijing, People’s Republic of China; 3Department of Neurology and ICCTR Biostatistics and Research Design Center, Boston Children’s Hospital and Harvard Medical School, Boston, MA 02115, USA
Correspondence: Bo Zhang; Qihui Chen Email [email protected]; [email protected]
Introduction: Factors influencing healthcare utilization in China have been frequently analyzed and discussed from various angles, based upon different objectives. However, few studies have attempted to categorize and summarize key determinants of healthcare utilization in China.
Methods: To fill this gap, we reviewed all empirical studies that made use of data from the China Health and Nutrition Survey (CHNS), a longitudinal survey covering nine Chinese provinces for nearly three decades. The review was guided by Andersen’s behavioral model, a conceptual framework widely used to analyze determinants of healthcare utilization.
Results: Our review discovered many strong and consistent predictors of healthcare utilization at the individual level, including predisposing factors (e.g., marriage status and education), enabling factors (e.g., income and wealth), and need factors (e.g., illness severity and health status); in contrast, contextual factors (e.g., employment rates and population health indices) have rarely been examined. Our review also revealed a few factors whose impacts differ from expectations in many studies (e.g., employment status and health insurance coverage). While several factors explored in the reviewed studies (e.g., urbanization and industrialization) are not part of Andersen’s model, some factors specified in the model (e.g., values and knowledge about health and health services) remain unexplored in the context of China.
Conclusion: Individual-level factors received much more attention than contextual-level factors in the reviewed studies. It leads to an inadequate understanding of the roles played by contextual factors. Among the individual-level factors that have been extensively examined, enabling variables affect healthcare utilization more than predisposing and need factors.
Keywords: healthcare utilization, health services, China, Andersen’s behavioral model
Introduction
Despite China’s numerous achievements over 40 years of economic reform, one enduring problem that could undermine the country’s future sustainable development is the large socioeconomic inequality among Chinese residents.1,2 Unequal access to healthcare is one key aspect of this problem. Inequitable healthcare utilization, in terms of the quality of healthcare services, access to medical facilities, efficiency of health insurance, etc., has been observed between rich and poor, between rural and urban inhabitants, and between the Han ethnic group and ethnic minority groups. (“Han Chinese,” “Han ethnicity,” or “Han ethnic group” refers to an East Asian ethnic majority group and nation native to China.3 In 2017, an estimated 1.3 billion Han Chinese were living in China, approximately 91.6% of the total population.4 There are 55 minority groups in China, but they account for only 8.4% of the population.) Unequal access is also seen across different regions in China.5–11
Healthcare utilization in China has been studied on numerous occasions; however, the existing findings are inconclusive. For example, the estimated relationship between the New Cooperative Medical Scheme (NCMS), a government-run health insurance program targeting the rural Chinese population, and health service utilization is not consistent across studies; some suggest that NCMS enrollment is not significantly associated with outpatient care,9,12 whereas others demonstrate that the NCMS increases the healthcare utilization of its enrollees and reduces their medical expenditures, especially with respect to poor people residing in the western regions.11,13 These mixed results make it difficult to develop a clear understanding of healthcare utilization in China and its determinants. For instance, studies that analyzed determinants without a clearly laid-out theoretical framework may raise concerns regarding “omitted-variable” bias. Furthermore, some findings disagree with previous studies, but the discrepancies remain unexplained, which casts doubt on the validity of these findings. Seeing a mountain of similar determinants and models with different findings, one naturally wonders: Which factors have been proven effective, and what should be improved in future research? Yet there exists no systematic analysis to answer these questions. Therefore, a comprehensive overview of the determinants of healthcare utilization in China, especially in terms of their ubiquity and the discrepancies in their influence, is needed to help inform policy-making regarding the promotion of healthcare utilization.
In this article, we attempt to provide a structured review by utilizing the framework of Anderson’s behavioral model,14,15 a classic model that has been widely adopted to understand healthcare utilization behavior in more developed settings. To the extent that China is currently transitioning from a lower-middle-income to an upper-middle-income country,16 this framework is expected to provide insights into potential changes in healthcare utilization behavior, expenditure patterns, and policy-making in the near future. Guided by this framework, we reviewed 16 key academic studies that relied upon data from the China Health and Nutrition Survey (CHNS), a longitudinal project that covers 12 provinces in China and spans nearly three decades (since 1989). More specifically, this review attempts to deepen our understanding of Chinese residents’ healthcare utilization from two perspectives, individual and contextual, involving three factors: predisposing, enabling, and need factors. The focus on CHNS-based studies ensures that the populations being examined in the reviewed studies are relatively consistent, thereby greatly enhancing the comparability of the research findings between studies. The long timespan covered in the CHNS data also allows us to assess the trends concerning access to and utilization of healthcare in China. Not only does our review provide a summary of the achievements and problems in the country’s healthcare system as revealed through the CHNS data, but it also identifies areas of future research that might help achieve efficient and equitable healthcare utilization in the near future.
The remainder of the article is structured as follows. “Healthcare utilization measurements in the China Health and Nutrition Survey” section provides a brief description of the CHNS and the measures of healthcare utilization upon which it relies. “Literature Retrieving Protocol” section describes our review methodology. “Review Framework” section briefly introduces the guiding framework of our analysis, i.e., the Andersen model. “Review Findings” section presents and discusses our key review findings. The final section concludes the article, derives policy implications, and points out a number of directions for future research.
Healthcare Utilization Measurements In The China Health And Nutrition Survey
Numerous studies have been conducted to examine individuals’ healthcare utilization behaviors. However, these studies were conducted in different contexts, usually based upon different underlying models, which renders their findings incomparable. To enhance the comparability of the findings of different studies, we focused our attention on studies that utilized data from the China Health and Nutrition Survey (CHNS), which constitutes one of the longest spanning datasets available in China and the most widely used dataset in studies on residents’ health-related behavior and outcomes, among other topics (all publications using CHNS data can be found at https://www.cpc.unc.edu/projects/china/publications, which included at least 1879 entries at the time of writing).
The CHNS is an international survey conducted collaboratively by the University of North Carolina at Chapel Hill and the Chinese Center for Disease Control and Prevention. The CHNS draws from a sample of approximately 7200 households, including over 30,000 individuals residing in 12 Chinese provinces and municipal cities that vary substantially in geographical features, economic development, public resources, and health indicators. In an effort to comprehensively explore the impacts of Chinese social and economic reforms on the health and nutritional status of the population, the CHNS collects detailed information not only from residents, but also from local food markets, family planning officials, and other community and social services (see the official website of the CHNS for more details: https://www.cpc.unc.edu/projects/china).
By design, the CHNS is a longitudinal household-based survey project, initially covering rural and urban areas of nine Chinese provinces (Guangxi, Guizhou, Heilongjiang, Henan, Hubei, Hunan, Jiangsu, Liaoning, and Shandong). The project has thus far completed 10 waves of surveys since the late 1980s (in 1989, 1991, 1993, 1997, 2000, 2004, 2006, 2009, 2011, and 2015). Three municipalities—Beijing, Chongqing, and Shanghai—were later included in 2011.
The CHNS includes three major components at different levels: household, individual, and community surveys. Sample households were selected using a multistage, stratified, random sampling procedure. In each CHNS province, two cities (one large, usually the provincial capital city, and one small, usually a lower-income city) and four counties were selected. All counties in a given province were stratified by income level (low, middle, and high), and a weighted sampling scheme was used to randomly select four of them. Within each chosen county, one community in the capital city and three rural villages were then randomly chosen. Within each municipality, two urban and two suburban communities were randomly selected. Finally, 20 households per community were selected to participate in the survey.
As the main component of the CHNS, the household survey collects detailed information on households’ sociodemographic configuration, household members’ economic activities (such as occupations and expenditures), time allocation among various activities (such as childcare and food purchasing), household assets, and healthcare and medical services utilization, as well as information regarding the local environment (such as drinking water and sanitation).
The individual survey, which was separated from the household survey component in 2004, contains questions related to individuals’ activities, marital status and lifestyle, and health status, highlighting health and nutrition issues such as physical activities; soft drink, alcohol, and caffeine consumption; smoking; diet structure; and body shape. The survey is designed separately for adults (aged 18 or older) and children (under age 18). Female respondents under the age of 52 are further asked to provide information on marriage, pregnancy, and birth history. For all respondents, a set of anthropometric indicators is also measured and recorded by medical professionals during the survey.
The community survey, filled out by administrative staff (e.g., village leaders) who are knowledgeable about the community (urban districts or rural villages), includes aspects of local health conditions (water, transportation, electricity, communication, etc.), services (family planning, health facilities, retail outlets, etc.), prevailing prices of food and specific living materials, and Global Positioning System (GPS) data on related locations in the community. Some public healthcare services information can also be found in the community survey.
The “Health services” section in the individual survey, standardized since 2004, is a key section that solicits information on healthcare and medical services among CHNS participants. In most survey waves, this section contains three parts: medical insurance, use of healthcare and medical services, and disease history. In general, information on illnesses and on all uses of the health system during the previous four weeks is collected for all household members. In addition to the individual survey, some related information on health services in the local community, such as the accessibility of medical services, is gathered in the community survey.
Literature Retrieving Protocol
An extensive literature search was initially conducted in November 2017 on the China Health and Nutrition Survey publications website (http://www.cpc.unc.edu/projects/china/publications) to retrieve studies on healthcare utilization in China using the CHNS data. The search using keywords “utilization,” “demand,” “use,” “service,” “services,” and “access” returned 10, 13, 16, 3, 8, and 13 publications, respectively, with a few duplicates. With a primary objective of reviewing studies relevant to healthcare utilization in China, the following four criteria were applied in the literature screening: 1) studies on “healthcare expenditure” and other aspects of healthcare services, rather than on “healthcare utilization,” were excluded; 2) studies that did not focus on the CHNS database were excluded; 3) studies that used “healthcare utilization” or “access to healthcare” as an explanatory variable in their analysis were excluded; given that our aim was to review factors impacting healthcare utilization in China, only studies that treated “use of healthcare” as the outcome variable of interest were included; and 4) non-English studies were not included. Applying these criteria, a total of 16 publications (one thesis, one book chapter, 11 journal articles, and three working papers) from the CHNS publication database were finally included in this review (see Table 1 for the full list of publications; Li et al17 was added after the search).
 |
Table 1 Basic Information On The Reviewed Studies |
Review Framework
Guiding Framework: Anderson’s Behavioral Model
Our review was conducted under the guiding framework of Anderson’s behavioral model of health services utilization, which has been widely used as a conceptual framework for understanding access to and utilization of health services.14,15 Originally developed by Ronald M. Andersen,26,27 this model suggests that healthcare utilization is determined by three key factors: predisposing, enabling, and need factors at both the individual and contextual level.
At the individual level, predisposing factors include demographic characteristics (e.g., age, sex, race/ethnicity, marital status), socioeconomic characteristics (e.g., education, social class, and employment status), and health beliefs (e.g., attitudes, values, and knowledge of health and health services). Enabling factors refers to resources or means that enable individuals to obtain health services, usually involving individual and community resources, such as health insurance, income, wealth, availability of services, and rural–urban strata, as well as resources or means that may impede healthcare service use. Need factors, conceptualized as either need perceived by the individual or need evaluated by professionals, are the most direct and important factors impacting health service utilization and are thus considered to be more immediate and powerful predictors of service use than predisposing or enabling factors.14
While individuals’ healthcare needs, resources, and predisposition reflect their behavioral choices, social structure signifies changes in the environment constrained by the neighborhood and society.15 Contextual factors are defined as conditions at the societal or community level that are beyond individual control, including environmental, macroeconomic, and policy factors. For example, environmental factors include employment rate, crime rate, social norms related to health services and health expenditure, and availability of healthcare providers, which can influence individuals’ perception of health service utilization. In terms of the influence of health policies as a contextual factor, a case in point is health insurance programs. For example, major health insurance policies implemented in China since the 1990s, such as the New Cooperative Medical Scheme (NCMS), the Urban Resident Basic Medical Insurance (URBMI), and the Urban Employee Basic Medical Insurance (UEBMI), provide their customers with different types of health insurance, reimbursement methods, and subsidy structures, which may influence Chinese residents’ access to and utilization of health services. In Andersen’s framework, contextual factors are also classified into three categories: contextual predisposing factors (e.g., demographic, social, and belief factors), contextual enabling factors (e.g., health policy, financing, and organization), and contextual need factors (e.g., environmental and population health indices).
Method For Summarizing Review Findings
In analyzing and summarizing the review findings, the Andersen model was first conceptualized as a “variable tree” that presents logical linkages among specific variables at various levels (Figure 1). We then compared each of the reviewed studies with the “variable tree” to investigate whether a particular variable specified in the conceptual model (e.g., a predisposing variable such as education or income) was employed in the study under review. If a particular variable was included in any of the 16 publications, we then summarized the regression results from all the studies involving that variable—in particular, typical findings and unique patterns revealed by the reported regressions—to determine the role that the particular variable played in affecting one’s healthcare utilization. In doing so, we were able to not only uncover gaps in our knowledge of the determinants of healthcare utilization in China (and thus the direction of future research and policy design), but also assess the performance of Andersen’s model in guiding researchers and policymakers to understand the functionality of the country’s health sector and healthcare system.
 |
Figure 1 Andersen’s behavior model of healthcare utilization. |
Review Findings
A recent study conducted by Li et al,17 which is also reviewed in this article, summarizes a number of important patterns of healthcare utilization in China from 1993 to 2011, based on the CHNS data. As shown by Li et al,17 the majority of patients, urban (58.87%) or rural (62.67%), chose outpatient care as their primary treatment option throughout the entire period of 1993–2011. However, the trend of outpatient care did not monotonously increase during this period. More specifically, both rural and urban adults’ utilization exhibited an increase in outpatient care during the mid-1990s, but there has been a slight declining trend since the mid-2000s. During the same period, a gradual increase in self-care was observed among rural and urban residents, in contrast to inpatient care. Note that since China started to implement a series of reforms in its healthcare system in the mid-2000s, the slight decline in formal healthcare (both outpatient and inpatient) after 2004 suggests that factors other than health policy and health insurance programs may be driving Chinese residents’ healthcare utilization behavior.
This section reports the main findings of our structured review of 16 key CHNS-based empirical studies, which involved 75 regressions on the determinants of healthcare utilization in China.
Individual-Level Factors
As noted in “Guiding framework: Anderson’s behavioral model” section, Andersen’s conceptual model involves three key factors—predisposing, enabling, and need factors—that may affect healthcare utilization at both the individual and contextual level.
Predisposing Factors
At the individual level, predisposing factors reflect influences coming from four aspects of life: demographics, social factors, genetics, and beliefs (Table 2).
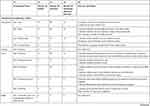 |  | 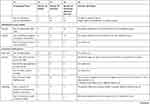 |  |
Table 2 Estimated Impacts Of Individual And Contextual Characteristics In Studies Reviewed |
The most frequently employed demographic variables include sex, age, marital status, and household structure. The influences of sex and marital status found in the reviewed studies (14 employing sex and 10 employing marital status) were quite consistent: in various contexts (e.g., whether one sought care at a medical or public health facility or used any kind of preventive care during the last four weeks), women are more likely to utilize healthcare than men (Table 2, row 1), and married individuals are less likely to utilize healthcare than other individuals (Table 2, row 3). A possible explanation for these patterns is that men and married individuals have a higher price elasticity of demand for healthcare than women and unmarried individuals, whereas women with specific physiological conditions (e.g., pregnancy) have a lower elasticity of demand for healthcare.7,28
Somewhat surprisingly, the influence of age found in these studies was rather mixed: while seven regressions found that individuals are likely to reduce healthcare utilization as they become older, another seven regressions found the opposite pattern (Table 2, row 2). In theory, the influence of age is ambiguous. On the one hand, young people tend to invest more in their human capital (e.g., education and health), simply because they have a longer horizon during which to recoup returns on their investments;29 on the other hand, younger people are generally healthier than the elderly and are thus less concerned about their own health. The lack of consensus on the impact of age suggests that more research should be conducted to examine why these discrepancies in the findings exist, thereby helping to deepen the understanding of the real impact of age, which is of particular importance for a society with a large aging population such as China.30 For example, any attempt to understand the impact of age among elderly individuals should isolate it from other confounding factors, such as retirement, which has been found to greatly change elderly individuals’ food consumption structure in China,31 which may have important implications for their health and health-related behavior.
Finally, household size and structure variables were analyzed in two studies, which found that household size is negatively correlated with the utilization of formal medical services.11,22 Because China has now relaxed its population policy (the so-called one-child policy),32 the average household size is expected to increase, although at a modest scale.33 Thus, proper measures may need be taken in the near future to mitigate the potential negative effects of increasing household size.
In the social dimension, education has been found to be a significant predictor of healthcare utilization in China (Table 2, row 6). Our findings support the commonsense conclusion that better-educated individuals tend to use more formal services and preventive care, whereas less-educated individuals are more likely to seek informal healthcare.6,7,10,11 Individuals who have completed more years of education are usually better informed about potential health risks and problems.34–37 They also tend to be wealthier and thus better able to cope with health problems using their relatively more abundant resources.38
In contrast, another two social factors in Andersen’s model, employment (Table 2, row 7) and occupation (Table 2, row 8), do not seem to be key determinants of Chinese individuals’ healthcare utilization behavior. Only two studies found that employed individuals tend to use more healthcare services than unemployed individuals.6,11 Additionally, three regressions (in two studies) revealed an ambiguous relationship between occupation and healthcare utilization.6,8 Three other studies examined the relationship between the ownership type of enterprises (state-owned enterprises (SOEs), collective, and private) and employees’ healthcare utilization behavior.8,18,19 Most of the regressions in these three studies found that SOE employees tend to utilize more healthcare, presumably because SOEs usually offer workplace clinics and comprehensive insurance coverage to their employees; only one regression showed the opposite.8,18
With regard to the role of ethnicity as a social factor in Andersen’s model, among the several studies that examined this factor,7–9 only one demonstrated that, compared with Han individuals, ethnic minorities have less access to hospitals than to clinics (Table 2, row 10).7 To the extent that ethnic minorities usually reside in remote and mountainous areas in China,39 this finding suggests that more hospitals may be needed in those areas.
It is worth noting that none of the reviewed studies examined the roles of “genetics” or “beliefs” variables (i.e., attitudes, values, and knowledge about health and health services) (Table 2, rows 4 and 11), which is presumably due to the lack of data on these variables. To the extent that genetics or beliefs have an important impact on people’s health behavior and health outcomes,40–42 they are likely to also impact their utilization of healthcare services. Thus, future studies that examine the roles of these factors are expected to be fruitful.
Enabling Factors
Individual-level enabling factors include two categories: financing and organizational factors.
The most important financing factors include income (wealth) (Table 2, row 12) and health insurance coverage (Table 2, row 13), each playing an important role in the reviewed studies. More than 85% of the regressions reviewed used individual income or family wealth as an explanatory variable. Not surprisingly, the influence of income is statistically significant in general—nearly three-fourths of the statistically significant regressions reported in these studies found that wealthier individuals use significantly more healthcare than their less-wealthy counterparts (Table 2, row 12). Note, however, that four regressions from one study, that of Liu and Zhao,22 found that low-income individuals use more healthcare. This study argues that low- and middle-income families have more access to healthcare services due to their enrollment in the Urban Resident Basic Medical Insurance (URBMI) program. Some authors also considered the impact of community-level healthcare prices, which, in theory, serves as an opposing factor to income and wealth, but most of the estimates of price effects are not statistically significant (Table 2, row 30).5,7,22,21 These findings suggest that further economic growth is likely to induce more Chinese individuals to utilize healthcare services.
Furthermore, roughly 90% of the regressions we reviewed employed individual insurance coverage as an explanatory variable; five studies even focused on estimating the (causal) effect of health insurance on healthcare utilization.9,11,22,25,23 More than half of the 68 regressions found significant impacts of health insurance coverage, and more than two-thirds of those regressions showed that individuals covered by healthcare insurance programs (e.g., NCMS, URBMI, etc.) use more medical care than their uninsured counterparts (Table 2, row 13). Interestingly, however, there were still 10 regressions (from six studies) that found a statistically significant and negative impact of health insurance coverage on healthcare utilization.6,8,11,18,25 Several explanations have been proposed. One study suggested that the negative impact of health insurance coverage on healthcare seeking was presumably due to insufficient observations (only 19 observations in the specific regression) and thus was not a generalizable finding.18 Others argued that the respondents may have been covered by health insurance programs other than the NCMS, so that the comparison group was a combined group consisting of uninsured people and people covered by other programs, which led to a downward bias in the estimated impact of the NCMS.11 Others suggested that reforms of health insurance programs (e.g., URBMI) increased health insurance cost sharing through a combination of deductions, coinsurance, etc., which caused the demand for healthcare to decrease afterwards.25 Finally, it is also possible that those covered by the NCMS and other insurance programs were less likely to visit folk doctors compared with people who are uninsured.6
The third financing factor in the Andersen framework, social support, defined as any “emotional, informational, tangible, and affectionate support generated through the social network,” was not examined in any of the reviewed studies (Table 2, row 14).
As the second category of individual-level enabling factors, organization of health services is defined as the availability of a regular source of medical care or transportation to that source. The most commonly chosen measures in the reviewed studies were transportation time and method. Although there were rarely statistically significant regression results (Table 2, rows 16–19), the relationship between the use of a speedy travel method and access to more qualified medical care (such as a hospital) can be summarized as a positive trend.7 However, the estimated relationship between travel time and the use of care is still inconclusive; some found it to be negative,11,19 while others found it to be positive, and the explanation is that some individuals will be willing to take more time to travel for more advanced healthcare services.7,11
It is worth noting that the variable urban–rural strata was viewed as an enabling factor in the earliest literature that we reviewed.8 However, as the complexity increased over time and due to the different insurance programs provided in urban and rural areas, many CHNS-based studies focused separately on urban and rural residents, which eliminates the opportunity to a draw rural–urban comparison. Among the studies that found a significant rural–urban gap in healthcare utilization, the direction is not conclusive, although more regressions (nine versus four) showed that the likelihood of utilizing healthcare is much higher among urban adults than rural adults.5,9,17 Other variables related to the dynamic of the rural–urban relationship, such as urbanization and the “side effect” of industrialization, were also discussed in a previous study (Table 2, rows 21–22).21 The authors found that urbanization variables had no significant effect on the demand for healthcare. Additionally, industrialization had a negative impact on the healthcare demand in rural areas because of the increasing percentage of people working outside villages.
Need Factors
The major components of individual-level need factors are self-perceived health status and health status evaluated by medical professionals. Because the severity of illness is one of the most important factors that affects healthcare utilization, 12 studies used health status as an explanatory variable in their regressions; nine of them preferred the self-perceived measure (presumably due to the inaccessibility of doctor-rated health status data) and three used chronic conditions (Table 2, rows 23–24). Consistent with common sense, all regressions, regardless of which specific measure was being used, found a statistically significant association between the severity of illness and healthcare utilization.
Contextual Factors
Rarely have existing studies on healthcare utilization in China examined contextual characteristics. None of the reviewed studies included contextual predisposing factors or need factors, such as a community-level predisposing index (e.g., demographic characteristics of a community, including its age, gender, and marital status composition), health-related measures of the physical environment, population health indices, etc., in their analyses (Table 2, rows 28–35). Only a few regressions employed some contextual enabling factors, e.g., community financing levels,10 amount and distribution of health service facilities and personnel, and the quality of services provided.7,10,22,19,20 The results are, in general, intuitive: higher levels of per capita community income, more healthcare facilities, and better qualified doctors in the community enable individuals to access more healthcare.
Discussion
Patterns Identified Under Andersen’s Framework
Andersen’s model is one of the most classic and comprehensive conceptual frameworks for understanding the multiple dimensions of access to and utilization of healthcare. Many studies have also quoted this model as the underlying conceptual framework of their regression models.8–10,21,43 Although the specific Chinese context and limitations of the CHNS database impose certain constraints on comprehensive application of the full model, a number of general patterns from the studies reviewed above can still be identified under the guidance of Andersen’s framework.
First, much more attention was paid to individual-level than contextual-level factors, which leads to an inadequate understanding of the roles of contextual factors (especially predisposing and need factors) in the context of China. In Andersen’s model, the contextual module includes the effects of macro- or community-level factors on healthcare utilization, such as the average levels of various predisposing factors among the population of interest and environmental- and health-related measurements, as well as specific rates of mortality, morbidity, and disability of the population. Yet these factors are generally absent from the reviewed studies (Table 2, rows 28–35). While some studies do include regional dummies in their regressions, that approach does not allow for an assessment of the impact of underlying contextual factors. Future research may incorporate more contextual factors (especially predisposing and need factors such as demographic characteristics of a community, health-related measures of the physical environment, population health indices, etc.) in the empirical model to gain a deeper understanding of how community and environmental factors help shape Chinese residents’ healthcare utilization behavior.
Second, a comparison of the influences of different variables employed in the reviewed studies clearly suggests that enabling variables, such as income and wealth, health insurance coverage, and geographic location (e.g., rural versus urban), affect healthcare utilization more significantly than predisposing and need factors. In other words, Chinese individuals’ healthcare utilization depends not only on a pure demand for curing illness or improving physical fitness, but also on other socioeconomic attributes, and the latter may play a more important role. This finding implies that the socioeconomic development of Chinese society in the near future will likely boost individuals’ healthcare utilization. The significant impacts of enabling factors (especially those found to be conditional on the impacts of need factors) also predict that the decline in socioeconomic inequality in China since 20081,2 is likely to reduce inequality in healthcare utilization in the near future.
Third, research on issues related to Chinese individuals’ healthcare utilization attempts to extend Andersen’s framework and incorporate unique features of the country’s socioeconomic development, including not only the evolution of medical insurance programs, but also issues related to urbanization, industrialization, social inequality, etc. (Table 2, rows 21–22). Regardless of whether these variables can be incorporated smoothly into the original Andersen framework as coherent components, these attempts have already greatly pushed forward the evaluation of the effectiveness of China’s healthcare policy. More empirical research on and evidence related to these fields are clearly needed to illuminate the mechanism behind a society’s development and the functionality of its healthcare system. Taking China’s healthcare system and reforms as case studies, future research may be able to expand the scope of Andersen’s model to incorporate more features of the developing world.
Lastly, our structured review reveals some factors whose impacts differ from expectations. For instance, the influence of age on healthcare utilization is not unidirectional; while some studies found that individuals utilize more healthcare services as they age, other studies found the opposite pattern (Table 2, row 2). Most surprisingly, some studies found that health insurance coverage may even negatively impact healthcare utilization (Table 2, row 13). These unexpected findings would not have been revealed without this review. They also highlight the pressing need for further scrutiny of variables that yield unexpected impacts: Are they caused by methodological flaws or by actual problems relating to China’s healthcare system?
Implications For Healthcare Utilization In China In The Near Future
Given several clear directions in China’s socioeconomic development and related policies, the above review findings could help predict the trend of Chinese individuals’ healthcare utilization in the foreseeable future, from various perspectives.
From a demographic perspective, rapid population aging, combined with government policies that raise elderly individuals’ income, is expected to induce more healthcare utilization in both rural and urban China. As in many other economies in East Asia, China is currently at its peak of population aging. In 2017, the proportion of Chinese citizens above 60 years old reached 241 million, representing 17.3% of the population.44 While our review did not find a consistent pattern of age effects (Table 2, row 2), we expect population aging to have a positive impact on healthcare utilization in the near future, as elderly individuals’ disposable income is likely to increase significantly, for two reasons. First, China has recently implemented a universal pension program targeting its rural population,45 which will certainly raise rural elders’ disposable income. Second, China is considering raising the official retirement age for public employees from 60 to 65 for men and from 55 to 60 for women,46 which will certainly increase disposable income for many urban elders. Given our review finding of the overall positive and statistically significant income effect (Table 2, row 12), the additional pension income and salary can be expected to induce elders to utilize more healthcare services.
Another potential demographic trend is increased average household size owing to the recent relaxation of China’s one-child policy,32 which, given our finding of a negative household-size effect (Table 2, row 4), is likely to reduce healthcare utilization for some households with multiple children. However, recent survey findings also suggest that the willingness to have a second child among Chinese couples is at best modest.33 Thus, the increased household size due to the relaxation in population policy and the resulting negative effect on healthcare utilization are likely to also be modest.
From a socioeconomic development perspective, China’s robust economic growth is likely to drive up healthcare utilization in the near future. While economic growth has slowed down somewhat recently, the current gross domestic product (GDP) growth rate (around 6.5%) is still among the highest in the world. According to the World Bank, China has become an upper-income country.16 Given the robust growth of the Chinese economy, our review finding of the positive effect of income/wealth (as an enabling factor; Table 2, row 4) predicts that Chinese individuals will utilize more healthcare in the near future. In addition, the decline in socioeconomic inequality in China since 2008, owing largely to government policies,1,2 is likely to reduce inequality in healthcare utilization in the near future.
From a policy perspective, our review findings suggest that some contextual enabling factors, such as community income, health insurance coverage, amount and distribution of health service facilities and personnel, and quality of services provided, all help to push up healthcare utilization. The implementation of the “Healthy China” plan (2030) will certainly enhance the aforementioned aspects of health policy in China,47 inducing more healthcare utilization in the near future.
Conclusion
Focusing on healthcare utilization in China, this article reviewed 16 studies that used the CHNS data to study realized access to healthcare. The impacts of contextual and individual factors on healthcare utilization in China were carefully summarized and discussed under the framework of Andersen’s behavioral model. Two conclusions can be drawn from our structured summary: First, individual-level factors received much more attention than contextual-level ones in the reviewed studies, which leads to an inadequate understanding of the roles played by contextual factors (especially predisposing and need factors, such as demographic characteristics of a community, health-related measures of the physical environment, population health indices, etc.) in the context of China. Second, among the individual-level factors that have been extensively examined, enabling variables, such as income and wealth, health insurance coverage, and geographic location (e.g., urban versus rural), affect healthcare utilization more significantly than predisposing and need factors. Given the ongoing demographic and socioeconomic trends in China, these individual-level enabling variables predict that healthcare utilization is likely to increase in the near future. Yet, to improve utilization and achieve equitable access to healthcare facilities, additional research needs to be done to further investigate the understudied factors that may influence such utilization.
Our review also revealed several unexpected findings: First, several regressions found a statistically significant and negative impact of health insurance coverage on healthcare utilization. Second, the influence of age in these studies was rather mixed: while half of the studies found that younger individuals utilize more healthcare services than elderly individuals, the other half found the opposite. Fourth, while (self-reported) health status has been explored to created explanatory variables for healthcare utilization, the existing explanatory variables in this dimension are all measures of physical health status; mental health issues remain largely untouched. Finally, none of the reviewed studies examined the roles of “genetics” or “beliefs” variables (i.e., attitudes, values, and knowledge about health and health services).
Finally, in this review, factors that were previously not explored in the Andersen model (e.g., urbanization, industrialization, and social inequality) were examined, which suggest a need to expand the scope of the original model and develop more guided frameworks to incorporate these factors in future studies. Moreover, inconsistent results urge us to consider possible homogeneity in the impacts of these variables; more research is thus needed in this regard. Moreover, with respect to healthcare management and policies, some phenomena relating to inequality (especially the rural–urban divide) were also explored, but this line of research is still in its early stage. Further research may continue to focus on and improve upon this line of inquiry in the future.
Acknowledgements
Dr. Shu Zhang’s research was partially supported by the Funds for International Cooperation and Exchange of the National Natural Science Foundation of China, grant no. 71761147004, and the Central Public-interest Scientific Institution Basal Research Fund from the Chinese Academy of Agricultural Sciences, grant no. 161005201901-1-1. Dr. Qihui Chen’s research was partially supported by the Humanities and Social Sciences Fund of the Ministry of Education of China, grant number 18YJC790010. We thank Dr. Ning Zhang from the University of Massachusetts Amherst for her discussion with the research team and her initial effort on “Guiding framework: Anderson’s behavioral model” section, which brought our attention to Anderson’s behavioral model as a conceptual framework for understanding utilization of health services.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhuang J, Li S. Understanding recent trends in income inequality in the People’s Republic of China. ADB Economics Working Paper. 2016.
2. Jain-Chandra S, Khor N, Mano R, et al. Inequality in China – trends, drivers and policy remedies. IMF Working Paper; 2018. doi:10.5089/9781484357538.001
3. Wang Y, Lu D, Chung Y, Xu S. Genetic structure, divergence and admixture of Han Chinese, Japanese and Korean populations. Hereditas. 2018;155:19. doi:10.1186/s41065-018-0057-5
4. Central Intelligence Agency. China. CIA World Factbook. 2019. Web. Accessed August 11, 2019.
5. Xie E. Income-related inequalities of health and healthcare utilization. Front Econ China. 2011;6:131–156. doi:10.1007/s11459-011-0125-5
6. Yang W. China’s new cooperative medical scheme and equity in access to healthcare: evidence from a longitudinal household survey. Int J Equity Health. 2013;12:1–13. doi:10.1186/1475-9276-12-20
7. Vedom J, Cao H. Patterns of the use and the choice of healthcare facilities among the Han and Minority populations in China. In: Cao H, editor. Ethnic Minorities and Regional Development in Asia: Reality and Challenges. Chapter 5. Amsterdam: Amsterdam University Press; 2009:65–82.
8. Henderson G, Akin J, Li Z, et al. Equity and the utilization of health services: report of an eight-province survey in China. Social Sci Med. 1994;39:687–699. doi:10.1016/0277-9536(94)90024-8
9. Lei X, Lin W. The New Cooperative Medical Scheme in rural China: does more coverage mean more service and better health? Health Econ. 2009;18:S25–S46. doi:10.1002/hec.v18.2s
10. Fan L, Liu J, Habibov NN. A multilevel logit estimation on the determinants of utilization of preventive healthcare and healthy lifestyle practice in China. World Med Health Policy. 2015;7:309–328. doi:10.1002/wmh3.160
11. Liu D, Tsegai D. The New Cooperative Medical Scheme (NCMS) and its implications for access to healthcare and medical expenditure: evidence from rural China. ZEF Discussion Papers Dev Policy. 2011;155:1–42.
12. Yu B, Meng Q, Collins C, et al. How does the New Cooperative Medical Scheme influence health service utilization? A study in two provinces in rural China. BMC Health Serv Res. 2010;10:1–9. doi:10.1186/1472-6963-10-116
13. Wagstaff W, Magnus L, Gao J, et al. Extending health insurance to the rural population: an impact evaluation of China’s new cooperative medical scheme. J Health Econ. 2009;28(1):1–19. doi:10.1016/j.jhealeco.2008.10.007
14. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. doi:10.2307/2137284
15. Andersen RM, Davidson PL, Baumeister SE. Improving access to care. Changing US Healthcare Syst. 2013;33–69.
16. World bank. China Overview. Available from: https://data.worldbank.org/country/china.
17. Li J, Shi L, Liang H, et al. Urban-rural disparities in health care utilization among Chinese adults from 1993 to 2011. BMC Health Serv Res. 2018;18(1):102. doi:10.1186/s12913-018-2905-4
18. Henderson GE, Akin JS, Hutchinson PM, et al. Trends in health services utilization in eight provinces in China. Social Sci Med. 1998;47:1957–1971. doi:10.1016/S0277-9536(98)00337-2
19. Chen C, Liu T. Healthcare utilization after economic reform in mainland China: a multinomial logit approach. Issues Stud. 2001;37:87–104.
20. Akin JS, Dow WH, Lance PM, et al. Changes in access to healthcare in China, 1989–1997. Health Policy Plan. 2005;20:80–89. doi:10.1093/heapol/czi010
21. Milcent C, Feng J. Decrease in the healthcare demand in rural China: a side effect of the industrialization process. PSE Working Papers n2010. Vol. 10; 2010:1–31.
22. Liu H, Zhao Z. Impact of China’s urban resident basic medical insurance on healthcare utilization and expenditure. Discussion Paper series, Forschungsinstitut zur Zukunft der Arbeit Vol. 6768; 2012:1–33.
23. Zhan Z. The relationship between urban resident basic medical insurance and health utilization of the urban unemployed in China. Master dissertation research paper, Georgetown University. 2013;1–28.
24. Dai B. Does China’s new cooperative medical scheme promote rural elders’ access to healthcare services in relation to chronic conditions? Int Health. 2015;7:32–41. doi:10.1093/inthealth/ihu050
25. Huang F, Gan L. The impacts of China’s urban employee basic medical insurance on healthcare expenditures and health outcomes. Health Econ. 2015;26:149–163. doi:10.1002/hec.3281
26. Kehrer BH, Andersen RM, Glaser WA. A behavioral model of families’ use of health services. J Hum Resour. 1972;7(1):125. doi:10.2307/145064
27. Andersen RM, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Memorial Fund Q J. 1973;51:95–124. doi:10.2307/3349613
28. Manning WG, Phelps CE. The demand for dental care. Bell J Econ. 1979;10(2):503–525. doi:10.2307/3003349
29. Cropper ML. Health, investment in health, and occupational choice. J Political Economy. 1977;85(6):1273–1294. doi:10.1086/260637
30. Sander M, Oxlund B, Jespersen A, et al. The challenges of human population ageing. Age Ageing. 2015;44:185–187. doi:10.1093/ageing/afu189
31. Chen Q, Deng T, Bai J, et al. Understanding the retirement-consumption puzzle through the lens of food consumption−fuzzy regression-discontinuity evidence from urban China. Food Policy. 2017;73:45–61. doi:10.1016/j.foodpol.2017.09.006
32. Chen Q. Relaxed population policy, family size and parental investments in children’s education in rural Northwestern China. Int J Educ Dev. 2017;54(C):39–50. doi:10.1016/j.ijedudev.2017.03.009
33. Fang D, Pei M. Study on the influencing factors of residents’ fertility intention ——based on the empirical research of CGSS2015 data. World Surv Res. 2018;9:9–13. in Chinese.
34. Arendt JN. Education effects on health: a panel data analysis using school reform for identification. Econ Educ Rev. 2005;24(2):149–160. doi:10.1016/j.econedurev.2004.04.008
35. Braakmann N. The causal relationship between education, health and health related behavior: evidence from a natural experiment in England. J Health Econ. 2011;30:753–763. doi:10.1016/j.jhealeco.2011.05.015
36. Parinduri RA. Does education improve health? Evidence from Indonesia. J Dev Stud. 2017;53(9):1358–1375. doi:10.1080/00220388.2016.1228880
37. Zhong H. Effects of quantity of education on health: a regression discontinuity design approach based on the Chinese Cultural Revolution. China Econ Rev. 2016;41:62–74. doi:10.1016/j.chieco.2016.08.011
38. Zhao M, Konishi Y, Glewwe P. Does information on health status lead to a healthier lifestyle? Evidence from China on the effect of hypertension diagnosis on food consumption. J Health Econ. 2013;32(2):367–385. doi:10.1016/j.jhealeco.2012.11.007
39. Zhao Q, Chen Q, Xiao Y, et al. Saving forests through development? Fuelwood consumption and the energy-ladder hypothesis in rural southern China. Transformations Bus Econ. 2017;16(3):199–219.
40. Waters EA, Muff J, Hamilton JG. Multifactorial beliefs about the role of genetics and behavior in common health conditions: prevalence and associations with participant characteristics and engagement in health behaviors. Genet Med. 2014;16(12):913–921. doi:10.1038/gim.2014.49
41. Short SE, Stefanie M. Social determinants and health behaviors: conceptual frames and empirical advances. Curr Opin Psychol. 2015;5:78–84. doi:10.1016/j.copsyc.2015.05.002
42. Zhu C, Zhang X, Zhao Q, et al. Hybrid marriages and phenotypic heterosis in offspring: evidence from China. Econ Hum Biol. 2018;29:102–114. doi:10.1016/j.ehb.2018.02.008
43. Phillips KA, Morrison KR, Andersen R, et al. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33(3, Part I):571–596.
44. NBSC (National Bureau of Statistics China). China Statistical Yearbook. China: China Statistics Press;2017. (in Chinese).
45. Zhao Q, Brosig S, Luo R, et al. The new rural social pension program in rural China: participation and its correlates. China Agric Econ Rev. 2016;8(4):647–661. doi:10.1108/CAER-07-2016-0116
46. Feng Q, Yeung WJ, Wang Z, et al. Age of retirement and human capital in an aging China, 2015–2050. Eur J Popul. 2019;35(1):29–62. doi:10.1007/s10680-018-9467-3
47. State Council. Outline for “Healthy china” Plan (2030). Beijing: State Council; 2016. Available from: http://news.xinhuanet.com/health/2016-10/25/c_1119786029.htm.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
