Back to Journals » Integrated Pharmacy Research and Practice » Volume 8
Undergraduate pharmacy students’ attitudes and perceived barriers toward provision of pharmaceutical care: a multi-institutional study in Nepal
Authors Baral SR , Parajuli DR, Shrestha S , Acharya SR, Dahal P , Poudel P , Ghimire S, Palaian S , Shrestha N
Received 28 January 2019
Accepted for publication 26 April 2019
Published 5 June 2019 Volume 2019:8 Pages 47—59
DOI https://doi.org/10.2147/IPRP.S203240
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Jonathan Ling
Sanjay Raj Baral1,* Daya Ram Parajuli,2,* Shakti Shrestha,3,* Santosh Raman Acharya,4 Prasanna Dahal,5 Prakash Poudel,6 Saruna Ghimire,4 Subish Palaian,7 Naveen Shrestha8
1Department of Pharmacy and Pharmacology, Chitwan Medical College, Bharatpur-10, Chitwan, Nepal; 2School of Nursing and Health Sciences, Flinders University, Adelaide, Australia; 3School of Pharmacy, University of Queensland, Brisbane, QLD, Australia; 4Department of Pharmacy, Valley College of Technical Sciences, Kathmandu, Nepal; 5Department of Pharmacy, College of Medical and Allied Sciences, Purbanchal University, Gothgaun, Morang, Nepal; 6Department of Pharmacy, Novel Academy, Pokhara-8, Nepal; 7College of Pharmacy, Gulf Medical University, Ajman, UAE; 8CiST College, Kathmandu, Nepal
*These authors contributed equally to this work
Background: Pharmaceutical care (PC) has a significant impact on optimizing pharmacotherapy and improving patients’ quality of life. We aimed to determine the attitudes and perceived barriers of final year pharmacy undergraduates towards provision of PC services in Nepal.
Methods: A cross-sectional study was conducted among 232 students using a 13-item-standard PC attitude survey (PCAS) questionnaire and 12-itemed PC barrier questionnaires. Mann–Whitney U test and Kruskal–Wallis tests were used to measure the median difference between groups, at alpha=0.05, and Spearman’s rho test was used to measure the strength of the correlation.
Results: Majority of students were self-motivated in undertaking the current pharmacy education (178, 76.7%) and had no previous incomplete grades that could delay their graduation (177, 76.3%). Over 80% of students had a positive attitude toward all items of PCAS (agreed and strongly agreed) except for two items. Whereas, 61 (26.3%) disagreed and strongly disagreed that providing PC takes too much time and effort. The major barriers perceived were inadequate PC training (176, 75.9%), inadequate drug information resources in the pharmacy (170, 73.3%), and lack of access to patient medical records in the pharmacy (165, 71.1%). A significant relationship was noticed between positive attitude towards PC and three factors; source of motivation, current employment in pharmacy job, and incomplete grades delaying graduation. Age factor was significant but negatively correlated with the scores of positive attitudes namely “I would like to perform PC as a pharmacist practitioner”, “Providing PC is professionally rewarding” and “I feel that the PC is the right direction for the provision to be headed”.
Conclusion: Nepalese undergraduate pharmacy students had positive attitudes toward PC. Exercising proper pharmacy practice regulations and educational efforts to overcome the perceived barriers may lead to better delivery of PC.
Keywords: pharmacy practice internship, pharmaceutical care, undergraduate pharmacy student, Nepal
Introduction
Background and rationale
Over recent years, the role of pharmacists has expanded from traditional product-oriented dispensing to patient-focused pharmaceutical care (PC) practice. Pharmacists are now working collaboratively with other health professionals as an integral part of the health-care team to provide optimized patient care services in hospitals and various clinical settings.1,2 PC used to be considered as “the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life”.3 More recently, the Pharmaceutical Care Network Europe promulgated the definition of PC as “the pharmacist’s contribution to care of individuals in order to optimize medicines use and improve health outcomes”.4 Studies have revealed that involvement of pharmacists towards PC services resulted in significant positive outcomes in the identification and prevention of drug therapy and disease-related problems, particularly in diabetes,5 heart failure,6 asthma,7 hypertension,8 breast and ovarian cancer,9 cardiovascular diseases,10 asthma and chronic obstructive pulmonary diseases.11 Moreover, studies have shown positive attitudes of students towards PC in several countries including Qatar,12 Ethiopia,13 Saudi Arabia,14 Nigeria,15 and Pakistan.16 These studies have identified several major barriers in achieving PC such as inadequate drug information sources, lack of access to patient information and workplace for counseling, time constraint, insufficient professional skills, poor image of the pharmacist and economic incentive.12,13,15
In Nepal, pharmacy education started formally four decades back in the Institute of Medicine, Tribhuvan University.17 Currently, four Universities (Pokhara, Purbanchal, Kathmandu and Tribhuvan) are running four-year undergraduate courses18–21 while 40 colleges have a certificate level course (three-year diploma in pharmacy) under the Council for Technical Education and Vocational Training.22 Each year approximately 400–500 new pharmacists are registered in Nepal Pharmacy Council (NPC). The NPC is an official body to regulate pharmacy education in Nepal.23 Under its responsibility for setting up pharmacy practice standards, it has drafted National Good Pharmacy Practice (NGPP) guidelines which highlight the need for qualified and skilled manpower, proper facilities and several other requirements for the provision of better PC services in Nepal. However, Nepalese pharmacists are still struggling to translate PC into clinical practice probably due to the knowledge-practice gap,24 poor implementation of NGPP guidelines, absence of well-established training centers,25,26 lack of implementation of guidelines about career pathway,27 lack of professional development facilities, lack of skilled manpower,24 fewer trained pharmacists,28 and poor implementation of available hospital pharmacy guidelines.29
Nevertheless, the undergraduate pharmacy curriculum of all the Universities of Nepal incorporates some relevant topics of PC which act as a foundation for futuristic PC careers. These topics include medication history taking, patient counseling, reporting adverse drug reactions (ADRs), procedure for checking a prescription, record keeping, etc. However, poor allocation of the credit hours for the PC contents makes it obvious that students lack theoretical knowledge of PC before they attend academic internship during their final semester or final year. In addition to this, the two to four weeks duration of the academic internship in hospital and community pharmacy18–21 is rather short and the dearth of guidelines for their supervision makes it more challenging. In their study Katoue et al suggested that the knowledge of pharmacy students’ attitudes and perceived barriers may serve as an important guide to curricular change and improvement.30 Therefore, we assessed the attitudes and perceived barriers of final year pharmacy undergraduates of Nepal towards the provision of PC.
Methodology
Study design, setting and participants
A cross-sectional descriptive study was conducted among 232 undergraduate final semester/year pharmacy students of Nepal who had completed a mandatory academic internship in hospital or a community pharmacy (response rate: 92.8%) during July and August 2016. Students who refused to participate and absentees at the time of data collection were excluded. These participants were enrolled from 13 out of 19 undergraduate pharmacy colleges of Nepal. Six colleges which had started their program recently had no final year students and were thus excluded. The four-year undergraduate pharmacy program in the semester system is operated by colleges affiliated with Pokhara, Purbanchal, and Kathmandu Universities, whereas all the colleges under Tribhuvan University operate a yearly system.
Data collection tool
A self-administered modified 13-item standard pharmaceutical care attitudes survey (PCAS) questionnaire, originally developed and validated in the US,31 and applied in earlier studies in various settings (Qatar, Ethiopia, Saudi Arabia, Nigeria, Pakistan and US)12–16,32 was used after pretesting among 20 students of Valley College of Technical Sciences, Kathmandu (Cronbach’s α=0.765), which led to the estimated power of 64%.33 This tool is a five-point Likert scale (1=strongly disagree to 5=strongly agree) consisting of three constructs: professional benefit, professional duty, and return on effort. In the construct “return to effort” the scoring was reversed since the wording of the sentence was negative (5=strongly disagree to 1=strongly agree). The maximum possible score in the entire construct was 15. Hence, the score of 15 would be considered the maximum score for a positive attitude in the first two constructs while the same would be considered maximum score for a negative attitude.
Data on demographic details (age, gender, ethnicity and marital status) based on Nepal Demographic and Health Survey 2006,34 educational determinants (previous incomplete grade, attendance to educational training, type of certificate/intermediate education, and the source of motivation for the study), job type at the time of the study and the interest of the students for future career were collected to gather knowledge on exact pharmaceutical scenario of Nepal.
Professional benefit construct included the summation of scores for eight items: pharmacy students can perform PC during their clerkships; I think the practice of PC is valuable; I would like to perform PC as a pharmacist practitioner; providing PC is professionally rewarding; I feel that PC is the right direction for the provision to be headed; I feel that the PC movement will benefit pharmacists; I feel that the PC movement will improve patient health and; I feel that practicing PC would benefit my professional career as a pharmacy practitioner.
Professional duty was a cumulative score of three items: all pharmacists should perform PC; pharmacists in all healthcare settings primary responsibility should be to prevent and solve medication-related problems; pharmacist’s primary responsibility should be to practice PC.
Similarly, the return on effort included a total score of two items: providing PC takes too much time, and effort, and providing PC is not worth the additional workload that it places on the pharmacist. The item numbers six and 13 in the PCAS tool were reverse scored to account for the negatively worded question.
We used 12-item questionnaires to identify the perceived barriers for Nepalese students to provide PC to patients. This tool was also pretested together with the PCAS questionnaire. Among the 12 items, 10 were adopted from the previous studies12,13 and the remaining two were added by the investigators being deemed relevant within the country context after consultation with experts. The barriers included: inadequate drug information resources in the pharmacy, lack of access to the patient medical record in the pharmacy, lack of therapeutics knowledge, lack of understanding of PC, inadequate training in PC, lack of workplace for counseling in the pharmacy, inadequate technology in the pharmacy, lack of self-confidence, time constraints, poor image of pharmacist’s role in society, very limited opportunity in government and private hospitals, and inadequate (hospital and community pharmacy) internship period.
Sample size and sampling technique
There were a total of 13 undergraduate pharmacy colleges in Nepal running four years of undergraduate pharmacy course exclusive of those not having final year/semester students during the study period. The total number of students in the final year/semester from all these colleges was 480. Hence, considering 95% CI and 5% margin of error, a sample size of 219 was determined. The sampling was performed using clustered random sampling technique. Each college was considered as a cluster and the required sample from each of the colleges was taken through simple random sampling.
Ethical consideration
The ethical approval for this study was obtained from the Institutional Review Committee of Chitwan Medical College, Nepal dated 15 July 2016 (Ref No: CMC-IRC-2072/073-105). Our study adhered to the principles outlined in the Declaration of Helsinki.35 Furthermore, the study was conducted only after the approval from the head of each college that participated in this study. Additionally, written consent was also obtained from all the eligible students prior to their participation in the study.
Data analysis
Data were entered in Epi-Data 3.1 (The EpiData Association, Odense, Denmark)_. Results were reported as frequency and percentage for categorical variables, median and IQR for numerical variables and both for Likert items. The normal distribution of the numeric variables was confirmed using Shapiro–Wilk test (P>0.05). Median differences between groups were evaluated using Mann–Whitney U test or Kruskal–Wallis test where appropriate. Statistical analyses were performed in IBM SPSS 22.0 (Statistical Package for Social Sciences version 22.0) for Windows (IBM Corporation, Armonk, NY, USA). Spearman’s rho test was used to measure the strength of correlation between two variables (r = +1 for perfect positive correlation and r = −1 for perfect negative correlation). For all the statistical tests, two-tailed P<0.05 were considered statistically significant.
Results
A total of 232 students were included in the analysis who met the eligibility criteria. The number of participants from the 13 included undergraduate colleges affiliated with four universities are illustrated in Table 1. Nearly one-third of the participants (34.5%) were from Pokhara University whereas the lowest number were from Kathmandu University (12.1%).
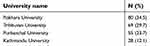 | Table 1 Number of participants from different universities |
Sociodemographic characteristics of the students
The sociodemographic characteristics of the participants are described in Table 2. The mean age of the students was 24 years and ranged between 20 and 31 years. There were more male students (53.4%), the majority were unmarried (90.5%) and had completed 10+2 or intermediate in science (equivalent to high school with science major) (58.6%) before commencing the undergraduate pharmacy education. The majority of the students undertook current pharmacy education because they were self-motivated (76.7%) and were not employed in any pharmacy related job at the time of the study such as community pharmacy (34.4%), hospital pharmacy (29.7%) and the pharmaceutical industry (20.3%). Notably, three-quarters of the students (76.3%) had no previous incomplete grades that could delay their graduation. Nearly 9 out of 10 students (87.1%) had attended pharmacy practice related seminars, symposiums, and workshops, other than those required by their undergraduate syllabus. A high proportion of students expressed their postgraduation career interest in the field of the pharmaceutical industry (33.6%) followed by hospital pharmacy (30.6%).
 | Table 2 Sociodemographic characteristics of the students (N=232) |
Students’ attitudes towards pharmaceutical care
The response of participants in each item of PCAS is summarized in Table 3. More than 80% of the students agreed or strongly agreed that PC practice is the primary responsibility of the pharmacists (83.1%) and it should be practiced by all pharmacists (88.8%). Nearly all the students agreed or strongly agreed that the practice of PC is valuable (94.8%) and primary responsibility of pharmacists in health-care setting should be to prevent and solve medication-related problems (94%). The majority of the students expressed their interest in performing PC as a pharmacist practitioner (87.1%) and considered it to be professionally rewarding (84.9%) or beneficial to their professional pharmacy career as a pharmacy practitioner (90.1%). About three-quarters of the students agreed or strongly agreed that pharmacy students could perform PC during their clerkship or internship. Almost half of the students thought that providing PC takes too much time and effort (45.7%) and it is not worth the additional workload that it places on the pharmacist (51.7%). A total of 87.5% of the students felt that PC is the right direction for the provision to be headed. Further, 92.6% of the students agreed that PC movement would benefit pharmacists and 94% believed that PC improves patient health.
 | Table 3 Students’ attitudes towards pharmaceutical care in PCAS item (N=232) |
Students’ attitudes toward pharmaceutical care per PCAS scale
Students’ attitudes toward PC per PCAS scale on some demographic variables are expressed in Table 4. The median (IQR) score for professional duty, return on effort, and professional benefit were 14.0 (5.0), 5.0 (2.0), and 5.0 (3.0) respectively. There was a statistically significant difference in the median score of return on effort on the age (P=0.009) but not on gender, education in certificate/intermediate level, marital status and involvement in any pharmacy related job (Mann–Whitney U-test). Moreover, the difference in median score of professional duty and professional benefit on age, gender, education in certificate/intermediate level, marital status and involvement in any pharmacy related job was not significant (Mann–Whitney U-test).
 | Table 4 Students’ attitudes towards pharmaceutical care per PCAS scale |
Students’ perceived barriers to pharmaceutical care
The potential barriers to PC provision as perceived by the students are depicted in Table 5. Inadequate training in PC (75.9%), inadequate drug information resources in the pharmacy (73.3%), lack of access to the patient medical record in the pharmacy (71.1%) and lack of limited workspace in government and private hospitals (69.3%) were perceived as the main barriers to PC provision by most of the students.
 | Table 5 Students’ perceived barriers for pharmaceutical care provision (N=232) |
Relationship between students' attitudes towards pharmaceutical care and their qualitative characteristics
We observed a statistically significant relationship between positive attitudes towards PC and three factors, namely source of motivation, current employment in pharmacy related job and incomplete grades delaying graduation (Table 6). Various sources of motivation had a statistically significant difference in the median score of students thinking that the practice of PC is valuable at P=0.048 (Kruskal–Wallis test). The highest scores [(median (IQR)] was observed in those who were forced by family and those influenced by friends or seniors [(both 2.0 ([1.0)]), followed by self-motivationl and others with score 1.0 (1.0) in both the cases. Similarly, there was also statistically significant difference in the median score in the positive attitude towards PC (I feel that the PC is the provision to be headed; P=0.046 (Mann –Whitney U-test) and current employment). However, both employed and unemployed students had similar median (IQR) score of 2.0 (1.0). Interestingly, previous incomplete grades that may cause a delay in graduation was also related with two questions of positive attitudes namely “Providing PC is professionally rewarding” and “I feel that PC movement will improve patient health” at P=0.021 and P=0.030 respectively (Mann–Whitney U-test). The result showed that those who had complete and incomplete grades had similar median (IQR) score that is 2.0 (1.0) for the earlier question and 1.0 (1.0) for the latter.
 | Table 6 Relationship between student attitude towards pharmaceutical care and their qualitative characteristics. |
Correlation between students' attitudes towards pharmaceutical care and age
Table 7 depicts that age was significantly but negatively correlated with the scores of three questions of positive attitudes namely “I would like to perform PC as a pharmacist practitioner”, “Providing PC is professionally rewarding” and “I feel that the PC is the right direction for the provision to be headed” at P=0.004 (r=−0.190), P=0.044 (r=−0.133) and P=0.003 (r=−0.193) respectively. However, the correlation coefficient signifies a negligible correlation.
 | Table 7 Correlation between student attitude towards pharmaceutical care and age |
Discussion
This is a first nationwide multi-institutional survey to assess the undergraduate pharmacy students’ attitudes and perceived barriers towards the provision of PC in Nepal. The majority of the students were found to be self-motivated to undertake pharmacy education and had no previous incomplete grades. Furthermore, they were regularly attending pharmacy related seminars, symposiums and workshops, keeping themselves well informed about the current scene and career prospects regarding the pharmaceutical sector. All these components may serve as a basis for better understanding of PC. Their exhibition of interest to start a professional career after graduation in the pharmaceutical industry followed by the hospital pharmacy and pharmaceutical marketing reflects the current scenario of job opportunities and preference in Nepal for graduate pharmacists. The availability of more than 50 well-established pharmaceutical industries in Nepal might have influenced the career preference of graduate pharmacists more towards the industrial sector.36 Nevertheless, the scope of pharmacists in hospital pharmacy settings in Nepal is in its emerging phase,26,37,38 making it a secondary preference for graduates in our study. An initiative was taken by the Government of Nepal in 2015, where they passed the Hospital Pharmacy Service Directive stating that every hospital should have its own pharmacy with functional pharmacy and therapeutics committee along with the presence of at least one pharmacist in 26–50-bedd hospitals; one clinical pharmacist and two pharmacists in 51–100-bedd hospitals.29 We forecast that this effort will create a platform in developing a concrete career foundation for pharmacists in the hospital pharmacy settings in upcoming years. Pharmacists may work in various job placement sites within hospital pharmacies like medication counseling center, drug information center, pharmacovigilance and drug dispensing.
Our results revealed that undergraduate pharmacy students who performed academic internship had positive attitudes towards PC. This finding is consistent with the studies conducted in Qatar, Ethiopia, Nigeria, Pakistan, and Kuwait.12,13,15,16,30 Furthermore, a study conducted in Nepal has shown that even a short duration of community pharmacy internship (2 weeks) during which students received training on various aspects of pharmacy practice including medicine storage, inventory management, handling of damaged and expired drugs, responding to symptoms of patients, medication counseling, reporting ADRs to regional pharmacovigilance center, drug information services, etc played a significant role for students to acquire good knowledge in community pharmacy practice standards.39 Knowledge obtained from academic internship helps students apply their theoretical knowledge into practical settings to obtain effective patient care. The ultimate goal of training pharmacy students about the PC plan is to increase knowledge and competencies to prepare them for future employment. It is expected that students will gain in-depth knowledge about pharmacy operation in the community and hospital pharmacies, customer service, dispensing and counselling, understand patients medical profiles, product knowledge including side effects and ADRs, ordering and stock control, multidisciplinary work collaboration and ethical practices. These transferrable skills are linked with providing individual care, optimization of therapy and improving health outcomes. A recent systematic review from Nepal reported that a clinical pharmacy service reduced direct health-care costs, unnecessary use of medications, prescription errors, and improvement in drug utilization pattern and patients’ satisfaction.40 However, this review is subjected to a major limitation of sample size, short follow-up time, inadequate randomization and lack of control groups. There is still room for improvement in training pharmacy students to achieve appropriate clinical outcomes in the near future, perhaps evidence gathered from high-quality studies would further rectify it.
Evidence suggests that the majority of community pharmacies in Nepal are currently being operated by unqualified pharmacists who have acquired basic training in pharmacology and medication dispensing.24,41 This current scenario has been a major constraint for students to acquire knowledge on PC through internship in pharmacies of Nepal. Hence, though challenging, there is an urgent need to improve the current status of PC services provided by pharmacies operating in Nepal which primarily demands an immediate replacement of the unqualified pharmacists by registered pharmacists.
In our study, we observed a statistically significant difference (P=0.009) in the median score of return to effort between those over 25 years and those less or equal to 25 years. This signifies that younger students had positive attitude about the return to effort aspect of PC. Though in-depth analysis of age with the PCAS tool was beyond the scope of our research, upon examination it was found that a higher percentage of individuals over 25 years had job related to the pharmacy while younger students did not perceive time constraints as a barrier for the PC provision. The former was statistically significant, however, not for the latter. A study in Nigeria indicated that age did not have a significant influence on attitude towards PC,42 but they did not specify the score of a component of PC rather an overall score. Interestingly, a study in Saudi Arabia found that younger participants have a more positive attitude towards PC.14 Nonetheless, the impact of age on the attitude towards PC, particularly return to effort, might be worth considering in future studies.
The major perceived barrier for PC was inadequate training in PC. Nepal lacks an adequate focus on pharmacy practice in the current curriculum of the universities,18–21 and adequate training of pharmacists in non-communicable disease prevention and management,43 which might have contributed as a barrier to PC. The need for modification of the degree requirements and harmonization in thecurriculum of all the universities for the purpose of producing graduates capable of delivering PC, in service training of students in hospital and community pharmacy, development of model pharmacy practice site has already been addressed in the workshop comprising of experienced pharmacy professionals.44 Students participating in trainingare seldom given chance to perform appropriate pharmacy practice and they are perceived as a burden by the preceptors and administrators, rather than as a member for health-care contribution. Some of the training programs have shown remarkable contribution to improving pharmacy practice skills among the students.39 Furthermore, students have also reflected their will in participating in the workshops and training related to the pharmacy practice.45 Rovers et al revealed that students who used a guided interview process while interviewing patients were more likely to identify drug therapy problems.46 A study from Ethiopia also demonstrated a greater positive attitude toward PC for participants having more practical experience.13 Therefore, appropriate measures should be initiated for the implementation of sufficient training as a part of pharmacy practice course by all the universities of Nepal. A training parallel with theoretical education is suggestive. Training approach should focus towards the patient care and the regulatory authority should ensure they construct a framework to support the development of experimental training models. Well-designed researchshould be conducted to evaluate the impact of training on PC once the pharmacy students graduate as a part of outcome measurement.
We found inadequate drug information resources in the pharmacy as another perceived barrier for PC which is inconsistent with the study conducted among the pharmacy students in Qatar.12 Nepal suffers from lack of adequate drug information sources due to lack of availability of current literature, underprivileged documentation, unavailability of sufficient funds, substantial unavailability of trained manpower and pinched dissemination of little available information.47 Undertaking an approach toward providing the pharmacists with access to drug information resources by any means will serve them as a guide to exercise the provision of PC. Another perceived barrier to PC was lack of access to the patient medical records in the pharmacy. A previous finding reported that community pharmacies operating worldwide face the inability to obtain clinical and laboratory data of the patients as one of the barriers to PC provision.48 Moreover, findings support that pharmacists' access to medical records helps in identification of the medication-related problems49 and better patient care.50 PC is a multidisciplinary approach which delivers proper pharmaceutical services by means of taking patient history, compilation of laboratory data, and reviewing patients’ medical records to identify, prevent, and resolve drug therapy problems.51 In the context of Nepal, the provision for availability of patient medical records are limited in certain hospitals and clinics but not in the community pharmacies. Extension of its availability in such pharmacies as a part of PC services would directly benefit the patients.
Our results also revealed the lack of workspace for counseling in the pharmacy as another perceived barrier for PC. Previous studies on hospital pharmacy services in Nepal have demonstrated inadequate design of hospital pharmacies and unavailability of the provision of patient counseling.26,38 This is a pertinent problem which must be addressed as soon as possible both at policy level and at implementation level. Hospital pharmacists have a leading role to provide access to essential medicines52 which is a cornerstone of Universal Health Coverage (UHC).53 Hence, it is essential for pharmacy students to receive training on all the possible aspects of PC more appropriately in order to become a skilled future pharmacist for Nepal. Our study being a nationwide multi-institutional survey, the implication may be broadened to other developing countries where the pharmacy practice is still in infancy.
Conclusion
Nepalese undergraduate pharmacy students have an overall positive attitude towards pharmaceutical care. However, they identified inadequate pharmaceutical care training, insufficient drug information resources in pharmacies, lack of patient medication records in pharmacies and limited workspace in government and private hospitals as major barriers to pharmaceutical care practice. Strategies to overcome these barriers are necessary for the better delivery of pharmaceutical care services in the country.
Strength and limitations
The first and a major strength of this study is that it is the first study conducted in Nepal to assess the undergraduate pharmacy students’ attitudes and perceived barriers toward PC using the PCAS tool. Second, our study has gathered information on demographic details (age, gender, ethnicity, and marital status), educational determinants (previous incomplete grade, attendance to educational training, type of certificate/intermediate education, the reason for studying, and source of the motivation for the study), job type at the time of the study and interest of the student for a future career. The third strength is that our study is the first to measure whether the limited opportunities to work in government and private hospitals and inadequate internship duration (in hospital and community pharmacy) are the barriers for PC.
The major limitation of this study is that it was conducted in only one cohort of final year undergraduate students in Nepal and may not be generalized to other Asian countries or similar settings. Moreover, the outcome may depend on knowledge and extent of pharmacy practice training and education the students received during their study and internship period. The variation of the participants from different universities was due to the different calendar year of the universities. The PCAS tool has been validated using Cronbach’s alpha test, the contents on the local setting remains to be validated.
Recommendations for practice and policy
There is an urgent need to overcome the major barriers to achieve the better practice of PC in Nepal. There should be enough drug information resources in the pharmacy, and pharmacists need access to patient medical records for better understanding of the individual needs. The existing short academic internship period should be extended up to one year to meet international standards. Completion of an internship alone does not ensure the quality of the PC skills that the pharmacy students will learn, but, a well-organized PC practice and training system offered by a hosting institute will have a major impact. The changes might not be immediately visible but a responsibility to establish standard training program for future lies in the hands of academia, policymakers and pharmacy practitioners. The standard training program should then be implemented nationally as a consensus approach by all the universities as an internship model for undergraduate pharmacy students to produce competent graduates. Some changes in the current curriculum to increase the contents about PC may be useful. Designing a pre/post study (ie before and after internship) may help to evaluate the impact of the internship and it should be a future research area.
Ethics approval and consent to participate
All aspects of the work covered in this manuscript has been conducted with the ethical approval and consent of all relevant bodies and that such approvals are acknowledged within the manuscript.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We would like to kindly acknowledge outstanding cooperation from all the coordinators of participated colleges for the data collection. Funds for the conduct of this research were generated by the authors themselves.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bradley CP. The future role of pharmacists in primary care. Br J Gen Pract. 2009;59(569):891–892. doi:10.3399/bjgp09X473105
2. Toklu HZ, Hussain A. The changing face of pharmacy practice and the need for a new model of pharmacy education. J Young Pharm. 2013;5(2):38–40. doi:10.1016/j.jyp.2012.09.001
3. Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–543.
4. Allemann SS, van Mil JF, Botermann L, Berger K, Griese N, Hersberger KE. Pharmaceutical care: the PCNE definition 2013. Int J Clin Pharm. 2014;36(3):544–555. doi:10.1007/s11096-014-9933-x
5. Shao H, Chen G, Zhu C, et al. Effect of pharmaceutical care on clinical outcomes of outpatients with type 2 diabetes mellitus. Patient Prefer Adherence. 2017;11:897–903. doi:10.2147/PPA.S92533
6. Parajuli DR, Franzon J, McKinnon RA, Shakib S, Clark RA. Role of the pharmacist for improving self-care and outcomes in heart failure. Curr Heart Fail Rep. 2017;14(2):78–86. doi:10.1007/s11897-017-0323-2
7. Shanmugam S, Varughese J, Nair MAS, et al. Pharmaceutical care for asthma patients: a developing country’s experience. J Res Pharm Pract. 2012;1(2):66–71. doi:10.4103/2279-042X.108373
8. Cazarim Mde S, de Freitas O, Penaforte TR, Achcar A, Pereira LR. Impact assessment of pharmaceutical care in the management of hypertension and coronary risk factors after discharge. PLoS One. 2016;11(6):e0155204. doi:10.1371/journal.pone.0155204
9. Liekweg A, Westfeld M, Braun M, et al. Pharmaceutical care for patients with breast and ovarian cancer. Support Care Cancer. 2012;20(11):2669–2677. doi:10.1007/s00520-012-1385-z
10. Babar ZU, Kousar R, Murtaza G, Azhar S, Khan SA, Curley L. Randomized controlled trials covering pharmaceutical care and medicines management: a systematic review of literature. Res Social Adm Pharm. 2018;14(6):521–539. doi:10.1016/j.sapharm.2017.06.008
11. Poudel RS, Piryani RM, Shrestha S, Prajapati A. Benefit of hospital pharmacy intervention on the current status of dry powder inhaler technique in patients with asthma and COPD: a study from the Central Development Region, Nepal. Integr Pharm Res Pract. 2016;6:7–13. doi:10.2147/IPRP.S119202
12. El Hajj MS, Hammad AS, Afifi HM. Pharmacy students’ attitudes toward pharmaceutical care in Qatar. Ther Clin Risk Manag. 2014;10:121–129. doi:10.2147/TCRM.S56982
13. Tsega B, Bhagavathula AS, Sarkar BR, Melaku T, Shewamene Z. Impact of clerkship attachments on students’ attitude toward pharmaceutical care in Ethiopia. Adv Med Edu Pract. 2015;6:385–391. doi:10.2147/AMEP.S80802
14. Al-Arifi MN. Pharmacy students’ attitudes toward pharmaceutical care in Riyadh region Saudi Arabia. Pharm World Sci. 2009;31(6):677–681. doi:10.1007/s11096-009-9331-y
15. Udeogaranya PO, Ukwe CV, Ekwunife OI. Assessment of attitudes of University of Nigeria pharmacy students toward pharmaceutical care. Pharm Pract (Granada). 2009;7(3):145–149.
16. Rahim N, Nesar S. Pharmacy undergraduate students’ attitude toward pharmaceutical care in Pakistan. Int J Pharm Pharm Sci. 2012;4(4):113–116.
17. Bhuvan KC, Palaian S, Mohamed Izham MI. PharmD education in nepal: the challenges ahead. Am J Pharm Educ. 2011;75(2):38c. doi:10.5688/ajpe75238c
18. Pokhara University, Pokhara, Nepal [Curriculum Structure of Science Programs, B.pharm, Bachelor programs]. Available from: http://pu.edu.np/edu/science-curriculum/. Accessed July 10, 2018.
19. Purbanchal University, Biratnagar, Nepal [Academic programs]. Available from: http://purbuniv.edu.np/Program/?Id=5&Level=2. Accessed July 10, 2018.
20. Kathmandu University, Kathmandu, Nepal [Department of Pharmacy-Programs]. Available from: http://www.ku.edu.np/pharmacy/index.php?go=program. Accessed July 10, 2018.
21. Tribhuvan University, [Institute of Medicine-Constituent Campuses]. Available from: https://tribhuvan-university.edu.np/institutes/institute-of-medicine. Accessed July 10, 2018.
22.
23. Nepal Pharmacy Council. Available from: http://nepalpharmacycouncil.org.np/index.php?link=fees.php. Accessed July 15, 2018.
24. Ansari M. Evaluation of community pharmacies regarding dispensing practices of antibiotics in two districts of central Nepal. PLoS One. 2017;12(9):e0183907. doi:10.1371/journal.pone.0183907
25. Poudel BK, Ishii I. Assessment of physical premises of selected pharmacies of Nepal. SAGE Open Med. 2016;4:2050312116654590. doi:10.1177/2050312116654590
26. Shankar PR, Palaian S, Thapa HS, Ansari M, Regmi B. Hospital pharmacy services in teaching hospitals in Nepal: challenges and the way forward. Arch Med Health Sci. 2016;4(2):212–217. doi:10.4103/2321-4848.196212
27. Ranjit E. Pharmacy Practice in Nepal. Can J Hosp Pharm. 2016;69(6):493–500.
28. Ansari M, Alam K. Chapter 8 - Pharmacy Practice in Nepal. In: Fathelrahman AI, Ibrahim MIM, Wertheimer AI, editors. Pharmacy Practice in Developing Countries. Boston: Academic Press; 2016:147–168.
29. Directives and Guidance: government of Nepal, Department of Drug Administration; [Hospital Pharmacy Guideline 2018]. Available from: http://www.dda.gov.np/content/hospital-pharmacy-guideline-2072. Accessed December 10, 2018.
30. Katoue MG, Awad AI, Schwinghammer TL, Kombian SB. Pharmaceutical care education in Kuwait: pharmacy students’ perspectives. Pharm Pract (Granada). 2014;12(3):411. doi:10.4321/S1886-36552014000300002
31. Martin BC, Chisholm MA. Cross-validation of an instrument measuring students attitudes toward pharmaceutical care. Am J Pharm Educ. 1999;63(1):46.
32. Chisholm MA, Wade WE. Factors influencing students‘ attitudes toward pharmaceutical care. Am J Health Syst Pharm. 1999;56(22):2330–2335. doi:10.1093/ajhp/56.22.2330
33. Perneger TV, Courvoisier DS, Hudelson PM, Gayet-Ageron A. Sample size for pre-tests of questionnaires. Qual Life Res. 2015;24(1):147–151. doi:10.1007/s11136-014-0752-2
34. Bennett L, Dahal DR, Govindasamy P. Caste, Ethnic and Regional Identity in Nepal: Further Analysis of the 2006 Nepal Demographic and Health Survey. Maryland, USA: Macro International Inc; 2008.
35. Wilson CB. An updated Declaration of Helsinki will provide more protection. Nat Med. 2013;19(6):664. doi:10.1038/nm0613-664
36.
37. Poudel RS, Prajapati A. Hospital pharmacy profession in Nepal through the eye of a pharmacist. J Chitwan Med Coll. 2016;6(2):56–57. doi:10.3126/jcmc.v6i2.16691
38. Thapa S, Palaian S, Ibrahim MIM. Establishing a Hospital Pharmacy in Nepal: experiences and challenges. J Pharm Pract Commun Med. 2017;3(1):31–33. doi:10.5530/jppcm
39. Timsina S, Bhuvan KC, Adhikari D, Alrasheedy AA, Mohamed Ibrahim MI, Kaundinnyayana A. A new experimental community pharmacy internship module for undergraduate pharmacy students in western Nepal: overview and reflections. J Educ Eval Health Prof. 2017;14:18. doi:10.3352/jeehp.2017.14.18
40. Mikrani R, Naveed M, Mikrani A, Yasmeen S, Akabar M, Xiaohui Z. The impact of clinical pharmacy services in Nepal in the context of current health policy: a systematic review. J Public Health (Bangkok). 2019. doi:10.1007/s10389-019-01042-y
41. Bhuvan KC, Alrasheedy AA, Ibrahim MI. Do community pharmacists in Nepal have a role in adverse drug reaction reporting systems? Australas Med J. 2013;6(2):100–103. doi:10.4066/AMJ.2013.1544
42. Oparah AC, Eferakeya AE. Attitudes of Nigerian pharmacists towards pharmaceutical care. Pharm World Sci. 2005;27(3):208–214. doi:10.1007/s11096-004-2268-2
43. Khanal S, Nissen L, Veerman L, Hollingworth S. Pharmacy workforce to prevent and manage non-communicable diseases in developing nations: the case of Nepal. Res Social Adm Pharm. 2016;12(4):655–659. doi:10.1016/j.sapharm.2015.09.005
44.
45. Palaian S, Khanal S. Pharmacy students feed back on hospital and clinical pharmacy workshop: a study from Nepal. Self. 2008;24:88–89.
46. Rovers J, Miller MJ, Koenigsfeld C, Haack S, Hegge K, McCleeary E. A guided interview process to improve student pharmacists’ identification of drug therapy problems. Am J Pharm Educ. 2011;75(1):16. doi:10.5688/ajpe75116
47. Chhetri AK, Palaian S, Mishra P. Drug information services in Nepal: the changing perspectives. Kathmandu Univ Med J. 2008;6(21):117–121.
48. Farris KB, Fernandez-Llimos F, Benrimoj SI. Pharmaceutical care in community pharmacies: practice and research from around the world. Ann Pharmacother. 2005;39(9):1539–1541. doi:10.1345/aph.1G049
49. Gernant SA, Zillich AJ, Snyder ME. Access to medical records’ impact on community pharmacist-delivered medication therapy management: a pilot from the medication safety research network of Indiana (Rx-SafeNet). J Pharm Pract. 2017;31:1–9.
50. Warholak-Juarez T, Rupp MT, Salazar TA, Foster S. Effect of patient information on the quality of pharmacists’ drug use review decisions. J Am Pharm Assoc. 2000;40(4):500–508.
51. Schommer JC, Cable GL. Current status of pharmaceutical care practice: strategies for education. Am J Pharm Educ. 1996;60:36–42.
52. Duong MH, Moles RJ, Chaar B, Chen TF. Stakeholder roles in facilitating access to essential medicines. Res Social Adm Pharm. 2019;15(3):260–266. doi:10.1016/j.sapharm.2018.04.034
53. Bigdeli M, Laing R, Tomson G, Babar Z-U-D. Medicines and universal health coverage: challenges and opportunities. J Pharm Policy Prac. 2015;8(1):8. doi:10.1186/s40545-015-0028-4
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
