Back to Journals » Clinical Ophthalmology » Volume 17
Ultra-Widefield Imaging as a Teleophthalmology Screening Tool for Ocular Pathology
Authors Ahmad TR , Situ WA, Chan NT, Keenan JD, Stewart JM
Received 4 August 2023
Accepted for publication 9 October 2023
Published 30 October 2023 Volume 2023:17 Pages 3225—3234
DOI https://doi.org/10.2147/OPTH.S433864
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tessnim R Ahmad,1 Winnie A Situ,2 Nicholas T Chan,2 Jeremy D Keenan,1,3 Jay M Stewart1,2
1Department of Ophthalmology, University of California, San Francisco, CA, USA; 2Department of Ophthalmology, Zuckerberg San Francisco General Hospital and Trauma Center, San Francisco, CA, USA; 3Francis I. Proctor Foundation, University of California, San Francisco, CA, USA
Correspondence: Jay M Stewart, University of California, Department of Ophthalmology, 490 Illinois Street, Floor 5, San Francisco, CA, 94143-4081, USA, Tel +1 (628) 206-3123, Email [email protected]
Background: Prior studies have validated ultra-widefield imaging as a remote screening tool for diabetic retinopathy. The aim of this study was to determine its use in screening for any fundus pathology in a routine patient population.
Methods: In this prospective randomized study, patients underwent both slit lamp indirect ophthalmoscopy and ultra-widefield imaging. Ultra-widefield images were independently reviewed by two optometrists, and discrepancies were adjudicated by a retina specialist. Clinical findings from slit-lamp examiners and image-reviewers were coded into themes and clinically meaningful findings were extracted. Cohen’s kappa was used to estimate agreement for these findings between the two image-reviewers and between the image-reviewers and slit-lamp examiners.
Results: Nine-hundred eyes of 450 patients were examined and imaged, of which 616 eyes were analyzed. At least one abnormal fundus finding was present on ophthalmoscopy in 71 eyes (11%) and on adjudicated image interpretation in 166 eyes (27%). Agreement between the two image-reviewers was moderate to substantial for most clinically meaningful findings, including optic disc hemorrhage (κ = 0.8), macular exudates (κ = 0.7), and macular pigmentary changes (κ = 0.7). Agreement between examiners and image-reviewers was moderate to substantial for optic disc hemorrhage (κ = 1), indistinct optic disc margins (κ = 0.5), drusen (κ = 0.4), pigmentary changes (κ = 0.4), and hemorrhage (κ = 0.8). A total of 187 findings were detected by imaging but not examination, compared with 42 that were detected on examination but not imaging.
Conclusion: In a routine patient population, ultra-widefield imaging agreed with standard-of-care slit-lamp examinations and detected more fundus findings.
Keywords: ultra-widefield imaging, teleophthalmology, screening, telehealth
Introduction
Telemedicine is the application of digital technology for remote healthcare. Most teleophthalmology uses a “store and forward” model in which ocular images are captured and then assessed separately by trained reviewers.1 Teleophthalmology is expanding in the United Kingdom, where the Royal College of Ophthalmologists recommends using virtual clinics to meet the increasing demand for eye care services.2 The National Diabetic Eye Screening Programme increased access to diabetic retinopathy screening in England using community-based retinal photography, reducing the risk of vision loss at a population level.3 Adoption of teleophthalmology has been slower in the United States and is largely limited to centralized healthcare systems such as the Veterans Affairs (VA) Health System.4,5 However, the recent coronavirus disease 2019 (COVID-19) pandemic forced a decline in ophthalmology clinical volume and fueled interest in teleophthalmology.6–8
Traditional fundus photography captures 30 to 45 degrees of retina.9 The introduction of nonmydriatic ultra-widefield imaging techniques, which capture a 100-degree retinal view or greater in a single image, offers the potential to detect an anatomically and clinically broader range of pathology.10,11 Previous studies have shown that ultra-widefield imaging compares well with standard 7-field imaging and slit lamp indirect ophthalmoscopy for the assessment of diabetic retinopathy.12–17 Few studies have explored ultra-widefield imaging for the assessment of other fundus abnormalities.18–20 The primary aim of this study was to determine the reliability of ultra-widefield imaging, compared to slit lamp indirect ophthalmoscopy, for the detection of clinically meaningful fundus pathology in a routine patient population.
Methods
Procedure
In this prospective randomized study, patients without known eye disease were recruited from a Specsavers store in southern England. Specsavers is a British multinational optical retail-chain offering optician services and eye examinations. The Specsavers internal governance committee determined that informed consent could be waived as personally identifiable information was not collected. Participants underwent ultra-widefield imaging and slit lamp biomicroscopic examination. Consistent with standard of care in the United Kingdom, both ultra-widefield imaging and ophthalmoscopy were performed through nondilated pupils unless dilation was indicated during the examination (eg, if a potentially vision-threatening abnormality was detected).21 The order of the eye examined (ie, right versus left) and imaging-ophthalmoscopy sequence were randomized.
In-person ophthalmoscopic examinations were performed by certified optometrists (median clinical experience: 4 years, range: 1–38), referred to as ‘examiners’ in the present study. Examiners documented their examination findings in the Specsavers proprietary electronic medical record, which organizes findings by anatomic category (ie, optic disc, vessels, macula, peripheral retina). Examiners could select standard descriptions of normal findings (eg, normal optic disc margins, healthy rim) or free text abnormal findings.
Graduate optometrists captured ultra-widefield images following a specific protocol using the Clarus™ (CLARUS 500™, Carl Zeiss Meditec AG, Jena, Germany). Clarus captures true color images and a 133-degree field of view per frame. Montaging software combines two or more ultra-widefield images into a montage with a wider retinal view. Figure 1 demonstrates a sample montage composed of four ultra-widefield images. Montages were independently interpreted by two optometrists unaffiliated with Specsavers. These optometrists, termed ‘image-reviewers’ for the present study, included a junior optometrist with three years of clinical experience and a senior optometrist with 10 years of clinical experience. Image-reviewers viewed the right and left eyes in sequence but were masked to additional clinical information such as patient history, visual acuity, and anterior segment findings. Image-reviewers viewed the montages online and recorded their findings using a similar form as the examiners. They also assessed the quality of the montages using the published grading system outlined below.22
 |
Figure 1 Sample montage composed of four ultra-widefield fundoscopic images. |
Grade 1: excellent definition [of posterior segment structures]
Grade 2: good definition of most details
Grade 3: definition limited but permitting confident assessment
Grade 4: insufficient definition for confident assessment
Grade 5: only gross details or no detail visible
Validated diagnostic classification systems were not utilized as the eyes in this study were routine eyes without preexisting ocular diagnoses. The primary purpose of the study was to determine the presence or absence of fundoscopic pathology, not to stage particular diseases. In addition to the montages, the component ultra-widefield fundus photographs for a random subset of 10% of the montages were also interpreted to determine if the montaging process affected image interpretation. The two to four ultra-widefield images for each eye were presented alone (without the associated montages).
Analysis
Clinical findings from both examiners and image-reviewers were organized by anatomic category and then sorted alphabetically within each category to mask their source (examination versus imaging). A study author (TRA) coded these findings into themes using inductive thematic analysis.23 In this data-driven process, themes emerge from the data rather than a preexisting coding framework. Codes were refined through cycles of immersion (repeated reading of the data) and crystallization (reflecting on the analysis to identify patterns) until a preliminary codebook was developed. Most findings required a single iteration of coding. For example, examiners and image-reviewers provided various descriptions of drusen (eg, few small scattered drusen, small discrete drusen, fine drusen) which were categorized as “drusen.” On the other hand, various peripheral retinal pigmentary changes were initially categorized separately (eg, pigment epithelial changes, pigment hyperplasia, mottling, discoloration) and then combined. The preliminary codebook was reviewed by an ophthalmologist and retina specialist (JMS). A final codebook was developed and used to formally code all responses.
Then, TRA and JK narrowed the examination findings to those that, in clinical practice, would be expected to trigger referral or close monitoring. Discrepancies between image-reviewers for these clinically meaningful findings were adjudicated by an ophthalmologist (JMS) to create a consensus interpretation. The adjudicator was masked to the interpreters’ findings and knew only the anatomic category (eg, optic disc, vessels, macula, peripheral retina) for which the interpretations were discordant.
Cohen’s kappa was used to estimate reliability between reviewers, reliability between the examination and interpretation, and reliability between the interpretations for the montages and individual ultra-widefield images. Then permutation tests were performed to determine if the level of agreement was greater than would be expected by chance (Monte Carlo simulation, N = 1000 replications). Results are reported as kappa coefficients with confidence intervals. Statistical analysis was performed using R version 4 (R Foundation for Statistical Computing, Vienna, Austria).
Results
The study sample consisted of 450 patients (900 eyes) who underwent examination and ultra-widefield imaging in October 2020. Median age was 47 years (range: 8–88 years) and 57% were female. Five patients (1%) required dilation. Four ultra-widefield photographs per eye were taken for the first 201 patients (45%). The protocol was changed to two photographs per eye for the remaining 249 (55%) due to patient and optometrist fatigue. Examination records for four patients (eight eyes) were not available. Montages were created for 362 patients (81%; 616 eyes, 69%). The remainder could not be constructed due to poor image quality. Figure 2 shows the derivation of the final study sample. Of the constructed montages, approximately 90% of images were assessed to have sufficient definition to permit confident assessment (Table 1). Grades 4 and 5 were associated with lens opacities (eg, cataract) on in-person examination (junior OR 2.1, 95% CI 1.2–3.8, P = 0.016; senior OR 2.5, 95% CI 1.4–4.3, P = 0.001).
 |
Table 1 Montage Quality Ratings by Junior and Senior Interpreters |
 |
Figure 2 Flow chart showing derivation of the final study sample. |
A total of 50 codes were derived from the inductive thematic analysis, including 16 pertaining to the optic nerve, 7 to the vessels, 9 to the macula, and 18 to the peripheral retina (Table 2). Of those, 27 were derived from the examination, including 9 optic nerve, 2 vessel, 5 macula, and 11 peripheral retina. Sixteen of these examination codes were designated clinically meaningful, including 4 optic nerve, 2 vessel, 5 macula, and 5 peripheral retina. Figure 3 shows eye-level frequencies of the 16 clinically meaningful fundus findings by examination versus ultra-widefield imaging. At least one abnormal fundus finding was present on ophthalmoscopy in 71 eyes (11%) and on adjudicated image interpretation in 166 eyes (27%).
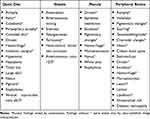 |
Table 2 Final Qualitative Codebook of Fundus Findings by Anatomic Category |
 |
Figure 3 Eye-level frequencies of 16 clinically meaningful fundus findings detected by clinical examination versus ultra-widefield image interpretation. |
Agreement Between Image-Reviewers
Of the clinically meaningful examination findings, inter-image-reviewer agreement was variable (Table 3). In total, the junior reviewer identified 271 abnormalities, compared to 106 by the examiners and 265 by the senior reviewer. Most findings showed moderate to substantial agreement, with the highest agreement for optic disc hemorrhage (κ = 0.8), macular exudates (κ = 0.7), and macular pigmentary changes (κ = 0.7). Of the 616 images judged to have at least one clinically meaningful examination finding by one or both image-reviewers, inter-reviewer discrepancies were observed and adjudicated for 186 images (248 abnormalities). The adjudicated interpretation agreed with the senior reviewer 57% of the time. The adjudicated interpretation was accepted as the consensus interpretation and used for the remaining analyses.
 |
Table 3 Eye-Level Inter-Interpreter Agreement for 16 Clinically Meaningful Fundus Findings |
Examination-Interpretation Agreement
Agreement between the examinations and consensus interpretations is shown in Table 4. There was moderate to substantial agreement for optic disc hemorrhage (κ = 1), indistinct optic disc margins (κ = 0.5), macular drusen (κ = 0.4), peripheral retinal pigmentary changes (κ = 0.4), peripheral retinal drusen (κ = 0.4), and peripheral retinal hemorrhage (κ = 0.8). Lower agreement was observed for optic disc pallor (κ = 0.2), high cup-to-disc ratio (κ = 0.3), vascular abnormalities (κ = 0.1–0.3), and macular pigmentary changes (κ = 0.3). Agreement could not be assessed for macular epiretinal membranes, exudates, and hemorrhages, or for peripheral retinal exudates and lesions because none of the in-person examinations documented these findings. A total of 187 findings were detected by image interpretation but not examination, most commonly an elevated cup-to-disc ratio (n = 31 images), arteriolar attenuation (n = 58), and pigmentary changes (n = 35). In contrast, 42 abnormalities were detected on examination but not image interpretation, with the most common being macular drusen (n = 11 images) and pigmentary changes (n = 10 images).
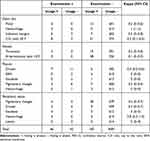 |
Table 4 Eye-Level Agreement for 16 Clinically Meaningful Fundus Findings Between Clinical Examination versus Ultra-Widefield Image Consensus Interpretation |
If the presence of any of the 16 findings was considered a reason for referral, then image review captured most patients who would have been referred based on slit-lamp examination (35 of 47). Besides these patients, image review identified an additional 88 patients for referral. Figure 4 shows the degree of overlap in patient-level referral between examination and image review.
 |
Figure 4 Venn diagrams depicting patient-level agreement for 16 clinically meaningful fundus findings, clinical examination versus ultra-widefield image interpretation. |
To determine whether the montaging process affected the image reviews, both the montages and constituent UWF photographs were interpreted for a random set of 60 eyes. The consensus interpretations of the montages demonstrated substantial agreement with UWF photographs for most findings (Table 5).
 |
Table 5 Eye-Level Agreement Between Montages and Individual Ultra-Widefield Images for 16 Clinically Meaningful Fundus Findings in a Subset of Eyes |
Finally, the 42 findings detected by clinical examination but not image review were re-assessed by the adjudicating ophthalmologist (JMS) to further investigate these false negatives. This re-review confirmed that 42% of findings (n = 14) contained the retinal findings specified by the examiners and were completely missed by the image reviewers. In 21% of cases (n = 7), the image contained the retinal findings specified by the examiners and had those same findings identified by the image-reviewers but in a different anatomic location (eg, examiners documented macular drusen whereas image-reviewers documented peripheral drusen). Finally, 36% of findings (n = 12) did not contain the retinal findings specified by the examiners.
Discussion
The main objective of this study was to determine the reliability of ultra-widefield imaging for the remote detection of clinically meaningful fundus pathology in a routine patient population. All participants underwent standard-of-care ophthalmoscopic examination and ultra-widefield imaging. Images were interpreted by two optometrists with variable clinical experience. There was moderate to substantial reliability between image-reviewers and moderate agreement between imaging and standard-of-care examination, though imaging detected a greater number of fundus pathologies.
The United Kingdom has one of the lowest densities of ophthalmologists among industrialized countries, resulting in care delays and preventable vision loss.24,25 High demand for eye care services has fueled interest in teleophthalmology, where images are captured and then analyzed separately by trained reviewers.2 Until recently, teleophthalmology relied on standard fundus photographs covering 30 to 45 degrees of retina, which could be stitched together.26 Ultra-widefield imaging broadens the field of view three to five times in a single capture through nondilated pupils. The camera used in this study captures true color images and a 133-degree field of view per frame.
Previous studies have compared ultra-widefield imaging to clinical examination for grading diabetic retinopathy severity. A 2014 study of 37 patients with varying degrees of diabetic retinopathy identified almost perfect agreement between two image graders and moderate agreement between ultra-widefield pseudocolor imaging and clinical examination.15 Another study of 51 patients identified a sensitivity of 94% and specificity of 100% for the detection of more than mild diabetic retinopathy, which the authors note fulfills basic telescreening requirements.17 Similarly, ultra-widefield imaging shows high agreement with standard 7-field imaging12,27 but with significantly shorter acquisition times.16 Ultra-widefield imaging has also been studied in combination with optical coherence tomography (OCT) for diabetic retinopathy. A recent study of 51 patients concluded true color imaging plus OCT allowed two-thirds of National Diabetic Eye Screening Programme referrals to be managed virtually. Further, the ultra-widefield images allowed identification of other referrable pathologies such as maculopathy, macular degeneration, and epiretinal membranes.18 A large study of 2,040 eyes of 1,023 patients showed that pseudocolor imaging plus OCT detected more eyes with higher grades of diabetic retinopathy compared with clinical examination alone.14
Few studies have explored the utility of ultra-widefield imaging for non-diabetic patients. A retrospective review of patients with rhegmatogenous retinal detachment who underwent pseudocolor ultra-widefield imaging and examination concluded that ultra-widefield imaging more precisely documented the extent of detachment. However, detection of retinal holes or tears and postoperative scarring was poor, especially in the inferior and superior periphery.19 In another study, 339 eyes of 170 subjects with a known history of ocular findings (eg, glaucoma, drusen, nevi) underwent traditional versus ultra-widefield image-assisted fundus examination. There was high agreement between the two modalities but an advantage for image-assisted examination in cases of disagreement.20
We studied a routine patient population, without known fundus pathology, to determine if ultra-widefield imaging could be used to appropriately identify and triage patients with clinically meaningful findings. We identified moderate to high inter-reviewer reliability for optic disc, macular, and peripheral retinal findings, and slight reliability for vessel abnormalities. There was generally good agreement between imaging and examinations. There was moderate to substantial agreement for most optic disc findings (except pallor and elevated cup-to-disc ratio), macular findings (except pigmentary changes), and peripheral retinal findings. Agreement could not be assessed for some macular and retinal findings (such as epiretinal membranes and exudates) as none of the in-person examinations documented these findings. A sub-analysis of individual ultra-widefield photographs for a subset of montages demonstrated the montaging process did not result in a loss of clinical information or image clarity. Some disagreement is expected, as image interpretation and ophthalmoscopy are inherently subjective and demonstrate both interobserver and intraobserver variability.28,29 Interpreter fatigue and the masked nature of image review may have played a role; image-reviewers interpreted nearly 1000 images without any clinical history. In a real-life setting, optometrists would view the fundus images at the time of the patient encounter, and thus would have more clinical context when interpreting the images, perhaps improving their utility. Importantly, the study was not designed using standardized grading forms with pre-defined abnormal fundus findings. Instead, clinicians and image reviewers could select standard descriptions of normal findings or free text abnormal findings. If clinicians and image reviewers used a form with pre-defined abnormal fundus findings, agreement would likely have been higher.
This study is limited by image quality. Nearly a third of montages could not be composed by the montaging software and another 7% were designated uninterpretable by the image reviewers. Poor lens clarity was associated with lower quality images. Ungradable images are a known barrier in teleophthalmology; they are a common reason for referral,30 especially as they may signify underlying pathology.31 Ungradable image rates were as high as 35% in early teleophthalmology programs using standard-field imaging systems,32 which were susceptible to small pupil sizes, ocular media opacities (eg, cataract, vitreous hemorrhage), imager inexperience,30 and dark irides.33 In contrast, ungradable image rates are reported to be less than 5% using ultra-widefield imaging.34 In this study, graduate student optometrists followed a written protocol to capture images. Of note, the camera was new to the eye center and the first images taken were for this project.
There are several other limitations to review. The purpose of this study was to screen for pathology in a routine patient population. The low prevalence of pathology may overstate statistical significance. The ophthalmoscopic examinations were performed through nondilated pupils, whereas dilated examinations may offer a fairer comparison for nonmydriatic ultra-widefield imaging. Nevertheless, comparing nondilated examinations to nonmydriatic imaging is true to the real-life context of the study, as the current standard-of-care in the United Kingdom is nondilated ophthalmoscopic examination.21 Finally, there are inherent limitations of using two-dimensional rather than stereoscopic images for the purposes of ocular screening. Supplemental information, including visual acuity, patient-reported symptoms, and other clinical data may be helpful.
In conclusion, in this study we found that ultra-widefield imaging agreed substantially with standard-of-care optometric examinations for the detection of most clinically meaningful fundus pathology, and that it detected a broader range of findings. In practice, ultra-widefield imaging may be used as a screening tool to identify patients requiring a dilated examination or specialty referral. Future studies with larger numbers of patients are warranted to verify its utility in routine patient populations.
Ethics Statement
The internal governance committee at Specsavers waived informed consent as only anonymized data were shared with UCSF. UCSF Institutional Review Board approval was not required as only anonymized data were analyzed.
Acknowledgments
We thank Dr. Josie Forte and Phil Gray at Specsavers for participant recruitment and data collection, and for sharing their expertise throughout the study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This is an unfunded study.
Disclosure
Dr Jay Stewart reports consulting fees for work unrelated to the present study from Carl Zeiss Meditec. The authors declare that they have no other conflicts of interest for this work.
References
1. Rathi S, Tsui E, Mehta N, Zahid S, Schuman JS. The Current State of Teleophthalmology in the United States. Ophthalmology. 2017;124(12):1729–1734. doi:10.1016/j.ophtha.2017.05.026
2. The Way Forward; 2017. Available from: https://www.rcophth.ac.uk/wp-content/uploads/2015/10/RCOphth-The-Way-Forward-Executive-Summary-300117.pdf.
3. Liew G, Michaelides M, Bunce C. A comparison of the causes of blindness certifications in England and Wales in working age adults (16-64 years), 1999-2000 with 2009-2010. BMJ Open. 2014;4(2):e004015. doi:10.1136/bmjopen-2013-004015
4. Liu Y, Torres Diaz A, Benkert R. Scaling Up Teleophthalmology for Diabetic Eye Screening: opportunities for Widespread Implementation in the USA. Curr Diab Rep. 2019;19(9):74. doi:10.1007/s11892-019-1187-5
5. Cavallerano AA, Conlin PR. Teleretinal imaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol. 2008;2(1):33–39. doi:10.1177/193229680800200106
6. Portney DS, Zhu Z, Chen EM, et al. COVID-19 and Use of Teleophthalmology (CUT Group): trends and Diagnoses. Ophthalmology. 2021;128(10):1483–1485. doi:10.1016/j.ophtha.2021.02.010
7. Parikh D, Armstrong G, Liou V, Husain D. Advances in Telemedicine in Ophthalmology. Semin Ophthalmol. 2020;35(4):210–215. doi:10.1080/08820538.2020.1789675
8. Sommer AC, Blumenthal EZ. Telemedicine in ophthalmology in view of the emerging COVID-19 outbreak. Graefes Arch Clin Exp Ophthalmol. 2020;258(11):2341–2352. doi:10.1007/s00417-020-04879-2
9. Panwar N, Huang P, Lee J, et al. Fundus Photography in the 21st Century--A Review of Recent Technological Advances and Their Implications for Worldwide Healthcare. Telemed J E Health. 2016;22(3):198–208. doi:10.1089/tmj.2015.0068
10. Nagiel A, Lalane RA, Sadda SR, Schwartz SD. ULTRA-WIDEFIELD FUNDUS IMAGING: a Review of Clinical Applications and Future Trends. Retina. 2016;36(4):660–678. doi:10.1097/iae.0000000000000937
11. Patel SN, Shi A, Wibbelsman TD, Klufas MA. Ultra-widefield retinal imaging: an update on recent advances. Ther Adv Ophthalmol. 2020;12:2515841419899495. doi:10.1177/2515841419899495
12. Aiello LP, Odia I, Glassman AR, et al. Comparison of Early Treatment Diabetic Retinopathy Study Standard 7-Field Imaging With Ultrawide-Field Imaging for Determining Severity of Diabetic Retinopathy. JAMA Ophthalmol. 2019;137(1):65–73. doi:10.1001/jamaophthalmol.2018.4982
13. Ashraf M, Shokrollahi S, Salongcay RP, Aiello LP, Silva PS. Diabetic retinopathy and ultrawide field imaging. Semin Ophthalmol. 2020;35(1):56–65. doi:10.1080/08820538.2020.1729818
14. Manjunath V, Papastavrou V, Steel DH, et al. Wide-field imaging and OCT vs clinical evaluation of patients referred from diabetic retinopathy screening. Eye. 2015;29(3):416–423. doi:10.1038/eye.2014.320
15. Purbrick RM, Izadi S, Gupta A, Chong NV. Comparison of Optomap ultrawide-field imaging versus slit-lamp biomicroscopy for assessment of diabetic retinopathy in a real-life clinic. Clin Ophthalmol. 2014;8:1413–1417. doi:10.2147/opth.S66700
16. Silva PS, Cavallerano JD, Sun JK, Noble J, Aiello LM, Aiello LP. Nonmydriatic ultrawide field retinal imaging compared with dilated standard 7-field 35-mm photography and retinal specialist examination for evaluation of diabetic retinopathy. Am J Ophthalmol. 2012;154(3):549–559.e2. doi:10.1016/j.ajo.2012.03.019
17. Neubauer AS, Kernt M, Haritoglou C, Priglinger SG, Kampik A, Ulbig MW. Nonmydriatic screening for diabetic retinopathy by ultra-widefield scanning laser ophthalmoscopy (Optomap). Graefes Arch Clin Exp Ophthalmol. 2008;246(2):229–235. doi:10.1007/s00417-007-0631-4
18. Lim WS, Grimaldi G, Nicholson L, Basheer K, Rajendram R. Widefield imaging with Clarus fundus camera vs slit lamp fundus examination in assessing patients referred from the National Health Service diabetic retinopathy screening programme. Eye. 2021;35(1):299–306. doi:10.1038/s41433-020-01218-x
19. Kornberg DL, Klufas MA, Yannuzzi NA, Orlin A, D’Amico DJ, Kiss S. Clinical Utility of Ultra-Widefield Imaging with the Optos Optomap Compared with Indirect Ophthalmoscopy in the Setting of Non-Traumatic Rhegmatogenous Retinal Detachment. Semin Ophthalmol. 2016;31(5):505–512. doi:10.3109/08820538.2014.981551
20. Brown K, Sewell JM, Trempe C, Peto T, Travison TG. Comparison of image-assisted versus traditional fundus examination. Eye Brain. 2013;5:1–8. doi:10.2147/eb.S37646
21. Standards of Practice for Optometrists and Dispensing Opticians. Available from: https://www.college-optometrists.org/clinical-guidance/guidance/knowledge,-skills-and-performance/the-routine-eye-examination#Conductingtheroutineeyeexamination.
22. Boucher MC, Gresset JA, Angioi K, Olivier S. Effectiveness and safety of screening for diabetic retinopathy with two nonmydriatic digital images compared with the seven standard stereoscopic photographic fields. Can J Ophthalmol. 2003;38(7):557–568. doi:10.1016/s0008-4182(03)80109-6
23. Crabtree BF, Miller WL. Doing Qualitative Research. Sage Publications; 1999.
24. Resnikoff S, Felch W, Gauthier TM, Spivey B. The number of ophthalmologists in practice and training worldwide: a growing gap despite more than 200,000 practitioners. Br J Ophthalmol. 2012;96(6):783–787. doi:10.1136/bjophthalmol-2011-301378
25. Foot B, MacEwen C. Surveillance of sight loss due to delay in ophthalmic treatment or review: frequency, cause and outcome. Eye. 2017;31(5):771–775. doi:10.1038/eye.2017.1
26. Cai S, Liu TYA. The Role of Ultra-Widefield Fundus Imaging and Fluorescein Angiography in Diagnosis and Treatment of Diabetic Retinopathy. Curr Diab Rep. 2021;21(9):30. doi:10.1007/s11892-021-01398-0
27. Kernt M, Hadi I, Pinter F, et al. Assessment of diabetic retinopathy using nonmydriatic ultra-widefield scanning laser ophthalmoscopy (Optomap) compared with ETDRS 7-field stereo photography. Diabetes Care. 2012;35(12):2459–2463. doi:10.2337/dc12-0346
28. Schwartz JT. Methodologic differences and measurement of cup-disc ratio: an epidemiologic assessment. Arch Ophthalmol. 1976;94(7):1101–1105. doi:10.1001/archopht.1976.03910040021004
29. Tielsch JM, Katz J, Quigley HA, Miller NR, Sommer A. Intraobserver and interobserver agreement in measurement of optic disc characteristics. Ophthalmology. 1988;95(3):350–356. doi:10.1016/s0161-6420(88)33177-5
30. Mansberger SL, Gleitsmann K, Gardiner S, et al. Comparing the effectiveness of telemedicine and traditional surveillance in providing diabetic retinopathy screening examinations: a randomized controlled trial. Telemed J E Health. 2013;19(12):942–948. doi:10.1089/tmj.2012.0313
31. Owsley C, McGwin G Jr, Lee DJ, et al. Diabetes eye screening in urban settings serving minority populations: detection of diabetic retinopathy and other ocular findings using telemedicine. JAMA Ophthalmol. 2015;133(2):174–181. doi:10.1001/jamaophthalmol.2014.4652
32. Ahmed J, Ward TP, Bursell SE, Aiello LM, Cavallerano JD, Vigersky RA. The sensitivity and specificity of nonmydriatic digital stereoscopic retinal imaging in detecting diabetic retinopathy. Diabetes Care. 2006;29(10):2205–2209. doi:10.2337/dc06-0295
33. Gupta V, Bansal R, Gupta A, Bhansali A. Sensitivity and specificity of nonmydriatic digital imaging in screening diabetic retinopathy in Indian eyes. Indian J Ophthalmol. 2014;62(8):851–856. doi:10.4103/0301-4738.141039
34. Silva PS, Horton MB, Clary D, et al. Identification of Diabetic Retinopathy and Ungradable Image Rate with Ultrawide Field Imaging in a National Teleophthalmology Program. Ophthalmology. 2016;123(6):1360–1367. doi:10.1016/j.ophtha.2016.01.043
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
