Back to Journals » Risk Management and Healthcare Policy » Volume 16
Trends of the Global, Regional and National Incidence, Mortality, and Disability-Adjusted Life Years of Malaria, 1990–2019: An Analysis of the Global Burden of Disease Study 2019
Authors Shi D, Wei L, Liang H, Yan D, Zhang J, Wang Z
Received 18 May 2023
Accepted for publication 21 June 2023
Published 26 June 2023 Volume 2023:16 Pages 1187—1201
DOI https://doi.org/10.2147/RMHP.S419616
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Donglei Shi,* Li Wei,* Hongsen Liang, Dongqing Yan, Junhang Zhang, Zhaojun Wang
Department of Thoracic Surgery, The Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, 518107, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhaojun Wang, Department of Thoracic Surgery, The Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, 518107, People’s Republic of China, Email [email protected]
Background: Malaria remains a substantial concern in the realm of public health on a worldwide level. Using information from the global burden of disease (GBD) 2019 for 204 countries and territories between 1990 and 2019, we assessed the burden of malaria.
Methods: Data on malaria were derived from the GBD 2019 study between 1990 and 2019. We evaluated the number of incidence, deaths, disability-adjusted life years (DALYs), age-standardized incidence rates (ASIR), age-standardized mortality rates (ASMR), and age-standardized DALY rates (ASDR), examining them across variables such as age, year, gender, country, region, and socio-demographic index (SDI).
Results: The burden of malaria decreased globally between 1990 and 2019. There were 2313.57× 105 incident cases and 6.43× 105 deaths in 2019, contributing to 464.38× 105 DALYs. Largest incident cases were observed in Western Sub-Saharan Africa [1151.72 (95% UI: 890.01– 1527.17)] × 105 in 2019. The only region where deaths increased between 1990 and 2019 was Western Sub-Saharan Africa. ASRs of malaria are distributed heterogeneously in different regions. The highest ASIR was observed in Central Sub-Saharan Africa [21,557.65 (95% UI: 16,639.4– 27,491.48)] in 2019. From 1990 to 2019, the ASMR of malaria declined. Compared to other age cohorts, the ASIR, ASMR, and ASDR for children aged between 1 to 4 years were found to be higher. Worst-affected regions by malaria infection were the low-middle SDI region and low SDI region.
Conclusion: Malaria threatens global public health, especially in Central Sub-Saharan Africa and Western Sub-Saharan Africa. Children 1– 4 years old continue to bear the most significant burden of malaria. The study’s results will guide efforts to reduce malaria’s impact on the global population.
Keywords: malaria, global burden of disease, ASIR, ASMR, ASDR
Background
Malaria continues to have an adverse impact on the health and well-being of individuals across the globe, jeopardizing their sustenance and quality of life.1 Despite the burden of malaria has decreased significantly over the past ten years,2 due to increased uptake of high-impact interventions, it continues to pose a significant global health threat. A rise from 245 million cases in 2020 to an expected 247 million cases worldwide in 84 malaria-endemic countries in 2021, with the majority of this increase coming from countries in the WHO African Region.3 The expected number of malaria-related deaths in 2021 was 619 000, a small decrease from 2020.3 The African continent accounts for 96% of malaria deaths, and most malaria deaths still occur in children under five.4 Malaria is prevalent in low-income countries, particularly among children, pregnant women, and other vulnerable populations such as migrants.
Malaria is a parasite-based disease spread by mosquitoes.5 There are approximately 30–40 species of anopheles mosquitoes that transmit malaria. Four distinct species of malaria parasites have been identified that infect humans, namely Plasmodium vivax, Plasmodium falciparum, Plasmodium malariae, and Plasmodium ovale.6 Among these, Plasmodium falciparum and Plasmodium vivax are the most widespread, with Plasmodium falciparum being the most lethal.1 Even though malaria can be fatal, illness and death can be prevented in most cases.5
Although malaria is mainly prevalent in the world health organization (WHO) African Region, there are significant variations in the prevalence of malaria across different countries and within different WHO regions.2 Burden of malaria must be better understood at the global and regional level. Understanding the burden of malaria in the global and regional level is crucial, it helps in identifying the areas that are most affected by malaria and where interventions are needed the most, and it helps in allocating resources and prioritizing interventions based on the burden of malaria in different regions. In a recent study, Liu et al directed their attention towards the global patterns and regional discrepancies in the incidence of malaria infection, while excluding the age-standardized mortality rates (ASMR) and age-standardized disability-adjusted life years (DALYs) rates (ASDR) attributable to the burden of malaria.7 The ASMR and ASDR allow for a more accurate comparison of the burden of malaria across different populations and time periods, as they account for differences in age distribution. In this study, we extracted specific data on the incidence, death, and DALYs rates of malaria by using the global burden of disease (GBD) 2019. We examined the temporal trends of malaria at the global and regional level from 1990 to 2019 to better comprehend the illness burden of malaria. We also examined the connection between malaria burden and the Socio-demographic Index (SDI). As a complement and extension of previous studies, our study could provides a comprehensive perspective on how the world can work toward eliminating malaria.
Methods
Overview
The GBD study, spearheaded by the Institute for Health Metrics and Evaluation (IHME), represents the most extensive observational epidemiological investigation ever carried out to date. As the health challenges of 21st-century change worldwide, the GBD study offers a valuable resource for understanding them.8 GBD provides a method to calculate health losses caused by numerous diseases, accidents, and risk factors. In more than 156 nations and territories, more than 7000 academics compiles and examines data on the GBD.9 The GBD database furnishes appraisals in the form of age-standardized rates per 100,000 individuals. The metrics are accompanied by their corresponding 95% uncertainty intervals (95% UI) as well.10 To establish a 95% uncertainty interval (UI) for each mortality and morbidity estimate, the 0.025 and 0.975 quantiles were determined from 1000 draws of the posterior distribution.11 The data was sourced from the GBD 2019 database, accessible at https://vizhub.healthdata.org/gbd-results/. The search parameters were set as follows: “Cause of death or injury” for the GBD estimate; “deaths, DALYs” for measure; “number and rate” for metric; “Malaria” for cause; “Global, Select all countries and territories, and Select 21 regions” for location; “All ages, Age-standardized, <5 years, 6–9 years, 10–14 years, 15–19 years, 20–24 years, 25–29 years, 30–34 years, 35–39 years, 40–44 years, 45–49 years, 50–54 years, 55–59 years, 60–64 years, 65–69 years, 70–74 years, 75–79 years, 80–84 years, 85–89 years, 90–94 years, 95+” for age; “Male, Female, and Both” for sex, and “1990–2019” for year. The general methodologies adopted to estimate the incidence, mortality, and DALYs attributable to malaria infection have been explicated elsewhere.12
Definition
Malaria is a disease caused by a parasitic infection transmitted through mosquito bites. The symptoms of uncomplicated malaria typically include persistent fever, chills or shivering, sweating, joint pain, and headaches, lasting for a duration of one to two weeks. During the attack, the individual is likely to experience lethargy and fever, which may result in a loss of daily function. As per the International Classification of Diseases, 9th (ICD-9) and 10th (ICD-10) revisions, malaria was identified and described as follows: ICD-9 (084–084.9, V12.03, V75.1) and ICD-10 (B50-B50.0, B50.8-B52.0, B52.8-B53.1, B53.8-B54.0, P37.3-P37.4).13 SDI is a rapid indicator of a nation’s progress. SDI is a composite statistic that includes the total fertility rate for people under the age of 25, the years of schooling for people above the age of 15, and lagged per-capita income.14
Estimation Methods
National routine surveillance systems and cross-sectional, geolocated, and community-representative observations of Plasmodium falciparum infection prevalence are the two main sources of malaria data. Different methods for calculating malaria mortality were required due to Plasmodium falciparum. Use a technique that creates a geographically diverse grid of case fatality rates in Plasmodium falciparum-infected nations. Instead, a very basic approach was employed to assign a nominal number of deaths to malaria in nations where Plasmodium vivax was the only species present. The Malaria Atlas Project modeled estimates for the population coverage of insecticide-treated bed nets, indoor residual spraying, and effective antimalarial medication treatment. These estimates were resolved to a 5 km × 5 km pixel-year level (for sub-Saharan Africa) and country-year level (outside of sub-Saharan Africa). High-resolution gridded population data were combined with pixel-level clinical incidence rate estimates (both within and outside of Africa) to determine the overall number of malaria cases per pixel-year. A two-step procedure used in GBD 2019 to assess the severity of malaria. By analyzing Medical Expenditure Panel Survey data, it was possible to develop severity splits for mild, moderate, and severe malaria in acute cases. Analyzed the proportion of straightforward instances that resulted in longer-term damage to estimate the long-term neurological burden caused by malaria.
Statistical Analysis
We evaluated the trend of the ASIR, ASMR, and ASDR in global, High SDI, High-middle SDI, Middle SDI, Low-middle SDI, and Low SDI. We produced world maps of malaria to demonstrate the geographic variation concerning malaria in the ASIR, ASMR, and ASDR in 2019. We estimated differences in the burden of malaria by age group and sex in 1990 and 2019. 204 countries and territories were classified into 21 regions according to the physical proximity and epidemiological homogeneity of these areas.9 Herein, we reported the ASIR, ASMR, and ASDR of malaria in 21 regions. We used R statistical software to analyze and display the data (version 4.1.2).
Results
Global Burden of Malaria
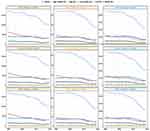
Over the past three decades, ASIR, ASMR, and ASDR impact of malaria has been steadily declining globally, and it started to decline significantly near 2000; they all decreased by approximately 50% in both sexes, females and males (Figure 1). Incident cases of malaria were observed to a slight decrease from 2427.86 (95% UI: 2007.66–2985.45) ×105 in 1990 to 2313.57 (95% UI: 1860.34–2902.17) ×105 in 2019 in global (Table 1). Meanwhile, the number of deaths, ASIR, ASMR, and ASDR, were different degrees of decline between 1990 and 2019 (Tables 1–3). Death number decreased from 8.41 (95% UI: 4.63–13.56) ×105 in 1990 to 6.43 (95% UI: 3.02–11.54) ×105 in 2019. ASIR decreased from 4084.08 (95% UI: 3388.02–4998.95) in 1990 to 3247.02 (95% UI: 2602.06–4109.56) per 100,000 population in 2019. ASMR decreased from 14.42 (95% UI: 7.95–23.21) in 1990 to 8.95 (95% UI: 4.23–16) per 100,000 population in 2019. ASDR decreased from 1074.99 (95% UI: 608.96–1721.22) in 1990 to 668.11 (95% UI: 337.28–1152.22) per 100,000 population in 2019.
 |
Table 1 Incidence Cases and ASIR of Malaria for Both Sexes in 1990 and 2019 |
 |
Table 2 Death Cases and ASMR of Malaria for Both Sexes in 1990 and 2019 |
 |
Table 3 DALYs Number and ASDR of Malaria for Both Sexes in 1990 and 2019 |
Regional and National Burden of Malaria
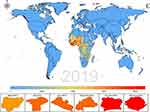
The ASRs of Malaria is distributed heterogeneously in different countries. Benin had the highest ASIR [27,623.5 (95% UI: 22,120–35,038.8)] per 100,000 population of malaria in 2019, followed by Liberia [27,428 (95% UI: 18,195.2–35,833.4)], Central African Republic [25,301 (95% UI: 16,640.2–35,405], Côte d’Ivoire [24,841.5 (95% UI: 16,135–35,485.1)], and Sierra Leone [24,122.6 (95% UI: 13,122.1–34,152.4)]. There were 118 countries and territories with zero ASIR in 2019 (Figure 2A, Appendix Table 1). Sierra Leone [162.53 (95% UI: 61.69–290.56)], Côte d’Ivoire [143.45 (95% UI: 67.72–268.08)], Liberia [130.78 (95% UI: 53.01–239.2)] are the top 3 countries with ASMR of malaria in 2019, there were 129 countries and territories with an ASMR of zero in 2019 (Figure 2B, Appendix Table 2). Sierra Leone [8615 (95% UI: 3642.3–14,846.9)] per 100,000 population has the highest ASDR of malaria in 2019, followed by Côte d’Ivoire [6871.7 (95% UI: 3576.5–11,949.6)], there were 116 countries and territories with an ASDR of zero in 2019 (Figure 2C, Appendix Table 3).
Figure 2 Continued. Figure 2 Continued.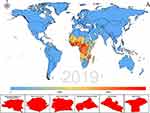
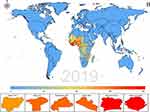
Largest incident cases were observed in Western Sub-Saharan Africa [1151.72 (95% UI: 890.01–1527.17) × 105] in 2019, followed by Eastern Sub-Saharan Africa [564.32 (95% UI: 423.93–732.38) × 105] across the 21 GBD regions. The highest ASIR was observed in Central Sub-Saharan Africa [30,614.03 (95% UI: 24,443.73–36,630.34)] and Western Sub-Saharan Africa [30,389.1 (95% UI: 24,508.25–37,164.36)] per 100,000 population in 1990, decreased to 21,557.65 (95% UI:16,639.4–27,491.48) and 19,092.54 (95% UI: 14,859.41–24,474.7) per 100,000 population in 2019, respectively. Central Sub-Saharan Africa, Central Latin America, Western Sub-Saharan Africa, and Eastern Sub-Saharan Africa could see an increase in incident cases of malaria between 1990 and 2019. Malaria incidence is kept zero from 1990 to 2019 in Central Europe, Australasia, High-income North America, Eastern Europe, and Western Europe. Incidence of malaria cases went down to zero in Southern Latin America and Central Asia in 2019 (Table 1). The highest deaths number was in Western Sub-Saharan Africa [3.96 (95% UI: 1.86–7.22) × 105], followed by Eastern Sub-Saharan Africa [1.19 (95% UI: 0.5–2.27) × 105], the remaining 19 regions all had very low deaths number in 2019. Western Sub-Saharan Africa was the only region where deaths increased between 1990 and 2019. The following regions all had zero deaths in 2019 (Australasia, Andean Latin America, Central Europe, Central Asia, Eastern Europe, East Asia, High-income North America, High-income Asia Pacific, Tropical Latin America, Southern Latin America, and Western Europe). From 1990 to 2019, the ASMR of malaria decreased, and there were nine regions where the ASMR was zero in 2019 (Table 2). Western Sub-Saharan Africa [273.87 (95% UI: 135.09–480.97) × 105] has the highest DALYs number in 2019, more than double that of Eastern Sub-Saharan Africa [94.45 (95% UI: 43.09–171.42) × 105], and was the only region to rise. Western Sub-Saharan Africa [5204.34 (95% UI: 2529.28–9325.86)] per 100,000 population had the highest ASDR in 2019. ASDR of malaria declined from 1990 to 2019. The ASDR was zero in 2019 in Central Europe, Australasia, Eastern Europe, Southern Latin America, High-income North America, and Western Europe.
Age and Sex Patterns
There was little difference between males and females in incident cases, deaths number, and DALYs number. Additionally, their ASRs showed similar differences (Tables 1–3). Figure 3 shows that highest ASIR, ASMR, and ASDR were 1–4 years old by sex globally in 1990 and 2019. ASIR showed a downward trend with increased age in females and males in 1990 and 2019. ASMR began to decrease from age group 1–4 to 30–34 years old and gradually began to rise to 70–74 years old, and after that, the ASMR decreased in females and males in 1990 and 2019. ASDR varies little from 10–14 years old to 75–79 years old in females and males in 1990 and 2019, and the ASDR is very low for people over 80–84 years old (Figure 3).
Association with the SDI
Between the five SDI regions, there were significant variations in malaria ASRs. Low-middle SDI region and Low SDI region suffered from severest malaria infection, followed Middle SDI region. High-middle SDI region and the High SDI region had very low malaria ASRs (Figure 1). The number of incident cases of malaria increased only in the low SDI region, from 1256.28 (95% UI: 1017.92–1498.38) × 105 in 1990 to 1467.72 (95% UI: 1184.39–1856.39) × 105 in 2019. The ASIR of malaria infection had the highest decrease in the low SDI region, from 17,324.72 (95% UI: 14,158.03–20,551.63) per 100,000 population in 1990 to 10,228.91 (95% UI: 8298.45–12,609.16) per 100,000 population in 2019. Malaria ASIR decreased from extremely low levels in 4.99 in 1990 to 0.17 per 100,000 population in 2019 in the high SDI region (Table 1). Death cases, DALYs number, ASMR, and ASDR of malaria showed a downward trend in five SDI regions between 1990 and 2019. In 2019, highest ASMR and ASDR were recorded in the low SDI region, 35.21 (95% UI: 14.88–66.15) and 2174.42 (95% UI: 1030.48–3877.18) per 100,000 population, respectively (Tables 2–3).
Relationship between SDI and malaria ASRs in 21 GBD regions from 1990 to 2019 was explored. Overall, our analysis revealed a detrimental correlation between ASRs and SDI for malaria spanning from 1990 to 2019. Notably, the turning point was around 0.5, beyond which ASRs did not show any significant increase despite an upward trend in SDI. Western Sub-Saharan Africa, Central Sub-Saharan Africa, and Southern Sub-Saharan Africa had higher than expected ASIR from 1990 to 2019. In contrast, the ASIR of malaria was lower than expected for South Asia, Tropical Latin America, and East Asia. Eastern Sub-Saharan Africa had an ASIR higher than expected in the early years. Oceania has a clear downward trend and has fallen below the expectation line but has recently risen above the expectation line. Western Sub-Saharan Africa, Southern Sub-Saharan Africa, and Central Sub-Saharan Africa had higher ASMR than expected from 1990 to 2019. Oceania presents an irregular nonlinear relationship between SDI and ASMR of malaria. Similar results can be found between SDI and ASDR of malaria (Figure 4).
Discussion
The burden of malaria has significantly been reduced in recent decades. Our results also confirm this point, we found that the ASRs of malaria decreased globally, with a significant decline beginning around the year 2000. The primary factor can be attributed to the significant increase in malaria interventions between 2001 and 2013, according to the WHO, the estimated 47% decline in global malaria mortality rates, which prevented approximately 4.3 million deaths between 2001 and 2013.1 The scale-up of interventions has led to millions of lives being saved worldwide, and malaria mortality has decreased by 36% from 2010 to 2020.15 The number of nations with an active malaria epidemic decreased from 108 in 2000 to 84 in 2021, indicating that progress toward its eradication is being made.3
Regions and countries differed significantly in terms of heterogeneity. At the regional level, an increase in malaria cases could be observed in Central Latin America, Central Sub-Saharan Africa, Eastern Sub-Saharan Africa, and Western Sub-Saharan Africa. At the same time, Western Sub-Saharan Africa was the only region where we observed an increase in the number of deaths between 1990 and 2019. We believe that the reasons may be complex, one of the primary reasons is inadequate funding for malaria control programs. Many countries in the region have limited resources and struggle to allocate sufficient funds to combat the disease effectively. Weak health systems also play a significant role, as they often lack the necessary infrastructure and trained personnel to provide adequate care and treatment for malaria patients. Another factor is the emergence of drug-resistant strains of the malaria parasite. This makes it more challenging to treat and control the disease, as traditional medications may no longer be effective. Climate change is also a contributing factor, as it can create more favorable conditions for the mosquitoes that transmit malaria to thrive and spread the disease.1,3 The specific reasons may need further investigation and research. It is imperative that prevention and management policies for malaria receive greater attention in these regions, it is essential to implement effective measures to prevent and control the spread of malaria, such as providing access to insecticide-treated mosquito nets, improving diagnosis and treatment services, and investing in research to develop new and more effective malaria prevention and treatment strategies. At the country level, African countries such as Benin, Sierra Leone, and Côte d’Ivoire have a high burden of ASIR, ASMR, and ASDR, but more than 100 countries have zero. Benin is among the 30 countries that have managed to achieve their goal of reducing the mortality rate by less than 40%.2 Besides, Sierra Leone is estimated to have achieved a reduction in the incidence of malaria cases by the year 2020 as compared to the incidence in 2015. Controlling malaria has proved to be extremely difficult in Africa. The transmission rate has again increased, and malaria infections in Africa increased by 7% to about 228 million between 2019 and 2020. Several potential causes have been identified, including insecticide-resistant mosquitoes, drug-resistant malaria, and, most recently, the COVID-19 pandemic.2
In areas with high transmission, malaria is most prevalent among children under five,16 and our results support this point. According to the GBD database, those under five years are counted for ages one to four years. Children under the age of five are more vulnerable to malaria due to their immature immune system, limited access to protective measures, and spend more time outside increasing their exposure to mosquito bites.3 Fortunately, the WHO recommends the use of the RTS,S/AS01 malaria vaccine to prevent Plasmodium falciparum malaria in children living in areas with moderate to high transmission rates. Implementation of this vaccine could potentially save tens of thousands of lives annually and contribute to reducing child mortality rates in Africa.17 The RTS,S/AS01 vaccine’s public health potential has been acknowledged by WHO, but integration of RTS,S into a country’s vaccine regimen faces significant obstacles.18 Therefore, malaria prevention interventions of children under five years of age are still needed.
Although there are more than 100 countries and territories with zero ASRs in 2019, the threat of imported malaria will continue to exist in countries where malaria has been eradicated.19 Malaria can be contracted by people from countries without malaria when traveling to countries endemic to malaria. Malaria can be effectively prevented through mosquito bite protection and chemoprophylaxis for travelers to malaria-endemic areas.6 It has been shown that the drugs used to prevent malaria are safe and well tolerated over the long term. Therefore, malaria prophylactic drugs are recommended for travelers to countries where malaria is endemic.
Malaria is predominantly found in impoverished regions of the world with tropical and subtropical climates.20 In this study, we observed that the low-middle SDI region and low SDI region suffered from severest malaria infection. The likely reasons for the high prevalence of malaria in Africa are the favorable weather conditions that allow for year-round transmission of the disease and the insufficiency of resources and socio-economic instability pose significant obstacles to implementing effective malaria control measures.20 Meanwhile, malaria has enormous costs for individuals, families, communities, and nations. Gross domestic product grew 1.3% slower per person annually in countries with high malaria transmission rates.21
In May 2015, the World Health Assembly adopted the Global Technical Strategy for Malaria 2016–2030 (GTS),1–3 which aims to achieve a reduction in malaria mortality and incidence of at least 40% from the 2015 baseline by 2020, 75% by 2025, and 90% by 2030.2 However, global burden of malaria mortality and morbidity was 94% in the African Region of the WHO in 2019, and only nine countries met the 2020 milestones. The main reasons are as follows: It is primarily due to the rapid population growth in sub-Saharan Africa. During the COVID-19 pandemic, significant disruptions in the delivery of malaria services have been highlighted. There are still too many people who are not receiving malaria interventions. Even there are still 30% of people around the world cannot access essential health care.22 Development made in nations that have eradicated malaria and those that have significantly lowered transmission levels shows best practices to direct development elsewhere. Best preventive measures are: wearing long-sleeved clothing, putting wire mesh on our homes, sleeping under bed nets, taking antimalarial medications according to the doctor’s advice, mosquito breeding areas should be cleaned, and insecticides should be sprayed inside or outside.23 It is possible to reduce the burden on health systems effortlessly with special measures like presumptive malaria management and mass drug management.23 Furthermore, it may be possible to reduce the burden of malaria by controlling disease-transmitting mosquitoes with genetically engineered gene-driven mosquitoes.4 The experiences during the COVID-19 pandemic in Nigeria demonstrated that the resources of various donors should be grouped and unified to reduce fragmentation and increase collective responses.24
Malaria studies had greatly aided by global funding. However, the funding gap between invested funds and the resources needed has recently increased dramatically. Achieving the global strategy will require more than triple the amount spent on malaria fighting in the next ten years.2 It will also be necessary to increase malaria funding in the future.
Infection with malaria poses serious risks to pregnant women, their fetuses, and their newborns.15 Malaria infection during pregnancy can lead to various adverse outcomes such as maternal anemia, preterm delivery, fetal loss, low birth weight, and cognitive impairment in newborns.25,26 One in four pregnant women in malaria-endemic African malaria-endemic areas was believed to carry a malaria infection at the time of delivery.27 WHO reported that 34% of pregnancies in the 33 moderate and high-transmission countries of the WHO African Region were exposed to malaria infection in 2020.2 Because the GBD database lacks data on pregnant women, this article cannot estimate the global burden of malaria among them. Malaria remains a significant threat to pregnant women. We should take targeted measures to protect pregnant women from malaria.
Our study used GBD 2019 to investigate the burden of malaria, but there are some limitations. First, The system dynamics model and statistical model were combined to produce estimates for the GBD results, which do not represent actual observation data and may not be accurate. Second, pregnant women are not specifically analyzed. Third, Low-income countries with poor health supervision systems may not accurately capture the true prevalence of malaria.
Conclusions
This study estimated the burden of malaria in the last 30 decades. From 1990 to 2019, there was a decline in the global burden of malaria, the degree of heterogeneity varied greatly between regions and nations. The burden of malaria remains elevated in Africa, particularly in Western and Central Sub-Saharan Africa. There is a particular need to pay more attention to children 1–4 years old. The findings of our study provided a scientific reference point for malaria prevention and control strategies in different countries and regions.
Ethical Approval
This study adhered to the principles outlined in the Declaration of Helsinki and was approved by the Ethics Committee of the Seventh Affiliated Hospital, Sun Yat-sen University (KY-2023-034-01).
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Global Technical Strategy for Malaria 2016–2030, 2021 Update. Geneva: World Health Organization; Licence: CC BY-NC-SA 3.0 IGO; 2021.
2. World Health Organization. World Malaria Report 2021. Geneva: World Health Organization; Licence: CC BY-NC-SA 3.0 IGO; 2021.
3. World Health Organization. World Malaria Report 2022. Geneva: World Health Organization; Licence: CC BY-NC-SA 3.0 IGO; 2022.
4. Garrood WT, Cuber P, Willis K, Bernardini F, Page NM, Haghighat-Khah RE. Driving down malaria transmission with engineered gene drives. Front Genet. 2022;13:891218. doi:10.3389/fgene.2022.891218
5. Centers for Disease Control and Prevention (CDC). About malaria; 2022. Available from: https://www.cdc.gov/malaria/about/.
6. Centers for Disease Control and Prevention (CDC). What is malaria? 2022. Available from: https://www.cdc.gov/malaria/about/faqs.html.
7. Liu Q, Jing W, Kang L, Liu J, Liu M. Trends of the global, regional and national incidence of malaria in 204 countries from 1990 to 2019 and implications for malaria prevention. J Travel Med. 2021;28(5):taab046. doi:10.1093/jtm/taab046
8. The lancet. Global burden of disease; 2022. Available from: https://www.thelancet.com/gbd.
9. Institute for Health Metrics and Evaluation. About GBD; 2022. Available from: https://www.healthdata.org/gbd/about.
10. Bezerra JMT, Barbosa DS, Martins-Melo FR, et al. Changes in malaria patterns in Brazil over 28 years (1990–2017): results from the global burden of disease study 2017. Popul Health Metr. 2020;18(Suppl 1):5. doi:10.1186/s12963-020-00211-6
11. Liu H, Qi J, Yang J, et al. Burden of liver complications related to non-alcoholic fatty liver disease in China from 2005–2019: observations from the global burden of disease study, 2019. Diabetes Obes Metab. 2023;25 Suppl 1:43–52. doi:10.1111/dom.15010
12. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
13. Global Burden of Disease Study 2019 (GBD 2019). Cause list mapped to ICD codes; 2022. Available from: https://ghdx.healthdata.org/record/ihme-data/gbd-2019-cause-icd-code-mappings.
14. Wang Z, Hu L, Li J, Wei L, Zhang J, Zhou J. Magnitude, temporal trends and inequality in global burden of tracheal, bronchus and lung cancer: findings from the global burden of disease study 2017. BMJ Glob Health. 2020;5(10):e002788. doi:10.1136/bmjgh-2020-002788
15. Centers for Disease Control and Prevention (CDC). Malaria’s impact worldwide; 2021. Available from: https://www.cdc.gov/malaria/malaria_worldwide/impact.html.
16. World Health Organization. Malaria; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/malaria;.
17. World Health Organization. Q&A on RTS,S malaria vaccine; 2022. Available from: https://www.who.int/news-room/questions-and-answers/item/q-a-on-rts-s-malaria-vaccine.
18. Laurens MB. RTS,S/AS01 vaccine (Mosquirix™): an overview. Hum Vaccin Immunother. 2020;16(3):480–489. doi:10.1080/21645515.2019.1669415
19. Xiao N, Xu Q, Feng J, et al. Approaching malaria elimination in China. China CDC Wkly. 2020;2(17):293–297. doi:10.46234/ccdcw2020.075
20. Centers for Disease Control and Prevention (CDC). Malaria’s impact worldwide; 2022. Available from: https://www.cdc.gov/malaria/malaria_worldwide/impact.html.
21. Andrade MV, Noronha K, Diniz BPC, et al. The economic burden of malaria: a systematic review. Malar J. 2022;21(1):283. doi:10.1186/s12936-022-04303-6
22. World Health Organization. Universal health coverage (UHC); 2022. https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc).
23. Saha J, Chouhan P. Malaria attack and COVID-19 pandemic: is it a double burdening public health concern? Parasite Epidemiol Control. 2022;19:e00277. doi:10.1016/j.parepi.2022.e00277
24. Ihekweazu C. Lessons from Nigeria’s adaptation of global health initiatives during the COVID-19 pandemic. Emerg Infect Dis. 2022;28(13):S299–S301. doi:10.3201/eid2813.221175
25. Rogerson SJ, Unger HW. Pregnancy and malaria: the perfect storm. Curr Opin Infect Dis. 2022;35(5):410–416. doi:10.1097/QCO.0000000000000859
26. Garrison A, Boivin MJ, Fiévet N, et al. The effects of malaria in pregnancy on neurocognitive development in children at 1 and 6 years of age in Benin: a prospective mother-child cohort. Clin Infect Dis. 2022;74(5):766–775. doi:10.1093/cid/ciab569
27. Zavala E, Rhodes M, Christian P. Pregnancy interventions to improve birth outcomes: what are the effects on maternal outcomes? A scoping review. Int J Public Health. 2022;67:1604620. doi:10.3389/ijph.2022.1604620
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.