Back to Journals » Risk Management and Healthcare Policy » Volume 16
Trends and Patterns of Systemic Glucocorticoid Prescription in Primary Care Institutions in Southwest China, from 2018 to 2021
Authors Li X, Zeng Z , Fan X, Wang W, Luo X, Yang J, Chang Y
Received 18 September 2023
Accepted for publication 2 December 2023
Published 21 December 2023 Volume 2023:16 Pages 2849—2868
DOI https://doi.org/10.2147/RMHP.S436747
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jongwha Chang
Xiaoyi Li,1,* Zhen Zeng,2,* Xingying Fan,1,3 Wenju Wang,4 Xiaobo Luo,4 Junli Yang,1 Yue Chang1,3,*
1School of Medicine and Health Management, Guizhou Medical University, Guiyang, Guizhou Province, People’s Republic of China; 2Second Affiliated Hospital of Guizhou University of Traditional Chinese Medicine, Guiyang, Guizhou Province, People’s Republic of China; 3Center of Medicine Economics and Management Research, Guizhou Medical University, Guiyang, Guizhou Province, People’s Republic of China; 4School of Public Health, Guizhou Medical University, Guiyang, Guizhou Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yue Chang; Xingying Fan, School of Medicine and Health Management, Guizhou Medical University, Gui’an New District, Guiyang, Guizhou Province, People’s Republic of China, Email [email protected]; [email protected]
Purpose: The purpose of this study was to investigate the prescribing patterns and usage trends of systemic glucocorticoids in primary care institutions located in Southwest China from 2018 to 2021.
Materials and Methods: A retrospective cross-sectional analysis of systemic glucocorticoids prescriptions was conducted in 32 primary care institutions located in Southwest China between 2018 and 2021. Prescriptions of systemic glucocorticoids were classified as appropriate or inappropriate use. Inappropriate use was further classified into (1) inappropriate indications and (2) inappropriate selection of glucocorticoids. Generalized estimation equations were employed to investigate the factors associated with inappropriate utilization of systemic glucocorticoids. The seasonal autoregressive integrated moving average (SARIMA) model was employed to predict the rate of inappropriate glucocorticoids prescriptions.
Results: A total of 203,846 (92.89%) prescriptions were included, both the number of systemic glucocorticoids prescriptions and inappropriate prescriptions increased in winter. Diseases of the respiratory system (68.90%) were the most frequent targets of systemic glucocorticoids use. Of all prescriptions, 73.18% exhibited inappropriate indications, while 0.05% demonstrated inappropriate selection. The utilization of systemic glucocorticoids was deemed inappropriate for diseases of the respiratory system (94.19%), followed by diseases of the digestive system (87.75%). Physicians, who were female or younger than 33 years old, possess lower levels of education and professional titles and exhibit a higher likelihood of inappropriately prescribing systemic glucocorticoids. The phenomenon of inappropriate glucocorticoids use was commoner among male patients aged 65 years and older. After conducting model verification, it was determined that the SARIMA model could be used to predict the monthly rate of inappropriate systemic glucocorticoids prescriptions in primary care institutions in southwest China.
Conclusion: The inappropriate use of systemic glucocorticoids remains a significant concern in primary care institutions. In this regard, continuing education and professional knowledge training of physicians should be strengthened in the future.
Keywords: systemic glucocorticoids, primary care institutions, prescription patterns, inappropriate use, usage trends
Introduction
Glucocorticoids (GCs) were synthesized in the late 1940s and have since been successfully applied in clinical practice.1,2 Due to its potent anti-inflammatory and immunosuppressive properties, GCs are extensively utilized in the treatment of various diseases, including rheumatic immune diseases, respiratory diseases, and infectious diseases.3–5 While GCs are widely utilized in clinical practice, there has been a noticeable increase in inappropriate usage. Inappropriate use of GCs can result in increased medical burden and various adverse reactions, such as inducing and aggravating infection, gastrointestinal bleeding or perforation, hypertension, and osteoporosis.6–11 Therefore, it is crucial to establish regulatory measures for the clinical application of GCs in order to ensure patient safety during medication administration.
Inappropriate use of systemic GCs has emerged as a global issue. In the United Kingdom, systemic GCs treatment has risen by over 30% within the past two decades, with more than 1% of the population receiving such therapy.12 Over the past 8 years, the rate of oral GCs prescriptions has increased by 14.1% in France.13 A survey conducted in India revealed that approximately 66% of pharmacists were unaware of the potential hazards associated with inappropriate use of GCs,14 and 36% of patients were found to be using these medications inappropriately.15 In the United States, 21% of the population were prescribed short-term outpatient oral GCs, with upper respiratory infections and allergies being the most prevalent indications.16 In China, inappropriate use of GCs is also common,17 particularly within primary care institutions.18,19 A survey of 27 primary care institutions showed that inappropriate GCs prescriptions accounted for 63.50% of total prescriptions.18 In order to regulate rational use of GCs, the Chinese government issued the Guidelines for Clinical Application of GCs in 2011.20 In addition, according to the Chinese Hospital Prescription Review and Management Standards,21 it is mandatory for hospitals to provide prescription comments on GCs. However, despite efforts to improve prescribing practices, inappropriate use of GCs remains prevalent in primary care institutions.19 In our previous study examining 2020 prescribing patterns across 58 primary care institutions, it was found that 68.20% of GCs prescriptions were deemed inappropriate.22
Current studies on GCs primarily focus on their common indications and adverse reactions.23–25 Several studies have examined prescription rates and prevalence of oral GCs.12,13,26,27 The rate of systemic corticosteroid prescriptions in patients with acute respiratory infections is high.28 In addition, there are studies describing prescribing patterns of topical GCs, and factors associated with inappropriate use.14,22 However, there is a lack of systematic and comprehensive research evaluating the long-term trend, current situation, and rationality of GCs use in primary care institutions.
Therefore, we conducted an analysis of prescriptions for systemic GCs in primary care institutions in Southwest China between 2018 and 2021. The aim of this study was to investigate the prescription patterns and usage trends of systemic GCs and determine associated factors for the inappropriate use of systemic GCs. We establish a theoretical foundation for primary care institutions in underdeveloped regions to develop relevant policies and specific measures that facilitate the appropriate utilization of systemic GCs.
Materials and Methods
Ethics Approval
The Ethics Committee of Guizhou Medical University approved this study (REC. 2021 Ethics Approval No. 249) in accordance with ethical guidelines. All participants (physicians) provided written informed consent to participate in the study (Additional File 1). In accordance with the requirements of the confidentiality agreement, all identifying information about the physicians and patients were not released. The study complied with the Declaration of Helsinki.
Study Design and Setting
A retrospective cross-sectional study was conducted from 2018 to 2021 in Guizhou, one of the economically disadvantaged provinces located in southwest China. In accordance with the hierarchical classification system for public hospitals in China, China’s hospital system consists of tertiary hospitals, secondary hospitals, and primary care institutions. Primary care institutions encompass township health centers and community health service centers. Our research was carried out at primary care institutions.
The data was collected from the Hospital Information System (HIS), developed by Guizhou Lianke Weixin Technology Co., LTD (LWTC). We have executed a tripartite agreement (Additional File 2) with the Information Center of Guizhou Provincial Health Commission (ICGPHC) and LWTC. The ICGPHC authorized us to obtain relevant data through LWTC. So far, a total of 132 public primary care institutions in Guizhou Province have implemented HIS system developed by LWTC. In order to ensure the continuity of prescriptions and the stability of the physician, inclusion criteria for the study were established as follows: (1) the designated primary care institutions are required to utilize HIS system developed by LWTC and (2) the selected outpatient physicians must have worked in the primary care institutions from 2018 to 2021. Ultimately, 32 primary care institutions were selected for this study.
Data Sources
The prescribing information of systemic GCs and demographic characteristics of patients were extracted from HIS system. The personal information of physicians was provided by the Personnel Management Department of primary care institutions.
The classification of diseases in this study was established according to the 10th edition of the ICD-10.29 Our study excluded topical systemic GCs such as eye drops, ear drops, aerosols, suspensions for inhalation, and creams. Systemic GCs hormones were categorized into short-acting, medium-acting, and long-acting preparations according to the duration of their action.21 We performed standardized cleaning and sorting before data analysis, and correct logic errors were rectified. All prescriptions are identified by code to connect physicians and patients, forming a database of medical service information.
Appropriate Classification of Glucocorticoids Prescriptions
According to the Guidelines for Clinical Application of Systemic GCs in China and the Hospital Prescription Review and Management Standards of the Ministry of Health, systemic GCs prescriptions were categorized as appropriate or inappropriate based on rational clinical use evaluation criteria. Due to the lack of systemic GCs dose and treatment time, inappropriate use of systemic GCs only includes (1) Inappropriate indications, such as the use of systemic GCs for purposes other than their intended anti-inflammatory effects, including antipyretic or analgesic purposes, and (2) Inappropriate selection of systemic GCs, such as opting for short-acting agents instead of long-acting ones.
Outcome Variables
The outcome variable was the rate of inappropriate systemic GCs prescriptions (IGR), calculated as the number of inappropriate prescriptions divided by the total number of systemic GCs prescriptions. Physician and patient characteristics and information about systemic GCs prescriptions were included as covariates.
Data Analysis
The prescribing frequencies of systemic GCs were analyzed to determine the appropriateness and patterns of prescription. Univariate analysis was performed to preliminarily determine the potential risk factors for inappropriate use of systemic GCs. The Generalized Estimation Equation (GEE) approach was employed to identify independent predictors associated with inappropriate use of systemic GCs. All statistical tests were two-sided, and P-value < 0.05 was considered statistically significant. The statistical analysis was performed using R version 4.2.1.
The seasonal auto-regressive integrated moving average (SARIMA) model was established using the data of GCs inappropriate prescribing frequencies from January 2018 to December 2020. Accuracy of the model’s predictions was assessed using data from January to December 2021. Firstly, the stationarity of time series is tested by sequence diagram or Augmented Dickey–Fuller (ADF) test. The non-stationary time series was converted into a stationary time series through differencing and seasonal differencing. Secondly, the autocorrelation function (ACF) graph and partial autocorrelation (PACF) graph were used to preliminarily determine the range of values for the model. Subsequently, the Box–Ljung test was employed to determine whether it exhibits a white noise sequence, and Box–Ljung test P-value >0.05 was the white noise sequence. The optimal model was determined using the determination coefficient (R2) and Bayesian Information Criterion (BIC). Finally, the optimal model was utilized to predict the monthly rate of inappropriate systemic GCs prescriptions in 2021, and its accuracy was verified by comparing it with actual value while conducting trend analysis. The fundamental structure of the SARIMA model is denoted as SARIMA (p, d, q) × (P, D, Q) s. Where, p represents the autoregressive order term; q denotes the moving average term; d and D signify the number of differences required to extract deterministic information from the original sequence and seasonality, respectively; P and Q indicate seasonal autoregression and seasonal moving average terms, while s stands for both seasonal period and cycle length. SPSS 26.0 software was used for time-series analysis and time variables were defined.
Results
A total of 219,438 systemic prescriptions for GCs were included in the study. After excluding topical prescriptions, 219,276 remained and the top five were selected. Ultimately, 203,846 (92.89%) systemic GCs prescriptions were analyzed.
Figure 1 illustrates the trends in the number of systemic GCs prescriptions and IGR from January 2018 to December 2021. The trend in prescription quantity and inappropriate use remains consistent, with a significant increase in the number of systemic GCs prescriptions during the winter months, accompanied by a corresponding rise in inappropriate usage. January 2020 saw the highest number of systemic GCs prescriptions at 6488, followed closely by February 2019 with 6280.
 |
Figure 1 Change in the number of systemic glucocorticoids prescriptions and IGR from 2018 to 2021. |
Figure 2 illustrates the inappropriate rates of systemic GCs prescriptions in different months of each year from 2018 to 2021. The average IGR was 71.88% between 2018 and 2021, with a peak of 86.96% in January 2018. It was determined that January was the peak of inappropriate prescription, while August demonstrated the lowest occurrence.
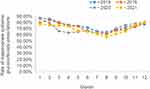 |
Figure 2 Monthly figure of rate of inappropriate systemic glucocorticoids prescriptions from 2018 to 2021. |
Table 1 presents the overall distribution of systemic GCs prescriptions stratified by diagnosis and rationality. Among all clinical diagnoses, diseases of the respiratory system (68.90%) and diseases of the skin and subcutaneous tissue (16.31%) were the most prevalent conditions for which these medications were prescribed. Among a total of 203,846 prescriptions, 73.18% exhibited inappropriate indications, while 0.05% demonstrated inappropriate selection. The utilization of systemic GCs was deemed inappropriate for diseases of the respiratory system (94.19%), followed by diseases of the digestive system (87.75%). The inappropriate rate of GCs prescriptions for acute upper respiratory infections at multiple and unspecified sites, acute tonsillitis, and acute bronchitis was as high as 100%. Unnecessary use of systemic GCs was prevalent in diseases of the digestive system and diseases of the circulatory system.
 |
Table 1 Distribution of Clinical Diagnoses and Appropriateness of Systemic Glucocorticoids Prescriptions |
Table 2 displays the distribution of systemic GCs prescriptions categorized by drug groups. The percentage of injectable and oral systemic GCs in total prescriptions was 90.84% and 9.16%, respectively. Dexamethasone (86.65%) is the most frequently prescribed systemic GCs in the injectable route. 75.38% of injectable systemic GCs and 51.95% of oral systemic GCs prescriptions were deemed inappropriate. Among injected systemic GCs, dexamethasone (77.40%) and methylprednisolone (73.45%) had higher rates of inappropriate use. The most frequent inappropriate indication of oral administration was prednisone (61.11%).
 |
Table 2 Distribution of Appropriateness of Systemic Glucocorticoids Use Categorized by Drug Type |
Table 3 summarizes the factors associated with inappropriate use of systemic GCs in univariate analysis. All variables demonstrated statistical significance in the univariate analysis (P < 0.001) and were therefore included in the multivariable model.
 |
Table 3 Factors Associated with Inappropriate Use of Systemic Glucocorticoids on Univariate Analysis |
Multivariate analysis revealed the factors associated with inappropriate systemic use of GCs, as presented in Table 4. Physicians, who were female or younger than 33 years old, possessed lower levels of education and professional titles and exhibited a higher likelihood of inappropriately prescribing systemic GCs. In addition, physicians with 21–40 years of experience exhibited a higher likelihood of inappropriately prescribing systemic GCs compared to those with less than 20 years or more. From the patient’s perspective, male patients over 65 years of age were more likely to receive inappropriate prescriptions for systemic GCs in 2021. Oral prescription and out-of-pocket prescriptions had the highest rate of inappropriate use.
 |
Table 4 Factors Predicting Inappropriate Use of Systemic Glucocorticoids on Multivariate Analysis |
Sarima
The original time-series plot in Figure 3 illustrates the monitoring data of IGR, which exhibited significant seasonality and certain periodic fluctuations that did not meet the requirements for sequence stationarity.
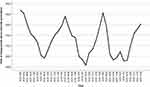 |
Figure 3 Timing plot of raw data on inappropriate rate of systemic glucocorticoids prescription. |
The timing chart depicting the IGR after first-order difference exhibited near-stationary (refer to Figure 4). As depicted in Figure 5, the residual ACF and PACF of the model exhibit no significant autocorrelation. Finally, the optimal model was determined as SARIMA (0, 1, 0) × (1, 1, 0)12, because it has the maximum R2 and the minimum BIC value. The model fitting with normalization yields a BIC value of −6.35 and an R2 coefficient of determination of 0.73. The Ljung–BoxQ test demonstrated a well-fitting model, as evidenced by the absence of statistical differences in the residuals (Q = 17.85, P = 0.40), indicating that they conformed to a white noise sequence.
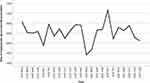 |
Figure 4 Sequence diagram of inappropriate rate of systemic glucocorticoids prescriptions after first difference. |
 |
Figure 5 Residuals ACF chart and residuals PACF chart of inappropriate rate of systemic glucocorticoids prescriptions after first-order difference. |
Evaluate the Performance of the Model
The dynamic trend of the predicted values in Figure 6 was basically consistent with the actual situation from January to December 2021. The actual value falls within the 95% confidence interval of the predicted value, indicating a high level of prediction accuracy for the SARIMA model.
 |
Figure 6 The SARIMA (0, 1, 0) × (1, 1, 0)12 model predicted results. |
Table 5 demonstrates the actual rate of monthly IGR is roughly consistent with the predicted rate. Compared to the actual value, the relative error falls within a range of 16%, with an average relative error of 8.40%. The SARIMA models were utilized to simulate and predict the monthly IGR in 2021, facilitating comprehension of the trend in such rates. Simultaneously, the predicted annual IGR trend was the same as the actual trend, with the peak of IGR in winter and the least in summer.
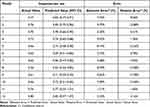 |
Table 5 Comparison of Actually Value and Predicted Value of Rate of Inappropriate Systemic Glucocorticoids Prescriptions in January–December, 2021 |
Discussion
In this retrospective study, we conducted an analysis of systemic GCs prescribing patterns and trends from 2018 to 2021 at 32 primary care institutions in Guizhou, China. The number of prescriptions for systemic GCs and the trend of inappropriate use were roughly consistent. 73.23% of prescriptions were deemed inappropriate use, with the majority (73.18%) being attributed to inappropriate indications, and inappropriate selection accounted for 0.05%. Physicians who possess lower levels of education and professional titles, under the age of 33, exhibit a greater propensity for inappropriate prescribing practices. After conducting model verification, it has been confirmed that the SARIMA model is suitable for predicting the monthly IGR of primary care institutions in southwest China.
As depicted in Figure 1, the changing trend of inappropriate systemic GCs prescription in each month was consistently correlated with the total systemic GCs prescription. This suggests that physicians who prescribe more systemic GCs are more likely to engage in inappropriate prescribing practices. Studies have indicated that excessive prescribing by physicians can elevate the likelihood of medical errors stemming from prescription inaccuracies or adverse reactions.30 On one hand, a higher volume of prescriptions may result in repeated prescriptions, drug interactions with high potential for harm, and long-term medication regimens.31 On the other hand, some physicians may feel compelled to meet patient expectations by issuing unnecessary or excessive prescriptions, thereby increasing the risk of inappropriate treatment. Therefore, it is necessary to enforce strict regulations on physicians’ prescribing behavior and enhance the management and review system for prescriptions.
As depicted in Figure 2, the IGR exhibits a significant increase during the winter season annually. The period is characterized by poor air quality and an elevation in atmospheric pollutants, which can result in respiratory illnesses among susceptible individuals. Studies have indicated that winter was associated with a heightened prevalence of acute upper respiratory tract infections.32 Therefore, the surge in diseases of the respiratory system during winter may serve as a primary contributing factor to the escalation of IGR.
Our study showed that up to 73.23% of systemic GCs were used inappropriately. In line with our prior research, a staggering 68.20% of systemic GCs prescriptions were deemed inappropriate.22 A separate study conducted in China revealed that 64.59% of GCs usage exceeded recommended indications, indicating a concerning trend towards inappropriate prescribing practices.33 According to a report from India, inappropriate use of systemic GCs is prevalent with 88.40% of cases being reported as such.34 In the United States, some primary care physicians prescribe systemic GCs without clear medical indications.35 A study conducted in China revealed that 42.20% of primary care physicians exhibited inadequate knowledge regarding hormone classification and contraindications.36 It can be inferred that the majority of primary care physicians possess inadequate knowledge regarding the indications for systemic GCs.
In Table 1, systemic GCs were predominantly prescribed for diseases of the respiratory system (68.90%), with 94.19% of these prescriptions being deemed inappropriate. Systemic GCs were not recommended for the treatment of acute respiratory infections, according to Centers for Disease Control and Prevention (CDC).37 In America, 23% of adult primary care visits for acute respiratory tract infections (ARTI) involved steroid injections.38 A cross-sectional study of outpatient departments of referral hospitals in Ethiopia found that 63.50% of glucocorticoids were used for respiratory diseases.39 In Puerto Rico, 75% prescriptions for patients diagnosed with the flu or common cold contained corticosteroids.40 A Korean study reported a 6.80% rate of steroid prescribing in respiratory infections.41 A previous study conducted in China revealed that physicians working in primary care institutions possessed limited knowledge regarding diseases of the respiratory system, with 65.1% being unaware of the most fundamental and crucial treatments for influenza.42 The findings of a randomized controlled trial (RCT) indicate that systemic GCs are ineffective in the treatment of lower respiratory tract infections.43 Previous research has also demonstrated the inefficacy of steroids in treating the common cold.41,44,45
In this study, inappropriate use of systemic GCs was found to be a common occurrence in the diseases of the digestive system (87.75%). One of the most prevalent manifestations is gingivitis and periodontal diseases, which aligns with the findings of Xiaobo Luo’s research.22 It should be emphasized that ICD-10 classify dental diseases into diseases of digestive system, and this study adopted ICD-10 as the standard for disease classification. Due to the potent anti-inflammatory effects of GCs, some clinicians may prescribe GCs directly for patients with pain caused by periodontitis without identifying the underlying cause. The primary etiology of periodontitis is oral bacterial infection, and the therapeutic approach should prioritize eradication of bacteria and reduction of inflammation in the oral cavity.46 Therefore, the use of GCs for periodontitis treatment is not recommended due to their potential adverse effects. Guidelines for Clinical Application of GCs in 2011 point out that GCs not only stimulate gastric acid secretion but also impair the protective function of gastric mucosa, thereby exacerbating pre-existing ulcers and potentially leading to severe complications such as gastrointestinal bleeding and perforation.20 Furthermore, the findings of a cohort study have substantiated an elevated risk of periodontal disease in asthmatic patients undergoing treatment with GCs, as compared to those who did not receive such therapy.47 Another review has demonstrated that systemic GCs therapy is associated with an increased susceptibility to developing periodontal disease.48
The findings of our study indicate that the rate of inappropriate utilization of systemic GCs in cases of acute upper respiratory tract infection (J06), acute bronchitis (J03), and acute tonsillitis (J20) is as high as 100%. Systemic GCs possess immunomodulatory and anti-inflammatory properties, making them a primary treatment option for upper respiratory tract infections.49 According to research, systemic GCs do not possess antiviral properties and are therefore an unsuitable treatment option for viral infections. In fact, the medication can compromise the body’s immune response and exacerbate the spread of infection.17,49 Therefore, the use of systemic GCs should not be a routine treatment for acute upper respiratory infections, acute bronchitis, and acute tonsillitis.
According to Table 2, the rate of GCs injection prescription (90.84%) is significantly higher than that of oral GCs prescription. In Ethiopia, injections account for 52.6% of systemic glucocorticoid prescriptions.39 According to a study conducted in the United States, it was found that clinicians administered injectable GCs more frequently than 40% of the time.38 One study revealed that in China, prescription rates of hormones and injections were significantly higher in economically disadvantaged western regions compared to their wealthier eastern counterparts.50 Due to a lack of awareness regarding the detrimental effects of misuse, it is commonplace for patients to request injections as a means of expediting their recovery from illness.51,52 According to related reports, 45.2% of physicians have encountered patients requesting unnecessary intravenous fluids.52 In addition, injection therapy can generate additional revenue for medical institutions and physicians themselves, which may contribute to the excessive use of injectable GCs by physicians.51,53 Excessive use of injected GCs not only escalates health-care expenses but also heightens the likelihood of eliciting severe adverse reactions and transmitting various blood-borne infections.54 Therefore, enhancing the health literacy of rural residents, strengthening drug regulation, and optimizing the allocation of medical resources are pivotal to addressing this issue.
In our study, more than half of injected (75.38%) and oral (51.95%) GCs were inappropriately used. In our previous study, 70.5% of injected GCs and 49.1% of oral GCs were inappropriately used.22 In the United States, 22.5% of patients received intramuscular GCs for acute upper respiratory infections.55 A study in China has shown that 16.53% of oral GCs were used for inappropriate indications.56 After the implementation of the Guidelines for Clinical Application of GCs, the clinical utilization of GCs in economically developed cities in China has become more rationalized. However, inadequate implementation of relevant management measures in less developed areas of southwest China still leads to prominent inappropriate use of GCs.19 We conclude that the safety and effectiveness of GCs in clinical treatment in primary care institutions deserve attention. A strict understanding of indications and contraindications is recommended prior to the clinical application of GCs, followed by the selection of a rational treatment plan based on the nature and characteristics of the diseases.49
In Table 4, the results of the multivariate analysis presented indicate that younger physicians (below the age of 33) and those holding lower professional titles (resident physicians) demonstrate an increased propensity for prescribing inappropriate systemic GCs. The majority of them only possess junior college degrees, which results in a lack of relevant professional knowledge and insufficient clinical experience. A study has revealed that junior physicians exhibit a twofold increase in the likelihood of making prescribing errors compared to their senior physicians.57 It has been reported that primary care institutions in Southwest China have grassroots health service personnel who generally hold low professional titles and have not received sufficient professional education.58 Therefore, it is imperative to enhance the continuous education of primary care physicians and elevate their overall literacy level. The proposal by Zhan suggests the adoption of blended learning as a means to provide targeted and continuous training for primary care physicians, with the aim of enhancing their professional skills.59 Rashid L Bashshur proposed the adoption of telemedicine-based diagnostic assistance systems to deliver high-quality medical services to rural populations.60
This study has demonstrated that inappropriate systemic GCs use was also associated with patient age. Inappropriate prescriptions are more prevalent among older patients, particularly those aged 65 and above. A study conducted in the United Kingdom investigated prescribing errors in primary care, and found that both patients aged 65 or above and under 15 years were at highest risk.57 Studies have demonstrated that patients with comorbidities tend to receive a higher number of prescribed medications, thereby resulting in an escalation of inappropriate prescriptions and the occurrence of adverse drug reactions.61 The current prevalence of multimorbidity among individuals aged 50 and above stands at 42.4%.62 In rural areas of China, the proportion of individuals aged 65 and above has reached 13.82%, surpassing that of urban areas by a significant margin. Due to economic and geographical factors, the majority of elderly individuals residing in rural areas opt to seek medical attention at the nearest primary care institution.63 In the United States, there is a lack of awareness among most primary care physicians regarding potentially inappropriate prescribing (PIP) for elderly patients and a limited understanding of prescribing guidelines.64 There are reports in China that 46.53% of primary care physicians have reported a lack of specialized training in geriatric pharmacotherapy, which often leads to excessive and inappropriate prescribing practices due to their inadequate knowledge in this area.61,65,66 Furthermore, the elderly themselves may contribute to inappropriate prescribing practices. In rural China, the elderly generally have limited educational attainment, resulting in low health literacy and inadequate knowledge of medication.65,67 Simultaneously, the elderly population acquires a lesser amount of knowledge regarding the prevention of adverse drug reactions.68 Therefore, it is imperative to enhance the specialized training of primary care physicians in rational drug utilization for elderly patients, while concurrently providing the elderly population with education and awareness on appropriate medication use.69
As a classical time-series model, the SARIMA model effectively captures both cyclical and seasonal variations.70 At present, the SARIMA model has been extensively utilized for predicting future patient visit rates and disease incidence.70–73 In our study, the SARIMA(0, 1, 0)×(1, 1, 0)12 model accurately predicted the IGR with an average error of only 8.40%. As predicted by our model (Figure 6), winter is the peak of inappropriate systemic GCs prescribing. Therefore, the SARIMA model established in this study can be utilized for early prediction and warning of monthly IGR in primary care institutions in Southwest China. This will enable relevant departments to timely formulate and implement countermeasures to reduce such abuse occurrences. It should be emphasized that a prediction model established through a single analysis cannot serve as a permanent prediction tool, and it can only be utilized for short-term predictions.70 In practice, it is essential to gather sufficient time-series data for validating the established model with new actual values and continuously incorporating fresh actual values to enhance the prediction model of IGR that can accurately reflect real-world scenarios.71
There are some limitations in this study. Firstly, the data presented in this study are limited to southwest China and therefore cannot be considered representative of systemic GCs usage across all primary care institutions throughout the country. Nevertheless, reproduction of the study in regions with comparable conditions remains feasible. Secondly, the study spans a significant period and necessitated primary care physicians to maintain uninterrupted employment at the same institution for more than 4 years. However, due to the high attrition rate of physicians in primary care institutions, our sample size was constrained. Thirdly, due to the limited time span, this study only verified that SARIMA model has a good short-term prediction ability of IGR in southwest China. In order to enhance the long-term prediction of IGR in southwest China, the data in future studies should be regularly updated and the model recalibrated.
Conclusion
The inappropriate use of systemic GCs remains a significant concern in primary care institutions. The use of GCs without appropriate indications is particularly prominent in diseases of the respiratory system. The primary factors contributing to the issue of inappropriate systemic GCs use were the relatively low professional titles and educational levels of physicians, as well as their limited professional knowledge and clinical experience in this specific area. In this regard, the continuing education and professional knowledge training of physicians should be strengthened in the future. The SARIMA model can facilitate early prediction and warning of monthly IGR in primary care institutions located in southwest China, thereby enabling relevant departments to develop timely countermeasures.
Abbreviations
GCs, glucocorticoids; HIS, Hospital Information System; LWTC, Lianke Weixin Technology Co., LTD.; ICGPHC, Information Center of Guizhou Provincial Health Commission; IGR, rate of inappropriate systemic GCs prescriptions; GEE, Generalized estimation equation; SARIMA, Seasonal auto-regressive integrated moving average; ADF, Augmented Dickey-Fuller; ACF, Autocorrelation function; PACF, Partial autocorrelation; R2, Determination coefficient; BIC, Bayesian information criterion; NCMS, New rural cooperative medical system; OR, Odds ratio; CI, Confidence interval; CDC, Centers for Disease Control and Prevention; ARTI, Acute respiratory tract infections; RCT, Randomized controlled trial; PIP, Potentially inappropriate prescribing.
Data Sharing Statement
The original contributions presented in the study are included in the article/Supplementary Materials, and further inquiries can be directed to the corresponding authors.
Acknowledgments
We express our gratitude to all the participating institutions for providing comprehensive information and indispensable assistance throughout this research. The authors also express their gratitude to all members of the investigational team for their diligent efforts in collecting the data. We would also like to acknowledge Edward McNeil, from Prince of Songkla University, Thailand, for his insightful feedback on improving this manuscript.
Author Contributions
All authors made a significant contribution to the research, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by the Natural Science Foundation of Guizhou Province, “Feedback intervention model of Gradient Boosting Decision Tree (GBDT) technology on glucocorticoid prescription control in primary care institutions” (Guizhou Science and Technology Foundation – ZK [2021] General 499). This research was also supported by the Medical Economics and Management Research Center of Guizhou Medical University (GMUMEM2022-A05).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chast F. Histoire de la corticothérapie. Rev Med Interne. 2013;34(5):258–263. doi:10.1016/j.revmed.2012.12.009
2. Barnes PJ. Glucocorticoids. Chem Immunol Allergy. 2014;100:311–316. doi:10.1159/000359984
3. Adcock IM, Mumby S. Glucocorticoids. Handb Exp Pharmacol. 2017;237:171–196. doi:10.1007/164_2016_98
4. Strehl C, Ehlers L, Gaber T, Buttgereit F. Glucocorticoids—all-rounders tackling the versatile players of the immune system. Front Immunol. 2019;10:1744. doi:10.3389/fimmu.2019.01744
5. Petta I, Dejager L, Ballegeer M, et al. The interactome of the glucocorticoid receptor and its influence on the actions of glucocorticoids in combatting inflammatory and infectious diseases. Microbiol Mol Biol Rev. 2016;80(2):495–522. doi:10.1128/MMBR.00064-15
6. Oray M, Abu Samra K, Ebrahimiadib N, Meese H, Foster CS. Long-term side effects of glucocorticoids. Expert Opin Drug Saf. 2016;15(4):457–465. doi:10.1517/14740338.2016.1140743
7. Rice JB, White AG, Scarpati LM, Wan G, Nelson WW. Long-term systemic corticosteroid exposure: a systematic literature review. Clin Ther. 2017;39(11):2216–2229. doi:10.1016/j.clinthera.2017.09.011
8. Fardet L, Petersen I, Nazareth I. Common infections in patients prescribed systemic glucocorticoids in primary care: a population-based cohort study. PLoS Med. 2016;13(5):e1002024. doi:10.1371/journal.pmed.1002024
9. Mebrahtu TF, Morgan AW, West RM, Stewart PM, Pujades-Rodriguez M. Oral glucocorticoids and incidence of hypertension in people with chronic inflammatory diseases: a population-based cohort study. CMAJ. 2020;192(12):E295–E301. doi:10.1503/cmaj.191012
10. Compston J. Glucocorticoid-induced osteoporosis: an update. Endocrine. 2018;61(1):7–16. doi:10.1007/s12020-018-1588-2
11. Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: A comprehensive review: Gastrointestinal and endocrinologic side effects. J Am Acad Dermatol. 2017;76(1):11–16. doi:10.1016/j.jaad.2016.02.1239
12. Fardet L, Petersen I, Nazareth I. Prevalence of long-term oral glucocorticoid prescriptions in the UK over the past 20 years. Rheumatology. 2011;50(11):1982–1990. doi:10.1093/rheumatology/ker017
13. Bénard-Laribière A, Pariente A, Pambrun E, Bégaud B, Fardet L, Noize P. Prevalence and prescription patterns of oral glucocorticoids in adults: a retrospective cross-sectional and cohort analysis in France. BMJ Open. 2017;7(7):e015905. doi:10.1136/bmjopen-2017-015905
14. Mathew S, Finny P, Samuel Johnson AK, et al. Evaluation of glucocorticoids utilization in central Kerala using pharmacy sales overview. Indian J Endocrinol Metab. 2021;25(6):516–519. doi:10.4103/ijem.ijem_439_21
15. Mulavelil R, Finny P, David A, Samuel PS, Armstrong LJ. Glucocorticoid use and misuse in a rural community of Kerala, India. Indian J Endocrinol Metab. 2022;26(3):234–238. doi:10.4103/ijem.ijem_430_21
16. Waljee AK, Rogers MA, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ Open. 2017;357:j1415. doi:10.1136/bmj.j1415
17. Li J, Jiang L, Li RB. Analysis about use of glucocorticoid drug in inpatients of our hospital in 2017. China Medical Herald. 2018;15(15):162–164+173.
18. Liu LM, Yu XG, Huang MY, et al. Review on prescriptions of essential medicines in 27 township hospitals in Jiangxi Province. Pharmac Rev. 2014;33(06):811–814.
19. Zhang JX, Xiong SJ, Xu C, et al. Investigation on the use of systemic glucocorticoids in 271 medical institutions in Guizhou Province. Chin J Hospital Pharm. 2020;40(02):219–224.
20. Standards for hospital prescription review and management (2010); 2022. Available from: http://www.nhc.gov.cn/wjw/ywfw/201306/094ebc83dddc47b5a4a63ebde7224615.shtml.
21. Guidelines for clinical application of glucocorticoids (2011); 2022. Available from: http://www.nhc.gov.cn/yzygj/s3585u/201102/91566d6e98df4916b8aa018e37605603.shtml.
22. Luo X, Yu S, Zeng Z, et al. Systemic glucocorticoid prescriptions pattern and factors of inappropriate use in primary care institutions of Southwest China. Front Public Health. 2022;10(10):952098. doi:10.3389/fpubh.2022.952098
23. Joseph RM, Hunter AL, Ray DW, Dixon WG. Systemic glucocorticoid therapy and adrenal insufficiency in adults: a systematic review. Semin Arthritis Rheum. 2016;46(1):133–141. doi:10.1016/j.semarthrit.2016.03.001
24. Shah P, Kalra S, Yadav Y, et al. Management of glucocorticoid-induced hyperglycemia. Diabetes Metab Syndr Obes. 2022;15:1577–1588. doi:10.2147/DMSO.S330253
25. Fardet L, Nazareth I, Petersen I. Long-term systemic glucocorticoid therapy and weight gain: a population-based cohort study. Rheumatology. 2021;60(3):152–1511. doi:10.1093/rheumatology/keaa289
26. Chalitsios CV, Shaw DE, McKeever TM. A retrospective database study of oral corticosteroid and bisphosphonate prescribing patterns in England. NPJ Prim Care Respir Med. 2020;30(1):5. doi:10.1038/s41533-020-0162-6
27. Einarsdottir MJ, Ekman P, Trimpou P, Olsson DS, Johannsson G, Ragnarsson O. High prescription rate of oral glucocorticoids in children and adults: a retrospective cohort study from Western Sweden. Clin Endocrinol. 2020;92(1):21–28. doi:10.1111/cen.14114
28. Lin KJ, Dvorin E, Kesselheim AS. Prescribing systemic steroids for acute respiratory tract infections in United States outpatient settings: a nationwide population-based cohort study. PLoS Med. 2020;17(3):e1003058. doi:10.1371/journal.pmed.1003058
29. World Health Organization. International Statistical classification of diseases and related health problems 10th revision (ICD-10)-2014-WHO version for 2014. Geneva, Switzerland: World Health Organization; 2014. Available from: http://apps.who.int/classifications/icd10/browse/2014/en#/X.
30. Guan X, Ni B, Zhang J, et al. Association between physicians’ workload and prescribing quality in one tertiary hospital in China. J Patient Saf. 2020;17(8):e1860–e1865. doi:10.1097/PTS.0000000000000753
31. Lillis S, Lord H. Repeat prescribing--reducing errors. J Prim Health Care. 2011;3(2):153–158. doi:10.1071/HC11153
32. Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol. 2020;7(1):83–101. doi:10.1146/annurev-virology-012420-022445
33. Luo YH, Yuan XB, Huang HW, Zeng CM. Analysis of the application of glucocorticoids in pediatric outpatient department of a hospital in 2012. Chin Pharm. 2014;25(18):1656–1658.
34. Masih S, Cynthia Stephen S, Joy Armstrong L, Finny P. Use and misuse of glucocorticoids in the community of Raxaul Block, North Bihar. Trop Doct. 2015;45(2):68–72. doi:10.1177/0049475514567756
35. Dvorin EL, Ebell MH. Short-term systemic corticosteroids: appropriate use in primary care. Am Fam Physician. 2020;101(2):89–94.
36. He J, Long XD, Pu YF, Zhang J. Investigation and analysis of cognition and application about antibiotics and glucocorticoids among rural doctors in Yunnan province. Chin Pharm. 2016;27(03):299–302.
37. Adult Treatment Recommendations CDC. Adult Treatment Recommendations (2017); 2023. Available from: https://wwwcdcgov/antibioticuse/community/for-hcp/outpatient-hcp/adult-treatment-rechtml.
38. Dvorin EL, Lamb MC, Monlezun DJ, Boese AC, Bazzano LA, Price-Haywood EG. High frequency of systemic corticosteroid use for acute respiratory tract illnesses in ambulatory settings. JAMA Intern Med. 2018;178(6):852–854. doi:10.1001/jamainternmed.2018.0103
39. Wondmkun YT, Ayele AG. Assessment of prescription pattern of systemic steroidal drugs in the outpatient department of Menelik ii referral hospital, Addis Ababa, Ethiopia, 2019. Patient Prefer Adherence. 2021;15:9–14. doi:10.2147/PPA.S285064
40. Quevedo J, Marsh W, Yulfo J, Alvarez O, Felici M, Rojias ME. Prescribing patterns and safety of mezclitas for respiratory illnesses. P R Health Sci J. 2012;31(3):138–144.
41. Kim T, Do YK. Prescription of systemic steroids for acute respiratory infections in Korean outpatient settings: overall patterns and effects of the prescription appropriateness evaluation policy. J Prev Med Public Health. 2020;53(2):82–88. doi:10.3961/jpmph.19.090
42. Pan Z, Yang T, Chi C, et al. An online survey of primary care physicians’ knowledge of common respiratory diseases in China. NPJ Prim Care Respir Med. 2022;32(1):28. doi:10.1038/s41533-022-00289-5
43. Hay AD, Little P, Harnden A, et al. Effect of oral prednisolone on symptom duration and severity in nonasthmatic adults with acute lower respiratory tract infection: a randomized clinical trial. JAMA. 2017;318(8):721–730. doi:10.1001/jama.2017.10572
44. Hayward G, Thompson MJ, Perera R, Del Mar CB, Glasziou PP, Heneghan CJ. Corticosteroids for the common cold. Cochrane Database Syst Rev. 2015;2015(10):CD008116. doi:10.1002/14651858.CD008116.pub3
45. Fashner J, Ericson K, Werner S. Treatment of the Common Cold in Children and Adults. Am Fam Physician. 2012;86(2):153–159.
46. Slots J. Periodontitis: facts, fallacies and the future. Periodontol 2000. 2017;75(1):7–23. doi:10.1111/prd.12221
47. Shen TC, Chang PY, Lin CL, et al. Risk of periodontal disease in patients with asthma: a nationwide population-based retrospective cohort study. J Periodontol. 2017;88(8):723–730. doi:10.1902/jop.2017.160414
48. Brasil-Oliveira R, Áa C, Sarmento VA, Souza-Machado A, Lins-Kusterer L. Corticosteroid use and periodontal disease: a systematic review. Eur J Dent. 2020;14(03):496–501. doi:10.1055/s-0040-1713954
49. Yang SJ. Analysis on the application of glucocorticoid prescription in outpatient department of our hospital from 2015 to 2016. Chin Mod Drug Appl. 2019;13(01):155–156.
50. Li Y, Xu J, Wang F, et al. Overprescribing in China, driven by financial incentives, results in very high use of antibiotics, injections, and corticosteroids. Health Aff. 2012;31(5):1075–1082. doi:10.1377/hlthaff.2010.0965
51. Jiang Q, Yu BN, Ying G, et al. Outpatient prescription practices in rural township health centers in Sichuan Province, China. BMC Health Serv Res. 2012;12:324. doi:10.1186/1472-6963-12-324
52. Wu D, Lam TP, Lam KF, Zhou XD, Sun KS. Doctors’ views of patient expectations of medical care in Zhejiang Province, China. Int J Qual Health Care. 2017;29(6):867–873. doi:10.1093/intqhc/mzx119
53. Li X, Krumholz HM, Yip W, et al. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–1812. doi:10.1016/S0140-6736(20)30122-7
54. Zhang Y. The study on the harmfulness, causes and control strategies overuse of injections in the primary medical institutions in Rural Areas of China. Chin Prim Health Care. 2010;24(05):3–6.
55. Parsel SM, Mohammed AE, Fort D, Barton BM, McCoul ED. Intramuscular corticosteroids for acute upper respiratory infections affects healthcare utilization. Ann Otol Rhinol Laryngol. 2020;129(10):988–995. doi:10.1177/0003489420929717
56. Tang Y, Shang N, Du X, Zhang YX, Wang DZ. Evaluation of off-label use of oral glucocorticoids in outpatients. Acta Acad Med Sin. 2015;37(4):430–434. doi:10.3881/j.issn.1000-503X.2015.04.011
57. Ashcroft DM, Lewis PJ, Tully MP, et al. Prevalence, nature, severity and risk factors for prescribing errors in hospital inpatients: prospective study in 20 UK Hospitals. Drug Saf. 2015;38(9):833–843. doi:10.1007/s40264-015-0320-x
58. Liang S, Deng H, Liu S, et al. Competency building for lay health workers is an intangible force driving basic public health services in Southwest China. BMC Health Ser Res. 2019;19(1):596. doi:10.1186/s12913-019-4433-2
59. Zhan X, Zhang Z, Sun F, et al. Effects of improving primary health care workers’ knowledge about public health services in rural China: a comparative study of blended learning and pure E-learning. J Med Internet Res. 2017;19(5):e116. doi:10.2196/jmir.6453
60. Bashshur RL, Howell JD, Krupinski EA, Harms KM, Bashshur N, Doarn CR. The empirical foundations of telemedicine interventions in primary care. Telemed J E Health. 2016;22(5):342–375. doi:10.1089/tmj.2016.0045
61. Lavan AH, Gallagher PF, O’Mahony D. Methods to reduce prescribing errors in elderly patients with multimorbidity. Clin Interv Aging. 2016;11:857–866. doi:10.2147/CIA.S80280
62. Yao SS, Cao GY, Han L, et al. Prevalence and patterns of multimorbidity in a nationally representative sample of older Chinese: results from the China health and retirement longitudinal study. J Gerontol a Biol Sci Med Sci. 2020;75(10):1974–1980. doi:10.1093/gerona/glz185
63. Sun X, Meng H, Ye Z, Conner KO, Duan Z, Liu D. Factors associated with the choice of primary care facilities for initial treatment among rural and urban residents in Southwestern China. PLoS One. 2019;14(2):e0211984. doi:10.1371/journal.pone.0211984
64. Ramaswamy R, Maio V, Diamond JJ, et al. Potentially inappropriate prescribing in elderly: assessing doctor knowledge, confidence and barriers. J Eval Clin Pract. 2011;17(6):1153–1159. doi:10.1111/j.1365-2753.2010.01494.x
65. Lin JJ, Huang WL. Investigation and analysis on medicine usage of the elderly in the rural areas of Fujian Province. J Nanjing Med Univ. 2016;16(02):105–110.
66. Leviatan I, Oberman B, Zimlichman E, Stein GY. Associations of physicians’ prescribing experience, work hours, and workload with prescription errors. J Am Med Inform Assoc. 2021;28(6):1074–1080. doi:10.1093/jamia/ocaa219
67. Xie Y, Ma M, Zhang Y, Tan X. Factors associated with health literacy in rural areas of Central China: structural equation model. BMC Health Serv Res. 2019;19(1):300. doi:10.1186/s12913-019-4094-1
68. Kim M, Suh D, Barone JA, Jung SY, Wu W, Suh DC. Health literacy level and comprehension of prescription and nonprescription drug information. Int J Environ Res Public Health. 2022;19(11):6665. doi:10.3390/ijerph19116665
69. Moure-Fernandez A, Hollinghurst S, Carroll FE, et al. Economic evaluation of the OSAC randomised controlled trial: oral corticosteroids for non-asthmatic adults with acute lower respiratory tract infection in primary care. BMJ Open. 2020;10(2):e033657. doi:10.1136/bmjopen-2019-033567
70. Wu WW, Li Q, Tian DC, et al. Forecasting the monthly incidence of scarlet fever in Chongqing, China using the SARIMA model. Epidemiol Infect. 2022;150:e90. doi:10.1017/S0950268822000693
71. Zhao D, Zhang H, Cao Q, Wang Z, Zhang R. The research of SARIMA model for prediction of hepatitis B in mainland China. Medicine. 2022;101(23):e29317. doi:10.1097/MD.0000000000029317
72. Mao Q, Zhang K, Yan W, Cheng C. Forecasting the incidence of tuberculosis in China using the seasonal auto-regressive integrated moving average (SARIMA) model. J Infect Public Health. 2018;11(5):707–712. doi:10.1016/j.jiph.2018.04.009
73. Liu J, Yu F, Song H. Application of SARIMA model in forecasting and analyzing inpatient cases of acute mountain sickness. BMC Public Health. 2023;23(1):56. doi:10.1186/s12889-023-14994-4
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
