Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Trends Analysis of HIV Infection and Antiretroviral Treatment Outcome in Amhara Regional from 2015 to 2021, Northeast Ethiopia
Authors Addisu T, Tilahun M , Wedajo S , Sharew B
Received 24 March 2023
Accepted for publication 30 June 2023
Published 4 July 2023 Volume 2023:15 Pages 399—410
DOI https://doi.org/10.2147/HIV.S411235
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Tseganew Addisu,1 Mihret Tilahun,2 Shambel Wedajo,3 Bekele Sharew2
1Department of Dental Medicine, School of Medicine, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia; 2Department of Medical Laboratory Sciences, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia; 3School of Public Health, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
Correspondence: Mihret Tilahun, Department of Medical Laboratory Science, College of Medicine and Health Sciences, Wollo University, PO. BOX: 1145, Dessie, Ethiopia, Tel +251- 920988307, Fax +251 333115250, Email [email protected]
Background: The persistent efforts of HIV/AIDS epidemiology remain one of the world’s most important community health threats. To avoid becoming an epidemic, UNAIDS has set three 90% fast-track targets for 2020, and Ethiopia has also changed its implementation since 2015. However, the achievement targets in the Amhara region have yet to be evaluated at the end of the programme period.
Objective: The aim of this study was to assess the Trends of HIV Infection and Antiretroviral Treatment outcome in Eastern Amhara Regional from 2015 to 2021, Northeast Ethiopia.
Methods: A retrospective study was conducted by reviewing the District Health Information System from 2015 to 2021. The collected data includes the trend of HIV testing services, the trend of HIV positivity, the yield of HIV testing approaches, the number of HIV positive patients linked to HIV care and treatment or access to lifelong antiretroviral therapy, viral load testing coverage, and viral suppression. A descriptive statistic and trend analysis were computed.
Results: A total of 145,639 people accessed antiretroviral therapy. The trend of HIV test positivity has been declining since 2015, peaking at 0.76% in 2015 and declining to 0.60% in 2020. A high level of positivity was reported in volunteer counselling and testing as compared with provider-initiated testing and counselling services. Following an HIV positive, there was an increase in linkage to HIV care and treatment. High suppression rates of viral load indicate testing coverage grew over time. The viral load monitoring coverage was 70% in 2021, with a viral suppression rate of 94%.
Conclusion and Recommendations: The trend in achievement in the first 90s was not consistent with predefined goals (90%). On the other hand, there was good achievement in the second and third goals. Hence, intensified case-finding approaches to HIV testing should be strengthened.
Keywords: HIV, antiretroviral treatment outcome, trends
Introduction
Viral load test is the preferred monitoring method for people living with HIV/AIDS (PLWHA) on antiretroviral therapy (ART). Monitoring viral load (VL) is used to assess the treatment progress, to detect treatment failure, and to assess transmission risk.1 Despite the persistent efforts to finish the HIV/AIDS epidemic, it remains one of the world’s most important public healthiness terrorizations and a target to the Sustainable Development Goal (SGD) 2030.2 The highlights of this report indicate the gradual decline in PLHIV that were estimated in 612,925 for the year 2021 to 609,349 for the year 2022, and also adult HIV new infection declined from 8772 to 8284 for the year 2021 and 2022, respectively.3 According to the Joint United Nations Programmed on HIV/AIDS (UNAIDS) report, 37.7 million people internationally were living with HIV in 2020, and Africa accounts for 25.5 million, of which eastern and southern Africa takes 80.7%. Regarding the incidence of HIV infection, globally there were around 1.5 million newly infected individuals, of which nearly a million occurred in Africa.4 Globally, in the year 2020 about 680, 000 people died from AIDS-related illnesses. Eastern and southern Africa accounts for half of the global AIDS-related deaths. Meanwhile, at the start of the widespread, 79.3 million [55.9 million–110 million] people have become infected with HIV and 36.3 million [27.2 million–47.8 million] people have died from AIDS-related illnesses. Globally, 28.2 million people living with HIV (PLHIV) were accessing antiretroviral therapy (ART) as of 30 June 2021.5
HIV medicines prevent HIV from multiplying (making copies of itself), reducing the amount of HIV in the body (known as the viral load). Less HIV in the body allows the immune system to recover and produce more CD4 cells.6 Reports showed after 12 months taking of ART, the virological suppression achievement was 80%. This is within the range of 71–84% of patients showing viral suppression after 12 months of ART.7,8
According to the Ethiopia Public Health Institute HIV estimate in 2020, 745,719 people living with HIV and 8426 annual deaths related to HIV/AIDS were reported.9,10 Similarly, according to the Ethiopian demographic and health Survey 2016 (EDHS 2016), in countrywide the HIV occurrence was 0.9%.11,12 The prevalence varies greatly by gender, geography, age, and socioeconomic status. In terms of the regional distribution of HIV estimation, the Amhara region is one of the highest-burden regions, with approximately 212,991 people living with HIV in 2020.13 Although the overall prevalence HIV/AIDS in Ethiopia’s is less than the epidemic threshold (1%) in eight regions, including Amhara, have a prevalence greater than 1% and are classified as HIV epidemic regions. In Ethiopia, 48,0000 HIV-positive people will have received antiretroviral therapy by 2020.14,15
In response to this epidemic, WHO declared three 90-90-90 fast-track targets to accomplish the Sustainable Development Goals (SDG) to end the epidemic of AIDS by 2030 within the context of confirming healthy lives and promoting well-being for all at all ages.16 In 2021, UNAIDS updated its fast-track targets to three: 95% of people living with HIV will know their HIV status; 95% of people who know their HIV status will receive antiretroviral therapy (ART), and 95% of those who receive ART will have viral suppression. In line with this, Ethiopia has endorsed the UNAIDS fast track targets by incorporating them into its National Strategic Plans (NSP) since 2015. The current Ethiopian National Strategic Plan (NSP) for HIV, 2021–2026, aims to achieve national HIV epidemic control by 2026, with new HIV infections and AIDS mortality rates of less than one per 10,000 people.17
In order to meet the predetermined goals, the World Health Organization (WHO) strengthen enhanced HIV testing service (HTS) and launched treat-all approach as a new treatment initiation criterion in 2016.1 Enhanced HIV case identification to achieve fist 90s or 95s has been implemented using different HIV testing modalities including volunteer counseling and testing (VCT) and provider-initiated testing and counseling (PITC) services. Then, the identified HIV positive cases will be linked to HIV care and treatment or will have access to lifelong antiretroviral therapy using rapid initiation approach (test and treat).18 This allows to achieve the second 90s or 95. In this new treatment approach, any HIV-positive client will initiate antiretroviral therapy regardless of CD4 cell count as well as the clinical stage of the disease. Previously, antiretroviral treatment was initiated based on the level of CD4 cell count and WHO clinical stages. Antiretroviral treatment will be started for HIV patients with a CD4 cell count of fewer than 500 cells/mm3 or in advanced clinical stages (Stage III or IV).19
The aims of antiretroviral therapy are to decrease viral load, improve CD4 cells, reduce the occurrence of opportunity infections, and improve overall health-related quality of life. Additionally, to suppress viral load less than 1000 copies/mL after first second-line antiretroviral therapy.20 In Ethiopia, viral load testing on the top 20 problematic areas began in 2016. The viral load test is considered the gold standard for monitoring treatment outcomes in HIV patients. As a result, 90% to 95% of those on ART are expected to achieve viral suppression.21
Despite the government of Ethiopia has already launched the 2nd HIV/AIFDS national strategic plan of Ethiopia (2021–2025), there is gap of treat-all approach and launching viral load testing as routine monitoring treatment outcomes, the progress towards achieving the three 90s was not evaluated in Amhara regional state perspectives. Knowing the current progress allows to craft appropriate action points for the achievement of three 95% the next five years as well as serve as baseline data for later comparison. Hence, the aim of this study was to assess the trends of HIV infection and antiretroviral treatment outcomes in Eastern Amhara Regional state from 2015 to 2021 from District Health information system (DHIS-2).
Methods
Study Area, Period and Setting
This study was carried out in Amhara regional state, Ethiopia. The Amhara Region is located in the northwestern part of Ethiopia between 8° 45’ and 13° 45’ North latitude and 36° 20’ and 40° 20’ East longitude. It has an estimated land area of 17.7 million square kilometers. Amhara is bordered to the north by Tigray Region, to the east by Afar, to the south by Oromia, to the southwest by Benishangul-Gumiz, and to the west by Sudan. Amhara is divided into 13 zones, each with eight town administrations. Agew Awi, East Gojjam, the Oromia specialty zone, North Gondar, North Shewa, North Wollo, South Gondar, South Wollo, Wag Hemra, West Gojjam, West Gondar, Welkayit Tegeda Setit Humera, and Central Gondar are some of these zones. By 2022, those zones, or the Amhara region, are expected to have a population of 23,115,999 people.
The HIV data was held by SMART care, the ART logbook, and the chronic ART follow-up form and reported in DHIS-2. Following each clinical appointment, these registries are updated. Every facility in the country uses the same documentation and reporting system. HIV patients are scheduled every three months in the COVID-19 era. At each appointment, patients will be evaluated for nutritional status, opportunistic infections, medication adherence, drug side effects, and the need to refill ART and other preventative medications.
Study Design and Data Collection
A retrospective study was carried out by reviewing the district health information system (DHIS-2) in the Amhara region from 2015 to 2021. Data on the trend of HIV testing services, the trend of HIV positivity, the yield in various HIV testing approaches, the number of HIV positive patients were linked to HIV care and treatment or access to lifelong ART, viral load testing coverage, and viral suppression were collected.
Source and Study Population
All clients who were diagnosed as HIV positive and HIV patients who have been receiving second-line antiretroviral therapy from 2015 to 2021 were considered as a source population for the trend analysis of antiretroviral treatment access, and those clients who were initiated antiretroviral treatment during the study period were considered as a source population for the trend assessment of viral load test coverage and viral re-suppression status.
Eligibility Criteria
All clients who experienced HIV testing service were enrolled in HIV care and treatment, and who had viral load records or tested were included in this study. All collected data in DHIS-2 during the study period were included.
Variables and Measurement
Number of HIV testing services (VCT and PITC approaches), Trend of HIV positivity and overall yield, Trend of HIV positive linkage or enrollment to HIV care and treatment, Trend of viral load coverage and viral suppression. Viral re-suppression or low viremia level is defined as having a viral load quantity under 1000 copies/mL at least six-month taking to second-line antiretroviral therapy.22
Data Collection Procedures
Standardized checklist was used to collect and extraction by reviewing regional District health information system (DHIS-2). DHIS2 is an open source, platform with web-based that commonly used as a health management information system (HMIS). Accordance with the national consolidated antiretroviral guideline the extraction sheet was created in.23
Data Quality Assurance
To confirm the data’s quality, the following steps were taken: Data collectors were trained on the purpose of the study, the content of the check list, and how to gather the necessary data over a two-day period. To ensure data quality, the extraction sheet was pre-tested on a head of the actual study. The data collection procedures were carefully monitored, and feedback was provided on site. In accordance with Ethiopia’s antiretroviral treatment guidelines, the extraction sheet was written in English. The checklist will be pretested, and any necessary changes will be made. Furthermore, data were collected by triangulating three data sources: the ART registration book, the follow-up card, and the ART database, to reduce data incompleteness. The data were entered into the Epidata Version 4.0.06 software package, and templates were programmed using Epidata check codes. Furthermore, exploratory data analysis will be carried out and possible errors managed.
Data Processing and Management
After data gathering, the completeness of the checklist was checked and entered into the Epi-Data Version 4.0.0.6 software package. The data were exported to Statistical Package for Social Science Version 25 statistical software as well as Stata Version 14 for further investigation. Exploratory data analysis was conducted in order to check possible errors, assumptions, and computing, transformation, or recoding prior to actual data analysis.
Data Analysis
A descriptive statistic was computed to describe the trend of the proposed objectives. For categorical variables, frequency and percent were computed and presented in a table and graph. For a continuous variable, first Kolmogorov–Smirnov and Shapiro–Wilk tests were used to check the distributional assumptions. The mean with standard deviation (SD) and median (interquartile range, IQR) were employed to check normally and skewedly distributed of continuous variables, respectively. Trend analysis was computed to see how the longitudinal trend changed across the proposed objectives.
Ethical Considerations
This study was conducted according to the Helsinki Declaration. The Ethical Review Board of Wollo University was granted ethical approval. Permission was also obtained from the respective zonal health departments. The informed consent was waived because we used document review as a data source. Besides, to keep the data private, anonymous techniques were employed throughout the research process.
Results
Study Description
This study reviewed HIV data (DHIS-2) for the Amhara region from 2015 to 2021. During the last observation period of 2021, a total of 145,639 people accessed antiretroviral therapy, of which more than 90% were adults aged greater than 14 years old. The trend of ART coverage was shown to have an improved pattern; from 113,992 in 2015 to 145,639 in 2021. The following are the yearly trends of HTS, access to ART or linkage to care and treatment, viral load suppression rate, and the trend of three 90s achievement. The trend of ART treatment access had shown a significant improvement as you moved from 2015 to 2021. During 2016 there were significant improvements in enrolment to HIV care and treatment (Table 1 and Figure 1).
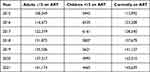 |
Table 1 Antiretroviral Treatment (ART) Coverage in Amhara Regional State, from 2015 to 2021 |
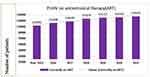 |
Figure 1 Trend of Antiretroviral treatment (ART) coverage in Amhara regional state, from 2015 to 2021. |
Trend of HIV Testing and Counselling (HTC) Services
From 2015 to 2021, there was a general trend of declining HTC service coverage. Both volunteer counseling and testing (VCT) and provider-initiated testing and counseling (PITC) service coverage also showed a downward trend. With regard to the trend of HIV test positivity, or yield, it has been declining since 2015, peaking at 0.76% in 2015 and declining to 0.60% in 2020. The highest HIV positivity yield from HTS approaches was found in VCT, where the maximum yield was 1.03% in 2017 and the lowest was 0.71%. The lowest yield was displayed by PITC, while the greatest yield was 0.64% in 2017 (Table 2, Figures 2 and 3).
 |
Table 2 Trend of HIV Testing and Counselling (HTC) Services Coverage and Yields in the Amhara Region, 2015–2021 |
 |
Figure 2 Trend of HIV testing and counselling (HTC) services in the Amhara region, 2015–2021. |
 |
Figure 3 Trend of HIV positivity or yield in different HTC approaches in the Amhara region, 2015–2021. |
Linkage to Care and Treatment
The overall trend of linkage to care and treatment following HIV positive results has shown a slightly increased pattern since 2018. Similar to that, from 2015 and 2017 there was an increasing trend. The highest peak of linkage to care and treatment was observed in 2017 and the lowest was in 2015 (79%) (Table 3 and Figure 4).
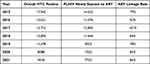 |
Table 3 Trend of Linkage to Care and Treatment Among Newly HIV Positive Clients in the Amhara Region, 2015–2021 |
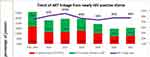 |
Figure 4 Trend of linkage to care and treatment among newly HIV positive clients in the Amhara region, 2015–2021. |
Viral Load Coverage and Suppression
High viral load suppression rates increased as viral load testing coverage grew over time. The viral load monitoring coverage surpassed 70% in 2021, with a total viral suppression rate of 94%. The viral load coverage has significantly improved since 2019. Prior to that, it was insufficient, with only 3 out of 10 PLHIV accessible for viral load testing services. The highest viral load suppression rate was observed in 2021 (94%), and the lowest was observed in 2015 (38%) (Table 4 and Figure 5).
 |
Table 4 Trend of Viral Load Coverage and Suppression in the Amhara Region, 2015–2021 |
 |
Figure 5 Trend of viral load coverage and suppression in the Amhara region, 2015–2021. |
Trend in the Achievement of Three 90s
Over the previous seven years, the first-90s achievement trend—which was around 71%—has not changed. This means, only seven out of ten HIV-positive individuals were knowing their positive HIV status during the last seven years of HTC service. Concerning the second 90s (ie, 90% of PLHIV accessed care treatment among those who recognize their HIV positive status), the highest peak of achievement was observed in 2017 and since then it has demonstrated a pattern of growth. Regarding the trend of the third 90s (ie, 90% of PLHV achieved viral suppression among those who were on antiretroviral therapy), there had been a remarkable improvement from 38% in 2015 to 94% in 2021 (Table 5 and Figure 6).
 |
Table 5 Trend in the Achievement of Three 90s in the Amhara Region from 2015–2021 |
 |
Figure 6 Trend in the achievement of three 90s in the Amhara region from 2015–2021. |
Discussion
This study designed to show the trend of HIV testing service utilization, linkage to care and treatment, viral load test coverage and viral suppression as well as three 90s achievement trends for the last six-year period in Amhara regional state.
The coverage of HTS has declined in the last six years in both the VCT and PITC approaches. In the current study both volunteer counseling and testing (VCT) and provider-initiated testing and counseling (PITC) service coverage also showed a downward trend. With regard to the trend of HIV test positivity, or yield, it has been declining since 2015, peaking at 0.76% in 2015 and declining to 0.60% in 2020. The highest HIV positivity yield from HTS approaches was found in VCT, where the maximum yield was 1.03% in 2017 and the lowest was 0.71%. The lowest yield was displayed by PITC, while the greatest yield was 0.64% in 2017. Similarly, research showed on the trend of yield or HIV positivity also shows a decrement pattern, which is consistent with the national level of HIV yield or positivity in 2017 and 2018.24 This result indicated that the emphasis on achieving the first 90% and screening for high-risk HIV testing services decreased over time. The other pertinent finding in this study was that the trend of positivity or yield was high in VCT as compared with PITC. The possible justification for the high HIV positive yield in the VCT service might be that positive clients may repeatedly visit VCT clinics after knowing their positive status for further confirmation. Besides, it might be clients who perceive a high risk of acquiring HIV infection and may visit HTS by self-initiation. On the other hand, the practice of PITC in routine care at numerous entrance points (inpatient, outpatient, TB and STI clinics, malnutrition, and postnatal clinics) lacks a screening focus, in which PITC services are offered in conjunction with risk screening services. Hence, this result implies that the implementation of the risk screening service for HIV testing was low or not implemented in accordance with the target screening guidelines.
In the current study, the trend of ART coverage was shown to have an improved pattern; from 113,992 in 2015 to 145,639 in 2021. The following are the yearly trends of HTS, access to ART or linkage to care and treatment, viral load decreasing rate, and the trend of three 90s achievement. The trend of HIV-positive clients being associated to care and treatment after discovering their positive status has improved over time. This is critical in meeting the second 90% goal, which states that 90% of positive clients should have access to HIV care and treatment. The Amhara region has made good progress toward the second 90-day goal. A large number of patients were enrolled in HIV care and treatment in 2017. This was due to Ethiopia’s full implementation of the new ARV treatment initiation criteria, particularly in the Amhara region. As a result, in 2017, all newly diagnosed HIV cases and all pre-ART cases received antiretroviral therapy.
The overall trend of linkage to care and treatment following HIV positive results has shown a slightly increased pattern since 2018. Similar to that, from 2015 and 2017 there was an increasing trend. The highest peak of linkage to care and treatment was observed in 2017 and the lowest was in 2015 (79%). Similarly, antiretroviral treatment adherence was positively correlated with the number of adherence counsellors. This finding is persistent with the findings of a multi-level study conducted in Cambodia.25 Adherence counsellors are formally assigned non-healthcare workers who provide adherence counselling, screening for psychiatry problem and substance use issues, tracing lost to follow-up cases, one-to-one counselling, and mass education about treatment and illness.26,27 As a result, in order to provide effective adherence counselling and other jobs, the number of adherence cohorts should grow in lockstep with the number of patients.
The magnitude of viral load test coverage was significantly improved in the last six-year period, in which it improved from 1.4% to 71.1%. Similarly, the viral load suppression rate also improved from 38% in 2015 to 94% in 2021. This finding was congruent with Ethiopian population-based HIV impact assessment result as well as the Amhara region had achieved the third 90 goal, in which among HIV patients who were taking ART, 90% of them should achieve viral suppression.28 The history of drug substitution is linked to viral re-suppression. Frequent first-line antiretroviral drug substitution reduces secondary treatment options and forces the reuse of previously substituted drugs. As a result, there will be an increased risk of drug resistance and failure to suppress viral load, particularly in areas where drug resistance testing has not yet been implemented during drug substitution. Backbone NRTIs are used in place of drugs from the same class that were previously used in first-line antiretroviral therapy.29,30
The overall trend of three 90s achievements showed that there was an increment pattern from year to year. However, the achievement of the first 90s (70% in 2021) was below the predetermined goal (90%) in Amhara regional state. Hence, for the next five years, to achieve 95% case identification, alternative HIV case finding strategies should be adopted and deeply implemented. However, the trend of second and third 90s achievement improved across time and achieved the predetermined goals. This achievement should be strengthened in the next five years to achieve the three 90. This study revealed that eight in ten HIV patients who were getting second-line antiretroviral therapy had achieved viral suppression.31 This result is inconsistent with studies conducted in resource-limited settings and is higher than a study conducted in South Africa. This variation is due to a classification difference in viral load measurement. Viral load quantities are below 400 copies/mL and 1000 copies/mL were used as cutoff points to define viral decrease in studies conducted in South Africa and the current study, respectively. In general, viral decrease in this study remains inconsistent with national and WHO/UNAIDS-set targets for viral suppression in 2030, which state that 95% of people on treatment will have suppressed viral load by 2026.32 Not accomplishing viral decreasing has both clinical and public health implications. Clinically, it increases the risk of drug resistance, second-line treatment failure, and demand for high-cost third-line antiretroviral therapy. Besides, at the community level, it also rises the chance of HIV transmission, even resistant strains.
Policy, Practice and Research Implication
The implementation of enhanced HIV case finding to achieve the first 90 was not low or the emphasis was decreased as time went by. The existing HCT service lacks identification of high-risk HIV clients. Hence, alternative and high-yield HIV testing services should be strengthened. High-yield case finding modalities include index case testing and partner notification, social network services, and PITC using an HIV risk screening tool at the health facilities. HIV positive cases from HTS cites have a good referral linkage, whether intra or inter-referral linkage. Having high viral suppression after initiation of ARV implies a significant number of HIV patients would have a better quality of life, immunological and clinical outcomes, as well as at a public level, it decreases the chance of HIV transmission even from mother to child after initiation of ARV.
Limitations of the Study
Retrospective design was used to analyze viral re-suppression, attrition, treatment failure, and death by reviewing multiple data sources, including chronic HIV follow-up forms (patient charts or cards), ART registration books, and the SMART care database. However, we were unable to collect and analyze information on behavioral, social, and psychological aspects, as well as clinical information such as organ function tests and drug 88 resistance testing. These limitations stemmed from the data gathering procedures, which involved reviewing medical records (document review). As a result, unmeasured covariate confounding must be taken into account when interpreting the reported associations.
Conclusion and Recommendations
Based on the result of this study, the following conclusions were made. The trend of HIV testing services and yield of positive results decreased across time in the Amhara region during the last six years. The VCT service had shown a better trend yield than that of the PITC service. The linkage of HIV positive cases to HIV care and treatment has an improved pattern across time. In the last six years, there has been a significant improvement in viral load coverage and suppression rates. The achievement of first-90 in the last six-year period was stagnant or had not shown any change, ARV treatment access and viral suppression had improved, as well as achieved the predetermined goals of the second and third-90s. The following recommendations were made based on the result of this study. Alternative molecular testing HIV testing modalities should promptly adopt and implemented in order to improve the achievement of first-90 or improve HIV case finding, the implantation of targeted HIV testing service using high risk identification tools should be enhanced in order to improve yield of PITC service, The viral load testing coverage service should also improve well.
Abbreviations
ART, Antiretroviral Therapy; DHIS-2, District Health Information System; EDHS, Ethiopian Demographic and Health Survey 2016; FMoH, Federal Ministry of Health; HTS, HIV testing and counselling Service; IQR, Interquartile Range; NSP, National Strategic Plan; PITC, Provider-Initiated Testing and Counseling; PLHIV, People Living with HIV; SD, Standard Deviation; SDG, Sustainable Development Goal; VCT, Volunteer Counseling and Testing; WHO, World Health Organization.
Data Sharing Statement
All data to the conclusions of this article are within the manuscript.
Acknowledgment
First and foremost, we would like to thank Wollo University, College of Medicine and Health Science for providing this research opportunity and financial support. We would like to extend our acknowledgement to Amhara regional health bureau and respective zonal departments, for their unreserved support for successful completion of this research work.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No external funds were obtained; only institutional support from Wollo university.
Disclosure
The authors state that they have no conflicts of interest in this research work.
References
1. World Health Organization. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach. World Health Organization; 2016.
2. Sarin N, Balakrishna P. Achieving the Sustainable Development Goal on Health (SGD 3). India: FLEDGE, India; 2018.
3. Wang Y, Kiwuwa-Muyingo S, Kadengye DT. Understating the barriers to achievement of the UNAIDS 90–90–90 goal in Tanzania using a population-based HIV impact assessment survey 2016–2017. AIDS Care. 2022;34(6):797–804. doi:10.1080/09540121.2021.1923631
4. Modi RA. HIV Disclosure, Retention in HIV Care, and Viral Load Suppression: A Study Among New to HIV Care Patients. The University of Alabama at Birmingham; 2018.
5. Heath K, Levi J, Hill A. The Joint United Nations Programme on HIV/AIDS 95–95–95 targets: worldwide clinical and cost benefits of generic manufacture. AIDS. 2021;35(1):S197–S203. doi:10.1097/QAD.0000000000002983
6. Viktor P. Effective AIDS treatment with resonance medicine. World J AIDS. 2022;12(2):111–119. doi:10.4236/wja.2022.122009
7. McMahon JH, Elliott JH, Bertagnolio S, Kubiak R, Jordan MR. Viral suppression after 12 months of antiretroviral therapy in low-and middle-income countries: a systematic review. Bull World Health Organ. 2013;91(5):377–385. doi:10.2471/BLT.12.112946
8. Zhou J, Sirisanthana T, Kiertiburanakul S, et al. Trends in CD4 counts in HIV-infected patients with HIV viral load monitoring while on combination antiretroviral treatment: results from The TREAT Asia HIV observational database. BMC Infect Dis. 2010;10(1):1–10. doi:10.1186/1471-2334-10-361
9. Shambel W. Antiretroviral medication adherence, depression, and treatment outcomes among adult HIV patients on second-line antiretroviral therapy in Eastern Amhara Region, Ethiopia; 2022.
10. Ethiopian Health and Nutrition Research Institute and Federal Ministry of Health. HIV Related Estimates and Projections for Ethiopia-2012. Ethiopian Health and Nutrition Research Institute and Federal Ministry of Health; 2012.
11. Arefaynie M, Yalew M, Damtie Y, Kefale B. Determinants of early sexual initiation among female youth in Ethiopia: a multilevel analysis of 2016 Ethiopian Demographic and Health Survey. BMC Women’s Health. 2020;20(1):1–8. doi:10.1186/s12905-020-01069-4
12. Aemro A, Jember A, Anlay DZ. Incidence and predictors of tuberculosis occurrence among adults on antiretroviral therapy at Debre Markos referral hospital, Northwest Ethiopia: retrospective follow-up study. BMC Infect Dis. 2020;20:1–11. doi:10.1186/s12879-020-04959-y
13. Worku ED, Asemahagn MA, Endalifer ML. Epidemiology of HIV infection in the Amhara region of Ethiopia, 2015 to 2018 surveillance data analysis. HIV/AIDS Res Palliat Care. 2020;12:307–314. doi:10.2147/HIV.S253194
14. Worku WZ, Azale T, Ayele TA, Mekonnen DK. HIV is still a major public health problem among pregnant women attending ANC in Referral Hospitals of the Amhara Regional State, Ethiopia: a cross sectional study. BMC Women’s Health. 2022;22(1):468. doi:10.1186/s12905-022-02059-4
15. Worku WZ, Azale T, Ayele TA, Mekonnen DK. Effects of HIV infection on pregnancy outcomes among women attending antenatal care in referral hospitals of the Amhara Regional State, Ethiopia: a prospective cohort study. Int J Women’s Health. 2022;14:1405–1423. doi:10.2147/IJWH.S382685
16. Bekker L-G, Alleyne G, Baral S, et al. Advancing global health and strengthening the HIV response in the era of the sustainable development goals: the international AIDS Society—Lancet Commission. Lancet. 2018;392(10144):312–358. doi:10.1016/S0140-6736(18)31070-5
17. World Health Organization. Progress Report 2016: Prevent HIV, Test and Treat All: WHO Support for Country Impact. World Health Organization; 2016.
18. Armstrong-Mensah EA, Tetteh AK, Ofori E, Ekhosuehi O. Voluntary counseling and testing, antiretroviral therapy access, and HIV-related stigma: global progress and challenges. Int J Environ Res Public Health. 2022;19(11):6597. doi:10.3390/ijerph19116597
19. Bigna JJR, Plottel CS, Koulla-Shiro S. Challenges in initiating antiretroviral therapy for all HIV-infected people regardless of CD4 cell count. Infect Dis Poverty. 2016;5(1):1–6. doi:10.1186/s40249-016-0179-9
20. Hailu GG, Wasihun AG. Immunological and virological discordance among people living with HIV on highly active antiretroviral therapy in Tigray, Northern Ethiopia. BMC Infect Dis. 2021;21(1):1–11. doi:10.1186/s12879-021-06206-4
21. Pham MD, Nguyen HV, Anderson D, Crowe S, Luchters S. Viral load monitoring for people living with HIV in the era of test and treat: progress made and challenges ahead–a systematic review. BMC Public Health. 2022;22(1):1203. doi:10.1186/s12889-022-13504-2
22. Wedajo S, Degu G, Deribew A, Ambaw F. Rate of viral re-suppression and retention to care among PLHIV on second-line antiretroviral therapy at Dessie Comprehensive Specialized Hospital, Northeast Ethiopia: a retrospective cohort study. HIV/AIDS Res Palliat Care. 2021;13:877–887. doi:10.2147/HIV.S323445
23. Mocellin LP, Ziegelmann PK, Kuchenbecker R. A systematic review and meta-analysis assessing antiretroviral therapy for treatment-experienced HIV adult patients using an optimized background therapy approach: is there evidence enough for a standardized third-line strategy? Syst Rev. 2022;11(1):243. doi:10.1186/s13643-022-02102-3
24. Peter T, Zeh C, Katz Z, et al. Scaling up HIV viral load–lessons from the large‐scale implementation of HIV early infant diagnosis and CD 4 testing. J Int AIDS Soc. 2017;20:e25008. doi:10.1002/jia2.25008
25. Sagaon‐Teyssier L, Mmadi Mrenda B, Khol V, et al. Adherence to PI‐based 2nd‐line regimens in Cambodia is not simply a question of individual behaviour: the ANRS 12276 2 PICAM study. Trop Med Int Health. 2017;22(11):1428–1435. doi:10.1111/tmi.12975
26. Chol C, Negin J, Garcia-Basteiro A, et al. Health system reforms in five sub-Saharan African countries that experienced major armed conflicts (wars) during 1990–2015: a literature review. Glob Health Action. 2018;11(1):1517931. doi:10.1080/16549716.2018.1517931
27. Damtie TA, Ibrahim AJ, Yikna BB. Supply chain management performance of HIV/AIDS commodities and factors affecting it at health facilities of SNNPRS of Ethiopia; from the perspective of achieving 90-90-90 strategies. Integr Pharm Res Pract. 2020;9:11–21. doi:10.2147/IPRP.S228162
28. Estill J, Ford N, Salazar-Vizcaya L, et al. The need for second-line antiretroviral therapy in adults in sub-Saharan Africa up to 2030: a mathematical modelling study. Lancet HIV. 2016;3(3):e132–e139. doi:10.1016/S2352-3018(16)00016-3
29. Kebede F. Severe Acute Malnutrition (SAM) associated mortality rate of children attending HIV/AIDS care in North West Ethiopia, 2009–2019. SAGE Open Med. 2022;10:20503121221081337. doi:10.1177/20503121221081337
30. Günthard HF, Saag MS, Benson CA, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2016 recommendations of the International Antiviral Society–USA panel. JAMA. 2016;316(2):191–210. doi:10.1001/jama.2016.8900
31. Canfell K, Kim JJ, Brisson M, et al. Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395(10224):591–603. doi:10.1016/S0140-6736(20)30157-4
32. Lesko CR, Chander G, Moore RD, Lau B. Variation in estimated viral suppression associated with the definition of viral suppression used. AIDS. 2020;34(10):1519. doi:10.1097/QAD.0000000000002579
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
