Back to Journals » Infection and Drug Resistance » Volume 14
Trend in Antimicrobial Resistance of Staphylococcus aureus: Results from the China Antimicrobial Surveillance Network (CHINET) in the Last 15-Year-Period Reports (2005–2019)
Authors Liang Y, Qiu L, Zheng X , Liu J
Received 29 April 2021
Accepted for publication 28 May 2021
Published 10 June 2021 Volume 2021:14 Pages 2179—2181
DOI https://doi.org/10.2147/IDR.S318005
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
This paper has been retracted.
Yingjian Liang, 1,* Lidi Qiu, 2,* Xiaobin Zheng, 1 Jing Liu 1
1Department of Pulmonary and Critical Care Medicine (PCCM), The Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, 519000, People’s Republic of China; 2Department of Infectious Disease Intensive Care Unit, The Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jing Liu; Xiaobin Zheng
Department of Pulmonary and Critical Care Medicine (PCCM), Fifth Affiliated Hospital of Sun Yat-sen University, 52 East Meihua Road, Zhuhai City, 519000, People’s Republic of China
Tel/Fax +867562528733
Email [email protected]; [email protected]
Abstract: In this report, we analyze the trends in antimicrobial resistance of Staphylococcus aureus according to the last 15-year-period reports of the China Antimicrobial Surveillance Network (CHINET). It is encouraging that there is a decreasing MRSA proportion in the infection of adults as well as better activity of non-beta-lactam agents in vitro in recent years. However, childhood MRSA infection as well as the tigecycline-resistant MRSA isolate in China deserves increasing concern.
Keywords: Staphylococcus aureus, antimicrobial resistance, China Antimicrobial Surveillance Network
Staphylococcus aureus (S. aureus) is a notorious opportunistic-pathogen responsible for a considerable section in a variety of infectious diseases, some of which are lethal.1 Antibiotic resistance surveillance can provide effective information in the clinical therapy of S. aureus infection for physicians. The consecutive microbiological surveillance among clinically significant isolates (such as S. aureus) has been ongoing in mainland China since 2005, named the China Antimicrobial Surveillance Network (CHINET). More and more hospitals from various provinces in China have participated in this programme since 2005. In the 2019 report, there were 36 tertiary hospitals from over 20 provinces or autonomous regions. Moreover, antimicrobial resistance of over 100,000 no-duplicate S. aureus isolates from routine laboratory work were submitted until 2019, which were informative to clinical physicians in treatment. Herein, we deciphered a trend of antimicrobial resistance among S. aureus from CHINET according to the last 15-year-period (2005–2019) reports, for physicians to develop a strategy in optimizing their approach of S. aureus infections.
All the data was downloaded from the website of the China Antimicrobial Surveillance Network (http://www.chinets.com). In vitro antimicrobial susceptibility of S. aureus isolates were determined by modified Kirby-Bauer disk diffusion method according to the Clinical and Laboratory Standards Institute (CLSI) guidelines. S. aureus ATCC 25923 was used as a quality control. Tigecycline (TGC) was evaluated according to the US FDA standard.
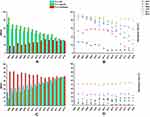
A total of 132,284 non-duplicate clinical isolates of S. aureus (including methicillin-sensitive S. aureus, MSSA and methicillin-resistant S. aureus, MRSA) was submitted during the 15-year surveillance period, 54,438 (41.15%) of which were MRSA, according to CHINET. The overall MRSA rate decreased from 69% in 2005 to 31.4% in 2019, and the prevalence of MRSA strains in adult cases had a similar trend that peaked in 2005 (85.8%) and then declined over the following 15 years (2019, 31.7%). The MRSA rate in children's infection cases has grown several times, peaking at 33.4% (2014), and has been stable at about 30% in the last 4-year period. Since 2012, the proportion of MSSA have been overweight than MRSA on CHINET. Regarding antimicrobial resistance, erythromycin (ERY) exhibited poor activity in MRSA (resistance rate over 70% since 2005) as well as MSSA (resistance rate over 45% since 2005) in this series of reports. Clindamycin (CLI) also exhibited low-to-moderate antimicrobial susceptibility in both MRSA (resistance rate over 50% since 2005) and MSSA (resistance rate over 20% since 2005). There is an abrupt growth in gentamicin (GEN) resistant MRSA isolates in 2006 (from 36.3% to 89.3%), but GEN has shown increased activity in vitro against MRSA since then. Levofloxacin (LEV) presented an extremely high resistance rate from 2005 to 2012 (over 80%). Antimicrobial activity of MRSA in GEN, LEV, and rifampicin (RIF) has gradually improved since 2012. Some of the tested antimicrobials revealed a higher resistance ratio in MRSA isolate rather than MSSA of the same time point, including RIF, GEN, LEV, CLI, and ERY, but trimethoprim–sulfamethoxazole (SXT) was not. Notably, it was the first time that CHINET reported TGC resistant MRSA on 2019 (0.7%). All S. aureus isolates were found to be susceptible to vancomycin, teicoplanin, and linezolid (Figure 1).
The CHINET Antimicrobial Surveillance Program has been ongoing since its inception in 2005 and the trends in MRSA proportion have declined in the last 15-year report, which is consistent with other regional as well as national surveillance programs, such as SENTRY.2 The noteworthy decreasing of MRSA isolate in the infection of adults is encouraging, but there has been concern about the considerable proportion in children, as it has greatly enhanced from 17.2% (2005) to 29.3% (2019), peaking at 33.4% in 2014. Moreover, it has stably contributed to about 30% of S. aureus infection in recent years, which indicated increased focus on infection prevention and stronger control interventions on children should be taken.
It is also encouraging that most of the non-beta-lactam agents exhibited better and better activity in vitro in recent years, both in MRSA and MSSA, but there is a high resistance rate of ERY, suggesting its potential therapy failure of S. aureus infection. There is no surveillance about the TGC susceptibility of S. aureus on CHINET report until 2019. However, our previous and others work has revealed the low TGC resistance rate of MRSA before 2019.3,4 Perhaps detailed research of TGC resistant MRSA should be under performed as there is scanty data about its molecular relatedness, resistant pattern, and virulence genes profiling in China. In summary, we elucidated the trend of antimicrobial among S. aureus based on the last 15-year-period CHINET report. Perhaps further insight about childhood MRSA infection as well as TGC resistant MRSA isolates in China should be warranted in the future.
Limitations
All the data was from CHINET, which indicated that those data of the hospital beyond this program may be ignored.
Data Sharing Statement
The data that supported this study was based on available data.
Acknowledgment
We gratefully acknowledge the contributions of the members of CHINET for collection of the isolates tested in the last 15 years (http://www.chinets.com/Data/AntibioticDrugFast).
Funding
This work was supported by Open project of Key Laboratory of Tropical Disease Control (Sun Yat-sen University), Ministry of Education (grant number 2020kfkt07).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chambers HF, Deleo FR. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat Rev Microbiol. 2009;7(9):629–641. doi:10.1038/nrmicro2200
2. Diekema DJ, Pfaller MA, Shortridge D, Zervos M, Jones RN. Twenty-year trends in antimicrobial susceptibilities among Staphylococcus aureus from the SENTRY antimicrobial surveillance program. Open Forum Infect Dis. 2019;6(Suppl 1):S47–S53. doi:10.1093/ofid/ofy270
3. Liang Y, Tu C, Tan C, et al. Antimicrobial resistance, virulence genes profiling and molecular relatedness of methicillin-resistant Staphylococcus aureus strains isolated from hospitalized patients in Guangdong Province, China. Infect Drug Resist. 2019;12:447–459. doi:10.2147/IDR.S192611
4. Wu D, Wang Z, Wang H, et al. Predominance of ST5-II-t311 clone among healthcare-associated methicillin-resistant Staphylococcus aureus isolates recovered from Zhejiang, China. Int J Infect Dis. 2018;71:107–112. doi:10.1016/j.ijid.2018.04.798
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.