Back to Journals » Infection and Drug Resistance » Volume 15
Trend Analysis of Intestinal Parasitic Infections at Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia from 2017 to 2021: A Five-Year Retrospective Study
Authors Workineh L , Almaw A , Eyayu T
Received 20 November 2021
Accepted for publication 4 March 2022
Published 10 March 2022 Volume 2022:15 Pages 1009—1018
DOI https://doi.org/10.2147/IDR.S350456
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Lemma Workineh, Andargachew Almaw, Tahir Eyayu
Department of Medical Laboratory, Debre Tabor University, Debre Tabor, Ethiopia
Correspondence: Lemma Workineh, Email [email protected]
Introduction: In Ethiopia, intestinal parasites are common due to poverty, poor personal hygiene, poor environmental sanitation, overcrowding, a lack of safe drinking water, and a lack of knowledge. As a result, evaluating the intestinal parasite morbidity pattern in low-income countries such as Ethiopia is important for designing intestinal parasite intervention programs that minimize the illness burden. Despite the high prevalence of the disease in the Debre Tabor catchment areas, there is a lack of data on the trend of intestinal parasites. As a result, the study’s goal was to close the gap on the patterns of intestinal parasite infection for better control and intervention programs.
Methods: A retrospective study was conducted from 2017 to 2021 at Debre Tabor comprehensive specialized hospital to determine the trend of intestinal parasite infection. The findings of 7965 saline wet mount stool examinations were collected from the laboratory registration book by trained data collectors over the last five years. The study excluded any data that lacked sociodemographic characteristics and the year of the stool examination. Finally, the data were analyzed by SPSS version 25.
Results: The overall prevalence of intestinal parasites during the study period (2017– 2021) was 2171 (27.3%) out of 7965 patients. Entamoeba histolytica/dispar (18.6%) was the predominant parasite, followed by Giardia lamblia (5.7%) and Ascaris lumbricoides (1%). Males (28.6%) were infected at a higher rate than females (26.2%) (P = 0.02). The intestinal parasite was reported in all age groups in the area, but the highest and the lowest prevalence were reported in the age groups of above 14 years (27.7%) and under five years (23.4%), respectively (P = 0.03).
Conclusion: The finding showed cyclic patterns of fluctuations in the prevalence of intestinal parasitic infections. Therefore, it is important to develop effective prevention and control strategies to prevent the distribution of intestinal parasites.
Keywords: Debre Tabor hospital, intestinal parasitic infection, trend analysis
Introduction
Intestinal parasitic infections (IP) are caused by intestinal helminths and protozoan parasites, which are the most common infections in developing countries.1 Intestinal helminths and protozoan infections have both been identified as major causes of illness and mortality worldwide.2 The most prevalent helminth parasites are Ascaris lumbricoides (A. lumbricoides), Trichuris trichiura (T. trichiura), and hookworm, which affect about one-sixth of the world’s population.3 Protozoa parasites such as Giardia lamblia (G. lamblia) and Entamoeba histolytica (E. histolytica) are also significant causes of morbidity worldwide.4 The IP infection has a major effect on an individual’s physical and mental development. It causes malnutrition, anemia, stunting, and cognitive impairment, and is thus a major public health issue throughout the world.5
These infections are most prevalent in tropical and subtropical regions of the developing world, where adequate water and sanitation facilities are lacking.6 Amoebiasis, ascariasis, hookworm infection, and trichuriasis are among the top ten most prevalent IP infections.7 IP infections contribute to a high global health burden, causing approximately 3.5 billion infections and 450 million clinical morbidities among most vulnerable populations in developing countries.8 According to a World Health Organization report, A. lumbricoides, hookworm, and T. trichiura infect around 1.3 billion, 1.25 billion, and 1 billion individuals worldwide, respectively.9
Moreover, the global burden of disease study shows amebiasis is responsible for more than 55,000 deaths and 2.2 million disability-adjusted life years, and giardiasis affects 5–10% of the population.10,11 IP is more prevalent and serious in Sub-Saharan Africa, where it is associated with a lack of clean water, poor sanitation, rapid population growth, and other economic and social issues. On the continent, more than 173 million people are infected with A. lumbricoides, while 198 million and 162 million people are infected with hookworms and T. trichiura, respectively.12 Intestinal parasitic infection affects the health status of an individual, mainly physical and mental development. It causes malnutrition, anemia, stunting, and cognitive impairment, and is thus a major public health issue around the world.
In Sub-Saharan Africa, Ethiopia has the second-highest ascariasis, third-highest hookworm, and fourth-highest trichuriasis infections.13 The number of individuals living in helminth endemic areas, particularly soil-transmitted helminths, is estimated to be 81 million in the country, including 9.1 million pre-schoolers, 25.3 million school-aged children, and 44.6 million adults.14 Similar to other African countries, IP is prevalent due to poverty, poor personal hygiene, environmental sanitation, overcrowding, low level of education and a lack of safe drinking water in Ethiopia.
More than half of the population in the country still uses open defecation, and most individuals in urban slums utilize unimproved sanitation facilities.15 IP has also been found to stick to plants, fruits, fingers, utensils, and door handles. Uncooked fruits and vegetables such as bananas, mangos, tomatoes, salads, and green peppers are commonly consumed raw, and they act as major vehicles for IP transmission in humans.16 Analyzing the IP morbidity pattern in low income countries like Ethiopia is really important for designing IP intervention programs to reduce disease burden. In the Debre Tabor catchment areas, there is a lack of data on the trend of IP despite the burden of the disease in the area. More than half of the population in the country still uses open defecation, and most individuals in urban slums utilize unimproved sanitation facilities.15 IP has also been found to stick to plants, fruits, fingers, utensils, and door handles. Uncooked fruits and vegetables such as bananas, mangos, tomatoes, salads, and green peppers are commonly consumed raw, and they act as major vehicles for IP transmission in humans.16 Analyzing the IP morbidity pattern in low income countries like Ethiopia is really important to design IP intervention programs in reducing disease burden. In Debre Tabor catchment areas, there is lack of data on trend of IP despite the burden of the disease in the area. As a result, the study’s goal was to close the gap on the patterns of IP infection in order to improve the disease control and intervention.
Methods
Study Area
Debre Tabor is located in the South Gondar zone of Amhara Regional State. It is the capital of the Farta district. In the northwest, it is 109 kilometers from Bahir Dar and 670 kilometers from Addis Abeba. The town is located at 11°51′N 38°1′E and is 2706 metres above sea level. The total population of the town is 64,381, out of which 32,623 (50.67%) and 31,758 (49.33%) are female and male, respectively, according to the South Gondar zone population projection. There are four government health institutions in the town. Among these, Debre Tabor comprehensive specialized hospital (DCSH) is one of the health institutions in the town and serves as a reference for the South Gondar community. The hospital was established in 1953 and serves more than 2.5 million people in its catchment area. The hospital is used as a teaching hospital for medical and health science students at Debre Tabor University. The hospital has medical, surgical, pediatric, gynecology, pharmacy, and laboratory departments. The laboratory department has parasitology, microbiology, hematology and immunology, clinical chemistry, and molecular laboratory departments. For the diagnosis of IP, a stool examination is performed in a parasitology laboratory (Figure 1).
 |
Figure 1 Map of the study are (Debre Tabor town). |
Study Design
A retrospective study was conducted to determine the trend of intestinal parasite prevalence from laboratory registration books over the past five years at DCSH (2017–2021).
Study Participants and Data Collection
The study participants were all individuals who were suspected of having intestinal parasitic infections and requested a stool examination during the study period. In the hospital, the only laboratory method to diagnose IP infection was direct saline wet mount. Therefore, 7965 patients’ data were collected from the parasitology registration book by the oriented data collectors. The laboratory results, such as the stage and species of the IP, were collected from the laboratory registration book by the data collection tool designed for this purpose. Furthermore, socio-demographic data like the year of data collection, sex, and age of the study participants were collected.
Exclusion and Inclusion Criteria
Over a five-year period, all IP suspected patients in the study area were included, and any data lacking sociodemographic characteristics and the year of stool examination performed, as well as data lacking species and stage of IP, were excluded.
Data Quality Control
Prior to data collection, the data collectors were trained and given the necessary instruments. The primary investigator checked a sample of the collected data for completeness and consistency every day. Finally, a representative sample of the extracted data was selected and checked for completeness, consistency, and accuracy. The primary investigator counted and documented the number of verified and suspected cases at the end of each data collection before sending it to data entry.
Data Processing and Analysis
SPSS version 25 software was used to enter and analyze the collected data. A descriptive statistic like a chi-square test was employed to compare the proportion of intestinal parasite isolates with patients’ socio-demographic information. A P-value of 0.05 was considered statistically significant.
Ethical Considerations
Prior to data collection, Debre Tabor University’s College of Health Sciences provided ethical clearance and this study was conducted in accordance with the Declaration of Helsinki. Individual names were deleted from the data acquired from the health center to maintain confidentiality, and only unique identification numbers were used to identify individuals.
Results
Socio-Demographic Characteristics of the Study Participants
During the study period (2017–2021), a total of 7965 stool samples were requested for intestinal parasite diagnosis in DCSH. Males made up 4603 (57.8%) of the suspected cases, while females made up the rest. The age of the study participants ranges from 1 to 90 years, with an average and standard deviation of 26.95 and 16.59 years, respectively. During the study period, 833 (10.5%), 844 (10.6%), and 6288 (78.9%) of IP suspected patients were under the age of five, 5–14 years, and greater than 14 years, respectively.
Prevalence of Intestinal Parasitic Infection from 2017–2021
The overall prevalence of the IP in the study area during the past five years was 2171/7965 (27.3% [CI=26.3–28.3%]). Ten different species of parasites have been identified in the study area. Of the total patients requested for stool examination, 1947 (24.5%) and 224 (2.8%) were infected by protozoa and helminths parasites, respectively. E. histolytica/dispar was the predominant parasite followed by G. lamblia and A. lumbricoides with a prevalence of 18.6% (95% CI = 17.8–19.4%), 5.7% (95% CI = 5.2–6.2%) and 1% (95% CI= 0.8–1.2%), respectively. The other identified parasites were hookworm, E. vermicularis, S. mansoni, H. nana, Taenia species, S. stercoralis, and T. trichiura (Table 1).
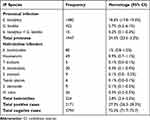 |
Table 1 Distribution of Intestinal Parasitic Infection at DCSH from 2017 to 2021 |
Annual Trend of Intestinal Parasitic Infection
The year with the highest proportion of IP cases was 2018, followed by 2019, and the year with the lowest proportion of IP cases was 2021. Overall, the percentage of IP increased from 25.8% in 2017 to 30.3% in 2018. Then it started to decline, from 26.9% in 2019 to 24.9% in 2021. From 2018 to 2021, the proportion of people infected with helminths dropped fast from 28.6% to 13.8%, whereas the number of people infected with protozoa fell slightly (Figure 2).
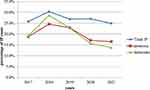 |
Figure 2 Annual trend of intestinal parasite infection at Debre Tabor comprehensive specialized Hospital, Northwest Ethiopia (2017–2021). |
As far as the prevalence of individual IP cases in relation to different years is concerned, a fluctuation of IP cases was observed. The highest average case (49) of all IP species has been observed in 2018 and the least average case of all IP species has been observed in 2021 (Table 2).
 |
Table 2 Annual Trends in Distribution of Intestinal Parasite Species at Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia (2017–2021) |
Trend of Intestinal Parasitic Infection in Relation to Gender and Age Groups
Regarding the IP cases between the genders, males were more infected with IP infection than females. Among the age groups, the adult population group (above 14 years) was more infected with IP as compared to other age groups. In general, IP infection was significantly associated with gender (x2 = 5.404, df = 1, p = 0.02) and age (x2 = 6.968, df = 2, p = 0.03) (Table 3).
 |
Table 3 Prevalence Intestinal Parasitic of Infection in Relation to Gender and Age at Debre Tabor Comprehensive Specialized Hospital from 2017 to 2021 |
In terms of IP classification in relation to gender, 1088 (89.9%) of female participants were infected by intestinal protozoan parasites and the rest were infected by intestinal helminths, while 859 (89.2%) of male participants were infected by protozoan parasites and the rest were infected by intestinal helminths. However, there was no statistically significant difference between male and female participants in terms of protozoa or helminth parasite infection (p = 0.595). Moreover, there is no statistical difference among age groups in terms of being infected by intestinal helminths or protozoans (Table 4).
 |
Table 4 Association of Intestinal Parasite Classification with Gender and Age at Debre Tabor Comprehensive Specialized Hospital (2017 to 2021) |
Regarding the annual trends of IP infection across the age groups, results showed a similar pattern of infection in males. However, in females, there was a slight rise in IP in the 2018 year and it began to fall from there (Figure 3).
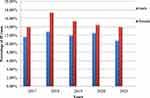 |
Figure 3 Annual trend of intestinal parasite percentage in relation to gender at Debre Tabor comprehensive specialized Hospital, Northwest Ethiopia (2017–2021). |
Regarding the annual trends of IP infection across the age groups, results showed a similar pattern of infection in males. However, in females, there was a slight rise in IP in the 2018 year and it began to fall from there (Figure 4).
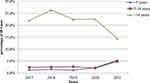 |
Figure 4 Annual trend of intestinal parasite proportion in relation to age group at Debre Tabor comprehensive specialized Hospital, Northwest Ethiopia (2017–2021). |
Discussion
Intestinal parasite infection is a neglected tropical disease and is a major public health problem in Ethiopia. As a result, maintaining regular surveillance and observing the trend of intestinal parasite infections in a specific community is a prerequisite for planning and evaluating existing programs as well as assisting in the development of appropriate intervention strategies. In the present retrospective study, it has been observed that the overall prevalence of intestinal parasitic infection over the last five years was 27.3% (CI=26.3–28.5%). This result was higher than those found in other Ethiopian studies: 9.3% in Mojo health center,17 6.23% in Bale Robe health center,18 and 16.65% in Wonago health center.19
The prevalence of this study, on the other hand, was lower than 45.6% in the University of Gondar student clinic,20 41.3% in the Gondar poly health center,21 and 53.3% in the Dembia district,22 35.5% in the Axum Saint Mary’s Hospital,23 34.5% in the Tikur Anbessa Hospital,24 and 47.9% in the Hawassa University Student Clinic.25
The disparity in prevalence between our study and others could be attributed to sociodemographic factors such as the study subjects’ educational status, occupation, or age. Geographic factors such as sanitation and climatic factors may also play a role in the variation. Protozoal infection was more prevalent than helminthic infection in our sample, accounting for 24.5% of the total. Similar to the present study, protozoan parasites were more common in studies from the University of Gondar,20 Bale Robe health center18 and Hawassa University student clinic.25 However, helminth infection was more prevalent than protozoan infection in a study from the Dambia district.22
The higher prevalence of protozoan parasites may be linked to poor personal and environmental hygiene, as protozoan parasites are transmitted mostly by the feco-oral route, which is transmitted indirectly through the intake of contaminated food and drink.26 The lower helminth prevalence could be due to a deworming program against helminths particularly soil-transmitted helminths and schistosomiasis in Ethiopia.27 Furthermore, because low temperatures are not conducive to helminth infection, the climatic conditions of our study area (high altitude and low temperature) may reduce the prevalence of helminth infection.28
The most common parasite found was E. histolytica/dispar with a prevalence of 18.6%, followed by G. lamblia (5.7%) and A. lumbricoides (1%). Similar findings have been reported in studies from Hawassa University student clinic,20 Tikur Anbessa hospital,24 University of Gondar student clinic,20 and Bale Robe health center.18 The higher prevalence of E. histolytica/dispar, G. lamblia and A. lumbricoides infections in the study might be attributed to poor sanitation and contaminated drinking water (since there is a shortage of clean drinking water in our study area). Furthermore, in the area, eating raw or unwashed vegetables is popular, which can readily facilitate the transfer of cysts or ova of these parasites.
The prevalence of total IP infection fluctuated throughout the years in the current study, with the highest annual prevalence (30.35%) in 2018 and the lowest prevalence (24.9%) in 2021. Similarly, IP fluctuations were observed at Mojo health center,17 University of Gondar student clinic,20 and Gondar poly health center.21 The difference in prevention and control strategies from year to year, as well as the socioeconomic conditions of the study individuals, could explain the likely trend variation.
Helminthes infection increased from 19.2% to 28.6% between 2017 and 2018, and then dropped to 13.8% in 2021, whereas protozoan infection fluctuated slightly year to year. This result is supported by research conducted in the Dambia district.22 From 2018 to 2021, mass drug administration for helminth infection, notably soil-transmitted helminthiasis and schistosomiasis, as well as temperature changes, could contribute to a rapid drop in helminth infection.
In terms of IP infection prevalence by gender, it was statistically significant (p=0.02) that males (28.6%) had more infections than females (26.2%). This finding was supported by research undertaken at the University of Gondar student clinic,20 Tikur Anbessa hospital,24 and the Dembia district.22 But males and females were equally affected by IP, according to studies from Mojo health center17 and Gondar Poly health center.21 The fact that males were more likely to be infected could be due to their involvement in outside activities such as agricultural activities, which could expose them to contaminated environments.
Regarding the distribution of the IP infection among age groups, a higher infection rate was observed in those aged over 14 years, followed by age groups 5–14 and 0–4 years, which is statistically significant (p = 0.03). This finding was consistent with the studies conducted at the Bale Robe health center18 and the Mojo Health center.17 However, a study conducted in Tikur Anbessa hospital has reported the highest prevalence of IP in children aged 5–14 years old.24 The high prevalence of IP infection in adult population groups as compared to children might be due to the occupationally related exposures of this age group.
Limitation
A stool examination diagnostic technique that is carried out in Ethiopia in general and in DCSH in particular is direct wet mount, which could underestimate the prevalence of IP in this retrospective study.
Conclusion
Intestinal parasitic infection was prevalent in 27.3% % of the patients requested for stool examination during the last five years. The findings revealed that the trend prevalence of IP infection fluctuated in a cyclic pattern. Infection rates were higher in protozoans than in helminths. Therefore, it is important to develop effective prevention and control strategies, including health education on the improvement of personal hygiene and environmental sanitation.
Abbreviations
DCSH, Tabor comprehensive specialized hospital; IP, intestinal parasites.
Acknowledgments
We would like to thank the Debre Tabor specialized hospital laboratory coordination office for letting us collect the data. We also want to express our gratitude to the data collectors.
Funding
No funding was obtained for this study.
Disclosure
The authors declare no competing of interest in this work.
References
1. Haque R. Human intestinal parasites. J Health Popul Nutr. 2007;25(4):387.
2. Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J. Helminth infections: the great neglected tropical diseases. J Clin Invest. 2008;118(4):1311–1321. doi:10.1172/JCI34261
3. World Health Organization. Soil-transmitted helminth infections. Available from:. www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections.
4. Hemphill A, Müller N, Müller J. Comparative Pathobiology of the Intestinal Protozoan Parasites Giardia lamblia, Entamoeba histolytica, and Cryptosporidium parvum. Pathogens. 2019;8(3):116. PMID: 31362451; PMCID: PMC6789772. doi:10.3390/pathogens8030116
5. Opara KN, Udoidung NI, Opara DC, Okon OE, Edosomwan EU, Udoh AJ. The impact of intestinal parasitic infections on the nutritional status of rural and urban school-aged children in Nigeria. Int J MCH and AIDS. 2012;1(1):73. doi:10.21106/ijma.8
6. Taiwo OT, Sam-Wobo SO, Idowu OA, Talabi AO, Taiwo AM. Comparative assessment of intestinal helminths prevalence in water, sanitation and hygiene (WASH) intervention and non-intervention communities in Abeokuta, Nigeria. Asian Pac J Trop Biomed. 2017;7(6):524–532. doi:10.1016/j.apjtb.2017.05.006
7. Tigabu A, Taye S, Aynalem M, Adane K. Prevalence and associated factors of intestinal parasitic infections among patients attending Shahura Health Center, Northwest Ethiopia. BMC Res Notes. 2019;12(1):1–8. doi:10.1186/s13104-019-4377-y
8. Mardu F, Yohannes M, Tadesse D. Prevalence of intestinal parasites and associated risk factors among inmates of Mekelle prison, Tigrai Region, Northern Ethiopia, 2017. BMC Infect Dis. 2019;19(1):1–8. doi:10.1186/s12879-019-4053-9
9. World Health Organization. Training Manual on Diagnosis of Intestinal Parasites: Tutor’s Guide [Electronic Resource]. World Health Organization; 2004.
10. Ghenghesh KS, Ghanghish K, BenDarif ET, Shembesh K, Franka E. Prevalence of Entamoeba histolytica, Giardia lamblia, and Cryptosporidium spp in Libya: 2000–2015. Libyan J Med. 2016;11(1):32088. doi:10.3402/ljm.v11.32088
11. Al Saqur IM, Al-Warid HS, Albahadely HS. The prevalence of Giardia lamblia and Entamoeba histolytica/dispar among Iraqi provinces. Karbala Int J Mod Sci. 2017;3(2):93–96. doi:10.1016/j.kijoms.2017.04.001
12. Molyneux DH, Hotez PJ, Fenwick A. “Rapid-impact interventions”: how a policy of integrated control for Africa’s neglected tropical diseases could benefit the poor. PLoS Med. 2005;2(11):e336. doi:10.1371/journal.pmed.0020336
13. Deribe K, Meribo K, Gebre T, et al. The burden of neglected tropical diseases in Ethiopia, and opportunities for integrated control and elimination. Parasit Vectors. 2012;5(1):1–5. doi:10.1186/1756-3305-5-240
14. Fedral Ministry of Health Ethopia. Second Edition of National Neglected Tropical Diseases Master Plan. Addis Ababa: Fedral Ministry of Health Ethopia; 2016.
15. Beyene A, Hailu T, Faris K, Kloos H. Current state and trends of access to sanitation in Ethiopia and the need to revise indicators to monitor progress in the post-2015 era. BMC Public Health. 2015;15(1):1–8. doi:10.1186/s12889-015-1804-4
16. Alemu G, Nega M, Alemu M. Parasitic contamination of fruits and vegetables collected from local markets of Bahir Dar City, Northwest Ethiopia. Res Rep Trop Med. 2020;11:17. doi:10.2147/RRTM.S244737
17. Chala B. Prevalence of intestinal parasitic infections in Mojo Health Center, Eastern Ethiopia: a 6-year (2005–2010) retrospective study. Epidemiol. 2013;3(119):2161. doi:10.4172/2161-1165.1000119
18. Chala B. A retrospective analysis of the results of a five-year (2005–2009) parasitological examination for common intestinal parasites from bale-Robe Health Center, Robe Town, Southeastern Ethiopia. Int Sch Res Notices. 2013;2013:694731.
19. Girum T. Prevalence of intestinal parasitic infections among patients with diarrhea at Wonago health center, southern Ethiopia: a retrospective study. Immunol Infect Dis. 2015;3(1):1–6.
20. Derso A, Yenealem G, Addisu A, Five-Year A. Trend of intestinal parasite prevalence among students attending clinic at University of Gondar, Northwest Ethiopia. J Parasitol Res. 2021;2021:1–5. doi:10.1155/2021/8897935
21. Ayelgn M, Worku L, Ferede G, Wondimeneh Y. A 5 year retrospective analysis of common intestinal parasites at Poly Health Center, Gondar, Northwest Ethiopia. BMC Res Notes. 2019;12(1):1–6. doi:10.1186/s13104-019-4735-9
22. Addisu A, Zeleke AJ, Bayih AG, et al. Trends and seasonal patterns in intestinal parasites diagnosed in primary health facilities in Northwest Ethiopia. J Infect Dev Ctries. 2020;14(06.1):58S–65S. doi:10.3855/jidc.11729
23. Feleke DG, Tarko S, Hadush H, Gebretsadik D, Zenebe Y, Seid A. Prevalence of intestinal parasitic infections in St. Marry Hospital, Axum, Northern Ethiopia: a retrospective study journal of tropical diseases. Age. 2017;7:100.
24. Tessema A, Yitayew B, Kebede T. Intestinal parasitic infections at Tikur Anbessa University Hospital, Ethiopia: a 5-year retrospective study. Int J Infect Dis Ther. 2016;1(1):22–26.
25. Menjetta T, Simion T, Anjulo W, et al. Prevalence of intestinal parasitic infections in Hawassa University students’ clinic, Southern Ethiopia: a 10-year retrospective study. BMC Res Notes. 2019;12(1):1–5. doi:10.1186/s13104-019-4747-5
26. Oishi CY, Seguí R, PC K, et al. Reduced prevalence of soil-transmitted helminths and high frequency of protozoan infections in the surrounding urban area of Curitiba, Paraná, Brazil. Parasite Epidemiol Control. 2019;1(7):e00115. doi:10.1016/j.parepi.2019.e00115
27. Federal Democratic Republic of Ethiopia Ministry of Health. Second edition of Ethiopia National Master Plan for neglected tropical diseases. Addis Ababa, Ethiopia; 2016. Available from: https://www.afro.who.int/publications/second-edition-national-neglected-tropical-diseases-master-plan-ethiopia-2016.
28. Blum AJ, Hotez PJ. Global “worming. climate change and its projected general impact on human helminth infections. PLoS Negl Trop Dis. 2018;12(7):e0006370. doi:10.1371/journal.pntd.0006370
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
