Back to Journals » Cancer Management and Research » Volume 14
Treatment Responses, Toxicity, and Survival in Patients with Classical Hodgkin Lymphoma Aged ≥50 Years: A Single-Center Experience Over Two Decades
Authors Çokgezer S, Elverdi T, Salihoğlu A, Ar MC, Öngören, Başlar Z, Eşkazan AE
Received 21 February 2022
Accepted for publication 1 June 2022
Published 7 June 2022 Volume 2022:14 Pages 1911—1921
DOI https://doi.org/10.2147/CMAR.S363235
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Seema Singh
Simay Çokgezer,1 Tuğrul Elverdi,2 Ayşe Salihoğlu,2 Muhlis Cem Ar,2 Şeniz Öngören,2 Zafer Başlar,2 Ahmet Emre Eşkazan2
1Department of Internal Medicine, Istanbul University-Cerrahpaşa, Cerrahpaşa Faculty of Medicine, Istanbul, Turkey; 2Division of Hematology, Department of Internal Medicine, Istanbul University-Cerrahpaşa, Cerrahpaşa Faculty of Medicine, Istanbul, Turkey
Correspondence: Ahmet Emre Eşkazan, Istanbul University-Cerrahpaşa, Cerrahpaşa Faculty of Medicine, Department of Internal Medicine, Division of Hematology, Fatih, Istanbul, Turkey, Tel +90 533 722 73 76, Fax +90 212 589 79 34, Email [email protected]
Introduction: The aim of this study was to evaluate treatment responses, toxicity, and survival among cHL patients aged ≥ 50 years.
Methods: We retrospectively identified all newly diagnosed cHL patients and only included cases who were ≥ 50 years old at the time of diagnosis and with data available between 1999 and 2020.
Results: There were 101 patients, of which 52 were between 50 and 59 years of age, and 49 patients were ≥ 60 years old. Sixty-two patients were male, and the most common histopathological subtype was mixed cellularity cHL (58.4%). ECOG PS, CCI, CIRS, and ACE-27 scores were significantly higher in patients aged ≥ 60 years than those of 50– 59 age group. While all patients aged 50– 59 years received ABVD as first-line therapy, 79% (n=39) of cases aged ≥ 60 years had ABVD. In patients receiving ABVD, 95% and 92.7% of the cases aged 50– 59 and ≥ 60 years had CR, respectively (p=0.999). Age groups were comparable in terms of hematological and non-hematological toxicities (p=0.369, p=0.127, respectively). Although not statistically significant, median survival was longer in patients receiving a transplant than in those without transplantation (108 months vs 52 months, p=0.069). In multivariate analysis, the risk of progression was higher in patients with lymphocyte ≤ 600/mm3 and in those who were unresponsive to first-line therapy (p=0.002 and p< 0.001, respectively). Patients with B symptoms, age ≥ 60 years, and CIRS > 3 had higher risk of mortality (p=0.001, p=0.012, p=0.038, respectively). By using these 3 parameters, we defined a new risk score, which divided our patient cohort into two as low- and high-risk groups. Low-risk patients had significantly higher survival rates than the high-risk group (83.9% vs 40.5%, p< 0.001).
Discussion: This new prognostic score should be further tested and validated in other patient populations. Although our study has some limitations including the limited number of patients and its retrospective nature, there are not so many studies in elderly cHL patients and elderly and/or frail patients are generally excluded in most of the clinical trials. Thus, this real-life single-center experience would contribute to the literature.
Keywords: classical Hodgkin lymphoma, cHL, elderly patients, survival, toxicity
Introduction
Classical Hodgkin lymphoma (cHL) is a relatively common malignancy (annual incidence of 2–3 per 100,000), and it accounts for <1% of malignancies and approximately 10% of all lymphomas.1 It has a bimodal distribution, with an increased incidence in adolescents or patients in their early 20s and over 55 years of age.2 Elderly cHL patients constitute 20–25% of all cases.3
The prognosis of cHL is generally inferior in the elderly than in younger patients. While the 5-year overall survival (OS) of patients with cHL is 86.6%, this is 57.5% in patients aged ≥60 years.4–6 The inferior prognosis in elderly cHL is multifactorial. Diagnosis in advanced disease stage, aggressive course of the disease, Epstein–Barr virus (EBV) associated disease, B symptoms, poor performance status, comorbidities are more common in elderly patients than in younger patients. Aging is generally associated with potential changes in the pharmacodynamics and pharmacokinetics of cytotoxic agents. In the elderly patient group, the tolerance of conventional therapy decreases and there is more treatment toxicity with more treatment-related deaths.4,5,7
First-line treatment of elderly fit cHL patients is given with a similar curative purpose to younger patients, and ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) remains the standard chemotherapy regimen for older cHL patients. By balancing the risk/benefit ratio, omission of bleomycin (AVD) or integration of brentuximab vedotin (BV) with AVD can be considered, especially in elderly patients aged 70 years and older.7,8 The optimal management of unfit elderly patients is still unclear. Eastern Cooperative Oncology Group performance status (ECOG PS),4 Cumulative Disease Rating Score (CIRS),9 Adult Comorbidity Evaluation-27 (ACE-27),10 and Comprehensive Geriatric Evaluation (CGA)4 are some of the comorbidity and PS indices that might guide individual treatment selection.
In this single-center retrospective study, we aimed to evaluate patient characteristics, treatment responses and toxicities, and survival among cHL patients aged 50 years and older.
Patients and Methods
We retrospectively identified all newly diagnosed cHL patients and only included cases who were ≥50 years old at the time of diagnosis and with data available between 1999 and 2020. Patients who received treatment at other institutions were not included. All pathology specimens were examined at our institution, and patients with an initial diagnosis outside our center had histopathological revision. Demographic data, histopathological, clinical and laboratory characteristics, treatment modalities, dose modifications, responses to chemotherapy, and toxicities were evaluated. ECOG PS, CIRS, ACE-27, and Charlson Comorbidity Index (CCI) were calculated by the authors according to the records in the patient files. In our center, all patients receiving an anthracycline-containing chemotherapy have a baseline transthoracic echocardiography (TTE), and the ejection fraction (EF) results in TTEs were recorded retrospectively. Prognosis was determined according to the German Hodgkin Study Group (GHSG) and International Prognostic Score-7 (IPS-7) for patients with early- and advanced-stage disease, respectively.2,6
We included patients who were diagnosed within a timeframe of 21 years, and thus, in some patients, PET/CT evaluations were not available at diagnosis and/or during follow-up. So, Deauville scores could not be evaluated for those patients. CT sections of those who were evaluated with PET/CT were taken into consideration, and standardization was achieved in patients who could not undergo PET/CT. For the response evaluation, patients were divided into complete response (CR), partial response (PR), stable disease (SD), and progression according to PET/CT or CT results.11,12 Depending on the response level, patients were further divided into two as CR and non-CR, where the non-CR group included cases with PR, SD, and progression. OS was defined as the time from the diagnosis to the date of the last visit or death. Progression-free survival (PFS) was defined as the time from the diagnosis to the first relapse/progression, or death. Treatment-related toxicities, which were observed during the therapy up to 28 days after the last dose, were classified according to the Common Terminology Criteria for Adverse Events (CTCAE v5.0).13 Data were evaluated for two groups (patients aged 50–59 years and ≥60 years), and these groups were compared with each other.
Statistical Analysis
Statistical Package for the Social Science program (SPSS 24.0 program) was used for statistical analysis. The conformity of the quantitative data to the normal distribution was evaluated with the Shapiro–Wilk test and graphical examinations. Independent groups t-test was used for the evaluation of the normally distributed variables between two groups. The Mann–Whitney U-test was used for the evaluation of the non-normally distributed variables between two groups. The Kruskal–Wallis test was used for the intergroup evaluations of more than two non-normally distributed variables. If it was significant, Dunn-Bonferroni test was used to determine the source of significance. Pearson chi-square, Fisher’s, and Fisher-Freeman-Halton exact tests were used to compare qualitative data, when necessary. Log rank test and Cox regression analysis were used to determine the factors affecting OS and PFS. P value <0.05 was considered statistically significant.
Results
Patients’ Characteristics at Diagnosis
We first identified 677 patients with newly diagnosed cHL. One hundred and thirty-two of these patients (19.5%) were ≥50 years old at the time of diagnosis, of which 101 had sufficient data to make our final patient cohort. Among these 101 patients, 52 (51.5%) were between 50 and 59 years of age, and 49 patients (49.5%) were ≥60 years old (Table 1). The median age of the entire cohort was 59 years (range, 50–85 years). Sixty-two patients (61.4%) were male, and the percentage of males among cases aged 50–59 years was significantly higher than that of cases who were ≥60 years (73.1% vs 49% p=0.013). The most common histopathological subtype was mixed cellularity (58.4%), followed by nodular sclerosis (20.8%). Fifty-four patients had advanced-stage disease, while there were 31 and 16 patients with early-stage unfavorable and favorable diseases, respectively. Sixty-one patients (60.4%) had B symptoms. The percentage of any comorbidity in patients ≥60 years was significantly higher than in patients aged 50–59 years (83.7% vs 48.1%, p<0.001) (Table 1).
 |
Table 1 Demographic and Clinical Characteristics of All Patients and the Different Patient Groups |
The most common comorbidities were hypertension (30.7%) and diabetes mellitus (20.8%). Ejection fraction (EF) was >50% in 89 patients (95.7%), cardiovascular pathologies such as heart valve dysfunctions, ventricular hypertrophies, pulmonary hypertension, diastolic dysfunction, pericardial effusion was found in 61.7% (n=58). The mean ± standard deviation (SD) EF% in patients ≥60 years was 57.8 ± 5.3, which was significantly lower than that of patients aged 50–59 (60.5 ± 4.9) (p=0.013). ECOG PS, CIRS, CCI, and ACE-27 scores were all significantly higher in patients aged ≥60 years than those of 50–59 age group (Table 2).
 |
Table 2 Different Scoring Systems in the Entire Patient Cohort and Two Age Groups |
Lymph node involvement in >3 regions was detected in 79.2% of the cases, and liver, spleen, and bone marrow involvement were detected in 13.9%, 27.7%, and 14.9% of the patients, respectively. Elevated ESR, extranodal, and bulky diseases were found in 56 (55.4%), 18 (17.8%), and 3 (3%) patients, respectively. Two groups were equally balanced regarding all these parameters (Supplementary Table 1).
Treatment Distributions, Responses, Transplantation, and Toxicities
While all patients aged 50–59 years received ABVD as first-line therapy, 79% (n=39) of patients ≥60 years had ABVD (p<0.001). AVD and mini-CHOP (400 mg/m2 cyclophosphamide, 25 mg/m2 doxorubicin, 1.4 mg/m2 vincristine, and 40 mg/m2 prednisolone) were given to 3 patients (3%) among cases who were ≥60 years old (Supplementary Figure 1). In patients receiving ABVD as first-line treatment, CR rates at interim evaluation were comparable between patients with IPS-7 = 0–3 and those with IPS-7 = 4–7 (62.8% vs 41.2%, p=0.092). At the end-of-treatment (EOT) evaluation, 95% (n=38) of patients aged 50–59 years and 92.7% (n=38) of patients aged ≥60 years achieved CR (p=0.999). There was no significant difference regarding response rates at interim and EOT evaluations following first-line treatment in the favorable and unfavorable early-stage patients according to GHSG (p=0.470 and p=0.837, respectively) (Supplementary Table 2).
None of the patients aged ≥60 years at diagnosis had received autologous hematopoietic stem cell transplantation (AHSCT) and/or allogeneic hematopoietic stem cell transplantation (allo-HSCT). On the other hand, 8 patients (15.4%) diagnosed between 50 and 59 years of age underwent AHSCT, whereas one patient (1.9%) received an allograft, and one patient (1.9%) received both AHSCT and allo-HSCT.
While full-dose chemotherapy was administered in 71 patients (70.3%), 30 patients (29.7%) needed a dose reduction. The percentage of patients needing a dose reduction was 38.8% among patients ≥60 years, whereas this was 21.2% for patients aged 50–59 years (p=0.053). In the patients receiving ABVD as first-line treatment, neutropenia (28.7%) and neuropathy (7.9%) were the most common grade 3–4 hematological and non-hematological toxicities, respectively. Among the entire patient cohort, cumulative incidence of grade 3–4 hematological and non-hematological toxicities were 49.5% and 14.9%, respectively, and there was no significant difference between age groups in terms of hematological and non-hematological toxicities (p=0.369 and p=0.127, respectively) (Supplementary Table 3). In addition, the percentages of patients with hematological and non-hematological toxicities were comparable in the CIRS ≤3 and >3 groups (p=0.100 and p=0.999, respectively). While the rates of grade 3–4 hematological toxicities were similar between patients receiving full and reduced-dose chemotherapy, grade 3–4 non-hematological toxicities were less common in those with a dose reduction (p=0.091 and p=0.042, respectively) (Supplementary Table 4).
Survival and Factors Having an Impact on PFS and OS
The median follow-up was 57 months (range, 1–264 months) for the entire cohort, and this was significantly longer in patients aged 50–59 years than that of cases who were ≥60 years (71.5 months vs 47 months, p=0.017) (Table 1).
Median PFS of patients ≥60 years of age was found to be significantly shorter than patients aged 50–59 years (32 months vs 59 months, p=0.043). Similarly, median OS was significantly shorter in patients who were ≥60 years than that observed in patients aged 50–59 years (49 months vs 75.5 months, p=0.048).
Among cases receiving salvage treatment, median OS was comparable between those with and without AHSCT/allo-HSCT [108 months (Q1=80 months, Q3=149 months) vs 52 months (Q1=22.5 months, Q3=89 months), p=0.069]. The 2-year OS were 90% and 75% for those with and without AHSCT/allo-HSCT, respectively, while 5-year OS were 80% and 58.3%, for the same populations. As a risk factor included in the IPS-7, patients with lymphocyte counts ≤600/mm3 at baseline and cases who were unresponsive to first-line treatment had inferior PFS than those with a baseline lymphocyte count >600/mm3 and cases who responded upfront chemotherapy (p=0.002 and p<0.001, respectively) (Figure 1A and B). Patients who were 50–59 years old, those without B symptoms, and cases with CIRS ≤3 had superior OS than patients ≥60 years, cases with B symptoms, and patients with CIRS >3 (p=0.001, p=0.012, and p=0.038, respectively) (Figure 2A–C).
 |
Figure 1 Progression-free survival (PFS) according to lymphocyte counts (A), EOT response (B) (EOT, end of treatment). |
 |
Figure 2 Overall survival (OS) according to age (A), B symptoms (B), Cumulative Disease Rating Score (CIRS) (C). |
Univariate Cox regression analysis showed that histopathological subtype, lymphocyte count, and EOT response appeared to have a significant prognostic impact on PFS (p=0.021, p=0.001, p<0.001, respectively) (Table 3). We then tested those statistically significant variables with multivariate Cox regression analysis using the backward elimination method. Lymphocyte count and EOT response variables kept their significance. The risk of progression in patients with lymphocyte count ≤600/mm3 was found to be 8.973 times higher than those with lymphocyte count >600/mm3 [(95% CI) = 8.973 (2.308, 34.893), p=0.002] (Table 3). The risk of progression in patients who did not respond to EOT was found to be 12.360 times higher than that of patients who responded to EOT [(95% CI) = 12.360 (3.625, 42.144), p<0.001] (Table 3).
 |
Table 3 Univariate and Multivariate Cox Regression Analysis for PFS |
Age at diagnosis, presence of B symptoms, CCI, CIRS, and ECOG PS scores had a significant prognostic impact on OS in the univariate Cox regression analysis (p=0.001, p=0.049, p=0.011, p=0.005, p=0.004, respectively). Variables with a significant impact on univariate analysis were then tested in the multivariate Cox regression model, and age at diagnosis, presence of B symptoms, and CIRS score continued to be significant. Patients aged ≥60 years had 3.711 times increased risk of mortality than patients who are between 50 and 59 years [(95% CI) = 3.711 (1.698, 8.112), p=0.001] (Table 4). The risk of mortality was found to be 2.987 times higher for patients with CIRS >3 patients compared to patients with CIRS ≤3 [(95% CI) = 2.987 (1.269, 7.030), p=0.012)]. Similarly, the risk of mortality was also found to be 2.357 times higher for patients with B symptoms, compared to patients without B symptoms [(95% CI) = 2.357 (1.048, 5.297), p=0.038)] (Table 4).
 |
Table 4 Univariate and Multivariate Cox Regression Analysis for OS |
In our study, we demonstrated that age, B symptoms, and CIRS had a prognostic impact on OS. And by using these 3 parameters, we created a new prognostic score. For all variables, scores were given as 0–1 point. Patients between 50 and 59 years old received 0 point, as patients ≥60 years had 1 point. Similarly, patients with B symptoms and CIRS >3 had 1 point for each, whereas cases without B symptoms and those with CIRS ≤3 received 0 point for each (Supplementary Table 5). Those with a total score of 0–1 were defined as the low-risk group, and those with a total score of 2–3 were the high-risk group. We have shown that survival of patients in the high-risk group was significantly lower than that observed in the low-risk patients (83.9% vs 40.5%, p<0.001) (Figure 3).
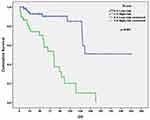 |
Figure 3 OS according to new survival score groups. |
During their follow-up, 26 patients (25.7%) died, and the most common causes of death were treatment complications (36.8%) and cHL-related death (10.5%). Seven patients (36.8%) died due to other causes [AA amyloidosis (n=1), congestive heart failure (n=1), graft-versus-host disease (n=1), decompensated liver failure (n=2), and ischemic cerebrovascular accident (n=2)], and secondary malignancies were detected in 5 patients, of which 3 died.
Discussion
It has been reported that cHL is more common in males in all age groups,11 including the elderly population.4,5,7 Most of our patients were also male; however, the percentage of female patients (51%) was slightly high in patients ≥60 years of age. Most probably this was due to the fact that 55.8% of the elderly population in our country is female.13
Mixed cellular cHL histology is more common in elderly patients (35%), but nodular sclerosis cHL has been reported to be the most common histology in both groups.14 While the most common histopathological subtype was nodular sclerosing in some studies,7 mixed cellular cHL was the most common subtype in others.4,5 In our study, mixed cellular was the most common subtype (58.4%), followed by nodular sclerosis cHL (20.8%).
Advanced disease (53.5%) and B symptoms (60.4%) were common in our population, and consistent with our findings, percentages of advanced disease and B symptoms were shown to be higher among elderly patients in previous studies.4,5,7,15–18
Different performance and comorbidity scales have been used in patients with cHL.4,7,16,18 In our study and in the study of Sykorova et al,4 the percentage of patients with a CIRS >3 in patients ≥60 years was 30.6% and 35.7%, respectively. The percentage of cases with ECOG PS 3–4 was significantly higher in patients ≥60 years than in patients 50–59 years, and similarly, in the study of Wrobel et al,7 rate of patients with ECOG PS 2–4 was higher in patients ≥60 years than that of patients 50–59 years (45% vs 23%, p=0.003). In the SHIELD study, modified ACE-27 comorbidity scale was used for comorbidity assessment,16 and 7.4% of the patients were frail, whereas 18.8% of our cases had an ACE-27 score of ≥3. Similar to our findings, in another study, the percentage of patients with a CCI score of ≥2 was significantly higher among cases ≥60 years when compared to younger cases (98% vs 8.3%, p<0.001).18 To the best of our knowledge, our study is the first one evaluating all these 4 scoring systems in cHL patients.
The optimal management of elderly cHL patients remains unclear.19 According to European Society for Medical Oncology (ESMO) guidelines, ABVD remains the standard regimen for the elderly fit patients. By balancing the risk/benefit ratio, bleomycin omission from ABVD (AVD) and integration of BV to AVD have been shown to be reasonable options with favorable outcomes.7,20 As a first-line treatment, ABVD was the most preferred regimen in our patient cohort, similar to other studies.4,5,7,21 In this study, 6% of the patients aged ≥60 years received AVD, while 4% had AVD + BV, which were compatible with the previous findings as AVD was received in 6.6%5 and 4% were administered AVD+BV.4
Response rates to first-line treatment in elderly cHL is another important issue. In the study of Wrobel et al,7 CR rate at the EOT evaluation was 64% in patients with advanced disease, which was 53.5% in our study. In another study, CR rates at the EOT PET/CT in patients <60 and ≥60 years of age were 47% and 42%, respectively (p=0.570).22 Similarly, in the study by Engert et al,14 CR rate was 86% in patients ≥60 years, while this was 90% in patients <60 years at the EOT evaluation. In our cohort, for those receiving first-line ABVD, CR rates were 92.7% and 95% for cases who are between 50–59 years and ≥60 years, respectively. On the other hand, this was slightly lower (70.7%) in patients who were ≥60 years in another study.4 These differences can be attributed to different treatment modalities administered in different patient cohorts and variability in the distribution of comorbidities and performance status across different studies.
Although it has been previously reported that more treatment-related toxicity and death are observed among elderly patient population,4,5 we did not find a significant difference between the age groups in terms of grade 3–4 hematological and non-hematological toxicities. Supporting this, there was no significant difference between the age groups in terms of grade 3–4 hematological and non-hematological toxicities in the study by Engert et al.14 Most probably, the reason for not observing higher rates of toxicities in our elderly frail patient population was because, more dose reductions were performed among this patient group.
There are few retrospective studies evaluating AHSCT in elderly cHL patients. In a single-center study with 15 patients ≥60 years who underwent AHSCT, 3-year OS was 88%.22 In our study, among patients with relapsed/refractory disease, 5-year OS was 80% for patients undergoing stem cell transplantation, which was similar to that was published by Böll et al.23 Although not statistically significant, among our patient cohort, median survival was longer in patients receiving a transplant than those without transplantation (108 months vs 52 months).
It was demonstrated that CIRS >3 and lymphopenia (<600/mm3) were independent risk factors for OS and PFS, respectively.4 In another study, in univariate analysis, baseline stage (I–II vs III–IV), age group (60–70 vs 71–80) and CCI (6≤ vs >6) were found to be independent prognostic factors for OS and cause-related survival, whereas in multivariate Cox regression analysis, baseline disease stage and age group were the only independent prognostic factors.5 Similarly, although age ranges were different, age had a significant impact on OS in our study. The study by Wrobel et al7 showed similar findings, and in a multivariate analysis, 3-year OS were calculated as 0.90 (95% CI; 0.82–0.98) and 0.81 (95% CI; 0.75–0.86) for early- and advanced-stage disease groups, respectively. In our study, 3-year OS was 86.5%, while they were 95.6% and 77.1% for the patients 50–59 years and ≥60 years, respectively. In a previous study, a significant decrease in mortality was found in patients without comorbidity and in patients with a CCI <2. In addition, male patients had a higher risk of death compared to females, and a significant increase in mortality was found in patients who received chemotherapy or radiotherapy alone compared to the combination of chemotherapy and radiotherapy.16 Unlike this study, we have shown that CCI, sex, and type of treatment did not have an impact on OS, while CIRS had an impact on OS.
Unlike in our study, patients aged ≥60 years were included in the study of Galli et al.24 While 54% of the cases in that study had CIRS ≥3, among our cohort, 30.6% of the patients ≥60 years had CIRS >3. In patients aged ≥60 years and receiving upfront ABVD, CR rate in our cohort was higher than that observed in that study (81% vs 92.7%). In addition, CIRS was found to be a prognostic factor for OS, as was displayed in our cohort, on the other hand, age was not. It has been emphasized that comorbidities have a more important impact on prognosis than age.24
With our new score, we have emphasized the possible superiority of CIRS among other comorbidity scores. The cHL patients were divided into two as low- and high-risk, and the high-risk patients had inferior survival than that observed in the low-risk group. Patients in the high-risk group might benefit from more intensive treatment modalities other than ABVD such as ABD + BV. We think this new prognostic score should be further tested and validated in other patient populations.
Our study has some limitations including the limited number of patients and its retrospective nature. Although the difference in toxicity rates among different CIRS subgroups is a subject of curiosity, we could not show this in our cohort, most probably due to the relatively low number of patients. However, since there are not so many studies on elderly cHL patients and elderly and/or frail patients are generally excluded in most of the clinical trials, we think that these real-life data with a relatively high number of patients for a unicenter study would contribute to the literature.
Conclusion
With this single-center study, we present our perspective on the clinical features, treatment modalities, treatment responses, toxicities, and survival in elderly patients with cHL treated over the past 2 decades. cHL seemed to be a highly curable disease, even in older patients. Treatment responses and toxicities were similar in patients aged 50–59 years and ≥60 years, most probably due to personalized treatment selection and dose reduction based on age, comorbidities, and performance status. Response status in the EOT evaluation and lymphocyte counts were associated with PFS, and age, CIRS, and B symptoms were associated with OS. Based on the new risk score created by using age, B symptoms, and CIRS, the presence of 2 out of 3 parameters was defined as high-risk. Initial assessments including age, B-symptoms, lymphocyte counts, comorbidity scores (especially CIRS), and performance status should be considered while planning the optimal treatment strategy in elderly patients with cHL.
Declarations
This study was approved by Istanbul University-Cerrahpaşa, Cerrahpaşa Faculty of Medicine Ethics Committee (16.02.2021, 83045809-604.01.02-35296), and it was in line with the Declaration of Helsinki. The study is a retrospective chart review without informed consent.
Disclosure
None of the authors have any conflicts of interest to declare in this work.
References
1. Vassilakopoulos TP, Asimakopoulos JV, Konstantopoulos K, Angelopoulou MK. Optimizing outcomes in relapsed/refractory Hodgkin lymphoma: a review of current and forthcoming therapeutic strategies. Ther Adv Hematol. 2020;11:2040620720902911. doi:10.1177/2040620720902911
2. Ansell SM. Hodgkin lymphoma: diagnosis and treatment. Mayo Clin Proc. 2015;90(11):1574–1583. doi:10.1016/j.mayocp.2015.07.005
3. Proctor SJ, Wilkinson J, Sieniawski M. Hodgkin lymphoma in the elderly: a clinical review of treatment and outcome, past, present and future. Crit Rev Oncol Hematol. 2009;71(3):222–232. doi:10.1016/j.critrevonc.2008.12.007
4. Sykorova A, Mocikovab H, Lukasova M, et al. Outcome of elderly patients with classical Hodgkin’s lymphoma. Leuk Res. 2020;90:106311. doi:10.1016/j.leukres.2020.106311
5. Moccia AA, Aeppli S, Güsewell S, et al. Clinical characteristics and outcome of patients over 60 years with Hodgkin lymphoma treated in Switzerland. Hematol Oncol. 2020;39:1–9.
6. National Cancer Institute. Cancer stat facts: Hodgkin lymphoma. Surveillance E, and End Results (SEER) Program; 2018.
7. Wróbel T, Biecek P, Rybka J, et al. Hodgkin lymphoma of the elderly patients: a retrospective multicenter analysis from the Polish Lymphoma Research Group. Leuk Lymphoma. 2019;60(2):341–348. doi:10.1080/10428194.2018.1482539
8. Helsing MD. Trofosfamide as a salvage treatment with low toxicity in malignant lymphoma. A Phase II study. Eur J Cancer. 1997;33(3):500–502. doi:10.1016/S0959-8049(97)89029-6
9. Salvi F, Miller MD, Grilli A, et al. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. J Am Geriatr Soc. 2008;56(10):1926–1931. doi:10.1111/j.1532-5415.2008.01935.x
10. Yancik R, Wesley MN, Ries LA, et al. Comorbidity and age as predictors of risk for early mortality of male and female colon carcinoma patients: a population-based study. Cancer. 1998;82:2123–2134. doi:10.1002/(SICI)1097-0142(19980601)82:11<2123::AID-CNCR6>3.0.CO;2-W
11. Diehl V, Re D, Josting A. Hodgkin’s disease: clinical manifestation, staging, and therapy. Hematol Basic Princ Pract. 2005;2005:1347–1377.
12. Türkiye İstatistik Kurumu. Haber Bülten. 2020; 33712. [Turkish]. Available from: https://data.tuik.gov.tr/Bulten/Index?p=Istatistiklerle-Yaslilar-2020-37227.
13. National Cancer Institute (US). Common terminology criteria for adverse events (CTCAE).v.5.0 [5x7]. Cancer Ther Eval Progr. 2017;155:90–92.
14. Engert A, Ballova V, Haverkamp H, et al. Hodgkin’s lymphoma in elderly patients: a comprehensive retrospective analysis from the German Hodgkin’s Study Group. J Clin Oncol. 2005;23(22):5052–5060. doi:10.1200/JCO.2005.11.080
15. Evens AM, Sweetenham JW, Horning SJ. Hodgkin lymphoma in older patients: an uncommon disease in need of study. Oncol. 2008;22(12):1369–1379.
16. Goyal G, Maldonado EB, Fan TJ, et al. Treatment patterns and outcomes in early-stage Hodgkin lymphoma in the elderly: a National Cancer Database Analysis. Clin Lymphoma, Myeloma Leuk. 2017;17(12):812–818. doi:10.1016/j.clml.2017.09.009
17. Carbone A, Spina M, Gloghini A, Tirelli U. Classical Hodgkin’s lymphoma arising in different host’s conditions: pathobiology parameters, therapeutic options, and outcome. Am J Hematol. 2011;86(2):170–179. doi:10.1002/ajh.21910
18. Major A, Jackson MW, Smith DE, Kamdar M, Rabinovitch R. Inferior outcomes and treatment disparities in elderly patients with classical Hodgkin lymphoma: a national cancer data base analysis. Leuk Lymphoma. 2019;60(5):1234–1243. doi:10.1080/10428194.2018.1522435
19. Eichenauer DA, Engert A, André M, et al. ESMO guidelines working group.Hodgkin’s lymphoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl4):iv19–iv29. doi:10.1093/annonc/mdy080
20. Carter J, David KA, Kritharis A, Evens AM. Current treatment options for older patients with Hodgkin lymphoma. Curr Treat Options Oncol. 2020;21(5). doi:10.1007/s11864-020-00745-9
21. Cencini E, Fabbri A, Sicuranza A, Santoni A, Bocchia M. Hodgkin lymphoma in the elderly: new perspectives and a 10-year monocenter real-life experience. Hematol Oncol. 2019;37(4):493–495. doi:10.1002/hon.2675
22. Puig N, Pintilie M, Seshadri T. High-dose chemotherapy and auto-SCT in elderly patients with Hodgkin’s lymphoma. Bone Marrow Transplant. 2011;46:1339–1344. doi:10.1038/bmt.2010.294
23. Böll B, Goergen H, Arndt N, et al. Relapsed Hodgkin lymphoma in older patients: a comprehensive analysis from the German Hodgkin Study Group. J Clin Oncol. 2013;31(35):4431–4437. doi:10.1200/JCO.2013.49.8246
24. Galli E, Cuccaro A, Maiolo E, et al. Comorbidity assessment to determine prognosis in older adult patients with classical Hodgkin lymphoma. Hematol Oncol. 2020;38:153–161. doi:10.1002/hon.2715
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
