Back to Journals » Open Access Emergency Medicine » Volume 15
Treatment Outcome, Pattern of Injuries and Associated Factors Among Traumatic Patients Attending Emergency Department of Dessie City Government Hospitals, Northeast Ethiopia: A Cross-Sectional Study
Authors Birhan S, Gedamu S , Belay MZ , Mera Mihiretu M , Tadesse Abegaz N, Fissha Adem Y , Tilahun Yemane T , Abdu Yesuf K
Received 27 May 2023
Accepted for publication 30 August 2023
Published 8 September 2023 Volume 2023:15 Pages 303—312
DOI https://doi.org/10.2147/OAEM.S419429
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hans-Christoph Pape
Sindu Birhan,1 Sisay Gedamu,2 Mulusew Zeleke Belay,2 Mengistu Mera Mihiretu,3 Nigusie Tadesse Abegaz,4 Yonas Fissha Adem,4 Tesfalem Tilahun Yemane,4 Kedir Abdu Yesuf4
1Department of Nursing, Dessie College of Health Sciences, Dessie, Ethiopia; 2Department of Nursing, Wollo University, Dessie, Ethiopia; 3Department of Health Systems and Management, Wollo University, Dessie, Ethiopia; 4Department of Public Health, Dessie College of Health Sciences, Dessie, Ethiopia
Correspondence: Yonas Fissha Adem, Email [email protected]
Background: Traumatic injuries are a major cause of emergency room visits and hospital workload, and they are a global health concern. Therefore, this study aimed to assess the pattern of injuries, treatment outcomes, and associated factors among traumatic patients attending the emergency department of Dessie City Government Hospitals, Northeast Ethiopia.
Methods: An institutional-based retrospective cross-sectional study was conducted among 415 traumatic patients selected by using a systematic random sampling technique, from July 1, 2019, to June 30, 2022. Data were collected through document review. The data were presented with frequency tables and graphs. Data were entered using EPI data version 4.6 and exported to SPSS version 26 for analysis. Both bi-variable and multivariable logistic regression analyses were performed to analyze the relationship between the independent variable and the outcome variable. As a measure of association, the adjusted odds ratio was utilized, which has a 95% confidence level. Statistically significant variables were those with a p-value of less than 0.05.
Results: From 420 patient charts, 415 traumatic patients’ charts were reviewed in this study, with a response rate of 98.8%. The prevalence of good treatment outcomes among traumatic patients was found to be 67% [95% CI: 62.2, 72.0]. In the final multivariable analysis, having comorbidity [AOR=, 0.31 95% CI: 0.16, 0.60], arriving within one hour [AOR=4.79, 95% CI: 2.10, 10.94], arriving two up to twenty-four hours [AOR=2.25, 95% CI: 1.34, 3.78] and being conscious at admission [AOR=1.82, 95% CI: 1.02, 3.26] had a significant association with a good treatment outcome among traumatic patients.
Conclusion: Trauma constitutes a major public health problem in our setting and contributes significantly to unacceptably high morbidity and mortality. Interventions should be targeted at urgent injury prevention and management strategies, along with the establishment of a pre-hospital emergency medical service system.
Keywords: injury, pattern, treatment outcome, associated factors
Background
Trauma remains a greatest cause of death for people between the ages of 15 and 44 worldwide,1 and a significant contributor to disability and income loss.2 A mean of 36 life years are lost for each trauma-related death since the incidence of trauma is particularly high in the younger population.3 Injury has been defined as damage to the body caused by an exchange of environmental energy that is beyond the body’s resilience.
There are two categories of injuries: unintentional and intentional (violence). The majority of accidents involving driving, fires, falls, poisonings, and drownings result in unintentional injuries. However, intentional or violence is divided into three categories: interpersonal (including violence against intimate partners), collective (including war), and self-directed (suicide).4
According to the World Health Organization (WHO), injuries account for 16% of all diseases worldwide. This results in 5.8 million fatalities from injuries annually, worldwide.5 WHO also estimates that in 2030, trauma is expected to rise to be the third cause of disability worldwide.6 Trauma affects all age groups, but there are peaks: younger age and older age.5,7
Injuries contribute to 5.4% of childhood deaths per year worldwide, and clinical outcomes are essential to addressing the burden of injury in low- and middle-income countries.8,9 The plan places a high priority on work-related injuries, including falls, fires, and road traffic accidents. The plan places a strong emphasis on the necessity of an effective emergency medical system in order to lessen the severity and effects of trauma and violence.10
The most likely injury victims were young, daily workers, drug users, and people with low monthly salaries. The distribution of injuries by mechanisms varies for deaths, hospitalizations, and emergency department visits.11,12 About 90% of injury-related deaths happened in low- and middle-income nations.13,14 One in five injury deaths was caused by road traffic accidents, which notably affect people aged 15 to 29. By 2030, it is anticipated to rank as the seventh greatest cause of death worldwide.11 Many factors affect the mortality and morbidity of injury, such as patient age, gender, the co-morbidity associated with chronic illnesses and body parts injured, and risky behavior such as the intake of multiple medications, excess alcohol use, and sedentary behavior, which can increase the risk of a fall and its consequences.15,16
Injuries are major health problems that commonly appear on the morbidity and mortality reports of health institutions in Ethiopia. Poor comprehensive emergency care system, availability and efficiency of an adequate pre-hospital care system in Ethiopia are very limited, though access to pre-hospital services and quick evacuation and transport to a hospital can save many lives, since the majority of those who die do so before they reach a hospital.8 In Ethiopia, epidemiologic studies revealed that the outcomes and patterns of injuries vary in different regions of the country. A study conducted at Gondar University found that the prevalence of injuries was 25%, of which 82% were young men. The most common causes of injury were personal injury (49.9%) and traffic accidents (48%).10,11 Another multicenter study conducted in the area of Amhara province showed a prevalence of injury of 55.5% in this area.11
Ethiopia does not have national injury prevalence rates or a national database injury registry for health planners and policymakers who need national injury prevalence rates. Therefore, there is a need to assess the prevalence of trauma and its impact in different regions of the country for injury planning and management strategies.11 Therefore, these research specific objectives were to provide data on treatment outcomes, patterns of injury, and associated factors in patients visiting the Emergency Department of Dessie City Government Hospitals. Since conducting research on trauma is worthwhile for gaining an understanding of the epidemiology of trauma and paramedic management of injuries, it may help inform clinical practice, enable better tailoring of paramedic education, and improve patient outcomes.
Methods and Materials
Study Design, Setting, and Period
Institution-based retrospective cross-sectional study was conducted in Dessie City Government Hospital, which is found in Amhara Regional State. Dessie is located at a distance of 402 km from Addis Ababa and 474.5 km from the capital city of the Amhara region, Bahir Dar. There are two government hospitals; those are Dessie Comprehensive Specialized Hospital and Boru Media General Hospital. The number of traumatic patients who visited emergency departments was 18,160 in the past three_year’s period in both government hospitals in Dessie City Administration. Among these, 13,520 traumatic patients were in Dessie Comprehensive Specialized Hospital, and the remaining 4640 traumatic patients were in Boru Media General Hospital. The study was conducted from July 1, 2019, to June 30, 2022.
Source and Study Population
Source Population
All trauma patients who visited Dessie City Government Hospitals.
Study Population
All trauma patients who visited Dessie City Government Hospitals during the past three years.
Inclusion and Exclusion Criteria
Inclusion Criteria
- Injured patients’ charts with complete data.
Exclusion Criteria
- Died at arrival were excluded.
Sample Size Determination
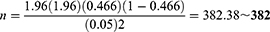
The total sample size (n) was calculated using the single population proportion formula and assuming, the proportion was 46.6%,11 95% confidence level, an accepted error of 5%, and finally adding a 10% non-response rate.
Where
n= required sample size
Z a/2 = critical value for normal distribution at 95% confidence interval which equals to 1.96 (Z value at alpha=0.05).
P= Proportion
d= an absolute precision (5% margin of error), therefore,
By considering a non-response rate (lost patients charts during the data collection period) of 10%, (382*0.1 = 38.2~38) then, the total sample size equals 382+38 = 420.
Sampling Technique and Procedures
First, from both government hospitals, the sample size was allocated proportionately to their size. The data was taken from each government hospital. The traumatic patients’ chart was selected by systematic random sampling in every K interval, using the formula (k = N/n, which is 18160/420 = 43). The first patient chart was selected by a simple random sampling technique, and then every 43th patient chart was included in the study until the required sample size was obtained (Figure 1).
 |
Figure 1 Flowchart for the sampling procedure. |
Study Variables
Dependent Variable
Treatment outcome (good/poor)
Independent Variables
- Socio-demographic characteristics (age, sex, marital status, occupation, residence, mode of transportation)
- Health-related factors: comorbidity, and GCS
- Injury related factors: Site of injury, type of injury, mechanism or cause of injury, nature of the injury, time to arrive institution, condition of the patient on arrival, operated on hospitalization.
- Behavioral factors: Alcohol intake, cigarette smoking, coffee drinking, and chat chewing
Operational Definitions
Good treatment outcome: is defined as if the patient was discharged with improvements and/or without complications (hearing loss, sight loss, amputations, and paralysis).12
Poor treatment outcome: is defined as if the patient was discharged with complications or referred to a higher health facility, or died in the hospital.12
Injury: physical damage to the body, intentionally or unintentionally.
Pattern of injury: The leading causes of injury among all injured patients during the study period are represented numerically.
Nature of injury: the physical characteristics of the injury, whether actual or just suspected, that led the patient to the emergency room.
Death at arrival: within an hour of being at the hospital, the cause of death.
Data Collection Tools and Quality Control
A pretested and structured checklist was used to retrieve the data from hospital records. The checklist was adapted from the WHO standard questionnaire for institute-based injury surveys.17 Data were collected from the patient’s charts about the outcome of treatment, the pattern of injury, and possible factors. Three BSC nurses who were chosen from other healthcare facilities and were under the supervision of two BSc healthcare professionals collected the data. Its quality was maintained by creating appropriate instruments for data gathering, doing pre-testing, and maintaining close monitoring. Additionally, before beginning actual data collection, BSC nurses who would be collecting the information had a two-day training session on data collection methodologies.
Data Processing and Analysis
Data were entered into EPI Data version 4.6, and then it was exported to SPSS version 26 for cleaning and analysis. To explain the study variables, various frequency tables, graphs, and descriptive summaries were used. A multivariable binary logistic regression model was used to analyze the relationship between the independent variable and the outcome variable. The Hosmer and Lemon show test and VIF were used to determine the model fitness and multicollinearity. Each independent variable’s relationship to the outcome variable was initially bi-variable analyzed, and any variables with a resulting p-value of less than 0.3 were added to the multivariable binary logistic regression model. The final model included only those variables with a p-value of 0.05 or less that were considered statistically significant. These variables were then given as odds ratios (OR) with a 95% confidence interval (CI) to indicate the strength and direction of the link.
Results
Socio-Demographic Characteristics of the Study Participants
From a total of 420 patient charts, 415 traumatic patients’ chart was reviewed in this study with a response rate of 98.8%. The majority of the traumatic patients 332 (80%) were males. Nearly half of the study participants 201 (48.4%) were Muslim by religion. Half of the participants 212 (51.1%) were urban dwellers (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Traumatic Patients in Dessie City Government Hospitals, Northeast Ethiopia, 2022 (n=415) |
Patterns of Injury Among Traumatic Patients
The most common injury body site among traumatic patients 126 (30.4%) were extremities, followed by the head which accounts for 88 (21.2%). On the other hand, the leading cause of injury among traumatic patients 163 (39.3%) were road traffic accidents, followed by gunshot injuries 98 (23.6%). The comments nature of injury among traumatic patients 149 (35.6%) were soft tissue injury, followed by fracture 144 (34.7%) (Table 2).
 |
Table 2 Pattern of Injury Among Traumatic Patients in Dessie City Government Hospitals, Northeast Ethiopia, 2022 (n=415) |
Injury-Related Factors Among Traumatic Patients
Majority of the participants 350 (84.3%) were conscious during admission. More than half the injured patients 268 (64.6%) arrived at the health facility between 2–24 hours. From all patient charts reviewed, 279 (67.2%) of them had normal (15) Glasgow coma scores (Table 3).
 |
Table 3 Injury-Related Factors Among Traumatic Patients in Dessie City Government Hospitals, Northeast Ethiopia, 2022 (n=415) |
Treatment Outcome of Injury Patient
In this study found, 137 (33%) with 95% CI, (28.0, 37.8) of injury patients had poor treatment outcomes and 278 (67%) with 95% CI, (62.2, 72.0) of injury patient had good treatment outcome (Figure 2).
 |
Figure 2 Treatment outcome among injury patients in Dessie City, Government hospitals, Amhara Region, Northeast Ethiopia, 2022 (n=415). |
Factors Associated with Treatment Outcome Among Injury Patients
To ascertain the presence of a relationship between the dependent variable and the independent variables at (P = 0.05) level of significance, bivariate and multivariate logistic regression models were fitted. For multiple binary logistic regression analysis, the variables that had a P-value of less than 0.3 with treatment outcomes among injured patients in the bivariate analysis were used.
In the final multivariable logistic regression model, three variables were significantly associated with treatment outcomes among injury patients at a 5% level of significance. The significant predictors of treatment outcome were comorbidity, time of arrival at the health facility, and the condition of the patients during admission.
Injured patients who had comorbidity [AOR =, 0.31, 95% CI: 0.16, 0.60], were 69% less likely to have good treatment outcomes as compared to those who did not have comorbidity. On the other hand, those who arrived within one hour and two to twenty-four hours were 4.79 times and 2.25 times more likely to have good treatment outcomes as compared to those who arrived greater than twenty-four hours, respectively [AOR = 4.79, 95% CI: 2.10, 10.94] and [AOR = 2.25, 95% CI: 1.34, 3.78]. Those injured patients, conscious during admission were 1.82 times more likely to have good treatment outcomes as compared to those who were unconscious patients [AOR = 1.82, 95% CI:1.02, 3.26] (Table 4).
 |
Table 4 Factors Associated with Treatment Outcome Among Injury Patients in Dessie City, Government Hospitals, Amhara Region, Northeast Ethiopia, 2022 (n=415) |
Discussion
In this study, 33% of injured patients had poor treatment outcomes. Hence, great attention should be given to those injured patients to improve this significant proportion of poor treatment outcomes. In this study’s findings, the overall prevalence of good treatment outcomes among traumatic patients was 67% with a 95% CI (62.2–72.0). The finding of this study is in line with the findings conducted in Addis Ababa (70%).4 Those findings are also in line with another study done in Central Tongu District (64%).18 The present finding of this study is higher as compared to the studies conducted in Nepal (51.1%).19 But this finding is lower as compared to the studies conducted in the South West Netherlands (90%),20 Addis Ababa Burn, Emergency, and Trauma Hospital (85.2%),15 and Gedeo Zone, South Ethiopia (93.9%).11 These variations could be attributed to socio-demographic differences in the study of the subjects. This discrepancy might also be attributed to the differences in accessibility of other health facilities.
In this study’s findings, the commonest mechanism (cause) of injury among traumatic patients was a road traffic accident (39.3%), followed by a gunshot injury (23.6%). It is contradicted by a study conducted in Gondar University Hospital, Northwest Ethiopia, which indicated that the main mechanism of injury among traumatic patients was assault (48.9%), followed by 45.2% of road traffic accidents.5 In this study, the three leading causes of death among traumatic patients were road traffic accidents, gunshots, and falls. Among injured body parts, the extremities account for 30.4%, followed by the head (21.2%). On the other hand, of all types of injuries, soft tissue injuries were the most common, one which accounts for 35.9%, followed by fractures (34.7%).
In this study, having comorbidity was found to be negatively associated with good treatment outcomes among traumatic patients. This finding is in line with the studies conducted in Addis Ababa, and Taiwan.15,21 Those who had comorbidity were 69% less likely to have good treatment outcomes as compared to those who did not have comorbidity. This might make sense given the fact that people with comorbidities are associated with poorer functional status, quality of life, and health outcomes, and comorbidities can raise your risk of problems or the emergence of a whole new health problem.
The other important variable that shows a positive association with good treatment outcomes was the condition of the patient at admission. This finding is also similar to those done in Addis Ababa, and the United States.15,20 Those who were conscious at admission were 1.82 times more likely to have good treatment outcomes as compared to those who were unconscious at admission. Being a conscious patient is not a potentially life-threatening situation. The conscious patient is not challenging, in terms of immediate care, diagnosis, specific treatment, or predicting prognosis, which leads to better outcomes.
On the other hand, time to arrival was also positively associated with the outcome variable among traumatic patients. The findings of this study are also in line with the study reported in Ethiopia, Nigeria, and Ruanda.11,22,23 Those who arrived at the health facility within two hours and two up to twenty-four hours were 4.79 and 2.25 times more likely to have good treatment outcomes as compared to those who arrived greater than twenty-four hours, respectively. This is thought to be because there were no medical institutions nearby and because many of the participants came from rural areas, which delayed referrals to higher institutions. The severity and outcomes of patients are negatively impacted by medical care delays. Hence, long wait times have the potential to have a negative impact on both staff, and patients by changing their behavior.
Strength and Limitation of the Study
The study was based on information gathered through a review of documents, and as such, the data might be susceptible to bias and might miss some important variables. However, its important contribution as a source of knowledge for the care and preventative tactics of trauma patients is one of its key strengths.
Conclusion
The overall prevalence of good treatment outcomes among traumatic patients was 67%. The commonest mechanism of injury among traumatic patients was road traffic accidents, followed by gunshot injuries. It’s recommended that healthcare facilities should design to overcome longer transport times for traumatic patients to the hospital. Healthcare providers should also provide a high level of care coordination for trauma patients with comorbid diseases. In addition, the health care provider needs to assess the patient’s level of consciousness and give special emphasis to those who were unconscious at the time of admission. The government should also design road safety interventions, and assure political instability to minimize road traffic and gunshot injuries.
Data Sharing Statement
Due to the dangers of participant identification and the difficulty of ensuring genuine anonymization, the datasets created and analyzed during the current study are not publicly available. However, the corresponding author may make subsets of the data available upon justifiable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the Institutional Research and Ethics Review Committee (IRB) of Wollo University, College of Medicine, and Health science. Individual patients were not harmed as long as confidentiality was maintained because the study was done by reviewing medical records. No personal information was included on the data collection form to maintain confidentiality, and no one other than the principal investigator had access to the recorded data. All methods were performed in compliance with the Declaration of Helsinki.
Acknowledgment
We would want to first and foremost express our sincere gratitude to Wollo University for providing this opportunity. Additionally, we would like to express our gratitude to Dessie Comprehensive Specialized Hospital and Boru Media General Hospital for helping us gather data for this thesis.
Disclosure
All authors declare that they have no competing interests.
References
1. Patton GC, Coffey C, Sawyer SM, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. 2009;374(9693):881–892. doi:10.1016/S0140-6736(09)60741-8
2. Copas DP, Moran CG. Major trauma care in England. Bone Jt. 2014;3(2):2–5.
3. Chiara O, Cimbanassi S. Organized trauma care: does volume matter and do trauma centers save lives? Curr Opin Crit Care. 2003;9(6):510–514. doi:10.1097/00075198-200312000-00008
4. Wolde A, Abdella K, Ahmed E, et al. East and central African journal of surgery pattern of injuries in Addis Ababa, Ethiopia: a one-year descriptive study. East Cent Afr J Surg. 2019;2019:14–22.
5. Awoke Ayele T, Zeleke BM, Tessema GA, Fentie Melak M. Magnitude and patterns of injuries among patients in Gondar University Hospital, northwest Ethiopia: an institutional-based study. Open Access Surg. 2017;10(April):25–31. doi:10.2147/OAS.S126043
6. Kasaye MD, Beshir MA, Endehabtu BF, et al. Medical documentation practice and associated factors among health workers at private hospitals in the Amhara region, Ethiopia 2021. BMC Health Serv Res. 2022;22(1):1–13. doi:10.1186/s12913-022-07809-6
7. Kirschke DL, Jones TF, Smith NM, Schaffner W. Photokeratitis and UV-radiation burns associated with damaged metal halide lamps. Arch Pediatr Adolesc Med. 2004;158(4):372–376. doi:10.1001/archpedi.158.4.372
8. Seid M, Azazh A, Enquselassie F, Yisma E. Injury characteristics and outcome of road traffic accident among victims at adult emergency department of Tikur anbessa specialized hospital, Addis Ababa, Ethiopia: a prospective hospital based study. BMC Emerg Med. 2015;15(1):1–9. doi:10.1186/s12873-015-0035-4
9. Laytin AD, Seyoum N, Kassa S, Juillard CJ, Dicker RA. Patterns of injury at an Ethiopian referral hospital: using an institutional trauma registry to inform injury prevention and systems strengthening. Afr J Emerg Med. 2020;10(2):58–63. doi:10.1016/j.afjem.2020.01.001
10. Woldemichael K, Berhanu N. Magnitude and pattern of injury in Jimma University specialized hospital, South west Ethiopia. Ethiop J Health Sci. 2011;21(3):155–165.
11. Abafita BJ, Abate SM, Kasim HM, Basu B. Pattern and outcomes of injuries among trauma patients in gedeo zone, dilla, South Ethiopia: a 5 years retrospective analysis. Ethiop J Health Sci. 2020;30(5):745–754. doi:10.4314/ejhs.v30i5.14
12. Bayissa BB, Alemu S. Pattern of trauma admission and outcome among patients presented to Jimma University specialized hospital, south-western Ethiopia. Trauma Surg Acute Care Open. 2021;6(1):6–10. doi:10.1136/tsaco-2020-000609
13. Misra P, Majumdar A, Misra M, et al. Epidemiological study of patients of road traffic injuries attending emergency department of a trauma center in New Delhi. Indian J Crit Care Med. 2017;21(10):678–683. doi:10.4103/ijccm.IJCCM_197_17
14. Peltzer K, Phaswana-Mafuya N, Arokiasamy P, et al. Prevalence, circumstances and consequences of non-fatal road traffi c injuries and other bodily injuries among older people in China, Ghana, India, Mexico, Russia and South Africa. Afr Saf Promot a J Inj Violence Prev. 2016;13(2):59–77.
15. Fikadu A, Sultan M, Michael M, Workina A. Pattern and outcomes of fall injuries and associated factors in emergency department at Addis Ababa burn, emergency and trauma hospital. Open Access Emerg Med. 2021;13(August):381–389. doi:10.2147/OAEM.S315546
16. Mulesi E. Comparison of Clinical Characteristics, Care and Outcomes of Trauma Patients Presenting During Regular and off Hours at Emergency Medicine Muhimbili. University of Health and Allied Sciences Department of Emergency; 2018.
17. Robert B, Brown EB, Jolois O. Injury surveillance guidelines. Lancet. 2004;97(1–2):1–14. doi:10.1016/s0165-2427(03)00160-0
18. Konlan KD, Doat AR, Mohammed I, et al. Prevalence and pattern of road traffic accidents among commercial motorcyclists in the Central Tongu District, Ghana. Sci World J. 2020;2020:1–10. doi:10.1155/2020/9493718
19. Shrestha VL, Bhatta DN, Shrestha KM, Kb GC, Paudel S. Factors and pattern of injuries associated with road traffic accidents in Hilly District of Nepal. J Biosci Med. 2017;05(12):88–100.
20. AlSulaim HA, Haring RS, Asemota AO, et al. Conscious status is associated with the likelihood of trauma centre care and mortality in patients with moderate-to-severe traumatic brain injury. Brain Inj. 2018;32(6):784–793. doi:10.1080/02699052.2018.1451658
21. Rau CS, Lin TS, Wu SC, et al. Geriatric hospitalizations in fall-related injuries. Scand J Trauma Resusc Emerg Med. 2014;22(1):1–8. doi:10.1186/s13049-014-0063-1
22. Yılmaz S, Calikoglu EO, Kosan Z. for an uncommon neurosurgical emergency in a developing country. Niger J Clin Pract. 2019;22(6):1070–1077. doi:10.4103/njcp.njcp_418_18
23. Mbanjumucyo G, George N, Kearney A, et al. Epidemiology of injuries and outcomes among trauma patients receiving prehospital care at a tertiary teaching hospital in Kigali, Rwanda. Afr J Emerg Med. 2016;6(4):191–197. doi:10.1016/j.afjem.2016.10.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.