Back to Journals » Integrated Blood Pressure Control » Volume 15
Treatment Outcome and Associated Factors Among Patients Admitted with Hypertensive Crisis in Public Hospitals at Harar Town, Eastern Ethiopia: A Cross-Sectional Study
Authors Samuel N , Nigussie S , Jambo A , Dechasa M , Demeke F , Godana A, Birhanu A , Gashaw T , Agegnehu Teshome A , Siraj A
Received 26 August 2022
Accepted for publication 22 November 2022
Published 13 December 2022 Volume 2022:15 Pages 113—122
DOI https://doi.org/10.2147/IBPC.S386461
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Turgay Celik
Nahom Samuel,1 Shambel Nigussie,1 Abera Jambo,1 Mesay Dechasa,1 Fekade Demeke,2 Abduro Godana,1 Abdi Birhanu,3 Tigist Gashaw,4 Assefa Agegnehu Teshome,5 Amas Siraj1
1Department of Clinical Pharmacy, School of Pharmacy, College of Health and Medical Science, Haramaya University, Harar, Ethiopia; 2Department of Epidemiology, College of Medicine and Health Science, Jigjiga University, Jigjiga, Ethiopia; 3College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 4Department of Pharmacology, School of Pharmacy, College of Health and Medical Science, Haramaya University, Harar, Ethiopia; 5Department of Biomedical Science, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia
Correspondence: Shambel Nigussie, Department of Clinical Pharmacy, School of Pharmacy, College of Health and Medical Science, Haramaya University, P.O. Box: 138, Dire Dawa, Ethiopia, Email [email protected]
Background: Hypertensive crisis is a significant global health issue that raises the costs to healthcare systems and requires specific attention to improve clinical outcome. There is scarce information on hypertensive crisis cases treatment outcome in the study setting.
Objective: This study aimed to assess treatment outcome and associated factors among patients admitted with hypertensive crisis at Public Hospitals in Harar Town, Eastern Ethiopia.
Methods: A cross-sectional study was conducted among 369 hypertensive crisis patients who had been admitted to the emergency department of Hiwot Fana Comprehensive Specialized Hospital and Jugol General Hospital from May 1, 2017, to May 1, 2022. All hypertensive crisis patients who fulfilled the inclusion criteria were included. The data were extracted from medical records using a data abstraction format. The collected data were analyzed using Statistical Package for Social Sciences version 22. Binary logistics regression model using bivariate and multivariable analysis with 95% confidence intervals and P-values were used to determine the association between variables.
Results: The medical records of 369 patients in total were reviewed. Of these, the medical records of 363 patients contained all the necessary information and were used in the study. More than half of the patients (238; 65.6%) were males. Among 363 patients admitted with hypertensive crisis, 98 (27.0%, 95% Confidence Interval (CI):22.5%-31.9%) of them had poor treatment outcome of hypertensive crisis. Being female (Adjusted Odds Ratio (AOR)=3.4; 95% CI=1.7− 7.9), residing in rural areas (AOR=2.4; 95% CI=2.7− 5.1), taking captopril during admission (AOR=5.6; 95% CI=2.4− 7.9), taking antihypertensive treatment before admission (AOR=0.5; 95% CI=0.2− 0.9), and being non compliant to treatment (AOR=2.7; 95% CI=1.4− 3.5) had statistically significant associations with poor treatment outcome of hypertensive crisis compared to their counterparts.
Conclusion: The magnitude of poor treatment outcome of hypertensive crisis was high. Sex, residence, non-compliance, and type of emergency drug administered during admission were substantially related with poor treatment outcome of hypertensive crisis. Health professionals should put great emphasis on emergency drugs administered during admission to achieve the desired outcome.
Keywords: hypertensive crisis, treatment, outcome, Eastern Ethiopia
Introduction
Over 80% of deaths from hypertension and related cardiovascular disorders occur in low- and middle-income countries, with the prevalence of hypertension predicted to reach more than 29% globally by 2025.1 The hypertensive crisis is a big worldwide health problem that increases the costs to health systems and needs special emphasis to improve clinical outcomes such as blood pressure control, complications, and mortality rate.2
Hypertensive crisis is defined as systolic blood pressure ≥180 mm Hg or diastolic blood pressure ≥120 mm Hg.3–5 Hypertensive Emergency (HE) and Hypertensive Urgency (HU) are two classes of a hypertensive crisis. HE is distinguished from HU by the quick degeneration of target organs (heart, brain, kidneys, and arteries) and the urgent threat to life it poses. Certain patients do not require anti-hypertensive treatment in the emergency room because they do not exhibit acute target organ damage (TOD) or a life-threatening condition, regardless of blood pressure levels.6
According to the findings of many studies, the prevalence of hypertension crisis is rising. HE rose from 3,309 per million cases in 2006 to 6,178 per million cases in 2013, according to a study done in an emergency clinic in the USA.7 According to a study done in Tanzania, around 68% of hypertensive patients admitted to the emergency room experienced hypertensive emergency.8 Likewise, another study found that hypertensive emergency accounted for 24% of hypertensive crisis cases.9
Uncontrolled blood pressure is more common in Ethiopia, which could put people at risk for hypertensive crisis. According to research among hypertension patients at Ayder Comprehensive Specialized Hospital, 52.5% of participants had uncontrolled blood pressure. More than one-fourth of patients (42; 29.8%) had hypertensive emergency, but more than two-thirds of patients (99; 70.2%) exhibited no signs of organ damage.6,10
Epidemiological information on the hypertensive crisis and its treatment outcome are limited in the setting of this study. Hence, this study is aimed to assess the treatment outcomes of hypertensive crisis and identify factors associated with treatment outcomes among hypertensive crisis patients who had been admitted to the emergency department in the study setting.
Methods and Materials
Study Area, Design, and Period
A cross-sectional study was conducted in the emergency departments of Hiwot Fana Comprehensive Specialized Hospital (HFCSH) and Jugol General Hospital (JGH). HFCSH serves as a referral hospital for Eastern Ethiopia, including Eastern Oromia, Dire Dawa City Administration, the Somali Regional State, and the Harari Regional State. Approximately 5,800,000 people are anticipated to live within the hospital’s catchment area, of which 2.85 million are female and 2.95 million are male.11 Currently, the hospital has roughly 238 beds with 294 functional rooms to provide a variety of services for the community. JGH is located in Feres Megala, Harari Region, Harar. The hospital provides services in Infectious & Tropical Diseases, Pediatrics, Emergency/Disaster Medicine, Women’s Health, Obstetrics and Gynecology, and Maternal–Fetal Medicine. The data were collected from May 2, 2022 to May 17, 2022.
Source and Study Population
The source population includes all adult hypertensive crisis patients who were admitted at the emergency departments of HFCSH and JGH. All adult hypertensive crisis patients who were admitted to the emergency department of HFCSH and JGH from May 1, 2017 to May 1, 2022, were the study population for this study.
Eligibility Criteria
All adult hypertensive crisis patients who were admitted at the emergency department of both hospitals were included. Hypertensive crisis cases with incomplete information on the medical record were excluded.
Sample Size and Sampling Procedure
There are two public hospitals (namely Hiwot Fana Comprehensive Specialized Hospital (HFCSH) and Jugol General Hospital (JGH)) in Harar town. Between May 1, 2017, and May 1, 2022, a total of 369 cases of hypertensive crises were recorded in the emergency department registries of the two public hospitals (236 in HFCSH and 133 in JH). Of these, 363 hypertensive crisis cases had complete data (232 in HFCSH and 131 in JH) and were included in the study. Hence, the sampling technique was a census type (included all cases who fulfilled the inclusion criteria).
Data Collection Method
The required data from patients’ medical records were recorded using a data abstraction format that was adopted from several studies.6,12,13 The English language version of the data abstraction format has been produced. Data abstraction format consists of socio-demography and clinical characteristics, treatment, and outcome of the hypertensive crisis patients. From the doctor’s initial assessment sheet, sociodemographic information and clinical traits were noted. On the other hand, vitals sheets were used to record blood pressure readings for nursing services at discharge. The follow-up sheet was used to record treatment compliance, which was evaluated and documented on each patient visit. Only the most recent visit was counted for patients who had several visits due to a hypertensive crisis. By using the medical record numbers from the emergency department’s registration manual, the medical histories of patients with hypertensive crisis were obtained. The medical records were retrieved from the medical record room after choosing the patient records’ numbers for hypertensive crisis patients. Three BSc nurses used a data abstraction format to obtain the relevant information.
Data Quality Control
Prior to the commencement of the actual data extraction, the data abstraction format was pretested on 5% randomly selected patients’ medical records who were experiencing hypertensive crisis at Haramaya General Hospital. During the pretest data collection, the data collectors identified as the drug regimen administered before admission and history of previous admission were available on medical records but not on the prepared data abstraction format. The data abstraction format’s final version was modified to address the errors that were identified during the pretest phase. Prior to collecting data, the data collectors received training. The supervisor oversaw and verified the data to guarantee its uniformity and completeness. When managing, storing, and analyzing the data, each piece of information was checked for accuracy and consistency.
Operational Definitions
Hypertensive crisis is defined as an acute elevation of blood pressure ≥180 mmHg systolic and/or ≥110 mmHg diastolic.
Hypertensive crisis: in this study hypertensive crisis of patients could be hypertensive emergency or hypertensive urgency.
Hypertensive emergency: defined as an acute elevation of blood pressure ≥180 mmHg systolic and/or ≥110 mmHg diastolic accompanied by acute target organ damage such as myocardial infarction, acute or worsening heart failure, pulmonary edema, ischemic stroke, hemorrhagic stroke, acute kidney injury, aortic dissection, hypertensive encephalopathy, and acute hypertensive retinopathy.
Hypertensive urgency: defined as an acute elevation of blood pressure ≥180 mmHg systolic and/or ≥110 mmHg diastolic without evidence of acute target organ damage.
Treatment outcome of hypertensive crisis: In this study, treatment outcome of hypertensive crisis could be good or poor.
Poor treatment outcome: death due to hypertensive crisis or referred to other hospitals due to unimproved status of hypertensive crisis based on final physician’s assessment.
Good treatment outcome: improved status of hypertensive crisis based on final physician’s assessment and discharged from the emergency department.
Data Analysis and Presentations
The data were imported using Epi Data statistical software version 3.1 and exported to Statistical Packages for Social Sciences (SPSS) version 22 for coding, cleaning, and analysis. Mean and standard deviation (SD) were used to summarize continuous variables, while frequency and percentage were used to portray categorical information. A binary logistics regression model using bivariate (Crude Odds Ratio (COR)) and multivariable analysis (Adjusted Odds Ratio (AOR)) with 95% confidence intervals and P-value were used to determine the association between variables. Variables with a P-value of less than or equal to 0.25 were transfered to a multivariable logistic regression analysis and the confounding variables were controled here in the final model. The presence and strength of association between dependent and independent variables was determined by the adjusted odds ratio and its 95% CI. A P-value of less than 0.05 was taken to show the presence of statistical significance.
Results
Patient Characteristics
The medical records of 369 patients were reviewed. Of those, the medical records of 363 patients contained all the necessary information and were used in the study. Nearly 55% of participants were above the age of 40 years. The mean age of participants was 41.2 years, with a standard deviation (SD) of 15.4. The majority of the participants (238; 65.6%) were males. About 260 participants lived in urban areas. The majority of patients (65.8%) had a history of pre-existing hypertension during admission. Thirty-one participants had organ damage by acute renal failure (Table 1).
 |
Table 1 Patient Characteristics of Emergency Department, Public Hospital, Harar, Ethiopia, 2022 |
Types of Hypertensive Crisis, Clinical Presentation, and Previous Treatment
Nearly 70% of participants were admitted with hypertensive urgency. Seventy-one patients had a clinical presentation of headache. More than half of the study participants (239; 65.8%) were on antihypertensive treatment before admission with hypertensive crisis. Of those who were on antihypertensive treatment, 65 (17.9%) participants took diuretics. More than half of the patients (149; 62.3%) were compliant to their treatment (Table 2).
 |
Table 2 Clinical Presentation and Previous Treatment, Public Hospital, Harar, Ethiopia, 2022 |
Treatment and Outcome
Thirty-one percent of the patients required oxygen supplementation, and near to 30% of patients needed ventilator support. Captopril was given to 70.2% of patients, while 29.8% were given intravenous hydralazine. Forty-one percent of patients were given IV fluid supplementation (Table 3). Among the admitted patients; 73% were discharged with an improvement of hypertensive crisis, while 17.07% had an unimproved status of hypertensive crisis at discharge and 9.9% died. All death was due to a hypertensive emergency. Among the 252 patients who were admitted with hypertensive urgency, 40 (15.9%) patients had poor treatment outcome. Of 111 patients who were admitted with hypertensive emergency, 58 (52.3%) patients had poor treatment outcome. Overall, among the 363 patients admitted with hypertensive crisis, 98 (27%, 95% CI= 22.5%−31.9%) patients had a poor treatment outcome (Figure 1).
 |
Table 3 Treatment of Hypertensive Crisis Patients and Laboratory Investigation During Admission, Public Hospital, Harar, Ethiopia, 2022 |
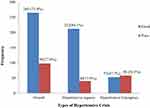 |
Figure 1 Treatment outcome of hypertensive crisis patients at discharge, Public Hospital, Harar, Ethiopia, 2022. |
Factors Associated with Poor Treatment Outcome of Hypertensive Crisis
In the multivariable logistic regression analysis, sex, residence, emergency drug administered during admission, and compliance to their treatment were significantly associated with poor treatment outcome of hypertensive crisis. Participants who were female were 3.4-times more likely to have poor treatment outcome of hypertensive crisis than those who were male: Adjusted Odds Ratio (AOR)=3.4; 95% confidence interval (CI)=1.7–7.9; P=0.01. The odds of poor treatment outcome of hypertensive crisis were 2.4-times higher among patients who lived in rural areas as compared to those who lived in the urban areas: AOR=2.4; 95% CI=2.7–5.1; P=0.03. Participants who were on captopril during admission were 5.6-times more likely to have a poor treatment outcome of hypertensive crisis as compared to those who were on hydralazine: AOR=5.6; 95% CI=2.4–7.9; P=0.01. The odds of a poor treatment outcome of hypertensive crisis decreased by 50% among patients who were on antihypertensives before admission. The participants who were non-compliant to their treatment were 2.7-times more likely to have a poor treatment outcome of hypertensive crisis compared with their counterparts (Table 4).
 |
Table 4 Multivariate Analysis of Factors Associated with Poor Treatment Outcome of Hypertensive Crisis at HFCSH and JGH, Harar, Ethiopia, 2022 admission |
Discussion
This study provides information on treatment, outcome, and its associated factors among patients admitted with hypertensive crisis in the emergency departments of HFCSH and JGH.
Among 363 hypertensive crisis cases, hypertensive urgency (69.4%) was more common than hypertensive emergency. Comparable findings were reported from Thailand, Italy, the USA, and Brazil, with high proportions of hypertensive urgency of 80.5%, 74.5%, 78%, and 60.4%, respectively.2,7,14,15 However, the current study finding was relatively higher than studies carried out in Tanzania (32%), eastern Sudan (38.3%), and Congo (24.4%).8,15,16 Different sample sizes and variations in the study setting could be the plausible causes of this disparity. Among patients presented with a hypertensive crisis, 65.6% of them were male. This high percentage of males were also present in hypertensive urgency, which is inconsistent with study reports from other regions of the world that reported a higher proportion of females than males.2,17–19 This variation might be due to differences in baseline sociodemographic characteristics of study participants.
In the current study, approximately two-thirds of hypertensive crisis patients had a history of pre-existing hypertension and this finding is in line with the study reported fromThailand.20 A high proportion of patients with hypertensive urgency had a previous history of hypertension than those with hypertensive emergency, which differs from a previous study conducted in Ayder Comprehensive Specialized Hospital.6 This disparity could be due to the non-compliance problem of patients to medication and lifestyle modification.
The percentage of non-compliance among patients in hypertensive crisis, especially in cases of hypertensive urgency, was high in prior research and comparable to this study’s results (37.7%).21–23 In line with previous research’ findings, non-compliance with therapy was found to be substantially related to a poor treatment outcome for hypertensive crisis.12,24–26 Compliance to treatment is the most important issue in order to improve blood pressure control and minimize hypertensive crisis associated morbidity and mortality.
In the present study, the majority (65.8%) of the patients had a history of hypertension treatment before admission with hypertensive crisis, which is similar with the previous study reported from northern part of Ethiopia. However, there is a difference in the utilized antihypertensive medications before admission.12 In the current study, the utilized antihypertensive medications include: diuretics, calcium channel blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers with diuretics, and diuretics with angiotensin-converting enzyme inhibitor. The discrepancy might be due to variations in the drug availability and presence of comorbidity among study participants. In this study, the most potent intravenous medication utilized for dropping blood pressure was hydralazine, which differ from a study conducted in Northeastern Thailand, where it was sodium nitroprusside.20 The plausible reason could be the difference in the availability of drugs.
In the current study, the most common target organ damage results were acute renal failure and ischemic stroke. However, acute coronary syndrome, left ventricular heart failure, cerebral infarction, pulmonary edema, and hypertensive encephalopathy were the most frequent consequences of hypertensive crisis documented in earlier studies carried out in Bahrain and Italy.27,28 This difference might be due to variety in health settings.
In this study, the magnitude of poor treatment outcome was high, which is similar to a previous report.29 The presence of acute end organ damage is a major poor prognostic indicator in hypertensive crisis.31 Patients presenting with a hypertensive crisis need the appropriate evaluation, medical regimen, and discharge instructions proposed by the updated guidelines.3 The present study found that all hypertensive crisis patients who died in the hospital were due to hypertensive emergency, which is in line with a study conducted at University of Gondar Specialized Hospital, northwest Ethiopia.12 However, the in-hospital mortality among patients with hypertensive emergency was lower than the study conducted in the Emergency Department (ED) of Muhimbili National Hospital.8 The probable explanation for difference is most patients in the study conducted in the Emergency Department (ED) of Muhimbili National Hospital did not receive the recommended ED management of their hypertension. The use of intravenous antihypertensive medication in acute management of hypertensive emergency is recommended as standard treatment.32–34
Regarding factors associated with hypertensive crisis, this study revealed that female patients were 3.4-times more likely to have poor treatment outcome of hypertensive crisis than male patients (95% CI=1.7–7.9). A similar finding was reported from a study conducted in Switzerland, which showed that being female was significantly associated with poor treatment outcome of hypertensive crisis.24 The likely explanation could be that those female patients may be less aware of cardiovascular complications linked to hypertension.
Furthermore, the present study found that the odds of poor treatment outcome of hypertensive crisis were 2.4-times higher among patients who lived in rural areas as compared to those who lived in the urban areas. The possible explanation might be hypertensive patients who lived in rural areas might not arrive promptly after experiencing hypertensive crisis.
Limitation of This Study
Due to the absence of a computerized system, the information in the records was entered manually, and sometimes it was difficult to read, providing few independent variables to the study, and this fact may also have an influence on the results. Due to the retrospective nature of the study, behavioral factors reported directly from the patient were not included. In this study factors associated with treatment outcome of hypertensive crisis were assessed using a cross-sectional design, which might not show causal relationships with potential factors.
Conclusion
Acute renal failure and ischemic stroke are the frequent types of end-organ damage in hypertensive emergency. The proportion of hypertensive urgency was found to account for a large percentage of patients. The magnitude of poor treatment outcome of hypertensive crisis was high. Sex, residence, non-compliance to their treatment and emergency drug administered during admission were significantly associated with poor treatment outcome of hypertensive crisis. The health professional should put great emphasis on the emergency drug administered during admission to achieve the desired outcome.
Ethical Consideration
An ethical clearance letter was obtained from Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee (IHRERC) under reference number IHRERC/019/2022. Haramaya University, College of Medical and Health Sciences IHRERC allowed the review of patients’ medical records with justifiable reason (for research purposes) regardless of patients’ consent. The head administrator of HFCSH and JGH provided consent on behalf of the patients. In addition, a formal permission letter to conduct the data collection was obtained from the head administrator of HFCSH and JGH. The names and unique identification numbers of patients were kept confidential and anonymous in compliance with the Declaration of Helsinki.
Acknowledgment
In appreciation for their cooperation, the authors would like to thank the administrators of two hospitals and data collectors.
Author Contributions
All authors made a significant contribution to the work in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There was no funding source for the study.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Kearney P, Whelton M, Reynolds KJL, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi:10.1016/S0140-6736(05)17741-1
2. Vilela-Martin JF, Vaz-de-Melo RO, Kuniyoshi CH, Abdo ANR, Yugar-Toledo JC. Hypertensive crisis: clinical–epidemiological profile. Hypertens Res. 2011;34(3):367–371. doi:10.1038/hr.2010.245
3. Rodriguez MA, Kumar SK, De Caro M. Hypertensive crisis. Cardiol Rev. 2010;18(2):102–107. doi:10.1097/CRD.0b013e3181c307b7
4. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159–2219.
5. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. J Hypertens. 2003;42(6):1206–1252.
6. Desta DM, Wondafrash DZ, Tsadik AG, et al. Prevalence of hypertensive emergency and associated factors among hospitalized patients with hypertensive crisis: a retrospective cross-sectional study. Integr Blood Press Control. 2020;13:95.
7. Janke AT, McNaughton CD, Brody AM, Welch RD, Levy PD. Trends in the incidence of hypertensive emergencies in US emergency departments from 2006 to 2013. J Am Heart Assoc. 2016;5(12):e004511.
8. Shao PJ, Sawe HR, Murray BL, Mfinanga JA, Mwafongo V, Runyon MS. Profile of patients with hypertensive urgency and emergency presenting to an urban emergency department of a tertiary referral hospital in Tanzania. BMC Cardiovasc Disord. 2018;18(1):1–7.
9. O’Brien E, Beevers DG, Marshall HJ. ABC of Hypertension: Eoin O’Brien, D. Gareth Beevers, Howard J. Marshall: Birtish Medical Journal publishing group; 1996.
10. Gebremichael GB, Berhe KK, Zemichael TM. Uncontrolled hypertension and associated factors among adult hypertensive patients in Ayder comprehensive specialized hospital, Tigray, Ethiopia, 2018. BMC Cardiovasc Disord. 2019;19(1):121. doi:10.1186/s12872-019-1091-6
11. Eyeberu A, Shore H, Getachew T, Atnafe G, Dheresa M. Neonatal mortality among neonates admitted to NICU of Hiwot Fana specialized university hospital, eastern Ethiopia, 2020: a cross-sectional study design. BMC Pediatr. 2021;21(1):1–9. doi:10.1186/s12887-021-02598-z
12. Gebresillassie BM, Debay YB. Characteristics, treatment, and outcome of patients with hypertensive crisis admitted to University of Gondar Specialized Hospital, northwest Ethiopia: a cross‐sectional study. J Clin Hypertens. 2020;22(12):2343–2353. doi:10.1111/jch.14056
13. Nakalema I, Kaddumukasa M, Nakibuuka J, Okello E, Sajatovic M, Katabira E. Prevalence, patterns and factors associated with hypertensive crises in Mulago hospital emergency department; a cross-sectional study. Afr Health Sci. 2019;19(1):1757–1767. doi:10.4314/ahs.v19i1.52
14. Pinna G, Pascale C, Fornengo P, et al. Hospital admissions for hypertensive crisis in the emergency departments: a large multicenter Italian study. PLoS One. 2014;9(4):e93542. doi:10.1371/journal.pone.0093542
15. Abdallah T, Ibrahem AA, Ali EA, Ahmed EG, Ali A. Clinico-epidemiological characteristics and survival outcome of patients with hypertensive crisis at Kassala Hospital, Eastern Sudan. J Crit Care Med. 2018;3:029–34.
16. Kadima JN, Bavhure B, Sepa JD, Murhura D. Hypertensive urgencies or emergencies and co-morbidities in Bukavu Referral Hospitals: clinical profile, management regimens, outcomes and drug related problems. J Basic Clin Pharm. 2018;9(1):1.
17. Elijovich F, Laffer CL. Acute Stroke: Lower Blood Pressure Looks Better and Better. American Heart Association; 2010:808–810.
18. Slama M, Modeliar SS. Hypertension in the intensive care unit. Curr Opin Cardiol. 2006;21(4):279–287. doi:10.1097/01.hco.0000231396.56738.d8
19. Cerrillo MR, Hernández PM, Pinilla CF, Claros NM, Otero ML. Hypertensive crises: prevalence and clinical aspects. Rev Clin Esp. 2002;202(5):255–258. doi:10.1016/S0014-2565(02)71046-1
20. Kotruchin P, Pratoomrat W, Mitsungnern T, Khamsai S, Imoun S. Clinical treatment outcomes of hypertensive emergency patients: results from the hypertension registry program in Northeastern Thailand. J Clin Hypertens. 2021;23(3):621–627. doi:10.1111/jch.14119
21. Carey RM, Whelton PK; Committee* AAHGW. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association hypertension guideline. Ann Intern Med. 2018;168(5):351–358. doi:10.7326/M17-3203
22. Bender SR, Fong MW, Heitz S, Bisognano JD. Characteristics and management of patients presenting to the emergency department with hypertensive urgency. J Clin Hypertens. 2006;8(1):12–18. doi:10.1111/j.1524-6175.2005.04898.x
23. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). J Am Med Assoc. 2014;311(5):507–520. doi:10.1001/jama.2013.284427
24. Saguner AM, Dür S, Perrig M, et al. Risk factors promoting hypertensive crises: evidence from a longitudinal study. Am J Hypertens. 2010;23(7):775–780. doi:10.1038/ajh.2010.71
25. Wu P-H, Yang C-Y, Yao Z-L, Lin W-Z, Wu L-W, Chang -C-C. Relationship of blood pressure control and hospitalization risk to medication adherence among patients with hypertension in Taiwan. Am J Hypertens. 2010;23(2):155–160. doi:10.1038/ajh.2009.210
26. Tisdale JE, Huang MB, Borzak S. Risk factors for hypertensive crisis: importance of out-patient blood pressure control. Fam Pract. 2004;21(4):420–424. doi:10.1093/fampra/cmh412
27. Zampaglione B, Pascale C, Marchisio M, Cavallo-Perin P. Hypertensive urgencies and emergencies: prevalence and clinical presentation. Hypertension. 1996;27(1):144–147. doi:10.1161/01.HYP.27.1.144
28. Husain RAA-BAAA. Hypertensive crisis: clinical presentation, comorbidities, and target organ involvement. Saudi Med J. 2010;31(8):916–920.
29. Lip G, Beevers M, Beevers DG. Complications and survival of 315 patients with malignant-phase hypertension. J Hypertens. 1995;13(8):915–924. doi:10.1097/00004872-199508000-00013
30. Varon J, Marik PE. Clinical review: the management of hypertensive crises. Crit Care. 2003;7(5):1–11. doi:10.1186/cc2351
31. Ipek E, Oktay AA, Krim SR. Hypertensive crisis: an update on clinical approach and management. Curr Opin Cardiol. 2017;32(4):397–406.
32. Varon J, Marik PE. The diagnosis and management of hypertensive crises. Chest. 2000;118(1):214–227.
33. Varon J. The diagnosis and treatment of hypertensive crises. Postgrad Med. 2009;121(1):5–13.
34. Elliott WJ. Clinical features in the management of selected hypertensive emergencies. Prog Cardiovasc Dis. 2006;48(5):316–325.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
