Back to Journals » Clinical Ophthalmology » Volume 16
Treatment of Corneal Irregularity in Radial/Astigmatic Keratotomy Patients Utilizing WaveLight Contoura
Authors Motwani M
Received 13 July 2021
Accepted for publication 26 October 2021
Published 11 January 2022 Volume 2022:16 Pages 111—126
DOI https://doi.org/10.2147/OPTH.S328050
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Manoj Motwani
Motwani LASIK Institute, San Diego, CA, 92121, USA
Correspondence: Manoj Motwani
Motwani LASIK Institute, 4520 Executive Dr., Suite 230, San Diego, CA, 92121, USA
Tel +1 858 554-0008
Email [email protected]
Purpose: To demonstrate the treatment of radial keratotomy-induced corneal irregularity with topographic-guided ablation (WaveLight Contoura).
Methods: Thirty-two eyes of 18 patients were treated for corneal irregularity post-radial keratotomy with WaveLight Contoura topographic-guided ablation utilizing LASIK and PRK and the San Diego Protocol for reconstructing corneas. These eyes were followed for six-months. Outcomes included: measurements of vision, refraction, residual higher-order aberrations, residual lower-order and higher-order aberrations, as well as loss or gains of lines of best-corrected visual acuity.
Results: All eyes had decreased corneal irregularity as evidenced by topographic analysis and reduction in manifest astigmatism, Contoura-measured astigmatism, higher-order aberrations, and higher-order aberrations grouped with lower-order aberrations excluding tilt (Grouped). The eyes of 5 sample patients are included in this manuscript to demonstrate the procedure, protocol, and outcomes.
Conclusion: Treatment with WaveLight Contoura whether as LASIK or PRK appears to be an effective treatment for corneal irregularity associated with radial/astigmatic keratotomy.
Keywords: WaveLight Contoura, topographic-guided ablation, LASIK, PRK, uniform cornea, measured astigmatism, radial keratotomy
Introduction
Radial keratotomy (RK) was a refractive surgical procedure for treatment of myopia developed by Svyatoslav Fyodorov of Russia in 1974.1,2 It uses radial corneal incisions (sometimes hexagonal for hyperopia) from the periphery of the cornea toward the central cornea that cause central flattening of the cornea for refractive affect.3 Due to the inexact, hand-made nature of the incisions, as well as slow and variable healing, irregular astigmatism is often present and the refractive effect can change over time. These patients can also suffer from poor night vision, variable vision, blurry vision and multiple images from often severe irregular astigmatism.3
This procedure was popular in the 1980’s in the United States,4,5 and continued to be utilized into the 2000’s in some parts of the world such as China.6 As patients have aged, many have had progressive hyperopia and worsening irregularity compounded by the onset of presbyopia.3 In some cases, the patients end up with debilitating levels of refractive error, poor vision, and multiple images.
This study demonstrates the results of treatment of the corneal irregularity and refractive error with topographic guided ablation utilizing the WaveLight Contoura System and the San Diego Protocol for reconstructive repair of corneas.
Materials and Methods
We retrospectively examined patients that had topographic guided ablation for their RK utilizing WaveLight Contoura (also termed T-CAT in this paper for brevity) and also had at least 6 months of follow-up results. We were able to analyze data from 32 eyes of 18 patients. All of these eyes had multiple radial incisions varying from 4 incisions to 16 incisions, and many also had astigmatic keratotomy (AK) incisions. LASIK flaps were created on 23 eyes, and PRK was performed on 9 of these eyes. Calculations were performed utilizing the San Diego Protocol for corneal reconstructive repair.7,8
LASIK flaps were made with Moria M2 microkeratome (Moria Inc; Besse, France) with Microspecialties (Micro Specialties Inc; Middletown, CT) microkeratome blades calibrated to 110 micron bed depth. For PRK, epithelium removal was performed via 20% alcohol solution placed on the corneal surface via 8 mm corneal well for 30 seconds, or by PTK utilizing the Nidek EC-5000 excimer laser. Manual removal of the epithelium was performed using a cellulose sponge and/or corneal epithelial scraper.
WaveLight Contoura was used to treat the corneal higher-order aberrations and irregular astigmatism of the anterior cornea. Surgical planning utilized the measured astigmatism up to the maximum 3 diopters allowed in the Contoura Food and Drug Administration (FDA) approval, with zero spherical correction due to refractive spherical power changes that occur with treatment of corneal irregularity.
Patients were counseled that the initial Contoura procedure would treat astigmatism/corneal irregularity and likely result in a significant power change even though no spherical correction would be performed. They were also told a second procedure would then correct the eyes to the desired refractive goal, whether Plano was achieved for distance or a nearsighted goal to treat presbyopia via monovision. Second enhancement procedures to treat residual refractive error were performed with Wavefront Optimized ablation 3 to 6 months after the original topographic guided ablation. All post-operative results in this paper include second enhancement procedures to adjust powers as necessary.
Unfortunately, the 5- and 5.5-mm optical zones for Contoura are not available in the United States so the smallest zone that can be used is 6 mm. Due to the high level of irregularity in many RK eyes, obtaining 6-mm wide Topolyzer Vario (Alcon Inc, Ft. Worth, TX) maps can be difficult, and some patients required multiple visits and treatment to optimize the corneal epithelium to obtain scans to allow treatment. In some patients, we have taken dozens to over one hundred plus images to obtain 6.0-mm scans.
Once corneal ablation was complete, 0.2 mg/cc mitomycin C (MMC) was applied for 20 secs to each laser-treated eye utilizing an 8-mm corneal shield. Corneal irrigation was performed after MMC placement with balanced salt solution.
All topographic guided ablation procedures were performed on the WaveLight EX500 (WaveLight Inc: Erlangen, Germany) excimer laser. All procedures were performed by one surgeon (MM) at one center in San Diego, California. All topographies were obtained utilizing the Topolyzer Vario (Alcon Surgical, Fort Worth, TX). All epithelial thickness maps (ETM) were obtained with the Optovue iVue (6-mm ETM) or Avanti (9-mm ETM) devices (Optovue, Fremont, CA).
Post-operative care consisted of prednisolone acetate 1% (generic) qid for 1 week, ofloxacin 0.3% (generic) qid x 1 week, and Prolensa qd PRN for pain during epithelial healing in PRK patients. Bandage contact lenses were placed overnight in all patients, and until the epithelial abrasion was healed in PRK patients. Fluorometholone ophthalmic suspension 0.1% (generic) was used bid x 5 weeks after the first week to prevent haze. Late in the treatment of this patient cohort, a switch was made to utilizing fluorometholone bid through the entire 6 week post-op period.
All patients signed written informed consent forms allowing their data to be used in this study. This study falls under the exemption of the Health and Human Services (HHS) Policy for the Protection of Human Research Subjects 45 CFR 46.104 for retrospective studies, and thus, no Institutional Review Board approval was required.9 This study also conforms to the Declaration of Helsinki guidelines.10 There were no safety-related incidents that occurred or were reported to Alcon Inc. or WaveLight during this trial.
Results
32 eyes of 18 patients are included in this study from 14 men and 4 women. The average patient age was 62 years, range 45 to 80 years. All patients had RK performed in the 1980s or 1990s.
Table 1 shows K values from the Topolyzer pre- and post-op, as well as K Max and K Mean. It also shows the reduction in Manifest and Contoura-measured cylinder.
 |
Table 1 Refractive Parameters |
In Table 2, Zernike polynomials are presented for 4th order higher-order aberrations (HOA), and also for Grouped polynomials includes lower-order aberrations (does not include tilt). Overall reduction of aberrations for all eyes was 52% for HOA and 39.7% for the Grouped values. All eyes had a reduction in HOA and Grouped values from pre-op to post-op.
 |
Table 2 Zernicke Polynomials |
One-tailed and two-tailed T tests were performed to look for statistical significance between comparisons of pre-op to post-op HOA values and Grouped values were statistically significant. It was determined that they were statistically significant. HOA tests resulted in p values of 0.0000084 and 0.000016 for the one- and two-tailed tests, respectively. Grouped tests resulted in p values of 0.00005158 and 0.000104.
Gains and loss of lines of vision of best-corrected visual acuity:
3 eyes lost 1–2 lines of vision (9.38%): 2 eyes of the same patient lost lines of vision – 2 lines in one eye, and 1 line in the other eye. 1 eye of one other patient lost 1 line of vision.
17 eyes gained 1–4 lines of vision (53.1): (9 eyes gained 1 line, 3 gained 2 lines, 3 gained 3 lines, and 1 gained 4 lines, 1 eye gained 7 lines of vision)
12 eyes achieved best-corrected visual acuity (BCVA) post-operatively equal to pre-op (37.5%).
The results of Case 1, a 54-year-old male with S/P RK in both eyes, are shown in Figures 1A–C, 2A and B, 3A–C, 4A and B and Tables 3–6.
 |
Table 3 Case 1 OD: 54-Year-Old Male S/P RK in Both Eyes |
 |
Table 4 Case 1 OD: 54-Year-Old Male S/P RK in Both Eyes |
 |
Table 5 Case 1 OS: 54-Year-Old Male S/P RK in Both Eyes |
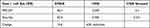 |
Table 6 Case 1 OS: 54-Year-Old Male S/P RK in Both Eyes |
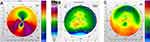 |
Figure 1 (A–C) Case 1, right eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
 |
Figure 2 (A and B) Case 1, right eye. Pre-op optical coherence tomography (OCT)/Post-op OCT. |
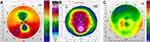 |
Figure 3 (A–C) Case 1, left eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
The findings from CASE 2, a 69-year-old female with S/P RK in both eyes, are provided in Figures 5A–C, 6A and B, 7A–C, 8A and B and Tables 7–10.
 |
Table 7 Case 2 OD: 69-Year-Old Female S/P RK in Both Eyes |
 |
Table 8 Case 2 OD: 69-Year-Old Female S/P RK in Both Eyes |
 |
Table 9 Case 2 OS: 69-Year-Old Female S/P RK in Both Eyes |
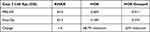 |
Table 10 Case 2 OS: 69-Year-Old Female S/P RK in Both Eyes |
The results from CASE 3, a 66-year-old male with S/P RK in both eyes, are shown in Figures 9A–C, 10A, 11A–C, 12A and Tables 11–14.
 |
Table 11 Case 3 OD: 66-Year-Old Male S/P RK in Both Eyes |
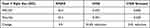 |
Table 12 Case 3 OD: 66-Year-Old Male S/P RK in Both Eyes |
 |
Table 13 Case 3 OS: 66-Year-Old Male S/P RK in Both Eyes |
 |
Table 14 Case 3 OS: 66-Year-Old Male S/P RK in Both Eyes |
The findings from CASE 4, involving a 67-year-old male with S/P RK in both eyes, are provided in Figures 13A–C, 14A, 15A–C, 16A and Tables 15–18.
 |
Table 15 Case 4 OD: 67-Year-Old Male S/P RK in Both Eyes |
 |
Table 16 Case 4 OD: 67-Year-Old Male S/P RK in Both Eyes |
 |
Table 17 Case 4 OS: 67-Year-Old Male S/P RK in Both Eyes |
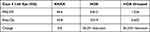 |
Table 18 Case 4 OS: 67-Year-Old Male S/P RK in Both Eyes |
The outcomes from CASE 5, a 61-year-old female with S/P RK in both eyes, are shown in Figures 17A–C, 18A and B, 19A–C, 20A and B and Tables 19–22.
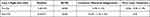 |
Table 19 Case 5 OD: 61-Year-Old Female S/P RK in Both Eyes |
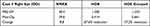 |
Table 20 Case 5 OD: 61-Year-Old Female S/P RK in Both Eyes |
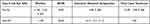 |
Table 21 Case 5 OS: 61-Year-Old Female S/P RK in Both Eyes |
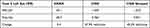 |
Table 22 Case 5 OS: 61-Year-Old Female S/P RK in Both Eyes |
Discussion
The treatment of irregular astigmatism with topographic-guided ablation utilizing the San Diego Protocol7 has been extremely effective not only for the creation of more regular corneas and treatment of extreme refractive errors but also for the restoration of vision in patients with severe corneal irregularity that had been unable to be treated successfully with other vision correction modalities or procedures. This is demonstrated by the striking differences between pre- and post-procedure topographies shown in the sample cases. Radial keratotomy by the nature of hand-made incisions will almost always lead to some level of corneal irregularity and higher-order aberrations, and there seems to be a hyperopic shift that occurs over years.
One of the most striking phenomena of the treatment of corneal irregularity was the change in spherical power after correction of the corneal HOA and astigmatism. In most eyes, this normalization of the cornea would lead to a fairly significant spherical power change with usually a reduction in hyperopia. The critical takeaway from this is that the high refractive errors in RK patients are partially caused by the multi-focal nature of the irregular cornea, and normalization of the cornea resulted in often dramatic reductions in spherical refractive errors. This indicates that excimer laser treatment of the actual refractive error without treatment of the corneal HOA is not the correct treatment choice, as in many cases a significant portion of the refractive error is coming from the corneal irregularity. Patients were counseled prior to the initial surgery that this would be a two-part procedure, with a second excimer laser correction utilizing WaveLight Wavefront Optimized (WFO) treatment occurring 4 to 6 months after the initial procedure.
Initially, corrections were performed with LASIK flaps if possible, and re-lifting of the flaps for the second planned correction was possible by simply dissecting along each incision from the center inwards with a blunt flap dissector even after several months. Although there was some concern for scarring and haze with utilizing surface ablation procedures for large corneal HOA corrections, the use of 20 seconds of MMC prevented significant haze in virtually of these cases. Haze and scarring have been minimal problems overall. This allowed for greater confidence as we transitioned into treating larger corrections, and corrections with transepithelial topo-guided PRK (case 5). We believe this latter procedure may be the ideal for RK reconstructive corneal repairs, as most of these eyes have large amount of epithelial compensation of their corneal irregularities, and the potential exists of creating more uniform corneas by accounting for the epithelial compensation as is evidenced by the topographies in case 5.
In patients where 6-mm Topolyzer scans could not be obtained, we have utilized trans epithelial PTK to grossly reduce corneal HOA by using the Nidek EC5000 laser in PTK and Optivue Optical coherence tomography (OCT) Epitheilal thickness mapping to determine the amount of epithelial removal. This has been successful in treating the irregularity with eventual ability to get 6-mm Topolyzer scans.
This brings up the greatest difficulty we had in treating RK eyes – obtaining 6-mm Topolyzer Vario scans. In almost all eyes, it is possible to obtain 5- or 5.5-mm scans, but obtaining 6-mm scans required for Contoura treatment are much more difficult. In some patients, we had to optimize the epithelial surface, take dozens of scans over multiple sessions to obtain even one 6-mm Topolyzer Vario scan. The staff and the patient have literally spent hours trying to obtain 6-mm scans on some patients, which did result in successful treatments, but the ability to use smaller optical zones with WaveLight Contoura would make this process dramatically easier. It has been unclear as to why Alcon/WaveLight will not allow smaller treatment zones (5.0- and 5.5-mm) with Contoura that were not expressly included in the FDA trial studies. In the Wavefront Optimized software, non-approved treatment zones are allowed with a warning that data was not available on them, but for some reason in this critical area of need these zones are locked out. It is even more puzzling since many past studies performed with repairing corneal irregularity utilized 5.0-mm zones. We strongly urge Alcon/WaveLight to allow the usage of the 5.0- and 5.5-mm treatment zones with Contoura in the US as an off-label procedure so that we can continue to not only aid patients but to decrease the amount of time that staff and patients must spend just to satisfy a 6.0-mm treatment zone.
Three eyes lost lines of best visual acuity. One patient lost a line of visual acuity in one eye, and this was due to surface epithelial compromise from dry eye/allergy combination. One other patient lost 2 lines BCVA in one eye and 1 line in the other eye. This patient had severe irregularity of his corneas, requiring multiple sessions to get scans, and then had an RK slit leak in one of his eyes requiring a suture be placed. This patient may have improved further over time, but was lost to follow-up at 9 months. All other eyes either achieved post-op BCVA equal to pre-op, or gained lines of vision.
Table 1 lists topographic K values pre- and post-operatively. It is notable how the post-op K1 and K2 values difference decreases and how the manifest cylinder also decreases post-op to only −0.32 (these results are after any second treatment with WFO as necessary). The final corneal spherical power is not dissimilar to the pre-op power, as demonstrated by the K mean which demonstrates that the original RK did have the planned refractive effect only with corneal irregularity.
Table 2 shows pre- and post-operative higher-order aberration values in microns for 6th order HO and also for the Grouped category which includes lower-order values but does not include tilt or piston. Post-operative HOA are reduced by an average of 52% and the Grouped category is reduced by an average of 46% for all eyes treated. The reduction of corneal HOA in some eyes was quite dramatic, as in 2 of the sample eyes above that had an 80% reduction of HOA post-operatively.
Before discussing the individual sample cases, case 3 and case 4 initial procedures were performed before OCT epithelial thickness mapping by Optovue was available so pre-op epithelial maps are not available.
Case 1
Case 1 shows the treatment for right (Figures 1 and 2) and left (Figures 3 and 4) eyes. This patient had severe corneal irregularity as evidenced by his high refractive error in both of his eyes, his very high pre-op HOA of 2.741 Left eye (OD)/2.049 Right eye (OS), as well as his best-corrected vision of only 20/40 in both of his eyes. This patient had large Contoura-measured astigmatism pre-operatively in both eyes, and large amounts of residual astigmatism correction that was corrected during the second WFO procedure. His corneal HOA was reduced a remarkable 77% OD and 63% OS and he ended up with 20/20 uncorrected vision in both eyes with a plano refraction. The change to his topographies pre-operatively to post-operatively is notable as well.
 |
Figure 4 (A and B) Case 1, left eye. Pre-op OCT/post-op OCT. |
Case 2
Case 2 shows the treatment for right (Figures 5 and 6) and left (Figures 7 and 8) eyes. This case shows dramatic decrease in irregularity on topography of both corneas, with 80% and 69% reduction in corneal HOA in OD and OS, respectively. Post-op corneal HOA were also very low at 0.128 and 0.189 microns OD and OS, respectively. This patient had other non-corneal (retinal) factors that limited the vision to 20/40 OS, but did achieve 20/25 and 20/40 vision uncorrected after 2 small WFO corrections OD and 1 small WFO correction OS. The OS topography is notable as the residual irregularity matches the pattern of epithelial thinning on OCT ETM, and this may well indicate that transepithelial treatment may have helped her further.
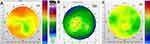 |
Figure 5 (A–C) Case 2, right eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
 |
Figure 6 (A and B) Case 2, right eye. Pre-op OCT/Post-op OCT. |
 |
Figure 7 (A–C) Case 2, left eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
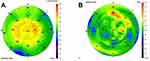 |
Figure 8 (A and B) Case 2, left eye. Pre-op OCT/Post-op OCT. |
Case 3
Case 3 demonstrates another significant change in topographic shape, and shows the characteristic hyperopic ablation shape from the second refractive correction in both eyes (Figures 9–12). Again it is interesting to note that this is not a smooth hyperopic ablation shape, as there is still some irregularity left likely due to epithelial compensation of the aberration pre-operatively preventing full measurement of the corneal HOA. The OD eye is also notable for having an obviously irregular shape on topography, but did not have a high level of corneal HOA pre-operatively so the reduction in HOA was not large. This demonstrates the limitation of utilizing only numerical corneal data to show irregularity, as visualization of the corneal topography demonstrates a more significant change to the cornea than the reduction in HOA would indicate. The OS eye shows a dramatic reduction in corneal HOA (80%), and residual HOA is only 0.133. This patient was elderly and the 20/25 vision in the OS was due to retinal visual limitation. As mentioned prior, no OCT ETM was available for this patient.
 |
Figure 9 (A–C) Case 3, right eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
 |
Figure 10 Case 3, right eye. Post-op OCT. |
 |
Figure 11 (A–C) Case 3, left eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
 |
Figure 12 Case 3, left eye. Post-op OCT. |
Case 4
This patient is notable for the large drop in refractive error with the first treatment of only the corneal HOA and Contoura-measured astigmatism (maximum treatable is −3.00D) (Figures 13–16). There is again a significant change to the topographic shape of the cornea with a decrease in irregularity, and a significant decrease in cornea HOA, less so in the OS eye. An additional note was the patient was seen almost 5 years after initial procedure as this paper was being finished for an unrelated problem, and was found to be stable for both refraction and vision, which had improved to 20/20 in the distance eye, and was correctable to 20/20 in the monovision eye. The patient was doing well overall without complaints.
 |
Figure 13 (A–C) Case 4, right eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
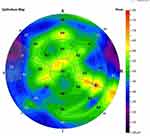 |
Figure 14 Case 4, right eye. Post-op OCT. |
 |
Figure 15 (A–C) Case 4, left eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
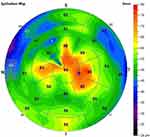 |
Figure 16 Case 4, left eye. Post-op OCT. |
Case 5
This case is notable for being a transepithelial topographic guided PRK procedure. OCT ETM was used to determine epithelial thickness, and the Nidek EC-5000 was used to remove the epithelial tissue down to the intended depth thereby using the epithelium as a mask to treat corneal irregularity that the Topolyzer cannot measure due to epithelial compensation. This patient does have retinal membrane issues as well as cataract formation that limit her vision to 20/40 even with the much more regular corneas post-treatment. The topographies are notable for a more regular, uniform shape than prior the other sample cases, as well as some level of decrease of epithelial thickening in the post-operative ETM, more so in the OD than the OS (Figures 17–20). This decrease in epithelial thickening is demonstrative of a decrease in corneal aberration that incites epithelial compensation.
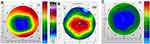 |
Figure 17 (A–C) Case 5, right eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
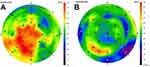 |
Figure 18 (A and B) Case 5, right eye. Pre-op OCT/ Post-op OCT. |
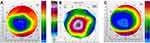 |
Figure 19 (A–C) Case 5, left eye. Pre-op Topolyzer/Pentacam pachymetry/Post-op Topolyzer. |
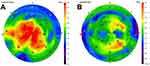 |
Figure 20 (A and B) Case 5, left eye. Pre-op OCT/Post-op OCT. |
Treatment utilizing transepithelial Contoura PRK has now become our favored treatment of RK eyes, as they all show large amounts of corneal epithelial compensation of corneal irregularity. This will be formally reported on in a future manuscript as more data is accumulated.
At this time, we see a limited to no role for corneal transplant in treating pos-RK eyes, as once Topolyzer Vario scans are obtained the treatment with topographic-guided ablation to reconstruct the cornea has excellent visual outcomes, especially with the transepithelial approach. In patients with high levels of corneal irregularity where 6-mm Topolyzer scans are unobtainable, it is possible to perform gross aberration reduction utilizing transepithelial decrease aberration that the epithelium is masking, thereby making a more regular surface that can eventually be scanned by the Topolyzer. Again, allowing a 5-mm treatment zone with Contoura would be greatly helpful.
Another need is a PTK treatment mode for the WaveLight EX500 laser. Although a PRK WFO approval was obtained by Alcon/WaveLight, the PTK mode FDA approval was not obtained and such a mode would be very useful in many ways. The Nidek EC5000 PTK mode does not follow the corneal curvature so is only useful for the center of the cornea. Of course having a Contoura Lightstream transepithelial PRK mode on the WaveLight would be incredibly useful as well.
Although we did not subject these patients to quality of vision surveys, virtually all of these patients reported not only improved vision but also an improvement in visual disturbances such as glare, doubling, blurry, light sensitivity, and other visual disturbances common to RK patients. Some patients remarked it “was the best vision they had ever had.” This is very significant, as although refractive error has been treated via different modalities for RK, the reduction of these visual disturbances is one of the key factors motivating RK patients to seek treatment.
Overall, treatment of RK-induced corneal irregularity with topographic guided ablation utilizing the San Diego Protocol has proven itself to be safe, effective, and has the potential to provide significant visual gain for the patient.
Acknowledgments
The author would like to thank Julie Crider, PhD, for medical editing contributions.
Disclosure
Dr Manoj Motwani reports patents issued (US patent nos. 10,857,032 and 10,857,033) that consist of the usage of topographic measured astigmatism to make a uniform cornea and the analysis and treatment of epithelial compensation during excimer laser treatment. The author reports no other conflicts of interest in this work.
References
1. Fyodorov SN, Durnev VV. Operation of dosaged dissection of corneal circular ligament in cases of myopia of mild degree. Ann Ophthalmol. 1979;11(12):1885–1890.
2. Tannebaum S. Svyatoslav Fyodorov, M.D.: innovative eye surgeon. J Am Optom Assoc. 1995;66(10):652–654.
3. Fu L, Patel BC. Radial Keratotomy Correction. Treasure Island (FL): StatPearls; 2021.
4. Radial keratotomy for myopia. American Academy of Ophthalmology. Ophthalmology. 1989;96(5):671–687. doi:10.1016/S0161-6420(89)32849-1
5. Assessment OP. Radial keratotomy for myopia. American Academy of Ophthalmology. Ophthalmology. 1993;100(7):1103–1115. doi:10.1016/S0161-6420(13)31536-X
6. Zhang JS, Liu X, Wang JD, et al. Outcomes of phacoemulsification using different size of clear corneal incision in eyes with previous radial keratotomy. PLoS One. 2016;11(12):e0165474. doi:10.1371/journal.pone.0165474
7. Motwani M. A protocol for topographic-guided corneal repair utilizing the US Food and Drug Administration-approved Wavelight Contoura. Clin Ophthalmol. 2017;11:573–581. doi:10.2147/OPTH.S127855
8. Motwani M. Biomechanical changes to the cornea from LASIK flap creation resulting in inaccurate ablations and suboptimal refractive outcomes with topographic-guided ablation. Clin Ophthalmol. 2020;14:2319–2327. doi:10.2147/OPTH.S263896
9. Electronic Code of Federal Regulations. Part 46-exempt research. 46.104. Available from: https://www.law.cornell.edu/cfr/text/6/46.104.
10. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
