Back to Journals » Journal of Pain Research » Volume 13
Treatment Expectations Towards Different Pain Management Approaches: Two Perspectives
Authors Schemer L, Rief W , Glombiewski JA
Received 29 January 2020
Accepted for publication 23 May 2020
Published 9 July 2020 Volume 2020:13 Pages 1725—1736
DOI https://doi.org/10.2147/JPR.S247177
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert B. Raffa
Lea Schemer,1 Winfried Rief,2 Julia A Glombiewski1
1Department of Clinical Psychology and Psychotherapy, University Koblenz - Landau, Landau 76829, Germany; 2Department of Clinical Psychology and Psychotherapy, Philipps-University Marburg, Marburg 35032, Germany
Correspondence: Lea Schemer
Department of Clinical Psychology and Psychotherapy, University Koblenz – Landau, Ostbahnstraße 10, Landau 76829, Germany
Tel +49 6341 280-35627
Email [email protected]
Purpose: Accumulating evidence suggests an association between patient expectations and treatment success across various types of pain treatments. Expectations among treatment caregivers, however, are often neglected. Despite international treatment guidelines, only a small minority of chronic pain patients undergo psychological interventions. Therefore, our aim was to explore expectations among treatment receivers and caregivers especially concerning their attitudes towards psychological pain treatments.
Methods: Two hundred ten (potential) treatment receivers (n=85 individuals suffering from chronic low back pain (CLBP); n=125 healthy controls) and 237 caregivers (n=75 physicians; n=64 psychotherapists; n=98 physiotherapists) provided ratings of expected treatment success for standardized vignettes describing patients suffering from CLBP and undergoing a pharmacological, psychological, or multimodal pain management program.
Results: Individuals suffering from CLBP generally had lower treatment expectations than healthy controls. Both psychotherapists and physicians had higher treatment expectations from their own individual treatment approach. All participants expected the multimodal approach to be most effective. The psychological approach was expected to be more effective than the pharmacological approach – except for the physicians, who expected both treatment approaches to be equally effective.
Conclusion: There is an urgent need to clarify, under which circumstances and how patient expectations can be altered among individuals suffering from CLBP. Our results appear to encourage the implementation of multimodal and psychological pain management approaches across various settings. We invite clinicians to reflect whether their own expectations are in line with the recommendations in international treatment guidelines.
Keywords: treatment expectations, chronic pain management approaches, psychological pain treatments, attitudes of treatment receivers and caregivers
Introduction
Chronic low back pain (CLBP) is one of the three leading causes for years lived with disability worldwide.1 Treatment guidelines usually recommend conservative treatment approaches over invasive interventions (eg, injections, surgery).2 Psychological pain therapies and multidisciplinary programs are considered especially effective. These were the only two treatment approaches recommended in all the guidelines from 15 countries.3 There is, however, evidence that approximately half of the patients suffering from chronic pain undergo monotherapy. Only 10% of patients receiving combination therapy participate in psychological pain treatments.4 There is thus a tremendous gap between treatment guidelines and their implementation in routine medical care.
Expectations are hypothesized to influence treatment outcome regardless of the treatment approach being delivered.5,6 The conceptual definitions of general health care expectations have been differentiated into four categories:7,8 a) predictive expectations represent individual beliefs about the amount of improvement to be expected after treatment, b) ideal expectations represent individual hopes and desires about the best possible treatment outcome, c) normative expectations represent personal beliefs about required treatment elements supposedly offered during treatment, and d) unformed expectations represent attitudes that are either implicit or not yet formed due to the lack of prior experience. So far, most research has focused on the influence of predictive expectations on treatment outcome. For example, one study found that expected pain relief and expected improvement in quality of life were significant predictors of treatment outcome of multidisciplinary pain treatments. Expected improvement in functioning was unrelated to treatment outcome however.9 Which kind of expectations and under which circumstances they are predictive of improved treatment outcome appears to be complex. Yet accumulating evidence suggests an association between patients’ expectations and treatment outcome across various types of pain treatment. Nijs and colleagues therefore recommend assessing patients’ attitudes and beliefs before delivering a specific pain treatment.10 Their assessment enables tailored educational programs to be implemented prior to the intervention in case of unfavorable expectations.
Negative expectations might be one reason why patients in standard medical care do not seek treatment approaches recommended by international treatment guidelines. At the same time, that appears to be only one side of the story. The other, often relatively neglected side is the attitudes and expectations of treatment caregivers. A systematic review found strong evidence for the relationship between attitudes of patients with back pain and their healthcare professionals, namely chiropractors, general practitioners, orthopedic surgeons, physiotherapists, and rheumatologists.11 For example, a biomedical orientation and elevated fear-avoidance beliefs among treatment caregivers was associated with neglecting the adherence to treatment guidelines and recommendation of limited work and physical activities. Attitudes and expectations of treatment caregivers might therefore be a further substantial reason why patients do not undergo the treatment in routine medical care as recommended in international treatment guidelines.
The goal of the present study was to investigate predictive treatment expectations from two different perspectives. (Potential) treatment receivers (individuals suffering from chronic low back pain, healthy controls) and caregivers (physicians, psychotherapists, physiotherapists) provided ratings of expected treatment success for standardized vignettes describing patients suffering from chronic low back pain and undergoing a pharmacological, psychological, or multimodal pain management program. From our results, we hope to deepen the understanding of treatment expectations by bridging the gap between the attitudes of treatment receivers and caregivers, especially towards psychological pain treatments.
Participants and Methods
Participants
Participants were recruited via local support groups, specialist group conferences, inpatient and outpatient treatment centers, specialist training institutes, related internet platforms and regional associations. All participants were informed about the study procedure via an information sheet. They gave written consent about participating. The study procedure was approved by the institutional ethics committee of the psychology department at the Philipps-University Marburg (2016–43k). The study was conducted in accordance with the Declaration of Helsinki. Inclusion criteria for caregivers were occupational status (>1 year) as a physician, psychotherapist, or physiotherapists. Treatment receivers were defined as individuals suffering from CLBP if they stated they had suffered from chronic back pain (>6 months) of at least moderate average pain intensity (>3 NRS) during the previous 4 weeks. If they stated they had suffered no back pain or only acute back pain (<6 months), we considered them as healthy controls. A total of n=530 participants completed the survey. Some participants were excluded from our later analyses for not meeting the inclusion criteria (n=53), missing values >50% (n=25), and/or for extreme values (n=5). Our final sample consisted of n=237 caregivers and n=210 treatment receivers.
Study Procedure
At the survey’s beginning, all participants (caregivers, treatment receivers) read three vignettes about different treatment approaches (pharmacological vs psychological vs multimodal) for the management of chronic low back pain. To rule out sequence effects, the vignettes were presented in randomized order. For each of these treatment approaches, participants had to rate their treatment expectation. Treatment receivers filled out additional questionnaires to assess their personal pain experience, pain-related disability, pain-related anxiety, and depressive symptoms. Caregivers provided information about their years of working experience, current work setting, and expertise in managing chronic pain. The study procedure is shown in Figure 1.
 |
Figure 1 Study procedure. CLBP, chronic low back pain; CEQ, Credibility Expectancy Questionnaire; PDI, Pain Disability Index; PASS, Pain Anxiety Symptom Scale; BDI, Becks Depression Inventory. |
Development of Vignettes
The vignettes were designed according to international guidelines.12 All vignettes shared certain features: they had similar lengths (∼ 200 words), were formulated in present tense (except for history and background information), the content followed a narrative, story-line progression, and their structure followed a similar scheme. First, it started with a description of a typical patient with chronic low back pain who reported to be suffering from low back pain due to a herniated disk, spinal canal stenosis, or spondylolisthesis. Despite successful surgery, this back pain persisted for unspecific reasons (5–8 years). All patients were presented as having a similar age (50–55 years old). Gender and type of previous medical conditions were balanced across the three different treatment approaches. Second, the diagnostic procedure within the given treatment approach was described. Third, the corresponding treatment goals were formulated. Fourth, the respective treatment elements were outlined in a detailed description. The first draft of each treatment approach’s vignette was written based on national treatment guidelines for chronic low back pain.13 Two experts adjusted the descriptions based on their clinical experience. An anesthetist and a psychologist, both specialists in chronic-pain management, provided comments and ideas for improvements. Lastly, a third expert on creating vignettes corrected the final descriptions.
Pharmacological Pain Management
The pharmacological approach’s vignette started with a detailed description of the pain anamnesis based on a medical examination and several pain questionnaires. This anamnesis identified the type of chronic pain as either neuropathic, inflammatory, or musculoskeletal. The subsequent pharmacological treatment goal was to reduce pain. Thus, the patient would be able to function better in daily life and better participate in physiotherapeutic and supplementary treatments. The following pharmacological treatment was tailored to the patient’s neuropathic pain. At the beginning, the patient received a prescription for Amitriptylin (antidepressant) and Pregabalin (antiepileptic). Both drugs were adjusted to avoid interaction effects possibly caused by the concurrent intake of a hypertension drug. The patient also received a recommendation for six physiotherapeutic sessions. After those physiotherapeutic sessions, the patient had another appointment with the anesthetist. The reaction to the newly prescribed medication was monitored for any improvements and negative side effects. The drug prescription plan was again adjusted to accommodate the patient’s complaints. If the drugs had shown no effect, it was possible to change the medication to opioids (eg, Tramadol). Furthermore, the patient was given two additional prescriptions for physiotherapeutic treatment (entailing six sessions each) and subsequent medical consultation.
Psychological Pain Management
The psychological approach’s vignette started with a detailed description of the diagnostic procedure based on several interviews and self-rating questionnaires. The intent of both methods is to assess individual dysfunctional cognitions, emotions, and behaviors that contribute to pain maintenance. The treatment goals were to reduce disability and to restore the patient’s quality of life. Moreover, the treatment’s intent was to expand upon the subjective understanding of chronic pain towards additional psychological processes. The description of the subsequent cognitive-behavioral therapy (with weekly appointments over about a year) entailed various treatment elements. During operant interventions, the patient learned to re-engage in previous activities (eg, garden work) by breaking those activities into smaller steps to avoid phases of excessive demands followed by long terms of recovery. At the same time, the patient learned to formulate concrete and realistic goals to purse essential life activities despite their chronic pain. During cognitive interventions, the patient learned to intentionally shift their attention away from pain. Moreover, the patient learned to distance herself or himself from dysfunctional cognitions (eg, “I try to avoid activities that intensify pain.”). During respondent interventions, the patient learned to deliberately relax their back with the help of biofeedback.
Multimodal Pain Management
The multimodal approach’s vignette started with a detailed description of the multidisciplinary diagnostic procedure, which entailed medical, physiotherapeutic, and psychological examinations. An individualized treatment plan was designed based on joint consultation involving all the disciplines engaged. The treatment goals were to reduce pain and pain-related disability. The patient should acquire a feeling of competence in managing pain. The patient would then be able to participate in his or her daily life again. The description of the following intensive care treatment (over 3 weeks) entailed various treatment elements from each discipline. During the medical treatment, the drug prescription plan was studied, making certain adjustments according to feedback from a detailed pain anamnesis. During the sport and exercise therapy (Nordic walking, specific back exercises), the patient was encouraged to engage in physical activities. Moreover, the patient was introduced to basic relaxation techniques. During group therapy sessions, the patient was given information on a biopsychosocial understanding of chronic pain. At the same time, the group could exchange experiences with others suffering from chronic pain. During individual therapy, the patient had the opportunity to reflect upon their own illness behavior and use their personal resources to better cope with chronic pain.
Measures
Treatment Expectancy
Treatment expectancy was considered a primary outcome and assessed via the Credibility Expectancy Questionnaire (CEQ).14 This questionnaire has two subscales. Three items measure cognitively based credibility (eg, ”How confident would you be recommending this treatment to a friend?”). Three additional items measure affectively based expectancy (eg, “How much improvement in the symptoms do you really feel will occur?”). The questionnaire applied two different scales, namely a 9-point scale (1 = not at all; 9 = very much) and a percentage rating scale (0% = not at all; 100% = very much), which were transformed to a common 9-point scale. In contrast to previous findings,14,15 a 1-factor solution best described item variance in our data for both treatment receivers and caregivers (see 3.2 Factor structure of CEQ). We therefore combined those two factors into a single scale. A higher sum score indicates higher treatment expectancy (6 = minimal index; 54 = maximum index).
Personal Pain Experience
Treatment receivers had to indicate their overall experience with pain (not only back pain, but all kinds of pain) on a 9-point scale (1= no experience, 9 = very much experience). Moreover, they were asked to indicate the kind of pain they were referring to. They were thus primed for their own personal experience with pain (both acute and chronic) when answering the subsequent pain-related questionnaires.
Pain-Related Disability
Pain-related disability was measured by the Pain Disability Index (PDI).16,17 Treatment receivers had to indicate their level of impairment of 7 essential life activities (e.g. Social activities: This category refers to activities with involve participating with friends and acquaintances other than family members. It includes parties, theater, concerts, dining out, and other social functions.) on an 11-point scale (0 = no impairment, 10 = complete impairment). A higher index indicates greater levels of disability (0 = minimal index, 70 = maximum index).
Pain-Related Anxiety
Pain-related anxiety was assessed by the Pain Anxiety Symptom Scale (PASS).18,19 Treatment receivers had to rate 20 items (eg, “I worry when I am in pain.”) regarding their frequency on a 5-point scale (0 = never, 4 = always). A higher sum score indicates a more severe degree of pain-related anxiety (0 = minimal index; 100 = maximum index).
Depressive Symptoms
Depressive symptoms were screened for via the Beck-Depressions-Inventory (BDI-FS).20,21 Treatment receivers had to select one statement from 7 groups of items which best described their emotional state on a 4-point scale (eg, 0 = “I do not feel sad.”; 3 = “I am so sad and unhappy that I can’t stand it.”). A higher sum score indicates higher level of depression (0 = minimal index; 21 = maximum index).
Experience with Back Pain
To differentiate between treatment receivers with and without chronic back pain, they had to indicate whether they had any experience (either through their own experience, through someone in their family, or through (close) friends with chronic back pain). Furthermore, they had to indicate whether they were then suffering from acute (yes/no) or chronic (>6 months) (yes/no) back pain. In case they indicated having back pain, they had to quantify their average pain intensity (0 = no pain, 10 = worst pain) and pain perception (0 = bearable, 10 = unbearable) during the previous four weeks on an 11-point scale.
Statistical Analyses
Analyses were conducted with the Statistical Package for Social Science (SPSS, Windows v.22: SPSS Inc, Chicago, IL). If criteria for univariate (z-score in excess of ± 3.29) and multivariate (Mahalanobis-distance criteria) outliers were met, data were not included (n=5). To ensure the comparability between groups (eg, regarding gender or years of work experience) and to be able to differentiate between them at the same time (eg, regarding sick leave status or level of disability), the sample characteristics were compared in a series of subsequent chi-square-tests (for categorical variables), t-tests and ANOVAS (for continuous variables). A principal axis analysis with oblique rotation (direct oblimin) was conducted to explore the factor structure of the CEQ among treatment receivers and caregivers. Several criteria were used to determine the number of factors. The Kaiser criterion specifies that factors must have eigenvalues greater than one. The parallel analysis allows the eigenvalues of a collected data set to be compared with the eigenvalues of a random data set.
Our primary hypotheses were analyzed via two-level linear mixed models. Analyses were run separately for treatment receivers and caregivers. To account for the repeated interrogation of the same individuals, we assumed random effects between individual participants (ie, autoregressive covariance structure). The influence of “treatment approach” and “group” were considered fixed effects. Full maximum likelihood estimation was used for all models. We followed a model building procedure. First, a model including main effects of “treatment approach” and “group” was compared to a model with no variables. Second, a model adding the interactional effect of “treatment approach x group” was compared to the first model. For the predictors of the mixed models, we set the level of statistical significance at p < 0.05. Significant predictors were further interpreted by subsequent post hoc tests with Bonferroni adjustment for multiple tests.
Results
Distinction and Comparability Between Groups
Treatment Receivers
As expected, patients reported significantly higher levels of disability (t (205) = 9.29, p < 0.001), more pain-catastrophizing thoughts (t (208) = 4.96, p < 0.001), and more depressive symptoms (t (140) = 7.78, p < 0.001) than the healthy controls. Treatment receivers differed in their sick leave (χ2(1) = 23.35, p < 0.001) and occupational status (χ2(5) = 38.38, p < 0.001) with more patients being on sick leave (29.4% vs 6.4%) or receiving a disability pension (31.8% vs 4.8%) than healthy controls. More patients reported having had experience with pharmacological (χ2(1) = 20.59, p < 0.001) psychological (χ2(1) = 7.73, p < 0.01), and multimodal (χ2(1) = 16.37, p < 0.001) pain treatment programs. In line with previous research,22 we noted significant group differences in the level of school (χ2(3) = 48.38, p < 0.001) and professional education (χ2(3) = 27.12, p < 0.001) with fewer patients stating they had a higher school degree (22.4% vs 68.8%) and/or a university degree (17.6% vs 49.6%) in comparison to healthy controls. Patients were significantly older than healthy controls (t (208) = 2.63, p < 0.01). The groups did not differ in their gender (χ2(1) = 1.23, p = 0.27). Taken together, patients and healthy controls were sufficiently distinct in the present sample (see Table 1).
 |
Table 1 Sample Characteristics for Treatment Receivers |
Caregivers
Treatment receivers did not differ in their gender (χ2(2) = 2.01, p = 0.37). Although there were group differences in being engaged in chronic back pain therapy (χ2(6) = 25.36, p < 0.001), most caregivers reported being somewhat involved in treating chronic low back pain among physicians (82.7%), psychologists (84.4%), and physiotherapists (82.7%). There were unexpected group differences in age (F[2, 234] = 11.70, p < 0.001) and years of working experience (F[2, 234] = 35.61, p < 0.001). While the physiotherapists were the oldest (M = 46.8, SD = 11.4) and had the most years of working experience (M = 23.5, SD = 0.11.4), psychotherapists were the youngest (M = 38.1, SD = 10.2) and had the fewest years of working experience (M = 9.5, SD = 8.6). However, neither age (r = 0.01) nor years of working experience (r = 0.01) were associated with treatment expectation ratings. These preexisting differences therefore appear irrelevant in terms of our analysis (see Table 2).
 |
Table 2 Sample Characteristics for Caregivers |
Factor Structure of CEQ
Treatment Receivers
Bartlett’s test of sphericity was significant (χ2(15) = 3507.40, p < 0.001) and the value of Kaiser-Meyer-Olkin measure of sampling adequacy was 0.86. Our data were therefore considered appropriate for use in principal axis analysis. The Kaiser criterion was met for a 1-factor solution (eigenvalue = 4.58). This eigenvalue was also greater than the eigenvalues of a random data set (eigenvalue = 0.20). The eigenvalue of a second factor (eigenvalue = 0.37) slightly exceeded eigenvalues of a random data set (eigenvalue = 0.12). However, this difference was rather small in comparison to a 1-factor solution. We therefore subsumed items into a single scale. The 1-factor solution explained 76.25% of the variance with factor loadings ranging from 0.81 to 0.90. The communalities of items ranged from 0.65 to 0.80. Internal consistency with Cronbach's α = 0.93 was excellent.
Caregivers
Bartlett’s test of sphericity was significant (χ2(15) = 5247,78, p < 0.001) and the Kaiser-Meyer-Olkin measure of sampling adequacy was 0.85. Our data were therefore considered appropriate for use in principal axis analysis. The Kaiser criterion was met for a 1-factor solution (eigenvalue = 4.65). This eigenvalue was also exceeded eigenvalues of a random data set (eigenvalue = 0.17). The eigenvalue of a second (eigenvalue = 0.45) slightly exceeded eigenvalues of a random data set (eigenvalue = 0.10). However, this difference was rather small in comparison to a 1-factor solution. We therefore subsumed the items into a single scale. The 1-factor solution explained 77.56% of the variance with factor loadings ranging from 0.78 to 0.91. The communalities of items ranged from 0.61 to 0.83. Internal consistency with Cronbach's α = 0.94 was excellent.
Effects on Treatment Expectation
Treatment Receivers
The statistical model including main effects proved to be a better explanation of the data than the model including no variables (χ2(3) = 166.95, p < 0.001). However, the statistical model did not significantly improve entering the interactional effect (χ2(2) = 3.52, p > 0.05). Therefore, we did not include the interactional effect to investigate treatment expectations among treatment receivers.
Treatment approach (F[2,258.80]= 98.49, p < 0.001) and group (F[1,209.47]= 18.89, p < 0.001) significantly predicted treatment expectation. For the main effect of treatment approach, post hoc pairwise analyses indicated that treatment expectations of the multimodal pain management approach were significantly higher compared to the psychological (mean ∆: 5.8; 4.1 to 7.4) and pharmacological (mean ∆: 10.1; 8.2 to 12.0) management approach. Treatment expectations of the psychological pain management approach were significantly higher compared to the pharmacological (mean ∆: 4.3; 2.1 to 6.6) management approach. For the main effect of group, post hoc pairwise analyses indicated that treatment expectations were significantly lower for patients compared to healthy controls (mean ∆: −3.7; −5.3 to −2.0). Treatment expectation ratings among treatment receivers are visualized in Figure 2.
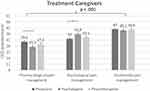
Caregivers
Our statistical model including main effects proved to be a better explanation of our data than the model including no variables (χ2(4) = 241.04, p < 0.001). The statistical model improved further by entering the interactional effect (χ2(4) = 18.63, p < 0.001). We therefore included the interactional effect to investigate treatment expectations among caregivers.
The treatment approach (F[2,281.96]= 179.66, p < 0.001) and interaction between treatment approach x group significantly (F[4,281.96]= 4.80, p < 0.001) predicted treatment expectations. Group did not predict treatment expectations (F[2,236.43]= 0.117, p = 0.89). For the main effect of treatment approach, post hoc pairwise analyses indicated that the multimodal pain management approach’s treatment expectations were significantly higher than the psychological (mean ∆: 5.9; 4.4 to 7.4) and pharmacological (mean ∆: 12.1; 10.5 to 13.7) management approaches were. The psychological pain management approach’s treatment expectations were significantly higher than the pharmacological (mean ∆: 6.2; 4.4 to 8.0) management approaches. For the interactional effect, post hoc pairwise analyses indicated that psychotherapists gave psychological pain management significantly higher treatment-expectations ratings than did the physicians (mean ∆: 4.0; 0.3 to 7.6). Likewise, physicians gave pharmacological pain management significantly higher treatment-expectations rating than did the psychotherapists (mean ∆: 4.3; 0.4 to 8.2). Physicians provided similar treatment-expectation ratings of the pharmacological and psychological pain management approaches (mean ∆: 2.3; −.8 to 5.4), while their treatment-expectation ratings of the multimodal pain management approach were highest. Treatment expectation ratings among caregivers are visualized in Figure 3.
Discussion
Summary of Main Findings
We investigated predictive treatment expectations towards different pain management approaches. For this purpose, both (potential) treatment receivers and caregivers provided ratings of expected treatment success for standardized vignettes describing patients suffering from chronic low back pain. Individuals suffering from chronic low back pain generally had lower treatment expectations than healthy controls regardless of the type of pain management approach described. Psychotherapists and physicians both had higher treatment expectations towards their own treatment approach. However, their treatment expectations did not differ from the multimodal pain management approach. All participants expected the multimodal pain management approach to be most effective. Moreover, participants expected the psychological pain management approach to be more effective than the pharmacological pain management approach – with the exception of the physicians, who expected both treatment approaches to be equally effective.
The Need for Expectation Optimization Among Patients
Effects of previous treatment history might explain why patients had systematically lower treatment expectations than healthy controls.23 So far, an impressive body of research suggests that treatment expectations influence treatment outcome across various chronic pain treatments.9 Therefore, our findings are of special importance, as they suggest that these pain treatments might not be achieving all their potential within the targeted population. There is an urgent need to clarify, under which circumstances treatment expectations can be altered, develop targeted strategies to enhance treatment expectations and evaluate their implementation in routine medical care. For example, expectation-focused psychological interventions (EFPI) have been developed to adapt the individual patient’s expectations.24 These strategies either attempt to convey adaptive expectations (ie, expectation optimization) and to eliminate maladaptive expectations by encouraging patients to test their beliefs in real-life situations (ie, expectation violation). Other approaches aim to induce certain expectations via verbal suggestion (= providing instructions regarding treatment outcome), conditioning (= pairing a neutral stimulus with an unconditioned stimulus that triggers a certain response), and mental imagery (= actively generating an event’s multisensory cognitive representation).25 According to the motivational model of pain self-management, the readiness for behavior change cannot only be achieved via the perceived importance of change (eg, discussing positive outcome expectations from pain self-management while acknowledging their costs), but also by increasing self-efficacy (eg, observing other patients engaging in self-management strategies).26 There is evidence that watching a DVD featuring patients suffering from chronic hemophilia-related joint pain triggers a stronger motivation to pain self-management than does reading information in a booklet.27 However, more research is needed to develop adequate strategies for enhancing treatment expectations and ultimately improving treatment impacts.
The Need for More Multimodal Pain Treatment Approaches
In line with international treatment guidelines,3 both treatment receivers and caregivers expected the multimodal pain treatment approach to be the most effective. Moreover, there was strong consensus that the psychological pain treatment approach would be more effective than standard pharmacological treatment. However, participants may have perceived the description of the psychological treatment more as a combined rather than a stand-alone treatment. The patients described in our vignettes underwent medical surgery before consulting a psychotherapist. Study participants might also have implicitly assumed that patients take additional medication prescribed by their general practitioner. Despite those factors, we consider the positive evaluation of psychological approaches our study reveals to be quite encouraging. To date, only a small minority of chronic-pain patients actually undergo additional psychological interventions.4 Therefore, the strong association between positive treatment expectations and psychological pain treatments provides convincing arguments for its further implementation into current healthcare systems, which are currently not designed to support this multimodal treatment approach.2
The Need for Caregivers to Reflect Upon Their Own Treatment Expectations
Of note is the fact that both physicians and psychotherapists held higher treatment expectations from their own treatment approach. Physiotherapist showed no specific, statistically significant response pattern compared to the other two groups, although their treatment expectations seemed to be similar to expectations among physicians. Although difficult to interpret in our cross-sectional design, this observation could have positive and negative consequences. On the one hand, treatment caregivers might pass on positive expectations to their patients. For example, therapeutic alliance and therapist competence influenced the success of psychotherapeutic treatment among individuals suffering from health anxiety.28 At the same time, excessive self-confidence might also be harmful. One study interviewed chiropractors, osteopaths, and physiotherapists about their reasons to continue treatment despite the lack of improvements.29 Clinicians in that study viewed their role beyond the traditional curative approach. For example, they indicated having discussed psychological issues with their patients. However, they did not refer to specific psychological syndromes associated with maladaptive pain behavior. Similarly, physicians in the present study were the only group who expected pharmacological and psychological treatment approaches to be equally effective. There may be a risk of overestimating individual professional skills. This appears especially relevant in outpatient settings in which physicians and psychotherapists usually work independently, meaning that interdisciplinary collaboration is less likely. In that sense, we fully agree with the idea put forward by Njis and colleagues:10 In addition to assessing and optimizing patients’ treatment expectations prior to treatment delivery, they invite clinicians to reflect on their own attitudes when working with individuals suffering from chronic pain.
However, these assumptions must remain hypothetical in the context of our cross-sectional design. More research is needed to fully understand how expectations among treatment caregivers affect routine medical care. Reliable measurement instruments are needed for this purpose. In contrast to previous research,14,15 our findings do not show that the CEQ questionnaire assesses two independent factors of cognitively based credibility and affectively based expectancy. However, the results from our parallel analysis to indicate factor extraction were somewhat inconclusive. Participants rated the treatment expectations for standardized vignettes describing typical chronic pain patients. Therefore, the affective component might not have differed much from their cognitive evaluation. This raises the question whether the affective component is as relevant to caregivers as it is to patients. One initial future research step must thus be to investigate the psychometric properties of the CEQ questionnaire among caregivers. This is the necessary first step to enable better compliance with treatment guidelines and to ensure further research on this subject.8,11
Strength and Limitations
The present survey incorporates opinions from treatments receivers and caregivers of treatment expectations from various chronic pain management approaches in the context of chronic low back pain. Vignettes were formulated according to international guidelines. Their treatment descriptions were based on treatment guidelines and were developed in cooperation with pain experts. The chronological order of vignettes was randomized to minimize sequential effects. Besides these strengths, some methodological flaws must be considered. First, our study applied a cross-sectional design, which only allows existing group differences to be characterized. Thus, explanations about their impact or source of origin remain purely hypothetical. Second, the allocation of treatment receivers in individuals with chronic low back pain and healthy controls relied solely on self-reports from study participants. Therefore, we cannot guarantee that patients met the objective criteria necessary to diagnose a chronic pain condition. Third, participants provided ratings for standardized patients. This procedure enabled general opinions towards various pain management approaches to be assessed. However, our participants’ evaluations might have differed had they referred to their own situation. Future studies could include additional questions asking participants about the treatment approach they would choose for themselves or recommend to their patients. It should also be noted that a specific patient group is portrayed in our vignettes. Although the overuse of surgical and invasive treatments in the context of chronic low back pain has been criticized for several years,30 most patients suffer from chronic pain for unspecific reasons and are not treated with surgical procedures. Fourth, we included physicians, psychotherapists, and physiotherapists specializing in various disciplines so as to ensure a representative sample of caregivers. However, we can make no statements concerning possible differences in attitudes among general practitioners and orthopedic surgeons, for example.
Conclusions
The multimodal pain management approach with psychological elements was associated with the highest treatment expectations among treatment receivers and caregivers. Our results therefore support their further implementation within the healthcare system. Individuals suffering from chronic low back pain had systematically lower treatment expectations than healthy controls. This finding highlights the need for systematic strategies to enhance treatment expectations among chronic pain patients. In addition, we invite clinicians to think about whether their own treatment expectations towards different pain management approaches match the recommendations of international treatment guidelines.
Acknowledgments
The authors wish to thank Maximilian Schwarz and Gabriele Külz for their support during the acquisition phase. This study was supported by a doctoral thesis scholarship from Philipps-University Marburg and was associated with the GRK 2271 “Breaking Expectations”. The publication was funded by the Open Access Fund of the University of Koblenz-Landau.
Disclosure
The authors have no competing interests to declare.
References
1. GBD. 2017 Disease and injury incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990 – 2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789–1858. doi:10.1016/S0140-6736(18)32279-7
2. Traeger AC, Buchbinder R, Elshaug AG, et al. Care for low back pain: can health systems deliver? Bull World Health Organ. 2019;97(6):423–433. doi:10.2471/BLT.18.226050
3. Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non‑specific low back pain in primary care: an updated overview. Eur Spine J. 2018;27(11):2791–2803. doi:10.1007/s00586-018-5673-2
4. Müller-Schwefe GHH. European survey of chronic pain patients: results for Germany. Curr Med Res Opin. 2011;27(11):2099–2106. doi:10.1185/03007995.2011.621935
5. Geurts JW, Willems PC, Lockwood C, et al. Patient expectations for management of chronic non-cancer pain: a systematic review. Heal Expect. 2017;20(6):1201–1217. doi:10.1111/hex.12527
6. Laferton JAC, Kube T, Salzmann S, et al. Patients’ expectations regarding medical treatment: a critical review of concepts and their assessment. Front Psychol. 2017;8:233. doi:10.3389/fpsyg.2017.00233
7. Thompson AGH, Suñol R. Expectations as determinants of patient satisfaction: concepts, theory and evidence. J Qual Heal Care. 1995;7(2):127–141. doi:10.1093/intqhc/7.2.127
8. Bialosky JE, Bishop MD, Cleland JA. Individual expectation: an overlooked, but pertinent, factor in the treatment of individuals experiencing musculoskeletal pain. Phys Ther. 2010;90(9):1345–1355. doi:10.2522/ptj.20090306
9. Cormier S, Lavigne GL, Choinière M, et al. Expectations predict chronic pain treatment outcomes. Pain. 2016;157(2):329–338. doi:10.1097/j.pain.0000000000000379
10. Nijs J, Roussel N, van Wilgen PC, et al. Thinking beyond muscles and joints: therapists’ and patients’ attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment. Man Ther. 2013;18:96–102. doi:10.1016/j.math.2012.11.001
11. Darlow B, Fullen BM, Dean S, et al. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain. 2012;16(2):3–17. doi:10.1016/j.ejpain.2011.06.006
12. Evans SC, Roberts MC, Keeley JW, et al. Vignette methodologies for studying clinicians’ decision-making: validity, utility, and application in ICD-11 field studies. Int J Clin Heal Psychol. 2015;15(2):160–170. doi:10.1016/j.ijchp.2014.12.001
13. Bundesärztekammer (BÄK), Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). Nationale Versorgungsleitlinie nicht-spezifischer Kreuzschmerz – kurzfassung; 2017. Available from: https://www.leitlinien.de/mdb/downloads/nvl/kreuzschmerz/kreuzschmerz-2aufl-vers1-kurz.pdf.
14. Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31(2):73–86. doi:10.1016/s0005-7916(00)00012-4
15. Smeets RJEM, Beelen S, Goossens MEJB, et al. Treatment expectancy and credibility are associated with the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. Clin J Pain. 2008;24(4):305–315. doi:10.1097/AJP.0b013e318164aa75
16. Ostelo RWJG, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain. Spine. 2008;33(1):90–94. doi:10.1097/BRS.0b013e31815e3a10
17. Dillmann U, Nilges P, Saile H, et al. Behinderungseinschätzung bei chronischen Schmerzpatienten. Der Schmerz. 1994;8(2):100–110. doi:10.23668/psycharchives.324
18. McCracken LM, Dhingra L. A short version of the Pain Anxiety Symptom Scale (PASS-20): preliminary development and validity. Pain Res Manag. 2002;7(1):45–50. doi:10.1155/2002/517163
19. Walter B, Hampe D, Wild J, et al. Die Erfassung der Angst vor Schmerzen: eine modifizierte deutsche Version der Pain Anxiety Symptom Scale (PASS-D). Der Schmerz. 2002;16:83.
20. Beck AT, Steer RA, Brown GK. BDI-Fast Screen for Medical Patients: Manual. San Antonia: TX: Psychological Corporation; 2000.
21. Kliem S, Brähler E. Beck Despressions-Inventar - FS: Deutsche Überarbeitung. Pearson: Frankfurt; 2013.
22. Leclerc A, Gourmelen J, Chastang JF, et al. Level of education and back pain in France: the role of demographic, lifestyle and physical work factors. Int Arch Occup Environ Health. 2009;82(5):643–652. doi:10.1007/s00420-008-0375-4
23. Kessner S, Forkmann K, Ritter C, et al. The effect of treatment history on therapeutic outcome: psychological and neurobiological underpinnings. PLoS One. 2014;9(9):e109014. doi:10.1371/journal.pone.0109014
24. Kube T, Glombiewski JA, Rief W. Using different expectation mechanisms to optimize treatment of patients with medical conditions: a systematic review. Psychosom Med. 2018;80(6):535–543. doi:10.1097/PSY.0000000000000596
25. Peerdeman KJ, van Laarhoven AIM, Keij SM, et al. Relieving patients’ pain with expectation interventions. Pain. 2016;157(6):1179–1191. doi:10.1097/j.pain.0000000000000540
26. Jensen MP, Nielson WR, Kerns RD. Toward the development of a motivational model of pain self-management. J Pain. 2003;4(9):477–492. doi:10.1016/S1526-5900(03)00779-X
27. Elander J, Robinson G, Morris J. Randomized trial of a DVD intervention to improve readiness to self-manage joint pain. Pain. 2011;152(10):2333–2341. doi:10.1016/j.pain.2011.06.026
28. Weck F, Richtberg S, Jakob M, et al. Therapist competence and therapeutic alliance are important in the treatment of health anxiety (hypochondriasis). Psychiatry Res. 2015;228(1):53–58. doi:10.1016/j.psychres.2015.03.042
29. Pincus T, Vogel S, Breen A, et al. Persistent back pain – why do physical therapy clinicians continue treatment? A mixed methods study of chiropractors, osteopaths and physiotherapists. Eur J Pain. 2006;10(1):67–76. doi:10.1016/j.ejpain.2005.01.008
30. Morlion B. Chronic low back pain: pharmacological, interventional and surgical strategies. Nat Rev Neurol. 2013;9(8):462–473. doi:10.1038/nrneurol.2013.130
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.