Back to Journals » OncoTargets and Therapy » Volume 8
Treating patients with advanced rectal cancer and lateral pelvic lymph nodes with preoperative chemoradiotherapy based on pretreatment imaging
Authors Otowa Y, Yamashita K , Kanemitsu K, Sumi Y, Yamamoto M, Kanaji S, Imanishi T, Nakamura T, Suzuki S, Tanaka K, Kakeji Y
Received 3 June 2015
Accepted for publication 11 August 2015
Published 29 October 2015 Volume 2015:8 Pages 3169—3173
DOI https://doi.org/10.2147/OTT.S89752
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Faris Farassati
Yasunori Otowa, Kimihiro Yamashita, Kiyonori Kanemitsu, Yasuo Sumi, Masashi Yamamoto, Shingo Kanaji, Tatsuya Imanishi, Tetsu Nakamura, Satoshi Suzuki, Kenichi Tanaka, Yoshihiro Kakeji
Division of Gastrointestinal Surgery, Department of Surgery, Kobe University Graduate School of Medicine, Kobe, Japan
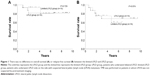
Abstract: Preoperative chemoradiotherapy (CRT) and lateral pelvic lymph node (LPLN) dissection (LPLD) based on pretreatment imaging are performed to improve oncological outcomes at our institution. However, the advantage of LPLD following preoperative CRT in advanced rectal cancer remains unclear. The objective of the present study was to assess the validity of this approach. Thirty-two patients with advanced rectal cancer were included in the study. All patients were treated with preoperative CRT and curative operation. Of these, 16 patients who were treated between August 2005 and June 2008 underwent LPLD on both sides (LPLD group). Sixteen patients who were treated between July 2008 and January 2013 underwent LPLD only on the side with suspected LPLN metastasis determined by pretreatment imaging; in cases without LPLN metastasis, only total mesorectal excision was performed (limited-LPLD group). The overall survival and relapse-free survival between the LPLD and the limited-LPLD groups were compared. Preoperative CRT was able to lower clinical lymph node status in 50% of the cases. In addition, pathological lymph node status did not exceed the pretreatment clinical lymph node status stage in the LPLD group. There were no differences in the overall survival and relapse-free survival between the two groups (P=0.729 and P=0.874, respectively). We conclude that multi-imaging studies have a very low risk of overlooking pathologically positive LPLN metastases. Therefore, limited LPLD is a feasible strategy for patients with advanced rectal cancer and suspicious LPLN metastases based on pretreatment imaging.
Keywords: neoadjuvant treatment, rectal cancer, chemoradiotherapy, lateral pelvic lymph node, MRI, CT
Introduction
Total mesorectal excision (TME) with preoperative chemoradiotherapy (CRT) is a widely accepted standard treatment for patients with advanced rectal cancer. However, the dissection of lateral pelvic lymph nodes (LPLNs) remains controversial. In Japan, the Japanese Society for Cancer of the Colon and Rectum (JSCCR) 2010 guidelines for the treatment of colorectal cancer recommends dissecting the LPLN, because of an increased risk for LPLN metastasis when advanced-stage lower rectal cancer extends below the peritoneal reflection.1 In Western countries, LPLN dissection (LPLD) is generally not performed because LPLD shows no benefit over adjuvant CRT,2 and there are no differences in local recurrence rates between preoperative radiation and LPLD.3,4
To improve the oncologic outcomes in patients with advanced rectal cancer, we have been performing preoperative CRT and bilateral LPLD at our institution, with good local control. The local recurrence rates have been acceptable, and there were no LPLN metastases that were initially diagnosed as negative during pretreatment imaging; however, patients had LPLD-related complications. Thus, we hypothesized that limiting LPLD would minimize the side effects of LPLD with minimal negative surgical outcomes. The objective of the current study was to assess the clinical validity of limiting LPLD in patients with advanced rectal cancer.
Patients and methods
Study population
In total, 32 patients with biopsy-proven, locally advanced (clinical primary tumor status of cT3–4 or positive clinical lymph node status) rectal cancer with the lower tumor border located above and bellow the peritoneal reflection were treated at Kobe University Hospital between August 2005 and June 2013. All study participants provided written informed consent, and the study design was approved by the ethics review board at Kobe University Hospital and conforms to the provisions of the Declaration of Helsinki.
Staging
The TNM stage was determined according to the seventh edition of the AJCC Cancer Staging Manual.5 According to the JSCCR classification, the lateral pelvic area is classified into four regions: internal iliac, obturator, external iliac, and common iliac.6 Although all LPLNs are not defined clearly as regional lymph nodes in the AJCC manual, we classified all LPLNs as such, based on a previous study by Akiyoshi et al.7
Clinical stage assessment was based on computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) studies. We defined lymph node metastasis as positive in the presence of one or more of the following: a lymph node larger than 8 mm by CT; a positive diffusion-weighted image by MRI; or a high-intensity spot by PET. However, the definitive determination for LPLD was made at the surgical team meetings. The imaging studies were conducted before CRT and 4–6 weeks following CRT to evaluate the clinical stage.
Treatment strategy
Patients received chemotherapy that consisted of tegafur–uracil (UFT) 200 mg/m2/day and leucovorin (LV) 75 mg/body/day for 28 days and radiotherapy at a total dose of 45 Gy. The lateral pelvic area was included in the radiation target volume. Surgery was performed 6–8 weeks after the completion of the preoperative CRT. LPLD was performed according to the JSCCR 2010 guidelines.1 All patients treated between August 2005 and June 2008 underwent bilateral LPLD (LPLD group, 16 patients). After July 2008, LPLD was performed on the side that was suspected positive for LPLN metastasis by pretreatment imaging, irrespective of the posttreatment imaging results; TME alone was performed on patients for whom preoperative imaging showed an absence of LPLN metastasis (limited-LPLD group, 16 patients).
Statistical analysis
Descriptive statistics were performed using the JMP statistical software package (JMP® 10; SAS Institute Inc., Cary, NC, USA). The LPLD and limited-LPLD groups were compared using the χ2 test or the Fisher’s exact test. Overall survival (OS) was calculated from the date of confirmed diagnosis at our hospital to the occurrence of the event or to the last known date of follow-up. Survival analysis was performed using the Kaplan–Meier method with the log-rank test. In all analyses, a P-value <0.05 was accepted as statistically significant.
Results
In the limited-LPLD group, nine patients were diagnosed as LPLN-positive based on pretreatment imaging. However, ten patients received limited LPLD: one patient received LPLD based on intraoperative findings, despite negative preoperative imaging results. There were no differences between the LPLD and limited-LPLD groups in patient characteristics, except for age (Table 1). Only one patient in the LPLD group had pathological LPLN metastasis, whereas three patients in the limited-LPLD group had LPLN metastases. The median follow-up periods for the LPLD and limited-LPLD groups were 7.8 (range: 0.9–9.5) years and 3.6 (range: 1.1–6.6) years, respectively.
The changes in lymph node status in relation to preoperative CRT are listed in Table 2. In all cases, pathological lymph node status did not exceed the pretreatment clinical lymph node status, suggesting that all LPLN metastases were successfully diagnosed preoperatively. None of the cases were false positive for LPLN metastases. In 50% of the cases, the lymph node status improved after preoperative CRT. In the LPLD group, the percentage of pathological LPLN status metastasis was 6.3% (one in 16 patients), and no false-negatives were observed. The numbers of local and distant recurrences observed in each group are listed in Table 3. No LPLN recurrence was observed in either the LPLD or the limited-LPLD group. Local and distant recurrence rates did not differ between the two groups.
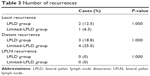  | Table 3 Number of recurrences |
The median operation time and the amount of lost blood were 405 minutes (range: 280–603) and 754.5 mL (range: 343–2,386), respectively, in the LPLD group, and 596 minutes (range: 382–858) and 715 mL (range: 100–5,345), respectively, in the limited-LPLD group. Surgical site infection was observed in 12 patients (75.0%) in the LPLD group and seven patients (43.8%) in the limited-LPLD group. Urinal dysfunction was observed in five patients (33.3%) in the LPLD group. In the limited-LPLD group, ten patients received LPLD and four patients (40.0%) had urinal dysfunction; two of these patients underwent bilateral LPLD.
Figure 1A represents the OS in the LPLD and limited-LPLD groups. The relapse-free survival (RFS) for the two groups is shown in Figure 1B. No significant differences were observed in the OS and the RFS between the two groups (P=0.729 and P=0.874, respectively).
Discussion
Based on the results of the German Rectal Cancer Study Group trial, preoperative CRT has become a standard treatment for rectal cancer in Western countries.8 There are several studies which assessed 5-fluorouracil (FU)/LV as pretreatment chemotherapy; however, there are no randomized trials to date.9,10 Ishihara et al reported the efficacy of UFT/LV with radiotherapy as a preoperative treatment for rectal cancer with no increases in postoperative complications.11 Histologically proven downstaging was observed in 42%–60% of patients, and 3-year OS was 86%–90% in patients treated with UFT/LV with radiotherapy.12,13
Several previous reports argue that pretreatment imaging may not be able to detect all pathologically positive LPLNs14,15 and that the number of false-negative LPLNs might be higher than that predicted.16 Our results show the accuracy of pretreatment diagnosis, with the absence of false-negative LPLNs in the LPLD group. This finding could be because of the combination of CT, MRI, and PET for assessment, resulting in an accurate diagnosis, and CRT for the improved management of LPLN metastases.
In Western countries, preoperative CRT is a standard treatment that has led to low local recurrence rates.8 However, CRT cannot manage all clinically positive LPLN metastases, as was the case in one of our patients with a pathologically positive LPLN, in agreement with a previous report.17 We believe that CRT alone cannot fully manage LPLN metastases; thus, LPLD provides an opportunity to control local recurrence following CRT.
LPLD is associated with a number of complications, including prolonged operation time, increased blood loss, and increased frequency of urinary and male sexual dysfunction, compared with those observed in patients who did not undergo LPLD.3 Thus, patients with suspicious LPLN should receive limited LPLD. We performed both CRT and LPLD based on the assessment by pretreatment imaging. The amount of blood loss was comparable between the two groups; however, the operation time was significantly longer for the limited-LPLD group than that for the LPLD group. As we have already mentioned, neither the LPLD group nor the limited-LPLD group experienced an LPLN recurrence. The limited-LPLD group had an OS and RFS that was equivalent to the LPLD group. Further, there were no false-negative LPLN cases in the LPLD group. These results suggest that determining suspicious LPLN metastases by pretreatment imaging is feasible and that limiting LPLD is associated with favorable surgical outcomes.
This study has certain potential limitations. First, the number of patients was relatively small, and the follow-up period for some patients was not long enough to most adequately evaluate the rate of recurrence. Second, we performed LPLD in all cases in which lymph node metastasis was suspected by imaging. This approach may have led to an increase in the enrollment of candidates for LPLD, because several studies have shown that a post-CRT LPLN >5 mm in diameter is significantly associated with metastasis.18,19 In the present study, each of the four patients who had pathologically positive LPLN metastases before treatment still had LPLNs of ≥8 mm after CRT. Thus, the imaging criteria of LPLN metastasis in patients treated with preoperative CRT are reliable and necessary to determine those who need to undergo LPLD.
Conclusion
Treatment with preoperative CRT and LPLD is advantageous in managing local recurrence. Advances in multi-imaging studies help to avoid overlooking pathologically positive LPLN metastases. Therefore, limiting LPLD is a feasible strategy for patients with advanced rectal cancer and suspicious LPLN metastasis following CRT.
Disclosure
The authors report no conflicts of interest in this work.
References
Watanabe T, Itabashi M, Shimada Y, et al; Japanese Society for Cancer of the Colon and Rectum. Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for the treatment of colorectal cancer. Int J Clin Oncol. 2015;20(2):207–239. | ||
Kim JC, Takahashi K, Yu CS, et al. Comparative outcome between chemoradiotherapy and lateral pelvic lymph node dissection following total mesorectal excision in rectal cancer. Ann Surg. 2007;246(5):754–762. | ||
Georgiou P, Tan E, Gouvas N, et al. Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol. 2009;10(11):1053–1062. | ||
Kusters M, Beets GL, van de Velde CJ, et al. A comparison between the treatment of low rectal cancer in Japan and the Netherlands, focusing on the patterns of local recurrence. Ann Surg. 2009;249(2):229–235. | ||
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A III, editors. AJCC Cancer Staging Manual. 7th ed. New York: Springer; 2010. | ||
Japanese Society for Cancer of the Colon and Rectum. Japanese Classification of Colorectal Carcinoma. 2nd English ed. Tokyo: Kanehara & Co; 2009. | ||
Akiyoshi T, Watanabe T, Miyata S, Kotake K, Muto T, Sugihara K; Japanese Society for Cancer of the Colon and Rectum. Results of a Japanese nationwide multi-institutional study on lateral pelvic lymph node metastasis in low rectal cancer: is it regional or distant disease? Ann Surg. 2012;255(6):1129–1134. | ||
Sauer R, Becker H, Hohenberger W, et al; German Rectal Cancer Study Group. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351(17):1731–1740. | ||
Roh MS, Colangelo LH, O’Connell MJ, et al. Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol. 2009;27(31):5124–5130. | ||
Lam CW, Chen WT, Liu MT, et al. Effect of preoperative concurrent chemoradiotherapy in locally advanced low rectal cancer after radical resection surgery. Int Surg. 2005;90(1):53–59. | ||
Ishihara S, Hayama T, Yamada H, Nozawa K, Matsuda K, Watanabe T. Benefit of tegafur-uracil and leucovorin in chemoradiotherapy for rectal cancer. Hepatogastroenterology. 2011;58(107–108):756–762. | ||
Cellier P, Leduc B, Martin L, et al. Phase II study of preoperative radiation plus concurrent daily tegafur-uracil (UFT) with leucovorin for locally advanced rectal cancer. BMC Cancer. 2011;11:98. | ||
Uzcudun AE, Batlle JF, Velasco JC, et al. Efficacy of preoperative radiation therapy for resectable rectal adenocarcinoma when combined with oral tegafur-uracil modulated with leucovorin: results from a phase II study. Dis Colon Rectum. 2002;45(10):1349–1358. | ||
Fujita S, Akasu T, Mizusawa J, Saito N, et al; Colorectal Cancer Study Group of Japan Clinical Oncology Group. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012;13(6):616–621. | ||
Yano H, Saito Y, Takeshita E, Miyake O, Ishizuka N. Prediction of lateral pelvic node involvement in low rectal cancer by conventional computed tomography. Br J Surg. 2007;94(8):1014–1019. | ||
Ogawa S, Itabashi M, Hirosawa T, Hashimoto T, Bamba Y, Kameoka S. Lateral pelvic lymph node dissection can be omitted in lower rectal cancer in which the longest lateral pelvic and perirectal lymph node is less than 5 mm on MRI. J Surg Oncol. 2014;109(3):227–233. | ||
Akiyoshi T, Ueno M, Matsueda K, et al. Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol. 2014;21(1):189–196. | ||
Oh HK, Kang SB, Lee SM, et al. Neoadjuvant chemoradiotherapy affects the indications for lateral pelvic node dissection in mid/low rectal cancer with clinically suspected lateral node involvement: a multicenter retrospective cohort study. Ann Surg Oncol. 2014;21(7):2280–2287. | ||
Akiyoshi T, Matsueda K, Hiratsuka M, et al. Indications for lateral pelvic lymph node dissection based on magnetic resonance imaging before and after preoperative chemoradiotherapy in patients with advanced low-rectal cancer. Ann Surg Oncol. Epub 2015. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.