Back to Journals » Clinical Interventions in Aging » Volume 18
Translation, Cultural Adaptation, and Validation of the Cantonese Version of SarQoL in Hong Kong’s Older Population: An Interviewer-Administered Questionnaire for Assessing Sarcopenia-Specific Quality of Life in Fieldwork Practice
Authors Yu R , Lai D, Leung G , Tam LY, Cheng C, Kong S, Tong C, Lu Z, Leung JC, Chan A, Kwok T , Woo J
Received 11 August 2023
Accepted for publication 10 October 2023
Published 9 November 2023 Volume 2023:18 Pages 1851—1861
DOI https://doi.org/10.2147/CIA.S431218
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Ruby Yu,1,2 Derek Lai,2 Grace Leung,2 Lok-Yan Tam,2 Clara Cheng,2 Sara Kong,2 Cecilia Tong,2 Zhihui Lu,1 Jason CS Leung,3 Amany Chan,3 Timothy Kwok,1,3 Jean Woo1,2
1Department of Medicine and Therapeutics, Faculty of Medicine, The Chinese University of Hong Kong, Shatin, New Territories, Hong Kong; 2The Jockey Club Institute of Ageing, The Chinese University of Hong Kong, Shatin, New Territories, Hong Kong; 3The Jockey Club Centre for Osteoporosis Care and Control, The Chinese University of Hong Kong, Shatin, New Territories, Hong Kong
Correspondence: Ruby Yu, Department of Medicine & Therapeutics, Faculty of Medicine, The Chinese University of Hong Kong, Room 124021, 10/F, Lui Che Woo Clinical Sciences Building, Prince of Wales Hospital, Shatin, New Territories, Hong Kong, Email [email protected]
Objective: This study examined the psychometric properties of the Cantonese version of the SarQoL® questionnaire.
Participants: A total of 118 (including 60 non-sarcopenic and 58 sarcopenic) community-dwelling older adults aged 65 years or above with Cantonese as their mother tongue.
Methods: Translation and cultural adaptation of the SarQoL were conducted using a standardized protocol. To validate the Cantonese SarQoL, psychometric properties including discriminative power, reliability (including internal consistency and test–retest reliability), and construct validity (including convergent and divergent validity), as well as floor and ceiling effects, were assessed.
Results: The translation of the questionnaire was completed without significant difficulties. Results indicated that the Cantonese SarQoL had (1) good discriminative power (sarcopenic participants had lower overall scores, mean = 66.1 vs 75.0, p < 0.001; the overall score was negatively predictive of the presence of sarcopenia, adjusted OR = 0.949, 95% CI = [0.912, 0.983]), (2) good internal consistency (Cronbach’s alpha = 0.835; correlations between domain and overall scores ranged from 0.576 to 0.868), (3) excellent test-retest agreement (intraclass correlation coefficient = 0.801), (4) good construct validity (convergent: moderate to strong correlations were found between the overall score and almost all of the SF-36 and EQ-5D domains; divergent: weaker correlations were found between the overall score and SF-36 social functioning, ρ = − 0.098, and EQ-5D self-care, ρ = − 0.331), and (5) no floor or ceiling effect.
Conclusion: The Cantonese SarQoL is valid and reliable, and thus can be used as an interviewer-administered questionnaire for assessing sarcopenia-specific quality of life in fieldwork practice.
Keywords: interviewer-administered questionnaire, psychometric, quality of life, sarcopenia, SarQoL, translation, validation
Introduction
Sarcopenia is defined as a progressive and generalized loss of muscle mass and muscle function due to advancing age.1–3 Traditional clinical outcomes that can be attributed to sarcopenia include falls, fractures, hospitalizations, and all-cause mortality.4–7 These outcomes can demonstrate the impact of sarcopenia from a public health perspective, but cannot reflect the health status or quality of life as perceived by the sarcopenic individuals, which are holistic and comprehensive indicators that are particularly important within the context of evaluating interventions and health services for treating sarcopenia.
Over recent years, several generic instruments such as the Short Form 36-item (SF-36)8 and EuroQol 5-dimension (EQ-5D)9 questionnaires have been used to measure the quality of life of those with sarcopenia, along with traditional clinical outcomes such as the number of falls and fractures over the past year. While SF-36 and EQ-5D allow comparison across various diseases or conditions to assist in the evaluation of interventions and health services, it has been argued that these instruments may not be specific and sensitive enough to capture the quality of life of sarcopenic individuals. For example, several published reports using the SF-36 questionnaire indicated that there were no reductions in quality of life in individuals with sarcopenia, or only in some specific domains such as physical function and vitality.10–13
In light of these issues, a sarcopenia-specific instrument, namely the Sarcopenia Quality of Life (SarQoL®) questionnaire, was developed in 2015 to measure and monitor the quality of life from the perspective of those with sarcopenia,14 which has been used to evaluate the effects of interventions in this regard.15,16 The SarQoL questionnaire was translated into different languages and was implemented in a variety of populations,17 which has proven to be a valid and reliable instrument after undergoing several rounds of psychometric evaluations.18
In Hong Kong, sarcopenia is highly prevalent, and its prevalence rate was found to be about 10% to 40% among older people aged 65 years or above, depending on the definition used.19,20 In this regard, different types of interventions have been developed and adopted in the community and residential care settings for treating sarcopenia in older people.21 This indicates the relevance and importance of a sarcopenia-specific instrument for measuring quality of life, and a natural candidate would be the SarQoL questionnaire as introduced above. However, although there are already several validated Chinese versions of the SarQoL questionnaire, they are more geared towards the populations in mainland China and Taiwan.22,23 In other words, none of them is specifically designed for the Hong Kong Cantonese dialect, which, perhaps unbeknownst to some non-Chinese speakers, is in fact a rather different language as compared with Mandarin. In brief, all the existing Chinese SarQoL are in the form of standard written Chinese, which is not the language that Hong Kong people speak in daily life conversations. This constitutes a major issue because older respondents can seldom comprehend and complete questionnaires entirely on their own. Instead, questionnaires are usually administered by facilitators (eg, research staff), who need to mentally and spontaneously translate the written Chinese into spoken Cantonese, before they can articulate the questionnaire items to the older respondents. This is clearly suboptimal, since in this case the item wordings are no longer standardized and the messages conveyed to the respondents may not be identical. Consequently, no sarcopenia-specific instrument for measuring quality of life is yet available in Hong Kong, rendering this topic much less studied in the local population.
To provide insight into the impact of sarcopenia on quality of life and how the positive effects of interventions may be converted into improvements in quality of life, the present study was aimed to translate the SarQoL questionnaire into Chinese Cantonese and to investigate its psychometric properties in order to establish its validity and reliability as an instrument to measure the quality of life in Cantonese-speaking sarcopenic individuals.
Methods
The SarQoL Questionnaire
The SarQoL questionnaire has 22 questions, which are made up of 53 items since some of the questions are in the form of a matrix table. Most of these items can be thought of as 3-, 4-, or 5-point Likert items, whereas the remaining are multiple-choice questions that permit more than one answers. The SarQoL involves an overall score, which is the sum of seven individual domain scores, namely D1 physical and mental health, D2 locomotion, D3 body composition, D4 functionality, D5 activities of daily living, D6 leisure activities, and D7 fears, with higher scores indicating better quality of life. Scoring of the SarQoL is rather complicated and non-intuitive, thus it is usually performed using a MS Access macro that can be obtained from www.sarqol.org. During the scoring process, the overall and domain scores are rescaled such that their maximum possible values become 100.
Cantonese Translation and Cultural Adaptation
The process of the translation and cultural adaptation of the questionnaire is illustrated in Figure 1. The English SarQoL was first translated into Cantonese by two bilingual experts (translators a and b) having Cantonese as their mother tongue. After that, the two translators compared their translations, sought a consensus, and obtained a preliminary version of the translated SarQoL. Following this, the preliminary version was back-translated from Cantonese into English by another two bilingual translators (translators c and d) having English as their mother tongue, who were blinded to the original version of the questionnaire. To obtain a pre-final version of the Cantonese SarQoL, the two backward translations were examined by an expert committee comprising two methodologists, one health professional, one linguistic professional, and the four translators involved in the previous translation processes. Subsequently, the pre-final version was administered face-to-face to 10 older adults to elicit their thoughts regarding the comprehension and cultural relevance of the questionnaire. These 10 participants had been diagnosed with sarcopenia and did not have significant cognitive problems hindering their comprehension abilities. The final version of the questionnaire was then obtained by modifying the pre-final version based on the comments obtained from the pilot study.
 |
Figure 1 Translation and cultural adaptation of the Cantonese SarQoL. |
The translation was performed without any major difficulties, and the final version can be found on www.sarqol.org. Based on the pilot results, a slight modification was made to a sub-item in question #17, namely “Do you currently have difficulty in undertaking any of the following daily activities: getting in or out of a car”, by adding the phrase “(taxi and private car)” at the end of the item to further elaborate and clarify what is meant by a “car”. This modification, which did not distort the original meaning conveyed by the item, was necessary because the literal translation of “car” in Cantonese can refer to many different types of vehicles.
Examination of Psychometric Properties
Participants
The Cantonese SarQoL was validated in a sample of community-dwelling older adults, who were recruited from a community-based cohort promoting bone health and fall prevention in Hong Kong. The present study included older adults aged 65 years or above with Cantonese as their mother tongue, whereas those with limb loss or were not mentally competent to give informed consent were excluded. A total of 118 eligible participants were invited to attend a health assessment at The Jockey Club Centre for Osteoporosis Care and Control, The Chinese University of Hong Kong, during which a team of trained research assistants administered the Cantonese SarQoL to them. A sub-sample of 58 sarcopenic participants were invited to re-attend the questionnaire interview after two weeks (Figure 2). All participants gave written consent, and the study complied with the Declaration of Helsinki and was approved by the Clinical Research Ethics Committee of The Chinese University of Hong Kong.
 |
Figure 2 Validation of the Cantonese SarQoL. |
Diagnosis of Sarcopenia
The diagnosis of sarcopenia was established according to the criteria of the consensus established by the Asian Working Group for Sarcopenia AWGS) in 2019,24 under which the presence of low muscle mass in combination with low muscle strength and/or low physical performance are required to diagnose that an individual has sarcopenia. For this purpose, muscle mass was measured using a multi-frequency Bioelectrical Impedance Analysis (BIA) device (InBody 770, Cerritos, CA, USA), which was re-calibrated each time before using. Muscle mass was considered low if the appendicular lean muscle per height square (kg/m2) was below the cut-off value (male: < 7.0; female: < 5.4). Muscle strength was evaluated by measuring the handgrip strength using a hydraulic hand dynamometer (Jamar Plus+, Chicago, IL, USA). A value less than 28 kg for male and 18 kg for female indicated low muscle strength. Physical performance was evaluated by measuring the gait speed on a 4-meter track, with a threshold value of 1.0 m/s.
Statistical Analysis
Validation of the Cantonese SarQoL was performed by examining its psychometric properties in the following aspects: 1) discriminative power, 2) internal consistency, 3) test-retest reliability, 4) construct validity, and 5) floor and ceiling effects. Except for 1), only the sub-sample of 58 sarcopenic participants were included. All analyses were performed in R, in particular, using the “psych” package when appropriate.
- Discriminative power (ie, the ability of the questionnaire to discriminate sarcopenic status) was examined by comparing the overall and domain scores between non-sarcopenic and sarcopenic participants using two-sample t-test. In addition, since the SarQoL may also be considered a screening tool for sarcopenia, logistic regression was performed by regressing sarcopenic status on the overall score, as well as other covariates for adjustment purpose.
- Internal consistency is traditionally examined by the Cronbach alpha,25 in which a value greater than 0.65 is deemed acceptable.26,27 The Cronbach alpha is usually considered a measure of item homogeneity, under the assumption that the overall score of the questionnaire is a simple average (or sum) of the individual items. For the present study, however, since the scoring of individual items is non-trivial, the Cronbach alpha was computed with respect to the seven domain scores instead. In addition, it should be noted that since the overall and domain scores are both rescaled such that their maximum possible values are 100 (but with different rescaling factors), the overall score is not simply the average of the domain scores. Thus, the Cronbach alpha was computed and reported for reference only, and should be interpreted with caution. On the other hand, Pearson’s correlations between the overall and domain scores were also estimated. Again, it should be noted that these correlations may be affected by the fact that the overall score is formed by the domain scores with unequal weighting.
- Test-retest reliability was examined by estimating the intra-class correlation coefficient (ICC) between the baseline and retest scores, including both the overall and domain-specific ones. An ICC greater than 0.7 is considered acceptable.28
- Construct validity, including convergent and divergent validity, was assessed by estimating the Pearson’s correlations between the SarQoL scores and two generic health-related quality of life instruments, namely SF-36 and EQ-5D. The SF-36 uses 36 questions to measure the functional health and well-being from the patient’s perspective. These questions can be categorized into eight domains, including physical functioning, role limitation due to physical problems, bodily pain, general health, vitality, social functioning, role limitation due to emotional problems, and mental health. On the other hand, the EQ-5D is a standard measure of health status, which records the perceived severity level of problems in five different dimensions, including mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Furthermore, the EQ-5D has a valuation index (ie, utility) that is formed by the above five dimensions based on utility theory.29
- Floor and ceiling effects were examined on the overall score. Due to the aforementioned non-trivial scoring system, the theoretical minimum possible value may vary across individuals (ie, not simply equal to a constant number, say, 0). Thus, for the purpose of the present study, floor and ceiling effects were defined with respect to the sample minimum and maximum values, respectively. In other words, the percentages of participants who attained an overall score equal to the sample minimum or maximum were examined.
Results
Baseline characteristics of the participants, including the variables of primary interest, demographics and covariates, and sarcopenia assessment results, are shown in Table 1. As expected, sarcopenic participants were significantly older (73.8 vs 71.2 years, p = 0.003) and had lower BMI (21.3 vs 24.3 kg/m2, p < 0.001). Results regarding the psychometric properties of the Cantonese SarQoL are presented below.
 |
Table 1 Baseline characteristic of participants |
Discriminative Power
Sarcopenic participants reported lower overall scores compared to the non-sarcopenic ones (66.1 vs 75.0, p < 0.001). All domain scores, except for D3 body composition and D6 leisure activities, were also significantly lower in the sarcopenic participants (Table 1). Similarly, logistic regression analysis (Table 2) demonstrated that the overall score was negatively associated with the presence of sarcopenia (OR = 0.949, 95% CI = [0.912, 0.983]), after adjusting for other covariates. As a side note, among the included covariates, age, sex, and BMI were also found to be significant predictors of sarcopenic status.
 |
Table 2 Logistic regression on sarcopenic status (n = 118) |
Internal Consistency
The Cronbach’s alpha computed based on the seven domain scores was 0.835. When one of the domain scores was dropped at a time, the values became 0.789, 0.788, 0.797, 0.783, 0.789, 0.895, and 0.818, respectively. On the other hand, all domains showed a significantly positive correlation with the overall score, ranging from ρ = 0.576 to 0.868 (Table 3).
 |
Table 3 Internal consistency and test-retest reliability of the Cantonese SarQoL (n = 58) |
Test-Retest Reliability
An excellent test-retest agreement was found in the overall score with an ICC of 0.801. For individual domains, the ICCs ranged from 0.437 to 0.737 (Table 3).
Construct Validity
Moderate to strong correlations were found between the overall score and almost all of the SF-36 and EQ-5D domains, for instance, SF-36 physical functioning (ρ = 0.819), SF-36 vitality (ρ = 0.750), and EQ-5D utility (ρ = 0.703) (Table 4). On the other hand, weaker correlations were found between the overall score and SF-36 social functioning (ρ = −0.098), as well as EQ-5D self-care (ρ = −0.331). It should be mentioned that the correlations between the overall score and the five EQ-5D domains (not including the utility index) were negative because of reverse coding.
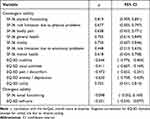 |
Table 4 Construct validity of the SarQoL overall score (n = 58) |
Floor and Ceiling Effects
The minimum and maximum values of the overall score in the sample were 34.84 and 93.94 (corrected to two decimal places), respectively. Each of these values were attained by one and only one participant. In fact, the second lowest and highest values were 36.30 and 91.58 (corrected to two decimal places), respectively, which were clearly distinguishable from the minimum and maximum values. Thus, it can be concluded that both the floor and ceiling effects were absent in the overall score.
Discussion
This study translated the SarQoL questionnaire from English into Cantonese and examined its psychometric properties. Results show that the Cantonese SarQoL questionnaire is ready for use as it has the ability to discriminate sarcopenic individuals from the non-sarcopenic ones, and has acceptable internal consistency, test-retest reliability, and construct validity, as well as having no floor or ceiling effect.
The translation of the questionnaire was completed without significant difficulties. A set of proven procedures was adopted to avoid subjectivity in the translation. The expert committee panel confirmed that the Cantonese SarQoL conveys the same meaning as the original English version. Based on a pilot sample, good face validity was demonstrated.
Regarding the psychometric properties, the present study is largely in line with earlier validation results obtained from the French, English and other populations.18,22,30,31 First, results indicate that the Cantonese SarQoL is able to discriminate between sarcopenic and non-sarcopenic individuals, in the sense that 1) the overall scores were significantly different across the two groups (ie, lower among the sarcopenic individuals), and 2) the overall score was a significant predictor of sarcopenic status (ie, a lower score was associated with a greater likelihood of being sarcopenic). One observation that deserves mention is that two of the domain scores, namely D3 body composition and D6 leisure activities, were not significantly different across the two groups. Although it is not a major issue with respect to the discriminative power of the overall score, some brief explanations are warranted. As regards D3 body composition, the underlying questionnaire items essentially ask the respondents whether, and to what extent, their physical appearances have changed. Since the participants recruited in the present study, regardless of their sarcopenic status, were relatively healthy and high-functioning individuals, it was less likely that the effects caused by sarcopenia, if any, were so detrimental that they could alter the physical appearance substantially. The explanation for D6 leisure activities is similar, which will be touched on again in the next paragraph.
Second, the Cantonese SarQoL has acceptable internal consistency and test-retest reliability. The values of the Cronbach’s alpha and ICC for the overall score were above 0.8, which was satisfactory. Except for D6 leisure activities, the Cronbach’s alpha computed when one of the domain scores was dropped at a time was lower than the original one, hinting that most of the domains are indeed measuring the same construct. As regards D6 leisure activities, although it had the lowest correlation with the overall score (the only one being < 0.6), and the Cronbach’s alpha mildly increased when this domain was dropped, it does not necessarily imply that its psychometric property is undesirable. Instead, such results may be attributed to the fact that all participants, who were recruited from a community-based cohort, were active members in the community centres. Given that the participants were already the more socially active ones, it is conceivable that sarcopenia would not exert as much influence on their quality of life in terms of participating in leisure activities. Indeed, as shown in Table 1, sarcopenic and non-sarcopenic individuals were not significantly different in this domain score. In other words, the sample in the present study probably consisted of those whose participations of leisure activities were affected by sarcopenia to a lesser extent, thereby yielding a seemingly weakened statistical relationship between this particular domain score and the overall score.
Third, the Cantonese SarQoL has acceptable construct validity, as the overall score demonstrated reasonable correlations with the various SF-36 and EQ-5D domain scores. In general, since most of the SF-36 and EQ-5D domains are measuring the same construct as SarQoL does (ie, quality of life), moderate to high correlations were considered evidence for establishing convergent validity. This is in contrast to some of the previous validation studies,22,30,31 which seemed to have considered those SF-36 and EQ-5D domain scores that are more related to mental and psychological health (cf, physical functioning) for the purpose of establishing divergent validity. However, given that numerous research have shown that sarcopenia can lead to poor mental health, for instance depression and depressive symptoms,32 it may not be reasonable to expect low or even negligible correlations between the SarQoL overall score and the mentally-related SF-36 and EQ-5D domain scores. After all, mental health is also a crucial determinant in quality of life, which is an aspect being explicitly measured in the SarQoL questionnaire as well. In view of the above, the present study treated these moderate to high correlations (eg, the one between SarQoL overall score and SF-36 mental health) as evidence for supporting convergent validity, rather than as counter-evidence against divergent validity. To conclude, the Cantonese SarQoL demonstrated acceptable convergent validity.
Notwithstanding the above, the SF-36 social functioning and EQ-5D self-care domains are exceptions that deserve special attention, since their constituent items involve specific wordings that are beyond the scope of the SarQoL questionnaire. For instance, one of the items in the SF-36 social functioning domain is “During the past 4 weeks, to what extent has your physical health or emotional problems interfered with your normal social activities with family, friends, neighbors, or groups?”, and the EQ-5D self-care domain asks whether the respondents have problems washing or dressing themselves. Although these two domains are related to quality of life, they are not those aspects that are directly assessed or mentioned in the SarQoL questionnaire. Thus, these domains should not be treated as exactly measuring the same construct as SarQoL does. Consequently, weaker correlations were expected, and divergent validity should be considered instead of convergent validity. In this regard, the Cantonese SarQoL indeed demonstrated acceptable divergent validity.
Last, the Cantonese SarQoL has no floor or ceiling effect. In other words, although the overall score does have lower and upper limits, it does not inaccurately coerce respondents into a single minimum or maximum category. Statistical variations of the score in the boundary of its numerical range can still be truthfully captured and reflected.
Strengths and Limitations
This study has several major strengths. First, since a standardized translation and validation protocol as proposed by the original developers of the SarQoL questionnaire was adopted, the present results can be easily compared with other validation studies conducted in various populations. Second, the Cantonese SarQoL can take into account the spoken nature of the language and hence can serve as a word-by-word interview prompt such that interviewers can elicit responses from illiterate participants without the need of finding an unbiased way to articulate the questionnaire verbally. This also explains why the Cantonese SarQoL needs to be developed, even though several Chinese versions have already been readily available.22,23
However, the study also has some limitations. For instance, since the participants were relatively healthy and community-dwelling individuals who regularly engaged in social and health promotion activities, they may not be representative of the general older population in Hong Kong. Consequently, some of the present results, such as the relatively poor internal consistency of D6 leisure activities, may not be completely generalizable. On the other hand, the percentage of sarcopenic participants (ie, low muscle strength and/or low physical performance) with severe sarcopenia (ie, low muscle strength and low physical performance) was not that high in this study (29.3%). Although this percentage actually coincided with the population prevalence estimated in other studies,33,34 it still poses the question as to whether the Cantonese SarQoL can be administered specifically to this subpopulation while retaining its validity and reliability. In this regard, further validation studies can be conducted by targeting those who live in long-term care institutions and may have a higher severity level of sarcopenia.
Conclusion and Implications
Despite advances in measurement tools, evaluation of interventions for managing sarcopenia in terms of improving sarcopenia-specific quality of life have been rare, with only some noteworthy exceptions.15,16 To keep pace with the “outcome movement” (ie, outcome-oriented) in healthcare services, the SarQoL questionnaire should be administered in conjunction with traditional measures of clinical endpoints, the results of which would be useful in gauging the interventional effects as well as facilitating comparisons across different contexts. Such a sarcopenic-specific quality of life instrument is not intended to serve as a substitute for clinical measures such as muscle mass, muscle strength, and physical performance. To the contrary, it would serve a complementary function in outcome assessment, making it easier for decision makers and healthcare administrators (eg, frontline community nurses and personal care workers) to identify the interventions or services that are the most useful in managing sarcopenia. To this end, the present study demonstrated that the Cantonese SarQoL is valid and reliable, which can thus be used as an interviewer-administered questionnaire for assessing sarcopenia-specific quality of life in fieldwork practice.
Acknowledgment
We would like to thank the participants of The Jockey Club Elderly Hip Fracture Prevention Programme, and the research team members of The Jockey Club Institute of Ageing and The Jockey Club Centre for Osteoporosis Care and Control of The Chinese University of Hong Kong, for their contributions to this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147(8):755–763. doi:10.1093/oxfordjournals.aje.a009520
2. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European working group on sarcopenia in older people. Age Ageing. 2010;39(4):412–423. doi:10.1093/ageing/afq034
3. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–2646. doi:10.1016/S0140-6736(19)31138-9
4. Yeung SSY, Reijnierse EM, Pham VK, et al. Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta‐analysis. J Cachexia Sarcopenia Muscle. 2019;10(3):485–500. doi:10.1002/jcsm.12411
5. Cawthon PM, Fox KM, Gandra SR, et al. Do muscle mass, muscle density, strength, and physical function similarly influence risk of hospitalization in older adults? J Am Geriatr Soc. 2009;57(8):1411–1419. doi:10.1111/j.1532-5415.2009.02366.x
6. Brown JC, Harhay MO, Harhay MN. Sarcopenia and mortality among a population‐based sample of community‐dwelling older adults. J Cachexia Sarcopenia Muscle. 2016;7(3):290–298. doi:10.1002/jcsm.12073
7. Liu P, Hao Q, Hai S, Wang H, Cao L, Dong B. Sarcopenia as a predictor of all-cause mortality among community-dwelling older people: a systematic review and meta-analysis. Maturitas. 2017;103:16–22. doi:10.1016/j.maturitas.2017.04.007
8. Syddall HE, Martin HJ, Harwood RH, Cooper C, Sayer AA. The SF-36: a simple, effective measure of mobility-disability for epidemiological studies. J Nutr Health Aging. 2009;13:57–62. doi:10.1007/s12603-009-0010-4
9. Rabin R, De Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–343. doi:10.3109/07853890109002087
10. Silva Neto LS, Karnikowiski MG, Tavares AB, Lima RM. Association between sarcopenia, sarcopenic obesity, muscle strength and quality of life variables in elderly women. Braz J Phys Ther. 2012;16:360–367. doi:10.1590/S1413-35552012005000044
11. Yadav A, Chang YH, Carpenter S, et al. Relationship between sarcopenia, six‐minute walk distance and health‐related quality of life in liver transplant candidates. Clin Transplant. 2015;29(2):134–141. doi:10.1111/ctr.12493
12. Beaudart C, Reginster JY, Petermans J, et al. Quality of life and physical components linked to sarcopenia: the SarcoPhAge study. Exp Gerontol. 2015;69:103–110. doi:10.1016/j.exger.2015.05.003
13. Morishita S, Kaida K, Tanaka T, et al. Prevalence of sarcopenia and relevance of body composition, physiological function, fatigue, and health-related quality of life in patients before allogeneic hematopoietic stem cell transplantation. Support Care Cancer. 2012;20:3161–3168. doi:10.1007/s00520-012-1460-5
14. Beaudart C, Biver E, Reginster JY, et al. Development of a self-administrated quality of life questionnaire for sarcopenia in elderly subjects: the SarQoL. Age Ageing. 2015;44(6):960–966. doi:10.1093/ageing/afv133
15. Tsekoura M, Billis E, Tsepis E, et al. The effects of group and home-based exercise programs in elderly with sarcopenia: a randomized controlled trial. J Clin Med. 2018;7(12):480. doi:10.3390/jcm7120480
16. Dupont J, Wauters E, Dedenye L et al. Are dietary intake and nutritional status of specific polyunsaturated fatty acids correlated with sarcopenia outcomes in community-dwelling older adults with sarcopenia? - Exploratory results from ENHANce. BMC Geriatrics. 2023, ;23 1 :272. doi:10.1186/s12877-023-04007-9
17. SarQoL. Sarcopenia quality of life. Available from: https://www.sarqol.org/.
18. Beaudart C, Biver E, Reginster JY, et al. Validation of the SarQoL®, a specific health‐related quality of life questionnaire for Sarcopenia. J Cachexia Sarcopenia Muscle. 2017;8(2):238–244. doi:10.1002/jcsm.12149
19. Yu R, Wong M, Leung J, Lee J, Auyeung TW, Woo J. Incidence, reversibility, risk factors and the protective effect of high body mass index against sarcopenia in community-dwelling older Chinese adults. Geriatr Gerontol Int. 2014;14:15–28.
20. Cheng KY, Chow SK, Hung VW et al, et al. Diagnosis of sarcopenia by evaluating skeletal muscle mass by adjusted bioimpedance analysis validated with dual-energy X-ray absorptiometry. J Cachexia Sarcopenia Muscle. 2021;12(6):2163–2173. doi:10.1002/jcsm.12825
21. Zhu LY, Chan R, Kwok T, Cheng KCC, Ha A, Woo J. Effects of exercise and nutrition supplementation in community-dwelling older Chinese people with sarcopenia: a randomized controlled trial. Age Ageing. 2019;48(2):220–228. doi:10.1093/ageing/afy179
22. Le X, Wei Y, Hao D, et al. Psychometric properties of the Chinese version of the sarcopenia and quality of life, a quality of life questionnaire specific for sarcopenia. Calcif Tissue Int. 2021;109(4):415–422. doi:10.1007/s00223-021-00859-8
23. Lee SC, Chang CF, Wang JY, Liang PJ. Translation and validation of the Taiwanese SarQoL, a quality of life questionnaire specific to sarcopenia. J Formos Med Assoc. 2023;122(3):249–257. doi:10.1016/j.jfma.2022.09.012
24. Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–307. e302. doi:10.1016/j.jamda.2019.12.012
25. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. doi:10.1007/BF02310555
26. DeVellis RF, Thorpe CT. Scale Development: Theory and Applications.
27. Nunnally JC, Bernstein IH. Psychometric Theory.
28. Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi:10.1016/j.jclinepi.2006.03.012
29. Wong ELY, Ramos-Goni JM, Cheung AWL, Wong AYK, Rivero-Arias O. Assessing the use of a feedback module to model EQ-5D-5L health states values in Hong Kong. Patient. 2018;11:235–247. doi:10.1007/s40271-017-0278-0
30. Beaudart C, Edwards M, Moss C, et al. English translation and validation of the SarQoL®, a quality of life questionnaire specific for sarcopenia. Age Ageing. 2017;46(2):271–276. doi:10.1093/ageing/afw192
31. Geerinck A, Scheppers A, Beaudart C, et al. Translation and validation of the Dutch SarQoL®, a quality of life questionnaire specific to sarcopenia. J Musculoskelet Neuronal Interact. 2018;18(4):463.
32. Chang KV, Hsu TH, Wu WT, Huang KC, Han DS. Is sarcopenia associated with depression? A systematic review and meta-analysis of observational studies. Age Ageing. 2017;46(5):738–746. doi:10.1093/ageing/afx094
33. Wu X, Li X, Xu M, Zhang Z, He L, Li Y. Sarcopenia prevalence and associated factors among older Chinese population: findings from the China Health and Retirement Longitudinal Study. PLoS One. 2021;16(3):e0247617. doi:10.1371/journal.pone.0247617
34. Petermann‐Rocha F, Balntzi V, Gray SR, et al. Global prevalence of sarcopenia and severe sarcopenia: a systematic review and meta‐analysis. J Cachexia Sarcopenia Muscle. 2022;13(1):86–99. doi:10.1002/jcsm.12783
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
