Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 12
Transient Osteoporosis of the Hip: Risk and Therapy
Authors Bashaireh KM , Aldarwish FM, Al-Omari AA, Albashaireh MA, Hajjat M, Al-Ebbini MA , Aleshawi AJ
Received 28 October 2019
Accepted for publication 18 December 2019
Published 9 January 2020 Volume 2020:12 Pages 1—8
DOI https://doi.org/10.2147/OARRR.S236324
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Khaldoon M Bashaireh,1 Fa’ek M Aldarwish,1 Ali A Al-Omari,1 Moath A Albashaireh,1 Mai Hajjat,2 Mohammad A Al-Ebbini,3 Abdelwahab J Aleshawi3
1Department of Special Surgery, Division of Orthopedics, Faculty of Medicine, Jordan University of Science and Technology, Irbid 22110, Jordan; 2Princess Rahma Pediatric Hospital, Jordanian Ministry of Health, Irbid, Jordan; 3Internship, King Abdullah University Hospital, Irbid 22110, Jordan
Correspondence: Khaldoon M Bashaireh
Department of Special Surgery, Division of Orthopedics, Faculty of Medicine, Jordan University of Science and Technology, PO Box: 3030, Irbid 22110, Jordan
Tel +962 799051087
Fax +962 2-7201064
Email [email protected]
Objective: The aim of this study was to investigate the impact of occupation in patients with transient osteoporosis of the hip (TOH). The study also compares two different types of management for this condition: conservative treatment and surgical drilling.
Methods: This was a retrospective case series study. The medical records for patients diagnosed with TOH at our institution within the period 2012–2017 were retrieved. General demographic data, clinical features, and diagnostic modalities were obtained. In addition, management procedures and their associated prognostic factors were acquired. The effectiveness of these procedures was assessed by the number of days of sick leave, the time needed for full recovery and the number of recurrences of TOH. Also, pain responses at 24 hrs, 48 hrs, and at 1 week were estimated subjectively through a “pain score” out of 10, and objectively through the degree of improvement in daily activity. The patients had a regular follow-up at 4- to 6-week intervals.
Results: In total, 15 cases of TOH, 14 men and one woman, were enrolled in the study. The mean age of the patients was 41 years (range 26–59 years). Out of the 15 cases, nine were healthcare professionals (eight physicians and one nurse). Ten patients underwent hip drilling for core decompression and five patients were treated conservatively. The time needed for full recovery was 5.8 weeks for those who underwent drilling, and 48.3 weeks for three patients receiving conservative treatment. The other two patients who were treated conservatively had not achieved full or near-full recovery at the time of reporting this study.
Conclusion: Physicians may be at increased risk of developing TOH. Further studies should be conducted to examine the role of this occupation as a risk factor. In addition, hip drilling should be considered as an effective treatment modality, especially in those patients who seek a faster recovery.
Keywords: hip, bone marrow edema, core decompression, healthcare professionals
Introduction
Transient osteoporosis of the hip (TOH) was first described in 1959 by Curtiss and Kincaid who reported the radiograph examinations in three pregnant women who had severe hip pain.1 More recently, the increasing utilization of magnetic resonance imaging (MRI) has allowed physicians to investigate edematous changes in bone marrow, an entity previously undetected on conventional radiographs such as radiograph. The first use of the term “bone marrow edema” was by Wilson et al in 1988, and the term “bone marrow edema syndrome” was described in 1993 after the investigation of histological specimens.2 Since then, the condition has received various definitions including “transient regional osteoporosis” and “chronic regional pain syndrome”.3
TOH is an uncommon disorder characterized by transient pain and disability with radiological findings such as osteopenia in the hip area.4 The populations mainly affected are middle-aged men, and pregnant women during the last trimester or the immediate post-partum period.5–7 It is an idiopathic event, not related to trauma and presents with a spontaneous sudden-onset pain in the hip, extending to the groin.5 It is associated with a limitation of movement and disability; nevertheless, the symptoms gradually disappear within 6–12 months.6 The main management lines include a conservative approach such as restricted weight-bearing, anti-resorptive medications and analgesics, or combined management including surgery.7 The pathogenesis of this condition is unclear, and at the present time, no study has investigated the role of occupation as a risk factor for TOH.
The aim of this study is to investigate the impact of occupation on patients with TOH. In addition, two different lines of management, conservative treatment and surgical drilling, are compared.
Materials and Methods
The study, clinical diagnosis, and treatment were conducted at King Abdullah University Hospital affiliated to Jordan University of Science and Technology. Also, the study is conducted in accordance with Declarations of Helsinki. After obtaining approval from the Institutional Review Board (IRB), we examined our institution’s medical records database and retrospectively identified patients who were diagnosed with transient osteoporosis of the hip (TOH) between January 2012 and December 2017. Electronic medical records were retrieved, personal contact was established, and general demographic data, clinical characteristics, and diagnostic modalities were obtained. In addition, management techniques and their associated prognostic course were acquired.
Only patients diagnosed as cases of TOH, confirmed by magnetic resonance imaging (MRI), were included. The general demographic data included age, sex, career, and body mass index (BMI). The clinical characteristics included smoking, alcohol consumption, trauma and family history, presenting symptoms (pain during activity, resting pain, nocturnal pain and limitations of movement) and duration, medication history, endocrine disease history, and hormonal profile. Different diagnostic tools were utilized such as plain radiograph, MRI, computed tomography (CT) scan, and bone scan, and the resultant findings were categorized as diagnostic findings or non-significant findings.
The main treatment methods were either conservative treatment through analgesics or surgical treatment by femoral head drilling for core decompression. The effectiveness of these modalities was assessed by multiple approaches. First, the amount of sick leave was calculated for all patients. Second, the time needed for full recovery was measured. Third, recurrences of TOH were noted and their time to full recovery was measured. Pain responses at 24 hrs, 48 hrs, and at 1 week were estimated subjectively through a “pain score” out of 10, and objectively through the degree of improvement in daily activity.
Setting
The diagnosis of TOH was based on acute onset of hip pain without any history of trauma, vascular incidents or infection, and which was confirmed through MRI to be due to bone marrow edema and joint effusion (intermediate signal intensity of bone marrow in the femur on T1-weighted images, increased intensity on T2-weighted images and delayed peak enhancement of edematous marrow). The diagnosis was also based on the resolution of symptoms and radiological findings. All patients underwent MRI of the hip joints at the time of presentation, and, if necessary, at the time of recurrence of symptoms. Standard T1-weighted axial and coronal images were obtained with and without intravenous gadolinium administration, along with T2- and T2-fat-suppressed weighted axial, coronal, and sagittal images. The imaging studies were reviewed and interpreted by two expert radiological consultants. All patients were informed of the diagnosis and they decided the preferred treatment method.
Surgical drilling for “core decompression” of the femoral head was performed by an experienced orthopedic surgeon (KB) who followed the same procedure in each patient. After consenting to the preferred treatment option, the patient is placed in supine position and under general or spinal anesthesia in an aseptic technique, small incision of 1 cm proximal and lateral aspect of the femur was created under fluoroscopic guidance introducing a guidewire laterally and proximal to the lesser trochanter directed from the lateral aspect of the femur through the neck reaching the head and limited to 5 mm subcortical generally toward the most affected area (in our cases most of the head and neck areas were affected) followed by drilling with a 7mm cannulated drill bit. Further drilling could be performed by using a smaller size drill bit or using a Kirschner wire which was used in 2 of our patients. Upon discharge, the patients were advised to follow a schedule of non-weight bearing on the affected limb for 2 weeks, then 50% weight bearing for a further 2–4 weeks, then increasing the weight bearing until full weight bearing after a further 4 weeks. Many patients achieved faster recovery and did a faster schedule.
For patients receiving conservative treatment, this included different forms of analgesics such as non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or opioids. The doses were as follows: for NSAID, it was diclofenac sodium 75 mg twice a day. For paracetamol, it was 1000mg my three times a day. For the opioid, it was tramadol 100 mg once a day. Restricted weight bearing ranged from non- to partial weight bearing depending on the progression of the clinical situation with regular follow-up at 4- to 6-week intervals and with the patient undertaking a range of home-based motion exercise. All cases were followed.
Statistical Analyses
Data were entered into a spreadsheet. Statistical analyses were performed using IBM SPSS Statistics software, version 21 (IBM Corp., Armonk, NY, USA). Limited statistical tests were applied due to the small sample size.
Results
Patient Demographics and Clinical Characteristics
Fifteen patients (14 men and one woman) with TOH were enrolled in the study. Their mean age was 41 years (range 26–59 years). Out of the 15 patients, there were nine healthcare professionals (eight physicians and one nurse). Their mean BMI was 28.2. More than half of the patients were smokers (eight patients) and two reported alcohol consumption. The duration of symptoms until diagnosis of TOH ranged from 14 days up to 1 year with a mean of 64.3 days and median of 30 days. The main presenting symptoms were pain during activity, resting pain, night pain, and limitation of movement. The left hip was affected in nine cases and the right hip in seven cases (one patient had bilateral TOH). No personal history of trauma or endocrine disorders was reported. However, a family history of TOH was present in three patients (2 mothers and one father). The clinical characteristics are summarized in Table 1.
 |
Table 1 General Demographic and Clinical Characteristics |
Diagnosis
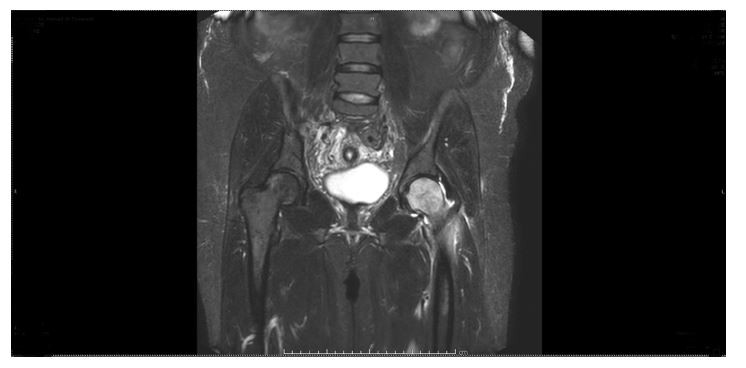
Each patient underwent MRI. The characteristic features on MRI, seen in all our patients, were a pattern of diffuse edema, the absence of focal defects, an intact articular surface, and the absence of a double-line sign, usually associated with joint effusion. The diffuse edema pattern was identified by a homogeneously decreased signal on T1-weighted images and a homogeneously increased signal on fat-suppressed T2-weighted images, extending from the superior articular surface of the femoral head to the femoral neck and intertrochanteric region (Figures 1 and 2). Bone scanning was performed on six patients and all revealed uniformly increased uptake at the affected femoral head extending down into the femoral neck and intertrochanteric region. As an initial step, radiograph examinations did not reveal specific findings in 11 patients, while in three patients, the radiograph images showed findings suggestive of subchondral cortical loss involving the femoral head and neck, osteopenia of the femoral head, and effusion with joint space preservation. A CT scan was performed in only a few cases.
 |
Figure 1 T2-weighted MRI: Coronal view indicating diffuse bone marrow edema of the left hip. |
 |
Figure 2 T1-weighted MRI: Axial view demonstrating bone marrow edema of the left hip. |
Treatment and Prognosis
Ten patients underwent hip drilling for core decompression and five patients were treated conservatively. The most frequent class of drugs used was NSAIDs Table 2. The effectiveness of the medication was assessed subjectively in patients who underwent hip drilling (assessed prior to surgery) and in those who received conservative treatment only. Most patients reported that the medication was ineffective or had little effect. Patients who elected for core decompression underwent surgery less than 1 month after the diagnosis apart from three patients who were operated 2, 4, and 5 months after diagnosis. The pain score was assessed prior to surgery, after 24 hrs postoperatively, and after 2 days and 1 week. The preoperative pain score ranged from 7 to 10. However, the score dropped significantly after that Figure 3. The time needed for full recovery was 5.8 weeks for those who underwent hip drilling for core decompression and was 48.3 weeks for three patients who received conservative treatment. At the present time, the other two of the five treated conservatively had not achieved full or near-full recovery.
 |
Table 2 Treatment Modalities |
 |
Figure 3 A chart indicating the changes in pain score for every patient underwent surgical drilling. |
Out of the 10 cases who underwent surgery, three had a recurrence (two of them less intense than the first episode and one more intense). Moreover, out of the five cases treated conservatively, two did not achieve full recovery and one of them had a recurrence. Table 3 summarizes the different prognostic indicators.
 |
Table 3 Prognostic Outcome |
Discussion
This study highlights the possibility that the occupation of physician may put these healthcare professionals at increased risk of developing TOH. Out of the 15 patients diagnosed with TOH at our institution, eight were physicians (53.3%) and nine cases (eight physicians and one nurse) were healthcare professionals (60%). Furthermore, this study demonstrates that hip drilling for core decompression provides faster recovery with less chance of recurrence and better pain control, especially for those whose career requires intensive work as physicians. Previously, only one study focused on the prevalence of occupation as a risk factor for TOH. Interestingly, those authors found that 11 out of 17 patients were physicians.8 Hadidy et al first raised the question of whether occupation, physician, in particular, is a risk factor for developing TOH.8 Moreover, Sharma et al reported a case of TOH in a 38-year-old male physician.9
The pathogenesis of TOH is still unclear. The literature supports several theories, but clear evidence is lacking. The strongest theory suggested is that a venous obstruction may play an essential role in TOH.10–12 Koo et al suggested that coagulopathic factors result in an intraosseous ischemic event, affecting the veins and venous sinusoids of the hip.12 Other models have shown elevated levels of lipoprotein and plasminogen activator inhibitor in TOH, which suggests that a hypofibrinolytic or thrombophilic process may cause intraosseous venous obstruction.13–15 Consequent complete fibrinolysis produces reperfusion and reactive hyperemia, which may explain the reversibility of the symptoms.15 Furthermore, Plenk et al demonstrated increased intramedullary pressures and abnormal intraosseous venography in their bone exploration model on TOH.11 Increased numbers of erythrocytes in bone biopsies of pregnant patients with TOH have also been reported, which reinforces the role of venous stasis.10 It is important to mention that the risk factors (other than pregnancy) suggested for TOH include trauma, alcohol consumption, steroid usage, smoking, hypothyroidism, hypophosphatasia, osteogenesis imperfecta, low testosterone levels, and low vitamin D (25-cholecalciferol).16–19 In this study, no hormonal abnormalities were detected among our patients, either clinically or biochemically. In addition, no trauma events were recalled. Alcohol consumption was reported in two patients who were not physicians. Accordingly, the occupation of the physician could be considered and investigated as an independent risk factor for TOH. In view of the aforementioned suggested venous occlusion pathophysiology, the higher prevalence of physicians could be explained by their long periods of standing and long work sessions. On the other hand, it would be explained by the easier access for consultations by the healthcare stuff although the musculoskeletal consultations are easily accessed and available for everyone and it is accounted the higher numbers of clinic and imaging referrals in our institution. Interestingly, three cases reported a family history with the same complaint. Previously, two reported cases have investigated the genetic factors. In these case reports, human leukocyte antigen (HLA) DR7 homology was commonly detected, and it was concluded that a certain HLA phenotype constitutes the risk of developing TOH.20,21 Recently, Karlıbel et al reported cases of TOH in the same family.22 Also, the familial presentation was first reported in three brothers with TOH in 1983.20 In addition, Bijl et al reported a daughter and a father with TOH in 1999.21
Surgical drilling for core decompression of the femoral head in the treatment of TOH is still a debatable approach among clinicians and researchers in terms of effectiveness, rapidity of recovery, the potential for complications, and the genuine need for it given that conservative treatment is quite effective.7 Many researchers have argued that, despite the fact that conservative treatment provides effective symptomatic relief, it never shortens the course of the disease. In other clinical studies, core decompression was shown to be an effective therapeutic measure with faster recovery.23 Some studies clearly identified core decompression of the femoral head as a treatment mode with significantly faster recovery but suggested that it is an unnecessary procedure.24 In this study, patients who underwent hip drilling experienced faster recovery, shorter duration of sick leave, better pain control, and a lower rate of recurrence. This could be extremely important for physicians whose career can be physically strenuous. Most cases who underwent hip drilling recovered in less than 1 month, which is even faster than conservative treatment with intravenous pamidronate, which had a 2-month recovery duration.
TOH as a distinct clinical entity is not well understood and is poorly studied in the literature; many practicing physicians are not aware of it. Correct diagnosis of this condition and discrimination from other hip pathologies such as avascular necrosis (AVN) of the femoral head, insufficiency fracture, and infection are important.25 TOH is easily misdiagnosed as AVN of the femoral head, AVN usually presenting with less acute onset and with the potential to progress into femoral head collapse. On the other hand, TOH has a more benign final outcome demonstrated by spontaneous resolution within 6–12 months.25 Imaging modalities used in the diagnosis of TOH include plain radiographs, which are usually normal in the early course of the disease; changes occur around 4 weeks after the onset of symptoms and they include diffuse osteopenia of the femoral head. Radiographs of AVN show a rim of sclerosis followed by femoral head collapse. MRI of TOH shows decreased signal intensity on T1-weighted images, and increased signal intensity on T2-weighted images.25 A bone scan reveals homogenous increased uptake in the femoral head and neck; however, it is sensitive to, but not specific for, TOH.25 We believe that TOH could be a subset of bone marrow edema syndrome, as it has many similarities with it, namely, an unknown cause, characteristic pain (which is usually out of proportion to the physical and radiological findings), vasomotor dysfunction of the extremity and it develops in the absence of an identifiable precipitating event. The urge need is to differentiate TOH from other similar serious clinical conditions such as avascular necrosis, insufficiency fracture, infective, and inflammatory arthritis.
Our study is not without limitations, the main points being the retrospective nature of the study and the small sample size. The role of bisphosphonates was not studied as the general protocol for the treatment of cases of TOH is either the conservative or surgical treatment. Also, the specific hip joint outcome was not studied as it is a retrospective study.
In conclusion, the occupation of a physician may put these healthcare professionals at increased risk of developing TOH or it may indicate that the healthcare stuff have easier access for investigations. Further studies should be conducted to understand the risk factor involved in this occupation. In addition, hip drilling for core decompression would be considered as an effective treatment modality, especially in those patients who seek a faster recovery. Orthopedic surgeons have to be aware of this condition and distinguish it from AVN.
Ethics Statement
Institutional approval was obtained from the Institutional Review Board at Jordan University of Science and Technology. This study was conducted in accordance with the Declaration of Helsinki. The consent was waived due to the retrospective nature of the study. We confirm that the privacy of the participants was saved, and the data were anonymized and maintained with confidentiality.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Curtiss PH
2. Wilson AJ, Murphy WA, Hardy DC, Totty WG Transient osteoporosis: transient bone marrow edema? Radiology. 1988; 167(3): 757–760. doi:10.1148/radiology.167.3.3363136
3. Cano-Marquina A, Tarin JJ, Garcia-Perez MA, Cano A Transient regional osteoporosis. Maturitas. 2014; 77(4):324–329. doi:10.1016/j.maturitas.2014.01.012
4. Mutluoglu M, Sonmez G, Sivrioglu AK, Ay H There may be a role for hyperbaric oxygen therapy in transient osteoporosis of the hip. Acta Orthop Belg. 2012; 78(5):685–687.
5. Emad Y, Ragab Y, El-Shaarawy N, Rasker JJ Transient osteoporosis of the hip, complete resolution after treatment with alendronate as observed by MRI description of eight cases and review of the literature. Clin Rheumatol. 2012; 31(11):1641–1647. doi:10.1007/s10067-012-2060-y
6. Patel S Primary bone marrow oedema syndromes. Rheumatology (Oxford). 2014; 53(5):785–792. doi:10.1093/rheumatology/ket324
7. Asadipooya K, Graves L, Greene LW Transient osteoporosis of the hip: review of the literature. Osteoporos Int. 2017; 28(6):1805–1816. doi:10.1007/s00198-017-3952-0
8. Hadidy AM, Al Ryalat NT, Hadidi ST, et al. Male transient hip osteoporosis: are physicians at a higher risk? Arch Osteoporos. 2009; 4(1–2):41–45. doi:10.1007/s11657-009-0025-9
9. Sharma G, Bhardwaj A, Relwani N, Dubey S. Transient osteoporosis of hip in a middle-aged man. Biomed J Sci Tech Res. 2017; 1(6):1574–1576. BJSTR.MS.ID.000489.
10. Rosen RA Transitory demineralization of the femoral head. Radiology. 1970; 94:509–512. doi:10.1148/94.3.509
11. Plenk PH
12. Koo KH, Jeong ST, Jones JP Borderline necrosis of the femoral head. Clin Orthop Relat Res. 1999; 358:158–165. doi:10.1097/00003086-199901000-00019
13. Koo KH, Ahn IO, Song HR, Kim SY, Jones JP
14. Berger CE, Kro¨ner AH, Minai-Pour MB, Ogris E, Engel A Biochemical markers of bone metabolism in bone marrow edema syndrome of the hip. Bone. 2003; 33:346–351. doi:10.1016/S8756-3282(03)00164-9
15. Orth P, Anagnostakos K Coagulation abnormalities in osteonecrosis and bone marrow edema syndrome. Orthopedics. 2013; 36:290–300. doi:10.3928/01477447-20130327-08
16. Diwanji SR, Cho YJ, Xin ZF, Yoon TR Conservative treatment for transient osteoporosis of the hip in middle-aged women. Singapore Med J. 2008; 49(1):17–21
17. Daniel RS, Farrar EK, Norton HR, Nussbaum AI Bilateral transient osteoporosis of the talus in pregnancy. Osteoporos Int. 2009; 20(11):1973–1975 doi:10.1007/s00198-009-0902-5
18. Jennings PE, Malley BP, Griffin KE, Northover B, Rosenthal FD Relevance of increased serum thyroxine concentrations associated with normal serum triiodothyronine values in hypothyroid patients receiving thyroxine: a case for “tissue thyrotoxicosis”. BMJ. 1984; 289:1645–1647 doi:10.1136/bmj.289.6459.1645
19. Duncan CR, Evans RA, Somers NM Bone death in transient regional osteoporosis. Bone. 1992; 13:161–165. doi:10.1016/8756-3282(92)90006-I
20. Albert J, Ott H Three brothers with algodystrophy of the hip. Ann Rheum Dis. 1983; 42: 421–424. doi:10.1136/ard.42.4.421
21. Bijl M, van Leeuwen MA, van Rijswijk MH Transient osteoporosis of the hip: presentation of (a) typical cases and a review of the liter-atüre. Clin Exp Rheumatol. 1999; 17: 601–604.
22. Karlıber Aİ, Aksoy KM, Lale A Familial transient osteoporosis of the hip? On account of three cases from the same family. Erciyes Med J 2018; 40(1): 45–49.
23. Calvo E, Fernandez-Yruegas D, Alvarez L Core decompression shortens the duration of pain in bone marrow oedema syndrome. Int Orthop. 2000; 24:88–91. doi:10.1007/s002640000120
24. Radke S, Kirschner S, Seipel V, Rader C, Eulert J Treatment of transient bone marrow oedema of the hip—a comparative study. Int Orthop. 2003; 27:149–152. doi:10.1007/s00264-003-0452-y
25. Balakrishnan A, Schemitsch EH, Pearce D, McKee MD Distinguishing transient osteoporosis of the hip from avascular necrosis. Can J Surg. 2003; 46(3):187–192.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
