Back to Journals » Clinical Ophthalmology » Volume 14
Topography-Guided Refractive Astigmatism Outcomes: Predictions Comparing Three Different Programming Methods
Authors Stulting RD , Durrie DS , Potvin RJ , Linn SH , Krueger RR , Lobanoff MC , Moshirfar M, Motwani MV , Lindquist TP , Stonecipher KG
Received 2 January 2020
Accepted for publication 24 March 2020
Published 24 April 2020 Volume 2020:14 Pages 1091—1100
DOI https://doi.org/10.2147/OPTH.S244079
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
R Doyle Stulting, 1 Daniel S Durrie, 2 Richard J Potvin, 3 Steve H Linn, 4 Ronald R Krueger, 5 Mark C Lobanoff, 6 Majid Moshirfar, 4, 7 Manoj V Motwani, 8 Timothy P Lindquist, 2 Karl G Stonecipher 9
1Woolfson Eye Institute, Atlanta, GA, USA; 2DurrieVision, Kansas City, KS, USA; 3Science in Vision, Akron, NY, USA; 4Hoopes, Durrie, Rivera Research, Draper, UT, USA; 5Cleveland Clinic, Cleveland, OH, USA; 6North Suburban Eye Specialists, Minneapolis, MN, USA; 7John A. Moran Eye Center, University of Utah, Salt Lake City, UT, USA; 8Motwani LASIK Institute, San Diego, CA, USA; 9TLC Laser Centers, Greensboro, NC, USA
Correspondence: R Doyle Stulting 224 Konawa LN, Loudon, TN 37774, USA
Tel +1 770-804-1684
Email [email protected]
Purpose: To identify the laser programming strategy that will achieve optimal refractive outcomes of LASIK with a topography-guided laser for eyes with a disparity between cylinder measured by manifest refraction and cylinder measured by topography.
Setting: Six surgeons at 5 clinical sites in the USA.
Design: Retrospective data review.
Methods: Preoperative, treatment, and postoperative data on 52 eyes that underwent topography-guided LASIK with the WaveLight EX500 Contoura® Vision excimer laser ablation profile in which the vectors representing the preoperative refractive cylinder and the cylinder measured by the WaveLight® Topolyzer™ VARIO Diagnostic Device (Vario cylinder) differed by >/= 0.50D and/or >/= 10 degrees of orientation were analyzed retrospectively. Data were contributed by six surgeons using the laser at 5 different clinical sites. Vector analysis of postoperative cylindrical refractive error and the actual laser programming strategy was used to calculate the cylindrical correction that would, theoretically, have completely eliminated postoperative refractive cylinder. This was compared to expected results using the preoperative manifest cylinder, the topographic cylinder, and the Phorcides Analytic Engine (Phorcides LLC, North Oaks MN; Phorcides). For analysis, subjects were stratified on the basis of the vector difference between Manifest and Topo cylinder (High, > 0.75 D; and Low, ≤ 0.75 D).
Results: The poorest calculated theoretical outcomes were obtained with the manifest refraction (centroid: − 0.43, 0.22; mean calculated error vector: 0.56 ± 0.42 D; p=ns). Better outcomes were obtained with the topographically measured refraction (centroid: 0.37, 0.02; mean calculated error vector: 0.47 ± 0.33 D; p=ns). The best outcomes were obtained with Phorcides (centroid: − 0.15, 0.06; mean calculated error vector: 0.39 ± 0.28 D; p=ns). The mean error vector magnitude in the Phorcides Low group was significantly lower than for the Manifest and Topo Low groups (0.26 D vs 0.48 D and 0.33 D; p< 0.01). The mean error magnitude in the Phorcides High group was nearly 0.25 D lower than for the Manifest High group (0.48 D vs 0.70 D; p< 0.01), but was the same as for the Topo High group (0.48 D vs 0.48 D).
Conclusion: Our study suggests that using the topographically measured cylinder or the cylinder selected by Phorcides will produce more desirable refractive outcomes than entry of the preoperative refractive cylinder as the basis for correction of myopia and myopic astigmatism with the WaveLight Contoura Vision excimer laser.
Keywords: LASIK, topography, excimer, laser, PRK, astigmatism
A Letter to the Editor has been published for this article.
Plain Language Summary
Laser refractive surgery is one of the most common elective eye surgical procedures in the world. Many individuals wishing to reduce their need for glasses decide to have it. Modern technology has made the procedure very safe and effective.
Most of the time, the surgery is based only on the prescription for glasses, usually determined in the office by asking patients to choose the lens that gives them the best vision (refraction). While this may be a good starting point, adjustments in the treatment to remove any irregularities in the curvature of the front surface of the eye (the cornea) may make the vision even better. Sophisticated instruments can measure the shape of the cornea in great detail. These devices produce a map of the corneal shape, called a topographic map, that resembles a contour map in geography that shows the peaks and valleys on the surface of the earth.
The FDA recently approved an excimer laser refractive treatment based on both the refraction and the corneal topography. Reported results were excellent. There are several possible methods to design the treatment, but only one was studied in the FDA clinical trial. This study was based on theoretical outcomes that might result if some alternative methods were used to design the treatment. While all results were good, the best results were found with a new software program that helps surgeons with their surgical planning.
Introduction
Most currently used refractive lasers employ wavefront-guided treatment profiles. Topography-guided treatment has traditionally been reserved for complex cases with irregular astigmatism.1 One topography-guided LASIK procedure (Contoura® Vision, Alcon, Fort Worth, Texas, USA) has been shown to provide excellent visual outcomes in normal eyes without irregular astigmatism, with 93% of eyes achieving 20/20 or better UDVA and 34% achieving 20/12.5 or better UDVA at 12 months.2
Because corneal topography does not provide any information about the refractive status of the eye, the user must enter low-order aberrations (sphero-cylindrical refraction), which are combined with high-order aberrations measured by a Placido topographer, to create a shot file designed to eliminate the refractive error of the eye by changing the corneal curvature. On the Treatment Plan page of the laser notebook, three sphero-cylindrical refractions are shown: Clinical, Measured, and Modified (Figure 1).
 |
Figure 1 Treatment planning page for the WaveLight Contoura® Vision laser. |
The Clinical refraction is the preoperative subjective manifest refraction. The cylinder from this entry is termed the Manifest cylinder in this report. The Measured refraction is the sphero-cylindrical correction that is necessary to neutralize regular, low-order corneal astigmatism after removal of high-order aberrations on the cornea. It is termed the Topo cylinder in this report (to distinguish it from the cylinder measured by refraction). The Topo cylinder is derived from Placido topography obtained by the WaveLight® Topolyzer™ VARIO Diagnostic Device (Vario; Alcon, Ft. Worth, TX). The Modified refraction, which is entered by the user, is then combined with high-order aberrations to create the refractive ablation that is intended to correct vision. This entry is termed the Treatment refraction in this report. The WaveLight laser provides the user with the opportunity to select the Modified refraction based on the desired clinical outcome, the Manifest cylinder, the Topo cylinder, or any other factor(s).
Optimally, the Manifest and Topo cylinder will be the same or similar, but in some cases, they differ by more than a trivial amount. Possible explanations for this difference include the presence of significant high-order corneal aberrations3–6 posterior corneal astigmatism, and lenticular astigmatism. Manifest and Topo cylinders tend to differ in eyes with high-order aberrations because the subject may choose a sphero-cylindrical refraction in an attempt to correct high-order aberrations. For example, a subjective refraction may result in cylinder that is selected by the subject in an effort to reduce the blur circle created by coma.4,5 If visually significant coma is treated by topography-guided LASIK, there is no longer a need for correction with low-order refractive cylinder when it is induced by the high-order aberrations.4,5 High-order aberrations may also produce a different subjective refractive cylinder that depends in magnitude and/or angle on the size and location of the pupil, as the pupillary opening restricts light striking the retina to portions of the cornea that may have different high-order aberrations.7
During the FDA clinical trial of the Contoura, the clinical protocol required that investigators enter the Manifest refraction as the Treatment refraction during treatment planning. This requirement was based on the early report of Tan et al that good outcomes could be obtained by programming the laser with the cylinder obtained by refraction, rather than that measured by topography.8 Throughout the FDA study, there was good agreement between Manifest and Topo cylinder because subjects with significant corneal high-order aberrations were specifically excluded from the trial, as required by the FDA.2
After approval, when the laser became widely used in clinical settings, it was used to treat eyes with more irregular topographies and greater disparity between Manifest and Topo cylinder than was encountered in the FDA clinical trial. Clinical experience after FDA approval of the laser led some to hypothesize that programming with the Manifest cylinder might not produce optimal results in eyes with significant HOA.
In 2016, Motwani reported 78% of eyes with 20/15 vision 3 months after initial treatment with the Contoura laser using the LYRA (Layer Yolked Reduction of Astigmatism) Protocol, which is based on the Topo cylinder with spherical adjustment to maintain the spherical equivalent of the manifest refraction4,9,10 This protocol also produced excellent Refractive Status and Vision Profile subjective patient survey outcomes.11
Also in 2016, Kanellopoulos used the Topo cylinder modified to preserve the spherical equivalent of the manifest refraction to obtain 20/16 or better in 50% of eyes, compared to 22% of eyes in which manifest refraction was used to program the laser.12
In a more recent study, Wallerstein et al programmed the laser with the magnitude of the manifest cylinder and the Topo axis. They compared results to those obtained by programming the laser with the manifest cylinder and the manifest cylinder axis. They found that the outcomes using the Topo axis were inferior to those obtained with the cylinder axis measured by the manifest refraction.6
These published findings and the unpublished experiences of others, including the authors of this paper, have led to further discussions about whether the method of programming the laser that was used during the FDA clinical trial produces optimal outcomes.
The purpose of this study was to analyze retrospectively the sphero-cylindrical refractive outcome when there was a disparity between the Manifest cylinder measured preoperatively and the Topo cylinder measured by topography (>/= 0.50 D and/or >/= 10 degrees). Known outcomes with actual programming strategies were used to simulate outcomes that would have been obtained by back-calculation using three different refractive inputs for treatment planning: Manifest cylinder (based on the clinical refraction), Topo cylinder (based on Placido topography obtained with the Vario topographer), and Phorcides cylinder (calculated using the Phorcides Analytic Engine, Phorcides LLC, North Oaks MN).
Methods
This study was determined to be exempt from IRB review according to 45 CFR 46.101(b)(4) by Salus IRB.
Refractive and treatment data from cases in which the preoperative manifest cylinder and topographic cylinder differed by 0.50D or more in magnitude and/or 10 degrees or more in orientation were contributed retrospectively by 6 users of the Contoura® Vision at 5 sites. Three-month postoperative examinations (range, 75–197 days) were completed before January 31, 2018. There was variability in the way investigators chose the cylindrical correction to be entered as the Treatment refraction, as this decision was left up to the discretion of the investigator (Table 1).
 |
Table 1 Treatment Method Actually Used at Each Site |
Subjects were stratified on the basis of the vector difference between Manifest and Topo cylinder with a cutoff of 0.75 D, as that yielded approximately half the data points in each group. They are referred to as the High (>0.75D difference; 33 eyes) and Low (≤0.75D difference; 19 eyes) groups in subsequent analyses.
Overall Difference from “Best”
The “Best” correction is the correction that produced, or would theoretically have produced, a zero cylinder postoperative outcome. It is the vector sum of the actual Treatment cylinder entered by the surgeon into the Modified blanks on the Treatment Design screen (Figure 1) and the refractive cylinder measured 3 months postoperatively.
Calculation of Theoretical Results
The theoretical sphero-cylindrical refractive error that would have resulted if Manifest, Topo, or Phorcides cylinder had been entered as the Treatment cylinder was calculated by vector subtraction of the three theoretical cylinder entries from the Best correction. In some cases, the Treatment cylinder was the same as the Manifest or Topo cylinder. Results are presented with descriptive analysis and double-angle vector plots. Statistical significance was determined by analysis of variance (ANOVA).
Results
Table 2 shows refractive details of the eyes included in this investigation. There was no statistically significant difference between the High and Low groups with regard to any of the preoperative variables. Table 3 shows the breakdown of the difference in astigmatism magnitude and orientation between the preoperative manifest and the topography-based values. As can be seen, half the eyes (26/52) differed by less than 20 degrees in orientation and 1.0D in magnitude.
 |
Table 2 Refractive Data Summary |
 |
Table 3 Difference in Refractive and Topographic Astigmatism Angle and Magnitude |
Figure 2 shows uncorrected visual acuities at 3 months, and Figure 3 shows the change in visual acuity from the preoperative examination to 3 months postoperatively. No complications or adverse events were observed in any of the eyes included in this study.
 |
Figure 2 Cumulative uncorrected visual acuities at 3 months. |
 |
Figure 3 Change in corrected distance visual acuity from preoperative exam to the 3-month postoperative exam. |
Manifest
Figure 4 shows a double-angle plot of the calculated error vectors that would theoretically have been obtained if the Manifest cylinder had been entered as the Treatment refraction. The error vectors tend to be with the rule (centroid: −0.43, 0.11). Summary data are shown in Tables 4 and 5. The mean calculated magnitude of the error vector was 0.56 ± 0.42 D (mean ± SD; Table 4). It was significantly greater in the High group (0.70 D) compared to the Low group (0.33 D; p = 0.002). In 15% of cases (8/52), the Manifest error vector was greater than 1.0D, and all of these were in the High group (Table 5).
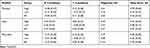 |
Table 4 Centroids and Error Magnitude for Expected or Actual Cylinder Error by Method |
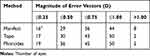 |
Table 5 Magnitude of Actual and Calculated Error Vectors by Method |
 |
Figure 4 Error vectors: difference between calculated Manifest and Best outcomes. Ellipses are the centroid ± SD for the low ( |
Topo
Figure 5 shows a double-angle plot of the calculated error vectors that would have been obtained if the Topo cylinder had been entered as the Treatment refraction. The error vectors tend to be against the rule (centroid: 0.37, 0.02). Summary data are shown in Tables 4 and 5. The mean calculated error vector was 0.47 ± 0.33 D (mean ± SD; Table 4). There was no significant difference between the magnitude in the High (0.47 D) and Low (0.48 D) groups. The magnitude of the error vector was greater than 1.0 D in 4% (2/52) of cases – one in the High group and one in the Low group (Table 5).
 |
Figure 5 Error vectors: difference between Topo and Best outcomes. Ellipses are the centroid ± SD for the low ( |
Phorcides
Figure 6 shows a double-angle plot of the calculated error vectors that would have been obtained if the cylinder derived from the Phorcides software had been entered as the Treatment refraction. The error vectors tend to be with the rule, but the deviation from the origin is minimal (centroid: −0.15, 0.06). Summary data are shown in Tables 4 and 5. The mean calculated error vector was 0.39 ± 0.28 D (mean ± SD; Table 4). The mean error vector magnitude in the Phorcides Low group was significantly lower than for the Manifest and Topo Low groups (0.26 D vs 0.48 D and 0.33 D; p < 0.01). The mean error magnitude in the Phorcides High group is nearly 0.25 D lower than for the Manifest High group (0.48 D vs 0.70 D; p< 0.01; Table 4), and the same as for the Topo High group. There were two cases of Phorcides error being greater than 1.0 D, both occurring when the vector difference between Manifest and Topo was >0.75 D (Table 5).
 |
Figure 6 Error vectors: difference between Phorcides and Best outcomes. Ellipses are the centroid ± SD for the low ( |
Discussion
Topography-guided corneal refractive surgery has historically been used as a “repair procedure” for the treatment of eyes with naturally-occurring corneal irregular astigmatism,1,12–14 complications of corneal refractive surgery,1,15-22 corneal transplants,16,18,20,23,24 and other corneal conditions.1,16,18 Topography-guided PRK has also been used for the treatment of corneal ectatic disorders in conjunction with corneal crosslinking with riboflavin and ultraviolet light25–27 and to prevent hyperopic regression following hyperopic LASIK.28 Topography-guided LASIK also produces excellent outcomes for the treatment of refractive errors in otherwise normal eyes.2,8 In one comparative study, topography-guided LASIK was found to produce lower high-order aberrations than wavefront-guided treatment.29
Requests for inclusion of eyes with naturally occurring, surgically induced, or pathological irregular astigmatism in FDA clinical trials were denied by the FDA. As a result, the FDA study does not provide prospective clinical trial outcomes for the treatment of eyes with even minimal corneal topographic abnormalities.2 In eyes such as this, which are frequently encountered in clinical practice, a disparity between astigmatism that is measured by refraction (Manifest) and that measured by topography (Topo) is more likely to occur.2 This creates a dilemma for the refractive surgeon using the WaveLight Contoura® Vision laser, because the surgeon must choose the sphero-cylindrical refraction to be entered in the treatment plan without reliable guidance from carefully conducted clinical trials.
Although some recent studies have achieved results similar to those obtained in the FDA trial,30,31 some of the authors of this report (MCL, TPL), as well as several other investigators,32–34 have been unable to obtain the excellent postoperative visual acuities obtained during the FDA trial when the same treatment protocol was applied to eyes encountered in routine clinical practice. Various alternative strategies have been proposed, therefore, to determine the appropriate laser entry for the Treatment sphero-cylindrical refraction.4,6,9,10,12
The current study was designed to address the question of how to program the WaveLight Contoura® Vision laser to produce optimal refractive outcomes for eyes in which there is a disparity between Manifest and Topo refractions. The most appropriate outcome measures for this determination would be uncorrected visual acuity and visual symptoms. Unfortunately, is it not possible to simulate the visual acuity and visual symptoms that would have been obtained if a refraction other than the one that was used to treat the patient had been applied.
One published study does examine retrospectively the planning strategy used among eyes gaining a line of best-corrected vision, but the variability and complexity of the strategy make it difficult to plan prospectively.35 We chose the actual and calculated sphero-cylindrical refractive outcome as our primary outcome measure for this analysis. Although imperfect, this provides a method to compare the actual outcome obtained with the surgeon’s selected treatment strategy and the theoretical, calculated outcome that might have been obtained with alternative methods.
Overall, the visual outcomes in the subjects we studied were excellent (Figure 2), with a tendency for increased uncorrected distance visual acuity (UCDVA; Figure 3) and no complications; however, a small, measurable residual refractive error remained in many of them. None of the 3 treatment strategies we tested would have completely eliminated postoperative refractive error for all patients. However, the results strongly suggest that the other strategies that we tested will produce outcomes that are superior to those obtained when the Manifest refraction is entered as the Treatment refraction, as was done in the FDA clinical trial. It is possible that consideration of posterior corneal and lenticular astigmatism that is inherent to Phorcides may provide an advantage of this method over alternatives, but this advantage seems to be less apparent with higher corrections, as was seen in the Topo High and Phorcides High groups.
Our results were obtained from theoretical calculations of outcomes in a small series of eyes, rather than actual results from a head-to-head comparison of laser programming strategies. Our conclusions were also based on calculated cylindrical outcomes, rather than UCDVA. A larger, prospective, multi-center clinical trial that includes UCDVA as a primary outcome variable should lead to further refinement of the appropriate strategy for determining the Treatment refraction for use with the Contoura laser for topography-guided LASIK in clinical, post-approval use for eyes routinely encountered in a commercial LASIK practice. In addition, a greater number of eyes might allow for more detailed sub-analyses, such as those necessary to determine whether the orientation of preoperative manifest or topographic astigmatism might have an effect on the optimal laser programming strategy. Finally, it is yet unknown whether correcting posterior astigmatism on the anterior cornea will lead to a longer-term compensatory effect by the epithelium affecting the clinical outcome. All of these factors must be investigated in well-designed, prospective clinical trials.
Funding
This study was conducted with funding for an investigator-initiated clinical trial from Alcon.
Disclosure
Drs Durrie, Potvin, Stonecipher, Stulting, and Krueger are consultants to Alcon. Science in Vision (Potvin) received funding for data analysis and manuscript preparation. Dr Lobanoff was the developer of the Phorcides Analytic Engine and has a financial interest in Phorcides, LLC. He is also a paid consultant for Alcon and has a patent pending on the technology behind the Phorcides software. Drs Stulting, Potvin, Krueger, and Stonecipher report grants from Alcon. Dr Daniel S Durrie helped organize the study for Alcon and is a consultant for J&J that has competitive equipment to the Alcon equipment used in the study. Dr Motwani reports grants from Alcon, Inc, outside the submitted work. In addition, Dr Motwani has a patent relating to the use of topographic guided ablation/Contoura for the creation of uniform corneas. The authors report no other conflicts of interest in this work.
References
1. Holland S, Lin DT, Tan JC. Topography-guided laser refractive surgery. Curr Opin Ophthalmol. 2013;24(4):302–309. doi:10.1097/ICU.0b013e3283622a59
2. Stulting RD, Fant BS, Group TCS, et al. Results of topography-guided laser in situ keratomileusis custom ablation treatment with a refractive excimer laser. J Cataract Refract Surg. 2016;42(1):11–18. doi:10.1016/j.jcrs.2015.08.016
3. Choi SK, Chang JW. Higher order aberration and astigmatism in children with hyperopic amblyopia. Korean J Ophthalmol. 2016;30(1):53–59. doi:10.3341/kjo.2016.30.1.53
4. Motwani M. The use of WaveLight(R) Contoura to create a uniform cornea: the LYRA protocol. Part 1: the effect of higher-order corneal aberrations on refractive astigmatism. Clin Ophthalmol. 2017;11:897–905. doi:10.2147/OPTH.S133839
5. Zhou W, Stojanovic A, Utheim TP. Assessment of refractive astigmatism and simulated therapeutic refractive surgery strategies in coma-like-aberrations-dominant corneal optics. Eye Vis (Lond). 2016;3:13. doi:10.1186/s40662-016-0044-8
6. Wallerstein A, Gauvin M, Qi SR, Bashour M, Cohen M. Primary topography-guided LASIK: treating manifest refractive astigmatism versus topography-measured anterior corneal astigmatism. J Refract Surg. 2019;35(1):15–23. doi:10.3928/1081597X-20181113-01
7. Wang Y, Zhao K, Jin Y, Niu Y, Zuo T. Changes of higher order aberration with various pupil sizes in the myopic eye. J Refract Surg. 2003;19(2 Suppl):S270–S274.
8. Tan J, Simon D, Mrochen M, Por YM. Clinical results of topography-based customized ablations for myopia and myopic astigmatism. J Refract Surg. 2012;28(11 Suppl):S829–S836. doi:10.3928/1081597X-20121005-04
9. Motwani M. The use of WaveLight(R) Contoura to create a uniform cornea: the LYRA protocol. Part 2: the consequences of treating astigmatism on an incorrect axis via excimer laser. Clin Ophthalmol. 2017;11:907–913. doi:10.2147/OPTH.S133840
10. Motwani M. The use of WaveLight(R) Contoura to create a uniform cornea: the LYRA protocol. Part 3: the results of 50 treated eyes. Clin Ophthalmol. 2017;11:915–921. doi:10.2147/OPTH.S133841
11. Motwani M, Pei R. The use of WaveLight Contoura to create a uniform cornea: 6-month results with subjective patient surveys. Clin Ophthalmol. 2018;12:1559–1566. doi:10.2147/OPTH.S175661
12. Kanellopoulos AJ. Topography-modified refraction (TMR): adjustment of treated cylinder amount and axis to the topography versus standard clinical refraction in myopic topography-guided LASIK. Clin Ophthalmol. 2016;10:2213–2221. doi:10.2147/OPTH.S122345
13. Lin DT, Holland S, Tan JC, Moloney G. Clinical results of topography-based customized ablations in highly aberrated eyes and keratoconus/ectasia with cross-linking. J Refract Surg. 2012;28(11 Suppl):S841–S848. doi:10.3928/1081597X-20121005-06
14. Pasquali T, Krueger R. Topography-guided laser refractive surgery. Curr Opin Ophthalmol. 2012;23(4):264–268. doi:10.1097/ICU.0b013e328354adf0
15. Alio JL, Belda JI, Osman AA, Shalaby AM. Topography-guided laser in situ keratomileusis (TOPOLINK) to correct irregular astigmatism after previous refractive surgery. J Refract Surg. 2003;19(5):516–527.
16. Ghoreishi M, Naderi Beni A, Naderi Beni Z. Visual outcomes of topography-guided excimer laser surgery for treatment of patients with irregular astigmatism. Lasers Med Sci. 2013.
17. Hafezi F, Mrochen M, Seiler T. Two-step procedure to enlarge small optical zones after photorefractive keratectomy for high myopia. J Cataract Refract Surg. 2005;31(12):2254–2256. doi:10.1016/j.jcrs.2005.04.026
18. Jankov MR
19. Kanellopoulos AJ. Topography-guided custom retreatments in 27 symptomatic eyes. J Refract Surg. 2005;21(5):S513–S518. doi:10.3928/1081-597X-20050901-19
20. Knorz MC, Jendritza B. Topographically-guided laser in situ keratomileusis to treat corneal irregularities. Ophthalmology. 2000;107(6):1138–1143. doi:10.1016/S0161-6420(00)00094-4
21. Lin DT, Holland SR, Rocha KM, Krueger RR. Method for optimizing topography-guided ablation of highly aberrated eyes with the ALLEGRETTO WAVE excimer laser. J Refract Surg. 2008;24(4):S439–S445. doi:10.3928/1081597X-20080401-22
22. Stojanovic A, Suput D. Strategic planning in topography-guided ablation of irregular astigmatism after laser refractive surgery. J Refract Surg. 2005;21(4):369–376. doi:10.3928/1081-597X-20050701-12
23. Cosar CB, Acar S. Topography-guided LASIK with the wavelight laser after penetrating keratoplasty. J Refract Surg. 2006;22(7):716–719. doi:10.3928/1081-597X-20060901-15
24. Mularoni A, Laffi GL, Bassein L, Tassinari G. Two-step LASIK with topography-guided ablation to correct astigmatism after penetrating keratoplasty. J Refract Surg. 2006;22(1):67–74. doi:10.3928/1081-597X-20060101-14
25. Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the athens protocol. J Refract Surg. 2011;27(5):323–331. doi:10.3928/1081597X-20101105-01
26. Kaufmann C, Bochmann F, Baenninger P, Thiel MA. Central corneal regularization–optimization of uncorrected visual acuity in keratoconus patients. Klin Monbl Augenheilkd. 2013;230(4):333–336. doi:10.1055/s-00000031
27. Krueger RR, Kanellopoulos AJ. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UVA cross-linking for progressive keratoconus: case reports. J Refract Surg. 2010;26(10):S827–S832. doi:10.3928/1081597X-20100921-11
28. Kanellopoulos AJ, Kahn J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J Refract Surg. 2012;28(11 Suppl):S837–S840. doi:10.3928/1081597X-20121005-05
29. El Awady HE, Ghanem AA, Saleh SM. Wavefront-optimized ablation versus topography-guided customized ablation in myopic LASIK: comparative study of higher order aberrations. Ophthalmic Surg Lasers Imaging. 2011;42(4):314–320. doi:10.3928/15428877-20110421-01
30. Kim J, Choi SH, Lim DH, Yang CM, Yoon GJ, Chung TY. Topography-guided versus wavefront-optimized laser in situ keratomileusis for myopia: surgical outcomes. J Cataract Refract Surg. 2019;45(7):959–965. doi:10.1016/j.jcrs.2019.01.031
31. Tiwari NN, Sachdev GS, Ramamurthy S, Dandapani R. Comparative analysis of visual outcomes and ocular aberrations following wavefront optimized and topography-guided customized femtosecond laser in situ keratomileusis for myopia and myopic astigmatism: a contralateral eye study. Indian J Ophthalmol. 2018;66(11):1558–1561. doi:10.4103/ijo.IJO_507_18
32. Faria-Correia F, Ribeiro S, Monteiro T, Lopes BT, Salomao MQ, Ambrosio R
33. Hashmani S, Hashmani N, Haroon H, Visual HY. Refractive outcomes of topography-guided laser-assisted in situ keratomileusis in virgin eyes. Cureus. 2018;10(1):e2131.
34. Shetty R, Shroff R, Deshpande K, Gowda R, Lahane S, Jayadev C. A prospective study to compare visual outcomes between wavefront-optimized and topography-guided ablation profiles in contralateral eyes with myopia. J Refract Surg. 2017;33(1):6–10. doi:10.3928/1081597X-20161006-01
35. De Stefano VS, Meister C, Ehlke GL, Krueger RR. Analysis of planning strategies in primary eyes gaining a line or more of visual acuity after topography-guided laser in situ keratomileusis. J Cataract Refract Surg. 2019;45(3):321–327. doi:10.1016/j.jcrs.2018.10.040
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.