Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 12
Topical 5 fluorouracil cream versus combined 5 flurorouracil and fractional erbium YAG laser for treatment of severe hypertrophic scars
Authors Tawfik AA , Fathy M , Badawi A , Abdallah N, Shokeir H
Received 16 October 2018
Accepted for publication 12 February 2019
Published 14 March 2019 Volume 2019:12 Pages 173—180
DOI https://doi.org/10.2147/CCID.S191137
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Abeer Attia Tawfik,1 Maha Fathy,2 Ashraf Badawi,1,3 Noha Abdallah,1 Hisham Shokeir1
1Dermatology Unit, Department of Medical Applications of Lasers (MAL), National Institute of Laser Enhanced Sciences, Cairo University, Giza, Egypt; 2Al-Houd Al Marsoud Hospital, Cairo, Egypt; 3Dermatology and Allergology Department, University of Szeged, Szeged, Hungary
Background: Topical 5 fluorouracil (5-FU) has been reported as one of the standard treatments for hypertrophic scars (HTS). Ablative fractional laser was found to have promising results in the delivery of topical drugs into the skin by creating vertical channels through which the drugs can penetrate the skin. So far there have been no comparative studies performed to compare both modalities in the same patient and same anatomical region, especially in severe HTS.
Objective: The aim of this study was to compare the effectiveness of topical 5-FU and combined topical 5-FU and laser in treating severe HTS.
Patients and methods: Twenty-four severe HTS lesions were treated by 5-FU monotherapy and 5-FU combined with ablative fractional erbium YAG laser. Each lesion was divided into two parts. One part was treated with topical 5-FU twice weekly for 8 months. The other part was treated with combined topical 5-FU and ablative fractional erbium YAG laser once per month for 8 months. The scars’ improvement was evaluated by Vancouver scar scale (VSS) and skin analysis camera.
Results: The assessment by VSS showed a significant reduction in the mean height, pliability, and vascularity of the lesions which were treated with combined approaches compared to 5-FU monotherapy. Pain and ulceration occurred at a higher rate in the combination therapy group.
Conclusion: Treatment of severe HTS with combined 5-FU and ablative fractional erbium YAG laser is more effective than 5-FU alone.
Keywords: hypertrophic scars, fractional erbium YAG laser, 5-FU, transcutaneous drug delivery, scar management, fractional lasers, skin ablation, wound healing
Introduction
Hypertrophic scar (HTS) is a common dermatological complaint caused by disruption of the normal wound healing process.1 It can occur as a result of burns, trauma, and surgical procedures or as a consequence of inflammatory skin disorders like severe acne.2 Pain, discomfort, and pruritus are common symptoms of HTS.3 Moreover, cosmetic concerns related to disfigurement and contractures may lead to psychological stress and functional disabilities that can affect the patient’s daily life.4 Accordingly, many modalities of treatment have been investigated as monotherapy or in various combinations such as surgical excision, occlusive dressings, topical and intralesional corticosteroids, interferon, cryosurgery, radiation, pressure therapy, laser therapy, retinoic acid, and silicone gel sheeting5 5 fluorouracil (5-FU) was first introduced by Fitzpatrick as a viable treatment option.6 It is a pyrimidine analog that inhibits the synthesis of deoxyribonucleic acids by irreversibly inhibiting thymidine synthase.7 Combination of 5-FU with adjuvant modalities has been explored to enhance its efficacy in treating HTS.8
On the other hand, fractional lasers produce arrays of nonselective, microscopic thermal damage zones throughout the epidermis and dermis.9 This tissue penetration leads to remodeling and production of new collagen.10 Erbium YAG produces columns with a narrower rim of thermal coagulation when compared to CO2 due to its higher affinity for absorption by water which leads to more ablation than coagulation.11 Laser-assisted drug delivery is an alternative to injection or other drug delivery methods into skin lesions.12 A previous study showed that the erbium YAG laser is safe and effective when used for ablation of the subcutaneous layers to enhance skin absorption of aminolevulinic acid,13 therefore, this study was conducted to compare the efficacy between topical 5-FU monotherapy and combined ablative fractional erbium YAG laser and 5-FU delivery in treatment of HTS.
Patients and methods
Twenty-four patients with HTS were included in this randomized, comparative study. Signed informed consent was obtained from each patient before enrollment in the study. A legal guardian provided written informed consent for any participant under the age of 18 years, including written informed consent for images to be published. The study was conducted according to the Declaration of Helsinki principles and was approved by the ethical committee of national laser institutional review board. The patients were instructed to avoid using any other modalities of treatment for HTS during the course of the study. Patients were excluded from the study if: they had been taking an oral retinoid 6 months prior to treatment, they had participated in a prior trial to treat the scar within the previous 12 months, they were pregnant and breast feeding, they had an active infection, they had lesions suspected to be malignant, they had a history of photodermatoses or skin cancer.
Treatment protocol
Each scar was divided into two parts. The allocation of treatment method was done randomly. One part was subjected to application of topical 5-FU only (Efudex 5% cream manufactured by Valeant pharmaceuticals, Laval, Canada) and the other part was subjected to combined 5-FU and ablative fractional erbium YAG laser (2,940 nm). The ablative fractional erbium YAG laser was used with a fractional hand-piece “PS01”. The spot size was 12 mm, pixel size was 450 µ, and density was 75 pixels. The short pulse mode 300 µs was used with a fluence of 3 J/cm2. Two passes were applied in two perpendicular directions, one horizontal and the other vertical (SkinPlus Erbium YAG laser, Fotona Medical Lasers, Ljubljana, Slovenia). Patients were asked to apply topical 5-FU 5% on both parts of the scar twice weekly after the laser session for 8 months.
Evaluation method
Vancouver scar scale (VSS)
VSS assesses four variables: vascularity, height/thickness, pliability, and pigmentation.14 Patient perception of his or her respective scars was not factored into the overall score.
Standardized photographs were taken at baseline, at every session, and 6 months after the end of the treatment (Kodak 14 megapixels, 4× zoom; Kodak, New York, NY, USA). A skin analysis camera system (Antera 3D; Miravex, Dublin, Ireland), which uses light emitting diodes and complex software, was used for quantitative assessment and recorded measurements in microns. The length, height, and width of the lesions were measured using digital LCD electronic 150 mm gage stainless steel vernier caliper ruler. The assessment of clinical improvement was measured regarding overall appearance, vascularity, hyperpigmentation, hypopigmentation, height, and pliability using VSS.
Statistical analysis
Data were analyzed using Statistical Program for Social Science (SPSS) version 20. Quantitative data were expressed as mean ± SD and qualitative data were expressed as frequency and percentage.
Independent samples t-test of significance was used when comparing two means. Paired samples t-test of significance was used when comparing related samples. Chi-squared test of significance was used in order to compare proportions of two qualitative parameters. Probability (P-value) <0.05 was considered significant, P-value <0.001 was considered as highly significant, and P-value >0.05 was considered insignificant.
Results
This was a randomized, intra-patient, comparative study. Twenty-four patients with severe HTS lesions participated in this study: ten females (41.7%) and 14 males (58.3%). Their ages ranged from 11–43 years with a median of 26 years. They presented with severe HTS due to various reasons (Table 1).The most common cause was post-traumatic wound (66.6%). The duration of the lesions ranged from 8 to 63 months with a mean ± SD (18.58±9.56) months. Facial lesions were most common (85.3%). Clinical examination showed that lesions which have been present for 1 year or less, were erythematous and harder than old lesions which were skin-colored and more pliable.
  | Table 1 Demographic data of patients |
All patients had skin type III and IV. Using VSS, the vascularity, pliability, pigmentation, and height were assessed in both treatment modalities. There was a significant decrease in the mean height and pliability of the parts treated with combined 5-FU and laser compared to the parts treated with 5-FU alone (P<0.001) (Table 2).
  | Table 2 Results of VSS: 5-FU vs the combined approach (laser + 5-FU) Abbreviations: VSS, Vancouver scar scale; 5-FU, 5 fluorouracil. |
Regarding the total percentage of improvement in VSS, the combination treatment showed moderate to excellent improvement in 100% of scars treated, whereas the 5-FU monotherapy revealed mild improvement in 41.67% (five patients) and moderate improvement in 58.33% (seven patients) (Table 3).
  | Table 3 Comparison between 5-FU only and laser + 5-FU regarding the total percentage of improvement Abbreviation: 5-FU, 5 fluorouracil. |
Excellent improvement was elicited in the pliability of eleven (91.7%) lesions which were treated with combined approach. Nine (75%) lesions showed moderate decrease in height when treated by 5-FU only, whereas nine (75%) lesions showed excellent improvement in height when treated by combined approach (Figures 1–4 and Table 4). On the other hand, the vascularity of the lesions increased with both therapeutic approaches. However there was a higher significant difference in the combined approach than in the 5-FU monotherapy group. Surprisingly, there was no significant difference in the pigmentation of lesions in both treatment modalities (Figures 1–4 and Table 4). The length, height, and width of the lesions were measured using digital LCD electronic 150 mm gage stainless steel vernier caliper ruler. The reduction in height was significant (Table 5) but there were no changes in length or width. The skin analysis camera system (Antera 3DTM) showed the severity of the HTS. Fine indentations and wrinkles appeared as orange and green dots and lines on the image, whereas very deep indentations and wrinkles appeared purple in color (Figure 5A, B).
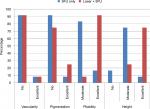  | Figure 1 Comparison between 5-FU alone and laser + 5-FU according to percentage of improvement in vascularity, pigmentation, pliability, and height. Abbreviation: 5-FU, 5 fluorouracil. |
  | Figure 2 This male patient presented with a post-traumatic scar. Note: The upper part was treated with 5-FU monotherapy and lower part with combined approach. Abbreviation: 5-FU, 5 fluorouracil. |
  | Figure 3 This male patient presented with a post-traumatic scar. Note: The upper part was treated with combined approach and lower part with 5-FU monotherapy. Abbreviation: 5-FU, 5 fluorouracil. |
  | Table 4 Comparison between 5-FU alone and laser + 5-FU according to percentage of improvement in vascularity, pigmentation, pliability, and height Abbreviation: 5-FU, 5 fluorouracil. |
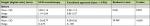  | Table 5 Height of hypertrophic scar lesions before and after treatment Abbreviation: 5-FU, 5 fluorouracil. |
The reported side effects were erythema, ulceration, and hyperpigmentation in both therapies. However, pain was reported only in parts treated by combined therapy approach. Erythema was observed more in the combined approach (75%) than in 5-FU monotherapy (50%) group with no statistically significant difference. There was no statistically significant difference in the total percentage of improvement regarding age, sex, site, skin type, and length and duration of the scar.
Similarly, ulceration was observed more in the combined approach (25%) than in 5-FU monotherapy (8.33%) group with no statistically significant difference. Finally, there was no clinical nor statistical difference in hyperpigmentation between approaches. A statistically significant difference (P-value 0.028) was associated with the combined approach regarding pain compared to 5-FU monotherapy (Table 6).
  | Table 6 Comparison between 5-FU only and laser + 5-FU regarding side effects Abbreviation: 5-FU, 5 fluorouracil. |
Discussion
This study confirmed that treatment of severe HTS using combined ablative fractional erbium YAG laser and topical 5-FU was more effective than the use of 5-FU monotherapy.
5-FU was considered as a safe option for the treatment of HTS, as it improved the appearance of proliferative scars and reduced the chance of recurrence.6,8 In this study, the use of 5-FU showed improvement in pliability, thickness, and height. Hietanen and Kaartinen compared the efficacy of intralesional triamcinolone to the efficacy of 5-FU injection in treatment of keloid scars. They revealed that both drugs are equal in clinical efficacy but the 5-FU injection led to increased proliferation rate. Moreover, the 5-FU did not affect vascular density in histological assessment.15 Shah et al suggested that 5-FU is an effective remedy for HTS and keloids if appropriately administered as a monotherapy.16
However, in this study, the combined use of fractional ablative erbium YAG laser with topical 5-FU cream showed a significantly better improvement. There are many studies which have proven the efficacy of ablative fractional erbium YAG laser as a successful method in treatment of HTS through remodeling and production of new collagen.12 Madni and Phelan revealed that burn patients who were treated with the 2,940 nm ablative fractional erbium YAG laser were highly satisfied with the improvement of their burn scars.17
Although there have been many studies which proved the efficacy of ablative fractional erbium YAG laser as a successful method in treatment of HTS, no studies have assessed the efficacy of the combined approach of the erbium YAG laser and 5-FU in severe HTS treatment. For a topical agent to be active, it must first traverse the rate-limiting outermost barrier of the skin: the stratum corneum. The second mechanism used in this study was the microchannels which were produced by the ablative fractional laser as a method of drug delivery.18,19
Fang et al agreed that the laser was the most potent technique to enhance 5-FU delivery among physical enhancement methods examined in their study on iontophoresis and electroporation.20 Prince et al compared use of intralesional and laser-assisted 5-FU in dermatology in a disease-specific systematic review, they studied 38 articles that met criteria for inclusion in their review, those articles included 14 randomized controlled trials and 24 case series. They found that the evidence was strongest for intralesional 5-FU in the treatment of keloids, HTS, and keratoacanthomas.21
In a study which was done by Marine Cavalie et al, the 2,940 nm ablative fractional erbium YAG laser was used in combination with topical betamethasone cream. The obtained results supported the interest of the laser-assisted delivery of steroids for treating keloids scars.17 So, we believe that both mechanisms augmented the effect of 5-FU in treatment of HTS. The side effects which we faced with the use of 5-FU were erythema, ulceration, and hyperpigmentation, which is why we instructed the patients to use it twice weekly. The limitation of this study was the lack of histopathological assessment. However, the authors used the Antera camera to show changes in scars as an objective, noninvasive method.
Conclusion
Fractional erbium YAG laser has been found to be an effective and safe device that enhances topical 5-FU delivery into the skin. Moreover, the effect of the fractional ablative laser will improve the effect of 5-FU on HTS.
Disclosure
The authors report no conflicts of interest in this work.
References
Reinholz M, Poetschke J, Schwaiger H, et al. The dermatology life quality index as a means to assess life quality in patients with different scar types. J Eur Acad Dermatol Venereol. 2015;29(11):2112–2119. | ||
Poetschke J, Gauglitz GG. Current options for the treatment of pathological scarring. J Dtsch Dermatol Ges. 2016;14(5):467–477. | ||
Baisch A, Riedel F. Hyperplastische Narben und Keloide Teil I: Grundlagen und Prävention [Hyperplastic scars and keloids. Part I: basics and prevention]. HNO. 2006;54(11):893–904. German | ||
Reinholz M, Schwaiger H, Heppt MV, et al. Comparison of two kinds of lasers in the treatment of acne scars. Facial Plast Surg. 2015;31(5):523–531. | ||
Bouzari N, Davis SC, Nouri K. Laser treatment of keloids and hypertrophic scars. Int J Dermatol. 2007;46(1):80–88. | ||
Fitzpatrick RE. Treatment of inflamed hypertrophic scars using intralesional 5-FU. Dermatol Surg. 1999;25(3):224–232. | ||
Badawi A. Role of lasers in facial rejuvenation. Giornale Italiano di Dermatologia e Venereologia : Organo Ufficiale, Societa Italiana di Dermatologia e Sifilografia. 2012;147(3):285–293. | ||
Wu X-L, Liu W, Cao Y-L. [Clinical study on keloid treatment with intralesional injection of low concentration 5-fluorouracil]. Zhonghua Zheng Xing Wai Ke Za Zhi. 2006;22(1):44–46. Chinese. | ||
Uebelhoer NS, Ross EV, Shumaker PR. Ablative fractional resurfacing for the treatment of traumatic scars and contractures. Semin Cutan Med Surg. 2012;31(2):110–120. | ||
Carniol PJ, Hamilton MM, Carniol ET. Current status of fractional laser resurfacing. JAMA Facial Plast Surg. 2015;17(5):360–366. | ||
Metelitsa AI, Alster TS. Fractionated laser skin resurfacing treatment complications: a review. Dermatol Surg. 2010;36(3):299–306. | ||
Sklar LR, Burnett CT, Waibel JS, Moy RL, Ozog DM. Laser assisted drug delivery: a review of an evolving technology. Lasers Surg Med. 2014;46(4):249–262. | ||
Fang JY, Lee WR, Shen SC, Fang Y-P, Hu C-H. Enhancement of topical 5-aminolaevulinic acid delivery by erbium:YAG laser and microdermabrasion: a comparison with iontophoresis and electroporation. Br J Dermatol. 2004;151(1):132–140. | ||
Baryza MJ, Baryza GA, Mary Jo MS, Baryza PT, Gregory A. The Vancouver scar scale: an administration tool and its interrater reliability. J Burn Care Rehabil. 1995;16(5):535–538. | ||
Hietanen KE, Järvinen TA, Huhtala H, Tolonen TT, Kuokkanen HO, Kaartinen IS. Treatment of keloid scars with intralesional triamcinolone and 5-fluorouracil injections – a randomized controlled trial. J Plast Reconstr Aesthet Surg. 2019;72(1):4–11. | ||
Shah VV, Aldahan AS, Mlacker S, et al. 5-fluorouracil in the treatment of keloids and hypertrophic scars: a comprehensive review of the literature. Dermatol Ther. 2016;6(2):169–183. | ||
Cavalié M, Sillard L, Montaudié H, et al. Treatment of keloids with laser-assisted topical steroid delivery: a retrospective study of 23 cases. Dermatol Ther. 2015;28(2):74–78. | ||
Madni TD, Nakonezny PA, Imran JB, Phelan H. Patient satisfaction after fractional ablation of burn scar with 2940 nm wavelength Erbium-Yag laser. Burns. 2018;44(5):1100–1105. | ||
Badawi AM, Osman MA. Fractional erbium-doped yttrium aluminum garnet laser-assisted drug delivery of hydroquinone in the treatment of melasma. Clin Cosmet Investig Dermatol. 2018;11:13–20. | ||
Fang J-Y, Hung C-F, Fang Y-P, Chan T-F. Transdermal iontophoresis of 5-fluorouracil combined with electroporation and laser treatment. Int J Pharm. 2004;270(1–2):241–249. | ||
Prince GT, Cameron MC, Fathi R, Alkousakis T. Intralesional and laser-assisted 5-fluorouracil in dermatologic disease: a systematic review. J Drugs Dermatol. 2018;17(3):274–280. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


