Back to Journals » Patient Preference and Adherence » Volume 10
Time to lack of persistence with pharmacological treatment among patients with current depressive episodes: a natural study with 1-year follow-up
Authors Li K, Wei Q, Li G, He X, Liao Y, Gan Z
Received 9 April 2016
Accepted for publication 11 August 2016
Published 31 October 2016 Volume 2016:10 Pages 2209—2215
DOI https://doi.org/10.2147/PPA.S109941
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Kanglai Li,1,* Qinling Wei,2,* Guanying Li,2 Xiangjun He,2 Yingtao Liao,2 Zhaoyu Gan2
1Very Important Patient Department, 2Department of Psychiatry, The Third Affiliated Hospital of Sun Yat-sen University, Tianhe District, Guangzhou, Guangdong, People’s Republic of China
*These authors contributed equally to this work
Introduction: Medication nonadherence remains a big challenge for depressive patients. This study aims to assess and compare the medication persistence between unipolar depression (UD) and bipolar depression (BD).
Methods: A total of 146 UD and 187 BD patients were recruited at their first index prescription. Time to lack of persistence with pharmacological treatment (defined as a gap of at least 60 days without taking any medication) was calculated, and clinical characteristics were collected. Final diagnosis was made at the end of 1-year follow-up.
Results: A total of 101 (69.2%) UD and 126 (67.4%) BD patients discontinued the treatment, with a median duration of 36 days and 27 days, respectively. No significant difference was found between UD and BD in terms of time to lack of persistence with pharmacological treatment. The highest discontinuation rate (>40%) occurred in the first 3 months for both groups of patients. For UD patients, those with a higher risk of suicide (odds ratio [OR] =0.696, P=0.035) or comorbidity of any anxiety disorder (OR =0.159, P<0.001) were less likely to prematurely drop out (drop out within the first 3 months), while those with onset in the summer (OR =4.702, P=0.049) or autumn (OR =7.690, P=0.012) were more likely to prematurely drop out than those with onset in the spring (OR =0.159, P<0.001). For BD patients, being female (OR =2.250, P=0.012) and having a history of spontaneous remission or switch to hypomania (OR =2.470, P=0.004) were risk factors for premature drop out, while hospitalization (OR =0.304, P=0.023) and misdiagnosis as UD (OR =0.283, P<0.001) at the first index prescription were protective factors.
Limitation: Conservative definition of nonadherence, low representativeness of sample.
Conclusion: Treatment discontinuation was frequently seen in patients with UD or BD, especially in the first 3 months of treatment. In spite of the similar pattern of medication persistence, UD and BD differ from each other in predictors of premature drop out.
Keywords: medication adherence, unipolar depression, bipolar depression
Introduction
Major depressive episode (MDE) is a very common and severe condition shared by unipolar depression (UD) and bipolar depression (BD) and is also the major reason for patients with BD to seek medical help. The chronicity and repeatability of its course make long-term treatment imperative. According to the current Practice Guideline for the Treatment of Patients with Major Depressive Disorder1 and the recent CANMAT guidelines for the management of patients with bipolar disorder,2 the routine treatment duration for new onset of UD or BD is up to 1 year. However, the epidemiology of persistence with pharmacological treatment in patients with UD or BD shows that rates of persistence run as low as 20%–30% over treatment periods ranging from 6 months to several years,3–6 meaning that more than half of the patients with UD or BD do not get adequate pharmacological treatment as the guidelines recommend.
Adherence has recently been suggested to be divided into these two components: persistence and compliance.7 Persistence is defined as continuously refilling prescriptions in accordance with the suggested duration of the therapy; it conceptualizes adherence as an “all or none” phenomenon.7 Compliance is the extent to which medication is taken in accordance with prescribed dosage and schedule. Adherence is understood as a behavioral continuum such that patients can be “partially” adherent. Recently, many studies have focused on adherence and compliance, while persistence has received less attention. In limited persistence studies,8 persistence was defined as the total number of days from the initiation of treatment to therapy modification (ie, discontinuation, switching, or combination with another pharmacological treatment), with a focus on comparing persistence with different medicines. However, persistence with any pharmacological treatment has rarely been investigated. From a clinical point of view, persistence with any pharmacological treatment partly reflects the continuity of care, which is regarded as a basic quality requirement, essential for following patients in their own context of life for a long time.3,9,10 In addition, the majority of studies were carried out in developed countries or regions using pharmacy records to track and follow up large cohorts of individuals. However, few attempts have been made to link the clinical characteristics of illness with the persistence of pharmacological treatment, since in these retrospective studies, much information about the clinical characteristics was unavailable and it was even difficult to confirm the diagnosis.4,11
In spite of the similarity in depressive symptoms, UD and BD differ greatly in age at onset,12 comorbidity,13 response to antidepressant treatment,14 and so on. Therefore, we hypothesized that the pattern of pharmacological treatment persistence might differ between UD and BD patients. In this study, we monitored the persistence of pharmacological treatment among patients with current depressive episodes from their first received medical prescription for 1 year, aiming to find out and compare the pattern of pharmacological treatment persistence between UD and BD.
Methods
Subjects
This study sample partly came from our previous study.15 Potential participants for this study were found and recommended by their first visiting psychiatrists. The cases were included if they met the following criteria: 1) fitted the diagnostic criteria of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) for MDE; 2) got their first medical prescription for MDE in the psychiatric department of The Third Affiliated Hospital of Sun Yat-sen University between January 2007 and December 2010; 3) aged between 16 years and 65 years; 4) were capable of understanding and completing the related questionnaire survey; and 5) submitted written informed consent. Patients with a psychiatric or physical disorder that prevented them from being interviewed or undermined their ability to provide accurate information and those who declined participation in the study or refused to provide informed consent were excluded. In addition, patients with history of pharmacological treatment for any listed mental disorders were also excluded. Totally, 352 potential patients were screened and 333 (94.6%) were eligible to be included in this study. Among the 19 (5.4%) excluded candidate subjects, three refused to submit written informed consent, two were not able to understand and complete the questionnaire survey because of illiteracy, and the rest had a history of pharmacological treatment for any DSM-IV-TR-listed mental disorder. All procedures used in the present study were reviewed and approved by the Clinical Research Ethics Committee of the Third Affiliated Hospital of Sun Yat-Sen University.
Assessment of persistence with pharmacological treatment
Time to lack of persistence with pharmacological treatment was the outcome measure employed in this study, which was defined as a gap of at least 60 days without taking any medication. The definition of lack of persistence here was different from that reported in the literature,3,6 which was defined as a gap of at least 30 days between subsequent medication fill. Because in clinical practice, if a patient fails to show up for ≥1 month after her/his scheduled appointment, there might be the possibility that the patient reduces the daily dose of the prescribed medication by half or even more on her/his own decision or refills the medication in other medical institutions. Under such circumstances, the patient continues the pharmacological treatment instead of abandoning it completely. Obviously, this condition should not be considered as the lack of persistence with pharmacological treatment. In addition, we enlarged the gap of treatment discontinuation from at least 30 days to at least 60 days out of the following consideration: first, a gap of 60 days can be more easily recognized than a gap of 30 days; second, DSM-IV-TR defined remission of UD or BD as absence of symptoms lasting at least 2 months, indicating that patients who come back for treatment after a gap of <2 months are less likely to stop the treatment because of remission. In this sense, treatment discontinuation lasting at least 60 days has more clinical implication.
Procedure
At the study entry, the Chinese version of the Structured Clinical Interview for the DSM-IV-TR Axis 1 Disorders (SCID-I) was performed for each participant to establish an initial diagnosis meeting the criteria of DSM-IV-TR. Sociodemographic and clinical characteristics (detailed information in Table 1) were collected using the self-compiled questionnaire. Each subject was followed up from the index prescription until the date of the earliest of the following events: lack of persistence with pharmacological treatment, emigration, death, and end of follow-up (1 year after the index prescription). The assessment of persistence with pharmacological treatment was based on the outpatient medical files, which were kept in our outpatient department, electronic records of prescription, and the patients’ self-report about whether and when they stopped the prescribed medication. If a patient did not show up for ≥2 months after the scheduled appointment, an interview was arranged with the study team members on the subsequent visit or by the end of 1-year follow-up via the telephone to ask when the pharmacological treatment was stopped. Time to lack of persistence with pharmacological treatment was calculated from the date of the first prescription to the date when pharmacological treatment was actually discontinued. During the period of follow-up, if a suspected switch was detected, the patients’ relatives or friends were asked to provide additional information. At the end of the study, a committee, consisting of three psychiatrists, reviewed all the data collected in the whole period of follow-up and came up with a final diagnosis according to the criteria of DSM-IV-TR about UD and BD. Differential diagnosis between UD and BD was not made until 1 year after entry into this study. This is because some cases have not yet experienced manic episodes, although they are bipolar disorder sufferers.16 As far as we know, no similar study has been conducted, especially in the People’s Republic of China.
During the study period, all treatment decisions or changes in treatment medications such as dose reduction, dose augmentation, switch, and discontinuation strategies were made by their treating psychiatrists and the participants. This study was carried out under naturalistic clinical settings.
Statistical analysis
The proportion of patients who discontinued pharmacological treatment was calculated for the two diagnostic cohorts at 0–90 days, 90–180 days, 180–270 days, and 270–360 days after the start of the treatment. Kaplan–Meier survival curves were used to examine time to lack of persistence with pharmacological treatment. Subjects were censored if the follow-up was terminated. In order to explore potential predictors of pharmacological treatment discontinuation, two Cox regression models, one for each diagnostic cohort, were fitted, and adjusted hazard ratios (HRs) with 95% CIs were estimated according to the level of exposure variables. The results were considered significant at P<0.05. Data management and statistical analysis were carried out using commercial statistical package SPSS 19.0 (IBM Corporation, Armonk, NY, USA), and the PHREG procedure was used to fit the Cox regression model.
Results
A total of 333 patients were enrolled in this study, with 146 receiving a diagnosis of UD and 187 receiving a diagnosis of BD at the end of this study. Compared to patients with UD, patients with BD had similar sex distribution, but were younger (26.8±9.2 years vs 37.2±12.8 years, P<0.01) and had an earlier illness onset (24.7±9.4 years vs 35.8±13.4 years, P<0.01). Of the BD population, 87 (46.5%) patients were misdiagnosed as UD at the entry of this study, while 16 (11.0%) patients with UD were treated as BD at the initiation of treatment (Table 1).
During the follow-up, 101 (69.2%) patients with UD and 126 patients (67.4%) with BD discontinued the treatment, with a median duration of 36 days (95% CI: 108–252) and 27 days (95% CI: 66–174), respectively. Figure 1 represents the Kaplan–Meier survival curves, showing similar discontinuation rate between UD and BD, which was further justified by log-rank test (P=0.945). Table 2 displays the discontinuation rate at each 3-month during the follow-up, which shows that the highest discontinuation rate occurred in the first 3 months, reaching >40%.
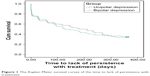  | Figure 1 The Kaplan–Meier survival curves of the time to lack of persistence with treatment. |
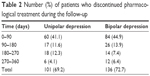  | Table 2 Number (%) of patients who discontinued pharmacological treatment during the follow-up |
In order to explore the potential risk of lack of persistence, Cox regression was conducted with time to lack of persistence as dependent variable and the clinical characteristics listed in Table 1 as independent variables, respectively, within each group. In individuals with UD, comorbidity of anxiety disorders was found to be a protective factor against treatment discontinuation (HR 0.503, 95% CI 0.299–0.848, P=0.010), other clinical variables did not impose significant impact on the time to lack of persistence. In patients with BD, hospitalization after the first visit was the only factor that was significantly associated with the time to lack of persistence (HR 0.529, 95% CI 0.284–0.988, P=0.046).
Given that >40% of patients discontinued treatment within the first 3 months after the treatment initiation, which was called here as “premature drop out”, binary logistic regression was done with premature drop out as dependent variable and the clinical characteristics listed in Table 1 as independent variables, the results are displayed in Table 3.
Table 3 shows a completely different predictive pattern of premature drop out between UD and BD: for patients with UD, higher risk of suicide and comorbidity of anxiety disorders served as protective factors against premature drop out, while onset at summer or autumn imposed higher risk of premature drop out than onset at spring; for individuals with BD, female or those with history of spontaneous remission or switch to hypomania were more likely to prematurely drop out, while those hospitalized after the first visit or misdiagnosed had lower possibility of premature drop out.
Discussion
As demonstrated previously,17–21 medication nonadherence among patients with mood disorder imposes a big challenge on clinical practice, but the rate of medication nonadherence varies with its definition and measurement. In the present study, we employed a definition of nonadherence that was different from and more conservative than that employed by most previous studies, where persistence with an initial medicine had typically been used.6,22,23 We assessed persistence with any pharmacological treatment, so that, switching from antidepressants to mood stabilizers was not considered as discontinuation when a depressive patient’s diagnosis was modified from UD to BD.
With this definition, >60% depressive patients who received pharmacological treatment for the first time discontinued treatment within the following 1 year. Similar discontinuation rates were found in a previous study,3 but in this study, >40% patients discontinued pharmacological treatment within the first 3 months. Possible explanation for such a high discontinuation rate might be that all the subjects enrolled in this study sought medical help for the first time in their lives when they knew little about the disease and the medication they received. Under such circumstances, they might be more vulnerable to premature drop out since an individual’s perception of the illness and medication has been proved to impact medication adherence.24,25 Such high discontinuation rates were also found in similar circumstances in a community survey.26 However, studies starting from the stage when treatment was relatively stable usually reported high medication adherence.27,28 This suggests that medication adherence might vary with the treatment stages.
Contrary to our expectation, our study did not find any significant difference in pattern of persistence with pharmacological treatment between UD and BD. Considering the conservative definition of persistence with pharmacological treatment, the pattern of persistence with pharmacological treatment reflects a pattern of medical help-seeking behavior for patients who need long-term treatment rather than the pattern of pharmacological treatment itself. In this sense, our conclusion is consistent with previous findings.3 However, we find that the predictors of early discontinuation completely differ between patients with UD and those with BD, meaning that although the pattern of medical help-seeking behavior is similar between patients with UD and those with BD, factors that affect or dominate such behavior differ between UD and BD. To our knowledge, this has not been reported earlier.
Just as this study and previous reports indicated, misdiagnosis is a big challenge for patients with BD. Unfortunately, no study in medication adherence has ever addressed such an issue. We found that misdiagnosis acts as a protective factor against early pharmacological treatment discontinuation for patients with BD, implying that antidepressant treatment helps improve treatment adherence among patients with BD. This finding is partly in line with the conclusion from a meta-analysis29 that antidepressants usage is not associated with an increased risk of discontinuation for patients with BD. Considering the controversial effect of antidepressant on BD patients,30–32 it is hard to judge whether patients with BD benefit from the use of antidepressants.
Limitations of this study
Several factors should be considered when interpreting this study’s results. First, only treatment interrupted for at least 60 days was investigated. In clinical practice, the pattern of treatment persistence is far more complicated than the definition of persistence with pharmacological treatment employed in this study. In other words, we cannot infer the pattern of treatment discontinuation ranging from 1 day to 59 days among patients with a current depressive episode. Second, for patients with bipolar disorder, only patients with current depressive episodes were investigated; therefore, our conclusion might not be generalized to patients with current manic or hypomanic episodes. Finally, patients enrolled in this study all came from the Psychiatric Department of The Third Affiliated Hospital of Sun Yat-sen University, which differs from other mental health institutions in terms of treatment provision and academic reputation. Though we do not know what these differences mean for treatment persistence, we caution against generalizing conclusions to depressive patients seeking medical treatment in other mental health institutions.
Conclusion
Treatment discontinuation was frequently seen in patients with UD or BD, especially in the first 3 months of treatment. In spite of the similar pattern of medication persistence, UD and BD differ from each other in predictors of premature drop out.
Acknowledgments
Funding for this study was provided by Natural Science Foundation of Guangdong Province (101510089010000214), Guangdong Department of Science & Technology Translational Medicine Center grant (2011A080300002), and Science and Technology Program of Guangzhou (201609010086). The Natural Science Foundation of Guangdong Province, Guangdong Department of Science & Technology Translational Medicine Center grant and Science and Technology Program of Guangzhou had no further role in study design, in the collection, analysis and interpretation of data, in the writing of the report, and in the decision to submit the paper for publication. The authors would like to gratefully acknowledge the contributions of Professor Jonathan Flint in editing this paper and the efforts of all of the nurses, technicians, and patients that participated in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Hyler SE. APA online CME practice guideline for the treatment of patients with major depressive disorder. J Psychiatr Pract. 2002;8(5):315–319. | ||
Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2013. Bipolar Disord. 2013;15(1):1–44. | ||
Conti V, Lora A, Cipriani A, Fortino I, Merlino L, Barbui C. Persistence with pharmacological treatment in the specialist mental healthcare of patients with severe mental disorders. Eur J Clin Pharmacol. 2012;68(12):1647–1655. | ||
Tanno S, Ohhira M, Tsuchiya Y, Takeuchi T, Tanno S, Okumura T. Frequent early discontinuation of SSRI prescribed by primary care physicians in young males in Japan. Intern Med. 2009;48(15):1263–1266. | ||
Shigemura J, Ogawa T, Yoshino A, Sato Y, Nomura S. Predictors of antidepressant adherence: results of a Japanese Internet-based survey. Psychiatry Clin Neurosci. 2010;64(2):179–186. | ||
Sawada N, Uchida H, Suzuki T, et al. Persistence and compliance to antidepressant treatment in patients with depression: a chart review. BMC Psychiatry. 2009;9:38. | ||
Cooper D, Moisan J, Gregoire JP. Adherence to atypical antipsychotic treatment among newly treated patients: a population-based study in schizophrenia. J Clin Psychiatry. 2007;68(6):818–825. | ||
Hassan M, Madhavan SS, Kalsekar ID, et al. Comparing adherence to and persistence with antipsychotic therapy among patients with bipolar disorder. Ann Pharmacother. 2007;41(11):1812–1818. | ||
Percudani M, Belloni G, Contini A, Barbui C. Monitoring community psychiatric services in Italy: differences between patients who leave care and those who stay in treatment. Br J Psychiatry. 2002;180:254–259. | ||
Sytema S, Micciolo R, Tansella M. Continuity of care for patients with schizophrenia and related disorders: a comparative south-Verona and Groningen case-register study. Psychol Med. 1997;27(6):1355–1362. | ||
Aikens JE, Kroenke K, Swindle RW, Eckert GJ. Nine-month predictors and outcomes of SSRI antidepressant continuation in primary care. Gen Hosp Psychiatry. 2005;27(4):229–236. | ||
Gan Z, Diao F, Wei Q, et al. A predictive model for diagnosing bipolar disorder based on the clinical characteristics of major depressive episodes in Chinese population. J Affect Disord. 2011;134(1–3):119–125. | ||
Goldberg JF, Perlis RH, Bowden CL, et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2009;166(2):173–181. | ||
O’Donovan C, Garnham JS, Hajek T, Alda M. Antidepressant monotherapy in pre-bipolar depression; predictive value and inherent risk. J Affect Disord. 2008;107(1–3):293–298. | ||
Gan Z, Diao F, Wei Q, et al. A predictive model for diagnosing bipolar disorder based on the clinical characteristics of major depressive episodes in Chinese population. J Affect Disord. 2011;134(1–3):119–125. | ||
Perlis RH, Miyahara S, Marangell LB, et al. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry. 2004;55(9):875–881. | ||
Lingam R, Scott J. Treatment non-adherence in affective disorders. Acta Psychiatr Scand. 2002;105(3):164–172. | ||
Burra TA, Chen E, McIntyre RS, Grace SL, Blackmore ER, Stewart DE. Predictors of self-reported antidepressant adherence. Behav Med. 2007;32(4):127–134. | ||
Lang K, Korn J, Muser E, Choi JC, Abouzaid S, Menzin J. Predictors of medication nonadherence and hospitalization in Medicaid patients with bipolar I disorder given long-acting or oral antipsychotics. J Med Econ. 2011;14(2):217–226. | ||
Narasimhan M, Hardeman SM, Johnson AM. Nonadherence in mood disorders: a formidable challenge in clinical practice. Asian J Psychiatr. 2011;4(1):22–25. | ||
Roca M, Armengol S, Salvador-Carulla L, Monzon S, Salva J, Gili M. Adherence to medication in depressive patients. J Clin Psychopharmacol. 2011;31(4):541–543. | ||
Gjerden P, Slordal L, Bramness JG. Prescription persistence and safety of antipsychotic medication: a national registry-based 3-year follow-up. Eur J Clin Pharmacol. 2010;66(9):911–917. | ||
Vlahiotis A, Devine ST, Eichholz J, Kautzner A. Discontinuation rates and health care costs in adult patients starting generic versus brand SSRI or SNRI antidepressants in commercial health plans. J Manag Care Pharm. 2011;17(2):123–132. | ||
Woolley SB, Fredman L, Goethe JW, Lincoln AK, Heeren T. Hospital patients’ perceptions during treatment and early discontinuation of serotonin selective reuptake inhibitor antidepressants. J Clin Psychopharmacol. 2010;30(6):716–719. | ||
Clatworthy J, Bowskill R, Rank T, Parham R, Horne R. Adherence to medication in bipolar disorder: a qualitative study exploring the role of patients’ beliefs about the condition and its treatment. Bipolar Disord. 2007;9(6):656–664. | ||
Olfson M, Marcus SC, Tedeschi M, Wan GJ. Continuity of antidepressant treatment for adults with depression in the United States. Am J Psychiatry. 2006;163(1):101–108. | ||
Muzina DJ, Malone DA, Bhandari I, Lulic R, Baudisch R, Keene M. Rate of non-adherence prior to upward dose titration in previously stable antidepressant users. J Affect Disord. 2011;130(1–2):46–52. | ||
Sajatovic M, Valenstein M, Blow F, Ganoczy D, Ignacio R. Treatment adherence with lithium and anticonvulsant medications among patients with bipolar disorder. Psychiatr Serv. 2007;58(6):855–863. | ||
Zhang Y, Yang H, Yang S, et al. Antidepressants for bipolar disorder: a meta-analysis of randomized, double-blind, controlled trials. Neural Regen Res. 2013;8(31):2962–2974. | ||
Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711–1722. | ||
Brunoni AR. Ceiling effects in the “effectiveness of adjunctive antidepressant treatment for bipolar depression” study: was the sky the limit? Rev Bras Psiquiatr. 2011;33(1):102–103. | ||
Amsterdam JD, Wang CH, Shwarz M, Shults J. Venlafaxine versus lithium monotherapy of rapid and non-rapid cycling patients with bipolar II major depressive episode: a randomized, parallel group, open-label trial. J Affect Disord. 2009;112(1–3):219–230. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


