Back to Journals » Infection and Drug Resistance » Volume 15
Time-to-Disability Determinants Among Leprosy Patients Enrolled for Treatment at ALERT Center, Addis Ababa, Ethiopia: A Survival Analysis
Authors Masresha BM , Biresaw HB , Moyehodie YA , Mulugeta SS
Received 25 February 2022
Accepted for publication 17 May 2022
Published 30 May 2022 Volume 2022:15 Pages 2729—2741
DOI https://doi.org/10.2147/IDR.S361799
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Bezanesh Melese Masresha,1,2 Hailegebrael Birhan Biresaw,1 Yikeber Abebaw Moyehodie,1 Solomon Sisay Mulugeta1
1Department of Statistics, Debre Tabor University, Debre Tabor, Amhara, Ethiopia; 2Department of Statistics, University of Gondar, Gondar, Amhara, Ethiopia
Correspondence: Bezanesh Melese Masresha, Department of Statistics, Debre Tabor University, Debre Tabor, Amhara, Ethiopia, Email [email protected]
Background: Mycobacterium leprae causes leprosy, which is a long-term or recurrent infection. The causative agent’s collusion with Schwann cells results in the irreversible loss of fringe nerve tissue; followed by incapacity, which includes not just actual impotence but also mental incapacity, creates a bad image of the transformed, resulting in segregation and societal humiliation of leprosy patients, as well as their families.
Methods: This study’s survival analysis includes a sample of 205 patients who were taking leprosy medication and had all essential data from January 2015 to December 2019 G.C. at the All African TB and Leprosy Rehabilitation and Training Centre. The Cox proportional hazard model was used to figure out what factors influence leprosy patients’ survival status during treatment.
Results: Among the 205 leprosy patients, 71 (34.63%) had at least one type of impairment grade during treatment. The Cox proportional model revealed that the most significant variables of impairment among leprosy patients were age, symptom duration, treatment category, living place, and sensory loss.
Conclusion: The study investigated and revealed characteristics associated with the survival status of leprosy patients in ALRT centers using survival analysis. Patients’ risk of worsening disability grade increased with age, was greater for patients with a long duration of symptom, was higher for defaulter patients, and was lower for patients who did not lose their sensibility throughout therapy. The existence of a difference in the survival curves between two or more groups of factors for the patient’s survival function was also discovered in this inquiry. Female patients, particularly those who were new to the medication, were shown to be more in their survival.
Keywords: disability, survival analysis, Cox proportional model
Introduction
Mycobacterium leprae causes leprosy, a chronic infectious disease. Because a big section of the population is naturally resistant to the disease, its morbidity is low. The skin and peripheral nerves are primarily affected by leprosy. The patient’s skin and neurologic examinations are used to make the diagnosis.1 Because infection can occur at any time based on opportunities and levels of exposure, leprosy is not a disease that is age or gender specific. Leprosy is more common among people who live in poor living conditions and eat poorly.2
Issues such as decreased capacity to work, a limited social life, and psychological issues, as well as stigma and discrimination can be caused toward people who have disability related with the disease.3,4 As a result, it is important to keep track of the prevalence of leprosy-related disability and assess the risk factors.
For marginalized and economically and socially poor populations, a better knowledge of the causes of disability and approaches to enhance disease care is essential. Another priority is minimizing the impact of living with leprosy-related impairments, which necessitates research into disability prevention and treatment, as well as the efficacy, accessibility, and effectiveness of rehabilitation services, assistive devices, and community-based rehabilitation programs.5 To comprehend and quantify the need and allocate resources, better estimates of the number of persons disabled by leprosy (and their needs) and estimates of the burden of leprosy disability are required.6
Leprosy instances with Grade 2 disabilities at finding (G2D) that had been accounted for worldwide by 2019 were 10,813 cases, and the extent of G2D cases was 5.3% among new cases, relating to 1.2 per million populace.7 In the drawn out vision of the arrangement, ”Towards Zero Leprosy” signifies ”zero contamination and illness, zero handicap, zero stigma and discrimination.” The medium-term objective is to remove leprosy, which is characterized as the interference of transmission of the infection, and a WHO working gathering has been refining definitions around here lately. This goal is unlikely to be met globally by 2030.
According to the Ethiopian leprosy mapping report (2015), leprosy is the top cause of delayed actual inability and causes genuine social disgrace among infectious illnesses. Ethiopia was considered a high-leprosy endemic country, announcing in excess of 1000 cases yearly. The rate of new leprosy cases with disability Grade II (visual impairment and deformities such as wounds, ulcers, foot drop, or claw hand) and pediatric leprosy remains high. All of those indicate the ongoing transmission of leprosy in the community. The relapse rate in the country showed significant increase. It also presented the existence of a considerable proportion of patients who are diagnosed and treated at an advanced stage of the disease and a significant number of patients had received inappropriate health care services. The research also well mentioned that the country would not be able to achieve disability reduction target in the near future, unless special disability prevention intervention is in place.2
The study by Shumet et al,8 “Prevalence of Disability and Associated Factors Among Registered Leprosy Patients in all Africa TB and Leprosy Rehabilitation and Training Center,” disability is quite common, with more than half of the patients presenting with one type of impairment. This high commonness of inability demonstrates the presence of issues as far as early case finding and treatment. On the off chance that patients had a chance of being discovered early, they might have been relieved from the illness before any of the entanglements showed up. The majority of the patients are from outside Addis Ababa, according to the report,8 which suggests that this might be due to misdiagnosis of patients at outlying health facilities, or patients might not have any information to look for medical services at the beginning phase; when they foster disability they generally really like to go a long way from their home to look for clinical assistance as they would rather not be perceived in their communities on account of the disgrace related with the disease.
This study aimed to find out how leprosy patients perform in the curing after they have started treatment by looking up their survival status whether they have cured or they have developed any kind of disability worsening from the disease. In addition, this study provides information about factors leading them to develop disability at any time in treatment follow-up using a survival analysis. This allows an opportunity for recovery workers, social specialists, clinicians, organizers, and strategy creators in taking proof based choices and decisions, which are fundamental to work on the nature of care, psychosocial backing, and treatment of the people impacted by sickness with leprosy and their families additionally helps in mindfulness improvement about the infection and its prescription.
Materials and Methods
Study Design and Area
The data for this investigation were gathered from the All African TB and Leprosy Rehabilitation and Training Centre (ALERT) in Addis Ababa, Ethiopia, using a retrospective cohort study approach.
Study Period and Source of Data
We employed secondary data sources in this investigation. All medical data of registered patients with leprosy cases of zero and one disability grade admitted for treatment to the ALERT Centre in Addis Ababa, Ethiopia, were evaluated retrospectively from January 2015 to December 2019 G.C.
Study Variable
Response Variable
The dependent variable was survival time of patients with leprosy from the date of enrollment for the treatment care until the occurrence of some worsening disability grade and the response time was the time at which the patient experiences a new disability upgrading, but the disability grade experienced by the leprosy patient can be either G1D or G2D as worsening. At the beginning of treatment, patients may have G0D, G1D or G2D, but we considered that the worse disability grade occurred during treatment taking as an event only for patients who first start the treatment with G0D and G1D. There is no more disability worsening during treatment for leprosy patients who already develop G2D because they already have experienced the final disability grade before starting the medication.
Independent Variables
Sex (female, male), living place of patients (Addis Ababa, out of Addis Ababa), patient category (relapse, default, new), leprosy type (MB, PB), body part where the first lesion appears (hands, feet, on both hands and feet, face), lesion type (macules, plagues, nodules, macnod), degree of sensory loss (marked, moderate, absent), lesion distribution (symmetric, part symmetric, asymmetric), thickness of nerve (yes, no), history for the disease (have no any contact, contact, family), smear result (zero, positive, negative), age and duration of the disease before starting the treatment.
Data Processing and Analysis
We employed descriptive and inferential statistical analyses. Non-parametric survival analysis approaches define survival in terms of the component under consideration, but they must overlook the influence of any other factors. When studying survival in relation to a single component, it is common to want to account for the effects of others. Furthermore, while the log rank test provides a P-value for group differences, it does not provide an estimate of the true effect size.
The use of a statistical model improves on existing approaches by allowing survival to be evaluated in relation to several factors at the same time, as well as providing estimates of the intensity of impact for each covariate. As a result, the Cox proportional hazards model is used in this work to provide useful insight into the survival process.
Data management has been done by STATA version 16 and R version 3.6.3 statistical software. SPSS version 23.0 has been used for data entering. Statistical decision was made at the 5% level of significance.
Inclusion and Exclusion Criteria
This study includes leprosy patients who started the medication with disability grade G0D or G1D registered for treatment with MDT at any time from January 2015 up to December 2019 at ALERT Center. All patients with incomplete data, and those who were transferred to other locations during treatment were excluded. Since G2D is the final disability grade, patients with this category will never experience the event of the study that was a new occurrence of some disability grade (G1D or G2D) for the patient during treatment and therefore those leprosy patients with a history of grade II disability (G2D) before starting the treatment during the study period were excluded. Thus, by considering such reasons and availability of the required data in the hospital, in this study, the appropriate sample size was taken as all patients based on the eligibility criteria.
The patients were sorted as having Grade 0, Grade I and Grade II disability according to the WHO inability reviewing framework. A patient showing no tangible or engine nerve work debilitation or loss of vision because of disease was considered as having Grade 0 disability. Grade II disability was determined at whatever point a patient introduced to have tactile nerve work disability influencing hands or feet without engine nerve work hindrance influencing these locales (because of infection) or visual debilitation better than 6/60 because of leprosy. Grade II disability was analyzed when there was engine nerve work weakness or apparent deformation of hands or feet or visual disability <6/60 because of the disease.
Ethical Considerations
The data used in the current investigation were collected previously by the health staff for treatment purpose/for diagnosis leprosy and to start follow-up treatment. To use this previously collected data, an ethical approval certificate has been obtained from the ethical clearance review committee of the College of Natural and Computational Science, University of Gondar, Ethiopia, with reference number: CNCS/10627/05/19/2020. In data collection, there was no written or verbal consent from participants. The reason was the investigators did NOT get participants rather, and secondary data were obtained in the patient's chart. The ethical approval committee approved the use of these secondary data for the current investigation. The data were de-identified by the investigators.
Results
Descriptive Results
The descriptive summary of baseline categorical covariates is given in Table 1. The medical cards of 205 leprosy patients were reviewed, 71 (34.63%) experienced the event or were disabled during treatment.
 |
Table 1 Descriptive Summary of Covariate Variables of Patients’ Data Taken at ALERT |
Table 1 shows the general characteristics for categorical covariates of leprosy patients involved in this study. Relatively among all, patients who were living outside of the capital city (Addis Ababa) experienced highest disability 69 (97.2%) as compared to leprosy patients who live in Addis Ababa 2 (2.8%). Patients who were male 57 (80.3%) experienced more disability than female 14 (19.7%) disability. Out of the total leprosy patients included in the study, 59 (83.1%) were disabled during treatment which was the highest disability for patients who have no family history of the disease or any contact with leprosy patient compared to other exposure history of patients. These were followed by leprosy patients who had family history of the disease with 7 (9.9%) of the disability. The category of exposure history of leprosy patients with the least percentage of disability was those who had contact with a leprosy patient out of family members with 5 (7%) of disability. Out of the total leprosy patients, 41 (57.75%) were disabled during treatment and this was the highest proportion of disability as compared with those without thickened nerve which recorded 30 (42.25%) of the disability. Most of the patients in this study were to have MB and they also recorded the highest percentage of disability 68 (95.775%) as compared to those with PB which was recorded to be 3 (4.225%) of the disability. It is also found that 61 (85.92%) patient disability is prevalent among the patients having positive smear result. About 37 (52.12%) patient disabilities were attributed to leprosy patients who have lesions on their hands at the first time of the disease. Most of the patients in this study were to have a symmetrical lesion distribution on their body, and they also recorded the lowest percentage of disability 22 (30.99%) as compared to those whose lesion distributed as asymmetric 23 (32.39%) disability and part symmetric 26 (36.62%) disability.
The mean age of leprosy patients at enrollment for the treatment was 33.78 years with a standard deviation (Std.dev) of 14.63, the minimum and maximum age in years was 6 and 80 respectively. The mean duration of symptom for patients at baseline with standard deviation (Std.dev) was 29.21 (22.53) months and the minimum and maximum duration in months was 1 and 96 respectively (Table 2).
 |
Table 2 Baseline Characteristics of Continuous Variables of Patients’ Data Taken at ALERT |
Non-Parametric Exploratory Analysis Methods
The Kaplan–Meier Estimate
Non-parametric survival analysis is very important to visualize the survival under different levels of the covariate, Moreover, it gives information on the shape of the survival and hazard functions of data set. Survival time distributions for time-to-disability was assessed for each group utilizing the K-M technique and in order to compare the survival curves of at least two groups, the log rank test has been utilized. The Kaplan–Meier survival curves for each study variable give an underlying understanding to the shape of survival function. The Kaplan–Meier survival curves see whether there is a distinction in time to disability between various classifications of the covariates. The median survival time of leprosy patient was 16 months (Figure 1).
 |
Figure 1 Kaplan–Meier survival function. |
Variables (from left to right in Figure 2): sex of patient, patient category, sensory loss, and patient’s living place respectively.
Based on the Kaplan–Meier survival curves, female patients, patients who live in Addis Ababa, patients without sensory loss, and patients who were newer for the treatment had higher survival probability than their counterparts (Figure 2).
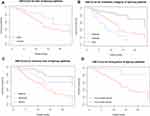 |
Figure 2 Survival function of time-to-disability by chosen covariates. |
The log rank test statistics were used to test whether there is a difference or not in the survival curve between two or more groups. The log rank test reveals that there is a significant difference (P-value <0.05) in the survival function of sex, living place, patient category, body part where the first lesion appears, degree of sensory loss, lesion distribution, and thickness of nerve (Table 3).
 |
Table 3 Results of the Log Rank Test for Each Categorical Variables of Leprosy Patients at ALERT |
Cox Proportional Hazards Model
Univariable Analysis
To examine the effect of each covariate and choose variables to include in the multivariable analysis, a univariable analysis was done. For the Cox proportional hazards model, the univariable analysis was fitted for each covariate. Sex of patients, age, duration before treatment, living place of patients, patient category, leprosy type, body part where the first lesion appears, lesion type, degree of sensory loss, lesion distribution, thickness of nerve, and smear result were significantly associated with disability during treatment status at a 25% level of significance. Those variables are candidate variables for multivariable analysis.
The confidence intervals of the HR for all significant covariates do not include one at a 5% level of significance. This showed that they are significant factors for determining disability among leprosy patients in ALERT Center, Addis Ababa, Ethiopia.
The HR of age of patients with leprosy was about 1.031 (1.0088, 1.0532), which implies that for a unit increase in age, the hazard of disability of patients was significantly increased by 3.1% (p-value =0.006) keeping all variables constant. A reduced risk of disability by 0.297 (0.1509, 0.5855) times for patients who were new for the treatment as compared to patients in the relapse category. Duration of the disease before starting the treatment for a patient is another factor that significantly predicts the disability time of patients from leprosy. That is, the hazard of disability of patients was significantly increased by 1.6% (p-value =0.024) for a unit increase in the duration of disease before treatment keeping all variables constant. In addition, there was a reduced risk of disability by 0.403 (0.1896, 0.8565) times for patients who do not have sensory loss indicating that loss of sensation was a significant factor to determine the disability from leprosy at 5% level of significance. Living place of leprosy patients was the other significant factor to develop disability during treatment. Leprosy patients who live in Addis Ababa were in less risk of disability 0.166 (0.0374, 0.7404) times than patients who do not live in Addis Ababa (Table 4).
 |
Table 4 Results of Multivariable Cox Proportional Hazard Model for Leprosy Patients at ALERT |
Test of Proportional Hazards Assumption
The proportional hazards (PH) assumption can be checked using statistical tests and graphical diagnostics based on the scaled Schoenfeld residuals.
From the output (Table 5), the test is not statistically significant for each of the covariates, and the global test is also not statistically significant. Therefore, we can assume the proportional hazards.
 |
Table 5 Test of Proportional Hazards Assumption Based on Schoenfeld Residuals for Significant Covariates |
Variables (from up to down in Figure 3): patient category (cat), degree of sensory loss (senloss) and patient living place (region) respectively.
From the graphical inspection, there is no pattern with time. The assumption of proportional hazards appears to be supported for the covariates sensory loss, patient category, and patient's living place (Figure 3).
 |
Figure 3 Plots of scaled Schoenfeld residuals versus analysis time with overlaid linear fit. |
A popular method for determining the functional form of a covariate is to plot the martingale residuals versus continuous covariates. Patterns in the plot for a continuous covariate may indicate that the variable is not correctly fit. The plots of martingale residuals against a continuous variable age and duration are examined (Figure 4).
 |
Figure 4 Martingale residuals against a continuous variable age and duration. |
The overall fit of the model was tested using a plot of the Cox–Snell residuals. The cumulative hazard of Cox–Snell residuals was plotted against the Cox–Snell residuals in this method, as demonstrated in Figure 5. The graphic shows that the Cox model has a decent overall fit. However, due to the lower effective sample size produced by prior failures and censoring, there is no indication of a systematic divergence from the straight line at the right. This can be predicted even if we had a well-fitting Cox model.9
 |
Figure 5 Cox–Snell residuals. |
Discussion
The study has empirically investigated and identified the factors that are associated with the survival during the treatment period of patients with leprosy in ALERT Center, Addis Ababa, Ethiopia, using survival methods. According to the findings in the preceding result, this study attains the following discussions.
Previous research has associated age upon diagnosis with an increased likelihood of having a physical disability from leprosy.10 The length of a disease and the time it takes to diagnose it are both known to be associated with age.11,12 Our results were similar in which age of the patient was the first factor that related to disability among leprosy patients as it was indicated in the Cox proportional hazard model in this study. The HR of age of patients with leprosy in log logistic- gamma shared frailty models was about 1.031, which implies that for a unit increase in age, the hazard of disability of patients was significantly increased by 3.1% (p-value = 0.006) keeping all variables constant. This result is similar to a study done by Shumet et al8 that shows for patients in the age group greater or equal to 30, disability was high; as people in this age group are engaged in physical work, they are vulnerable to different kinds of injuries. Our study also confirms lower chance of disability for patients who have no sensory loss. The risk of development of disability was reduced in those patients who do not loss sensory. Sensory function loss is a cause of repeated injury, ulceration, and limb shortening. Corneal sensation loss may result in unrecognized corneal injury and significant visual loss. Motor function loss is a cause of finger and toe clawing, failure of eye closure (lagophthalmos), and foot and wrist drop. This is also consistent with the results of the previous study by Shumet et al8 in Ethiopia reporting that those who presented with sensory loss were also more likely to have a disability.
Although we noticed increased occurrence of disability in patients seeking treatment late after the onset of disease (long symptom duration), a long duration of symptoms for leprosy patients before seeking the treatment have been significant risk factors for disability among leprosy cases. This may arise as patients ignored the initial symptoms as they thought the symptoms would disappear by themself. Most studies have reported statistically significant association between delay in diagnosis or a long duration of disease and Grade 2 disability. The results of this study found that the hazard of disability of patients was significantly increased by 1.6% (p-value = 0.024) for a unit increase in the duration of disease before treatment. This finding is consistent with studies on ”Prevalence of Disability and Associated Factors among Registered Leprosy Patients in All Africa TB and Leprosy Rehabilitation and Training Centre.” The study shows that the longer duration of symptoms lead to disability.8 This result is also in agreement with the findings in India by13 Sriivas et al which notes the odds of G2D/G1D at the time of diagnosis were significantly greater (Adj OR = 1.6, 95% CI: 1.3–2.2) among respondents with a patient delay of more than three months compared to those with a patient delay of less than three months (Adj OR = 1.6, 95% CI: 1.3–2.2). This is also in line with prior research, which found that patients who had symptoms for 6 to 12 months and more than 24 months had a higher risk of disability.10 Even if in this study sex and first lesion body part were not found to be statistically significant, others have noticed the greater rate of impairment connected with male sex and it was in our study as well.14 It can be explained by the fact that males are more prone to hand and foot damage as a result of their work.15 Described the most common location of disability as the feet, whereas others, like ourselves, identified the hands as the most commonly involved region in terms of disability.16 Another potential risk factor of disability was the treatment category of patients.
The majority of the patients came from outside of Addis Ababa. This could be due to patient misdiagnosis at outlying health facilities, or patients may lack the knowledge to seek health care at an early stage; by the time they acquire disability, they usually choose to travel a long distance;8 this was also true in our study results that the highest number of patients were living far from Addis Ababa and the higher risk to develop disability was for those leprosy patients who do not live in Addis Ababa.
The limitations of this study should be considered. The outcomes of this investigation were dependent on the accuracy and completeness of patient data because it was a retrospective observational study. However, the study results are good insights to have a look at leprosy patient survival status while taking treatment by critically assessing the potential factors on their survival.
Conclusion
Using survival analysis, the study explored and discovered parameters linked with the survival status of leprosy patients in ALRT centers. Age, disease duration, patient category, degree of sensory loss, and patient’s living place were all significant predictors of disability among leprosy patients, according to the Cox proportional model.
The risk of worsening of disability grade for patients during treatment taking increased with age, was higher for patients with a long length of symptoms, was higher for defaulter patients, and was lower for patients who did not lose their sensibility. The existence of a difference for the patient’s survival function in the survival curves between two or more groups of variables was also discovered in this investigation. The findings show that female patients, those who were newer to the treatment, who lives in Addis Ababa and those who did not lose sensation have a better chance of surviving.
Abbreviations
ALERT, All Africa Leprosy, Tuberculosis and Rehabilitation Training Centre; DG, disability degree; ENAPAL, Ethiopian National Association of Peoples Affected by Leprosy; FMOH, Federal Ministry of Health; G0D, grade zero disability; G1D, grade one disability; G2D, grade two disability; GLRI, German leprosy and TB Relief Association; HR, hazard ratio; MDT, multidrug therapy; MB, multi-bacillary; PB, Pauci-bacillary; TB, tuberculosis; WHO, World Health Organization.
Data Sharing Statement
On request, the data can be obtained from the corresponding author.
Ethical Considerations
The data used in the current investigation were collected previously by the health staff for treatment purpose/for diagnosis leprosy and to start follow-up treatment. To use this previously collected data, an ethical approval certificate has been obtained from the ethical clearance review committee of College of Natural and Computational Science, University of Gondar, Ethiopia, with reference number: CNCS/10627/05/19/2020. In data collection, there was no written or verbal consent from participants. The reason was the investigators did NOT get participants rather, and secondary data were obtained in the patients chart. The study was conducted according to the guidelines of the Declaration of Helsinki and the data were de-identified by the investigators.
Acknowledgments
We would like to acknowledge ALRT center to make all data available.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public commercial, or not for profit sectors.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Lastória JC, de Abreu M. Leprosy: review of the epidemiological, clinical, and etiopathogenic aspects-part 1. An Bras Dermatol. 2014;89:205–218. doi:10.1590/abd1806-4841.20142450
2. Baye S. Leprosy in Ethiopia: epidemiological trends from 2000 to 2011. Adv Life Sci Heal. 2015;2(1):31–44.
3. Van Brakel WH, Sihombing B, Djarir H, et al. Disability in people affected by leprosy: the role of impairment, activity, social participation, stigma and discrimination. Glob Health Action. 2012;5(1):18394. doi:10.3402/gha.v5i0.18394
4. Weiss MG, Utzinger J. Stigma and the social burden of neglected tropical diseases. PLoS Negl Trop Dis. 2008;2(5):e237. doi:10.1371/journal.pntd.0000237
5. Li J, Mu H, Ke W, et al. The sustainability of self-care in two counties of Guizhou Province, Peoples’ Republic of China. Lepr Rev. 2008;79(1):110–117. doi:10.47276/lr.79.1.110
6. Chandler DJ, Hansen KS, Mahato B, Darlong J, John A. Househ costs lepr react rural India. PLoS Neglected Trop Dis. 2015;9(1):e0003431. doi:10.1371/journal.pntd.0003431
7. Mondiale de la Santé W. Global leprosy (Hansen disease) update, 2019: time to step-up prevention initiatives–Situation de la lèpre (maladie de Hansen) dans Le Monde, 2019: le moment est venu d’intensifier les initiatives de prévention. Wkly Epidemiol Rec Relev Épidémiologique Hebd. 2020;95(36):417–438.
8. Shumet T, Demissie M, Bekele Y. Prevalence of disability and associated factors among registered leprosy patients in all Africa tb and leprosy rehabilitation and training centre (ALERT), Addis Ababa, Ethiopia. Ethiop J Health Sci. 2015;25(4):313–320. doi:10.4314/ejhs.v25i4.4
9. Khanal SP, Sreenivas V, Acharya SK. Comparison of cox proportional hazards model and lognormal accelerated failure time model: application in time to event analysis of acute liver failure patients in India. Nepal J Stat. 2019;3:21–40. doi:10.3126/njs.v3i0.25576
10. Moschioni C, Antunes CM, Grossi MAF, Lambertucci JR. Risk factors for physical disability at diagnosis of 19,283 new cases of leprosy. Rev Soc Bras Med Trop. 2010;43:19–22. doi:10.1590/S0037-86822010000100005
11. Jain S, Reddy RG, Osmani SN, Lockwood DNJ, Suneetha S. Childhood leprosy in an urban clinic, Hyderabad, India: clinical presentation and the role of household contacts. Lepr Rev. 2002;73(3):248–253. doi:10.47276/lr.73.3.248
12. Huan-Ying L, Yu-Lin P, Yang W. Leprosy control in Shandong Province, China, 1955–1983; some epidemiological features. Int J Lepr. 1985;53:79–85.
13. Srinivas G, Muthuvel T, Lal V, Vaikundanathan K, Schwienhorst-Stich E-M, Kasang C. Risk of disability among adult leprosy cases and determinants of delay in diagnosis in five states of India: a case-control study. PLoS Negl Trop Dis. 2019;13(6):e0007495. doi:10.1371/journal.pntd.0007495
14. Rajaram M, Pandiyan SS, Alagarsamy S. Grade 2 deformity and new leprosy cases, an issue of concern–a retrospective, descriptive study in a tertiary care hospital. J Evol Med Dent Sci. 2017;6(64):4630–4634. doi:10.14260/Jemds/2017/1001
15. Sarkar J, Dutt D, Dasgupta A. Disability among new leprosy patients, an issue of concern: an institution based study in an endemic district for leprosy in the state of West Bengal, India. Indian J Dermatol Venereol Leprol. 2012;78(3):328. doi:10.4103/0378-6323.95449
16. Ganesan DK, Muthunarayanan L. Is disability in leprosy still a burden? A cross-sectional study in a rural block in Tamil Nadu, India. Trans R Soc Trop Med Hyg. 2018;112(1):31–35. doi:10.1093/trstmh/try021
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
