Back to Journals » International Journal of General Medicine » Volume 14
Thyroid Dysfunction in Patients Admitted in Cardiac Care Unit: Prevalence, Characteristic and Hospitalization Outcomes
Authors AlQahtani A , Alakkas Z , Althobaiti F, Alosaimi M, Abuzinadah B, Abdulkhalik E, Alswat K
Received 19 November 2020
Accepted for publication 12 January 2021
Published 18 February 2021 Volume 2021:14 Pages 505—514
DOI https://doi.org/10.2147/IJGM.S292750
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Abdulrahman AlQahtani,1 Ziyad Alakkas,1 Fayez Althobaiti,1 Mohammed Alosaimi,1 Baraa Abuzinadah,1 Elshazly Abdulkhalik,2,3 Khaled Alswat4
1Internal Medicine Department, King Abdul Aziz Specialist Hospital, Taif, Makkah, Saudi Arabia; 2Consultant Cardiology, Cardiology Department, Al Azhar University, Cairo, Egypt; 3Cardiology Department, King Abdul Aziz Specialist Hospital, Taif, Makkah, Saudi Arabia; 4Department of Medicine, College of Medicine, Taif University, Taif, 21944, Saudi Arabia
Correspondence: Abdulrahman AlQahtani
Department of Medicine, College of Medicine, Taif University, P.O. Box 11099, Taif, 21944, Saudi Arabia
Tel +966 531901817
Email [email protected]
Introduction: Cardiovascular disease is one of the main causes of hospital admission and mortality, and thyroid dysfunction increases the risk of developing acute or exacerbation of chronic cardiac conditions. The aim of this study is to investigate the prevalence of thyroid hormone abnormality among patients in the cardiac care unit (CCU) patients and its relation to admission diagnosis, clinical, biochemical data, and hospital-related outcomes.
Methods: We conducted a retrospective cohort observational that included adult patients who were admitted to the CCU. We excluded those with known thyroid dysfunction and those who received amiodarone or IV contrast.
Results: A total of 374 patients with a mean age of 62.7+14.7 years old were included. Ischemic changes were observed in 70.6% of the patients based on the admission diagnosis. In comparison to the non-ischemic group, the ischemic group was more likely to be male (P=0.010), to be active/former smokers (P=0.011), to have diabetes (P=0.009), to have diastolic dysfunction (P=< 0.001), to have undergone thrombolysis (P=< 0.001), and to have been referred to a tertiary center (P=< 0.001). Euthyroidism was observed in 57.8% of the patients based on the thyroid function test at admission. Compared to patients with thyroid dysfunction, those with Euthyroidism were more likely to be active/former smokers (P=0.002), to have lower heart rates (P=0.018), to not have chronic kidney disease (P=0.016), to not have heart failure (P=0.006), to have lower thyroid-stimulating hormone (TSH) levels (P=< 0.001), and to have lower tricuspid regurgitation (P=0.042).
Conclusion: Thyroid dysfunction is common among patients admitted to the CCU. Non-significant positive correlations between TSH and hospitalization length, tertiary center referral, 30-day readmission, and in-hospital mortality when adjusting for potential confounders.
Keywords: thyroid disease, sick euthyroid, acute coronary syndrome, heart failure, ischemic heart disease, nonthyroidal illness syndrome, NTIS
Introduction
Cardiovascular disease poses one of the heaviest burdens on any health-care system. It is responsible for more than 17 million deaths worldwide and is one of the main causes of hospital admission. The prevalence of ischemic cardiac disease and its complications is the highest. Thus, the spotlight has been shined on primary and secondary prevention and identifying conditions that increase the risk of cardiac events through both biochemical and clinical data.1
Thyroid hormone has a major effect on the cardiovascular system.2–4 Changes in thyroid hormone levels (either up or down) produce effects on heart contractility, oxygen consumption, and systemic vascular resistance.5 The diagnosis and management of thyroid disorders are crucial as most of these changes are reversible. Thyroid disorders are common, affecting around 9–15% of the adult population and being more common in females, although the rate becomes more equal between men and women at advanced ages.6
Patients with hyperthyroidism usually present with symptoms and signs that are more related to the cardiovascular system.7 A state of hyperthyroidism affects the hemodynamics of the heart and increases the heart rate, systolic blood pressure, cardiac output, contractility, and left ventricular ejection fraction (LVEF), while it decreases peripheral vascular resistance. In severe cases of hyperthyroidism, these changes may eventually lead to high-output heart failure. In fact, some use the term “thyrotoxic cardiomyopathy” to describe the damage that may happen because of a severe chronic hyperthyroid state.3
An increased incidence of atrial fibrillation with hyperthyroidism has been well identified. The range of incidence is 2–20%,8 with 13.8% occurring in cases of overt hyperthyroidism, as opposed to 2.3% in the general population,9 especially in the elderly and those with cardiac disease.10,11 Hashimoto and Graves diseases are both noted to be more associated with mitral valve prolapse, which might be followed left atrium enlargement and atrial fibrillation.12 Subclinical hyperthyroidism may increase risk for mortality, coronary artery disease, and atrial fibrillation.13 Low thyroid-stimulating hormone (TSH) was linked with more risk for atrial fibrillation,14 and mortality from cardiovascular diseases.15
In contrast, hypothyroidism manifests with decreased heart rate, cardiac contractility, and cardiac output, along with a mild increase in diastolic blood pressure due to the effect on the renin-angiotensin-aldosterone system.6 Although these changes rarely cause heart failure by themselves, they may lead to worsening clinical conditions in patients with heart failure, as well as worsening hospital outcomes.16 Furthermore, hypothyroidism has been identified to affect lipid metabolism, and multiple studies have found that it is associated with higher cholesterol and low-density lipoprotein (LDL) levels.17 The prevalence of subclinical hypothyroidism is 7–10% among older women, and it has an effect on lipid metabolism17,18 with increased lipid and cholesterol levels, which appear to be parallel with serum TSH,7,19 accelerated atherosclerosis, and coronary artery disease.20
It has been found that 23.3% of the patients with acute myocardial infarction have Nonthyroidal Illness Syndrome (NTIS), which improves the predictive value of in-hospital cardiovascular deaths in such patients.21 It has also been linked in past and recent data with increased risk of all-cause mortality and major adverse cardiac events (MACE).22 Cardiovascular diseases are some of the major causes of hospital admission and the leading cause of death worldwide. Furthermore, thyroid dysfunction is a risk factor for cardiac disease, as well as mortality among patients with cardiac disease.1,23 Thus, the aim of this study is to investigate the prevalence of thyroid hormone abnormality in cardiac care unit (CCU) patients and its relation to admission diagnosis, clinical, biochemical data, and hospital-related outcomes.
Patients and Methods
A retrospective cohort observational study was conducted in the Cardiology Department at King Abdul Aziz Specialist Hospital in Taif City, Saudi Arabia. A total of 411 patients were considered for enrollment. The patients were selected from those who were admitted to the CCU due to acute cardiovascular events or exacerbation of chronic cardiac condition between December 2015 and December 2018.
The inclusion criteria were age older than 18 years, both sexes, and no known thyroid disease. We excluded 37 patients because they either had a history of thyroid disease or received amiodarone or IV contrast before blood extraction. After the exclusion, 374 patients were included. The data collected included diagnosis at admission, past medical history of either underlying cardiac disease or other conditions that are considered as a risk factor for cardiac disease, special habits, length of hospitalization, electrocardiograms, echocardiographic evaluations, clinical and biochemical data, and hospitalization-related outcomes.
Laboratory investigations included triglyceride (TGL), high-density lipoprotein (HDL), LDL, total cholesterol, and thyroid function tests (free thyroxine (FT4), free triiodothyronine (FT3), and TSH). The levels were measured from venous blood samples extracted at admission. The results were interpreted by a board-certified endocrinologist, and patients were categorized according to their thyroid state (Table 1) and as it listed FT4 had no significance to reaching the diagnosis of NTIS as it can be falsely high, normal, or low in ill patients as an effect of received treatment or due to the illness itself.24 Results that did not fit any of the mentioned conditions were classified as uninterpretable.
 |
Table 1 Interpretation of Thyroid Function Test |
Echocardiographic evaluation was conducted by a certified cardiologist (Philips CX50 Echocardiography). Information on left ventricular ejection fraction (LVEF), diastolic dysfunction, left ventricular hypertrophy (LVH), and valvular pathology were collected for all patients. Furthermore, we documented the presence of left or right bundle branch block through 12-lead electrocardiograms.
According to the diagnosis upon admission, patients were categorized into an ischemic group and non-ischemic group. We compared these groups’ baseline characteristics, thyroid state, underlying chronic diseases (both cardiac and non-cardiac), biochemical data, echocardiographic findings, and hospitalization-related outcomes. The study proposal was submitted to and approved by the Institutional Review Board (IRB) at Taif Health Affairs and the Medical Research Unit at King Abdul Aziz Specialist Hospital.
All qualitative and quantitative data were collected from patients’ medical records. The data were entered and coded through Microsoft Excel (Microsoft, Redmond, WA, USA) and analyzed using SPSS version 26 (SPSS Inc., Chicago, IL, USA). The clinical characteristics were compared for patients with and without thyroid dysfunction, and we defined statistical significance as p < 0.05. Chi-squared tests were performed for categorical variables, and unpaired t-tests were used for continuous variables.
Results
The 374 patients had a mean age of 62.7+14.7 years, were mostly Saudi males, and had a mean hospital stay of 4.0+4.4 days (Table 2). One-third of the sample was active/former smokers, and around 5% of them had right or left bundle branch block on electrocardiograms. The most common admission diagnosis was acute coronary syndrome, followed by heart failure. The least common diagnosis was valvular, congenital, and acute aortic syndrome. The most common thyroid diagnosis based on the thyroid function test at admission was euthyroidism, followed by NTIS, and the least common ones were T3 toxicosis and subclinical hyperthyroidism.
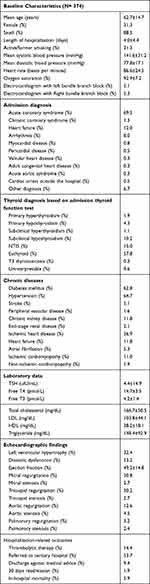 |
Table 2 Baseline Characteristics of the Whole Cohort |
The most common chronic diseases were hypertension, followed by diabetes mellitus (DM), and the least common were peripheral artery disease and non-ischemic cardiomyopathy. The mean results of the thyroid function test and lipid profile were in the normal/controlled range. Regarding the echocardiographic findings, one-third of the patients had LVH, while more than half of them had diastolic dysfunction and mitral regurgitation. More than half of the patients were referred to a tertiary center for intervention, and the in-hospital mortality rate was 5.9%.
Ischemic changes were observed in 70.6% of the patients based on the admission diagnosis (Table 3). Compared to the non-ischemic group, the ischemic group was more likely to be male (P=0.010), to have a shorter hospital stay (P=0.012), to be active/former smokers (P=0.011), to have higher oxygen saturation (P=0.001), to have DM (P=0.009), to have higher total cholesterol levels (P=<0.001), to have higher LDL levels (P=0.001), to have higher TGL levels (P=0.007), to have diastolic dysfunction (P=<0.001), to have undergone thrombolysis (P=<0.001), and to be referred to a tertiary center (P=<0.001). The ischemic group was less likely to have chronic kidney disease (P=<0.001), heart failure (P=<0.001), atrial fibrillation (P=<0.001), cardiomyopathy (P=<0.001), mitral regurgitation (P=0.030), tricuspid regurgitation (P=0.006), and aortic stenosis (P=0.029) when compared to the non-ischemic group.
 |
Table 3 Baseline Characteristics Based on the Admission Diagnosis Category |
Euthyroidism was observed in 57.8% of the patients based on the thyroid function test at admission (Table 4). Compared to those with thyroid dysfunction, those with euthyroidism were more likely to be active/former smokers (P=0.002), to have lower heart rates (P=0.018), to not have chronic kidney disease (P=0.016), to not have heart failure (P=0.006), to have lower TSH levels (P=<0.001), to have lower tricuspid regurgitation (P=0.042), and to have lower aortic regurgitation (P=0.007). The highest TSH level was observed in those with heart failure and acute aortic syndrome, while the lowest was observed in those with pericardial disease (Figure 1).
 |
Table 4 Baseline Characteristics Based on the Admission Thyroid Function Test |
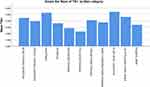 |
Figure 1 The mean TSH according to the admission diagnosis. |
Partial correlation analyses were done with adjustments for gender, age, total cholesterol, HDL, TGL, LDL, systolic and diastolic blood pressure, heart rate, oxygen saturation, DM, hypertension, cerebrovascular accident, peripheral vascular disease, chronic kidney disease, and end-stage renal disease and smoking history. The results showed non-significant positive correlations between TSH and each of the following: 30-day readmission (r=0.15, P=0.815), in-hospital mortality (r=0.026, P=0.679), referral to a tertiary center (r=0.058, P=0.349), and length of hospital stay (r=0.034, P=0.590).
Discussion
This study showed that most patients were male with a mean age of 62.7+14.7 years. A recent study showed similar sex and mean-age distributions to those observed in our study.25 Around 5% of the patients in our study had right and left bundle branch blocks, which is like a previous study.26 The prevalence of the left bundle branch block was higher in the previous study, and this difference is likely due to the lower percentage of the heart failure patients in our study.27
The most common diagnosis on admission was acute coronary syndrome, which had a prevalence of 69.3%. This is consistent with a recently published study.28 NTIS was only present in 15% of the patients which is similar to previous studies,29,30 while euthyroidism was prevalent in 57.8%. A recent study on critically ill patients showed that 84% of the patients having altered thyroid function.31 Most patients had DM and hypertension, and half of the sample had diastolic dysfunction. A recent systemic review showed that 48% of the hospitalized patients had diastolic dysfunction, which is consistent with our findings.32 The in-hospital mortality rate in our study was 5.9%, which is slightly higher than reported in a previous study from the United States, which showed an average annual rate of 3.4%.33 This difference is likely related to the study design and duration, along with the lack of facilities like cardiac catheterization units at our hospital.
In our study, 70% of the patients had ischemic changes, which were more common among males. This concurs with a previous study with a similar age distribution.34 Our study showed that 53.2% of the patients had diastolic dysfunction, which is also like other studies.35,36 Valvular disease was more prevalent in the non-ischemic group, as reported previously.37 This is likely explained by those with valvular disease presenting with heart failure rather than ischemic changes.
Our study showed that TSH is positively associated with 30-day hospital readmission, in-hospital mortality, referral to a tertiary center, and length of hospital stay. A recent study showed that TSH more than 4 is correlated with worse hospital outcomes.38 Another recent study showed that women with high TSH were at significantly higher risk of increased mortality from coronary artery disease.39 Most of our patients were male, and this more likely why our result was non-significant.
Conclusion
Thyroid dysfunction is common among patients admitted to the CCU, among which NTIS was been the most common diagnosis. Non-significant positive correlations between TSH and hospitalization length, tertiary center referral, 30-day readmission, and in-hospital mortality when adjusting for potential confounders.
Abbreviations
CCU, cardiac care unit; NTIS, non-thyroidal illness syndrome; TSH, thyroid-stimulating hormone; FT4, Free thyroxine; FT3, Free triiodothyronine; LVEF, left ventricular ejection fraction; LVH, left ventricular hypertrophy; LDL, Low-density lipoprotein; HDL, high-density lipoprotein; TGL, triglyceride; DM, diabetes mellitus; MACE, major adverse cardiac events; IRB, Institutional Review Board.
Ethics Approval and Consent to Participate
There are no apparent issues that interfere with the routine care of patients while conducting the study and as this study did not involve any treatment or intervention, due to the retrospective nature of it, so no consent was needed as it was approved by the Institutional Review Board (IRB) at Taif Health Affairs and the Medical Research Unit at King Abdul Aziz Specialist Hospital.
This study maintained Patient data confidentiality in accordance with the ethical standers of the Helsinki declaration and the national committee for BioEthics (NCBE) at King Abdulaziz city for science and technology, Saudi Arabia.
Funding
This project was supported by the Taif University Research Support Project Number (TURSP-2020/37), Taif University, P.O. Box 11099, Taif, 21944, Saudi Arabia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25. doi:10.1016/j.jacc.2017.04.052
2. Danzi S, Klein I. Thyroid disease and the cardiovascular system. Endocrinol Metab Clin North Am. 2014;43(2):517–528. doi:10.1016/j.ecl.2014.02.005
3. Dillmann WH. Cellular action of thyroid hormone on the heart. Thyroid. 2002;12(6):447–452. doi:10.1089/105072502760143809
4. Danzi S, Klein I. Thyroid hormone and the cardiovascular system. Med Clin North Am. 2012;96(2):257–268. doi:10.1016/j.mcna.2012.01.006
5. Kahaly GJ, Dillmann WH. Thyroid hormone action in the heart. Endocr Rev. 2005;26(5):704–728. doi:10.1210/er.2003-0033
6. Biondi B, Palmieri EA, Lombardi G, Fazio S. Effects of thyroid hormone on cardiac function: the relative importance of heart rate, loading conditions, and myocardial contractility in the regulation of cardiac performance in human hyperthyroidism. J Clin Endocrinol Metab. 2002;87(3):968–974. doi:10.1210/jcem.87.3.8302
7. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The colorado thyroid disease prevalence study. Arch Intern Med. 2000;160(4):526–534. doi:10.1001/archinte.160.4.526
8. Klein I, Danzi S. Thyroid disease and the heart. Circulation. 2007;116(15):1725–1735. doi:10.1161/CIRCULATIONAHA.106.678326
9. Klein I, Zipes DP, Libby P. Endocrine disorders and cardiovascular disease. In: Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine.
10. Frost L, Vestergaard P, Mosekilde L. Hyperthyroidism and risk of atrial fibrillation or flutter: a population-based study. Arch Intern Med. 2004;164(15):1675–1678. doi:10.1001/archinte.164.15.1675
11. Ruggeri RM, Trimarchi F, Biondi B. L-Thyroxine replacement therapy in the frail elderly: a challenge in clinical practice. Eur J Endocrinol. 2017;177(4):R199–R217. doi:10.1530/EJE-17-0321
12. Evangelopoulou ME, Alevizaki M, Toumanidis S, et al. Mitral valve prolapse in autoimmune thyroid disease: an index of systemic autoimmunity? Thyroid. 1999;9(10):973–977. doi:10.1089/thy.1999.9.973
13. Biondi B, Palmieri EA, Fazio S, et al. Endogenous subclinical hyperthyroidism affects quality of life and cardiac morphology and function in young and middle-aged patients*. J Clin Endocrinol Metab. 2000;85(12):4701–4705. doi:10.1210/jcem.85.12.7085
14. Sawin CT, Geller A, Wolf PA, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med. 1994;331(19):1249–1252. doi:10.1056/NEJM199411103311901
15. Parle JV, Maisonneuve P, Sheppard MC, Boyle P, Franklyn JA. Prediction of all-cause and cardiovascular mortality in elderly people from one low serum thyrotropin result: a 10-year cohort study. Lancet. 2001;358(9285):861–865. doi:10.1016/S0140-6736(01)06067-6
16. Rothberger GD, Gadhvi S, Michelakis N, Kumar A, Calixte R, Shapiro LE. Usefulness of serum triiodothyronine (T3) to predict outcomes in patients hospitalized with acute heart failure. Am J Cardiol. 2017;119(4):599–603. doi:10.1016/j.amjcard.2016.10.045
17. Duntas LH. Thyroid disease and lipids. Thyroid. 2002;12(4):287–293. doi:10.1089/10507250252949405
18. Razvi S, Ingoe L, Keeka G, Oates C, McMillan C, Weaver JU. The beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: randomized, crossover trial. J Clin Endocrinol Metab. 2007;92(5):1715–1723. doi:10.1210/jc.2006-1869
19. Staub JJ, Althaus BU, Engler H, et al. Spectrum of subclinical and overt hypothyroidism: effect on thyrotropin, prolactin, and thyroid reserve, and metabolic impact on peripheral target tissues. Am J Med. 1992;92(6):631–642. doi:10.1016/0002-9343(92)90782-7
20. Hak AE, Pols HAP, Visser TJ, Drexhage HA, Hofman A, Witteman JCM. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam study. Ann Intern Med. 2000;132(4):270–278. doi:10.7326/0003-4819-132-4-200002150-00004
21. Su W, Zhao XQ, Wang M, Chen H, Li HW. Low T3 syndrome improves risk prediction of in-hospital cardiovascular death in patients with acute myocardial infarction. J Cardiol. 2018;72(3):215–219. doi:10.1016/j.jjcc.2018.02.013
22. Chang C-Y, Chien Y-J, Lin P-C, Chen C-S, Wu M-Y. Nonthyroidal illness syndrome and hypothyroidism in ischemic heart disease population: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2020;105(8):8. doi:10.1210/clinem/dgaa310
23. Iervasi G, Molinaro S, Landi P, et al. Association between increased mortality and mild thyroid dysfunction in cardiac patients. Arch Intern Med. 2007;167(14):1526–1532. doi:10.1001/archinte.167.14.1526
24. Welsh KJ, Stolze BR, Yu X, Podsiadlo TR, Kim LS, Soldin SJ. Assessment of thyroid function in intensive care unit patients by liquid chromatography tandem mass spectrometry methods. Clin Biochem. 2017;50(6):318–322. doi:10.1016/j.clinbiochem.2016.11.022
25. Doğan S, Dursun H, Can H, Ellıdokuz H, Kaya D. Long-term assessment of coronary care unit patient profile and outcomes: analyses of the 12-years patient records. Turkish J Med Sci. 2016;46(3):801–806. doi:10.3906/sag-1502-88
26. Alventosa-Zaidin M, Guix Font L, Benitez Camps M, et al. Right bundle branch block: prevalence, incidence, and cardiovascular morbidity and mortality in the general population. Eur J Gen Pract. 2019;25(3):109–115. doi:10.1080/13814788.2019.1639667
27. Clark AL, Goode K, Cleland JGF. The prevalence and incidence of left bundle branch block in ambulant patients with chronic heart failure. Eur J Heart Fail. 2008;10(7):696–702. doi:10.1016/j.ejheart.2008.05.001
28. Al-Ghamdi MA. Morbidity pattern and outcome of patients admitted in a coronary care unit: a report from a secondary hospital in southern region, Saudi Arabia. J Community Hosp Intern Med Perspect. 2018;8(4):191–194. doi:10.1080/20009666.2018.1500421
29. Abdulaziz Qari F. Thyroid hormone profile in patients with acute coronary syndrome. Iran Red Crescent Med J. 2015;17:7. doi:10.5812/ircmj.26919v2
30. Kannan L, Shaw PA, Morley MP, et al. Thyroid dysfunction in heart failure and cardiovascular outcomes. Circ Heart Fail. 2018;11(12):e005266. doi:10.1161/CIRCHEARTFAILURE.118.005266
31. Loh KC, Eng PC. Prevalence and prognostic relevance of sick euthyroid syndrome in a medical intensive care unit.. Ann Acad Med Singapore. 1995;24(6):802–806.
32. Bouthoorn S, Valstar GB, Gohar A, et al. The prevalence of left ventricular diastolic dysfunction and heart failure with preserved ejection fraction in men and women with type 2 diabetes: a systematic review and meta-analysis. Diabetes Vasc Dis Res. 2018;15(6):477–493. doi:10.1177/1479164118787415
33. Akintoye E, Briasoulis A, Egbe A, et al. National trends in admission and in-hospital mortality of patients with heart failure in the United States (2001–2014). J Am Heart Assoc. 2017;6(12):12. doi:10.1161/JAHA.117.006955
34. Ten Haaf ME, Bax M, Ten Berg JM, et al. Sex differences in characteristics and outcome in acute coronary syndrome patients in the Netherlands. Netherlands Hear J. 2019;27(5):263–271. doi:10.1007/s12471-019-1271-0
35. Kindermann M. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28(21):2686. doi:10.1093/eurheartj/ehm379
36. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2017;177(4):251–259. doi:10.1530/EJE-17-0321
37. Hasdai D. Acute coronary syndromes in patients with pre-existing moderate to severe valvular disease of the heart: lessons from the Euro-Heart Survey of acute coronary syndromes. Eur Heart J. 2000;85(12):623–629. doi:10.1210/jcem.85.12.7085
38. Soeiro A, Araújo VA, Vella JP, et al. Is there any relationship between TSH levels and prognosis in acute coronary syndrome? Arq Bras Cardiol. 2000;132(4):113–118. doi:10.7326/0003-4819-132-4-200002150-00004
39. Åsvold BO, Bjøro T, Platou C, Vatten LJ. Thyroid function and the risk of coronary heart disease: 12-year follow-up of the HUNT Study in Norway. Clin Endocrinol (Oxf). 2020;105(8):911–917. doi:10.1210/clinem/dgaa310
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
