Back to Journals » Clinical Ophthalmology » Volume 17
Three-Year Outcomes of Immediate Primary Phacoemulsification on Acute Primary Angle Closure Eyes and the Fellow Eyes
Authors Suzuki T , Fujishiro T, Tachi N, Ueta Y, Okamoto Y, Fukutome T, Sasajima H , Ishida H, Watanabe Y, Hashimoto Y
Received 10 February 2023
Accepted for publication 27 March 2023
Published 5 April 2023 Volume 2023:17 Pages 1035—1045
DOI https://doi.org/10.2147/OPTH.S406067
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Takafumi Suzuki,1,2 Takashi Fujishiro,2 Naoko Tachi,1,3 Yoshiki Ueta,1 Yasuhiro Okamoto,1 Takao Fukutome,1 Hirofumi Sasajima,1 Hidetoshi Ishida,1,4 Yuji Watanabe,1 Yoshihiro Hashimoto1
1Department of Ophthalmology, Shinseikai Toyama Hospital, Imizu, Japan; 2Department of Ophthalmology, The University of Tokyo Hospital, Bunkyo, Japan; 3Tachi Eye Clinic, Toyama, Japan; 4Department of Ophthalmology, Kanazawa Medical University, Ishikawa, Japan
Correspondence: Takashi Fujishiro, Department of Ophthalmology, University of Tokyo Graduate School of Medicine, 7-3-1 Hongō, Bunkyō-ku, Tokyo, 113-8655, Japan, Tel +81-3-3815-5411, Email [email protected]
Purpose: This study investigated the long-term outcomes (> 3 years) of immediate primary phacoemulsification in eyes with acute primary angle closure (APAC) and in the fellow eyes with shallow anterior chamber to prevent APAC development.
Patients and Methods: This is a retrospective study of phacoemulsification for APAC using bilateral eyes. Best-corrected visual acuity (BCVA), intraocular pressure (IOP), and number of IOP-lowering medications at the preoperative examination (Pre), postoperative month 1 (1m), year 3 (3y), and last visit were compared between 14 eyes with APAC and their 14 fellow eyes. The number of corneal endothelial cells (CECs) at Pre and at more than 2 weeks after phacoemulsification was compared. The visual field mean deviation (MD) within 1 year after phacoemulsification and at the last visit was also compared.
Results: For APAC eyes, BCVA was significantly improved at 1m, 3y, and at the last visit as compared with Pre (p < 0.05). IOP significantly decreased at 1m, 3y, and at the last visit compared with Pre (p < 0.05). IOP-lowering medication use decreased significantly from Pre to 1m (p < 0.05). The number of CECs was not significantly different between Pre and more than 2 weeks after phacoemulsification. BCVA was significantly worse in APAC eyes than in fellow eyes at Pre (p < 0.05). IOP and the number of IOP-lowering medications were significantly higher in APAC eyes than in fellow eyes at Pre (p < 0.05).
Conclusion: Primary phacoemulsification improved visual acuity for APAC eyes and maintained good IOP control without the need for reoperation. Moreover, it preserved the number of CECs for the APAC and fellow eyes in the long term.
Keywords: acute primary angle closure, fellow eye, long-term outcome, phacoemulsification
Introduction
Glaucoma has the potential to gradually harm the optic nerve despite its initial lack of symptoms. Glaucoma is thought to affect 76 million individuals worldwide.1 Glaucoma lowers the quality of life, which is directly tied to health problems and financial losses. The frequency of glaucoma in older adults is 3.5% worldwide; by 2040, there will be 111.8 million people living with the condition.1 Globally, this illness is the main contributor to permanent blindness.2 Lowering the intraocular pressure (IOP) can stop or delay further advancement even if this damage is permanent.
Treatment is needed immediately for acute primary angle closure (APAC). Standard courses of treatment include i) miosis eye drops to remove the pupillary block; ii) eye drops or intravenous infusion of IOP-lowering medications; and iii) laser peripheral iridotomy (LPI) or phacoemulsification to remove the pupillary block.3–6
A few randomized control trials (RCTs) with more than 1 year of follow-up have reported on the clinical course after primary phacoemulsification without LPI.4,5,7 However, they did not use the fellow eyes as control.
To the best of our knowledge, a 3-year follow-up period has been the longest follow-up period after primary phacoemulsification for APAC reported to date,7 and there is no report regarding primary phacoemulsification for APAC using the fellow eyes as control.
Therefore, we retrospectively examined APAC eyes and the fellow eyes as control whose follow-up periods exceeded 3 years after primary phacoemulsification.
Materials and Methods
Ethics
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Shinseikai Toyama Hospital (approval number: 230123–2). Our study was retrospective, and we used an opt-out consent process; informed consent was waived by the Institutional Review Board of Shinseikai Toyama Hospital.
Patients
The patient database at Shinseikai Toyama Hospital was searched for patients with APAC who visited the hospital between October 2009 and October 2021. These records were reviewed. The inclusion criteria were as follows: (1) a history of intermittent blurring of vision with halos and at least two of the following symptoms: ocular or periocular pain, nausea, and/or vomiting; (2) IOP > 30 mmHg and presence of at least three of the following signs: conjunctival injection, corneal epithelial edema, mid-dilated pupil, shallow anterior chamber, and iris atrophy; (3) phacoemulsification performed in the APAC eye, followed by phacoemulsification of the fellow eye to prevent APAC development; (4) at least 3 years of follow-up; (5) age > 50 years; (6). The exclusion criteria were as follows: (1). Secondary glaucoma, such as neovascular glaucoma, phaco-lytic glaucoma, and uveitic glaucoma; (2) pseudo-phakic eyes, aphakic eyes, or eyes that underwent LPI; (3) patients with APAC in both eyes. Initially, 42 patients were included. Two patients were excluded because they had previously undergone phacoemulsification of the fellow eye at another hospital and we had no preoperative data for the fellow eye. Another two patients were excluded because their fellow eye had chronic angle closure glaucoma, which was inappropriate as control for the APAC eye. One patient was excluded because he had anisotropic amblyopia and we considered that there was a difference in ocular morphology between his right and left eye. In total, 23 patients were excluded because their follow-up period was less than 3 years. Eventually, 28 eyes from 14 patients who had a follow-up period of more than 3 years were included in the study. All the patients agreed to undergo phacoemulsification for the fellow eyes with shallow anterior chamber to prevent APAC development.
Ophthalmic Examinations
All patients in this study underwent comprehensive examinations including best-corrected visual acuity (BCVA) measured by Landolt C chart, IOP measurement, specular microscopy (Konan Medical FA3709P, Hyogo, Japan), and slit-lamp biomicroscopy. All IOPs were measured using non-contact tonometry (Nidek NT-530, Gamagori, Japan), and the average of three measurements was used. Visual field tests were performed using a Humphrey Field Analyzer (HFA; Carl Zeiss, Jena, Germany) with a SITA 24–2.
Treatment Protocol
All patients underwent phacoemulsification within days after the onset of APAC. After the patient arrived at the hospital, the pre-surgery ophthalmic examination and tests were finished. Topical administration of tropicamide and phenylephrine in place of LPI and phacoemulsification for the APAC eye were started immediately. When the patient experienced severe headache or nausea, we used IOP-lowering eye drops, oral acetazolamide, intravenous glycerol, or intravenous mannitol.
Under topical and sub-tenon anesthesia with 1–2 mL of 2% xylocaine, two surgeons (NT and YU) performed phacoemulsification with intraocular lens (IOL) implantation.
The anterior chamber was reformed with viscoelastic, and the angle was monitored with a Mori goniotomy lens (RE MEDICAL Inc., Osaka, Japan) following the insertion of the IOL. When peripheral anterior synechiae (PAS) were detected, goniosynechialysis (GSL) was performed without angle dissection. By putting viscoelastic material against the peripheral iris with a blunt needle inserted close to the PAS, the surgeons gently pushed the iris backward and revealed the trabecular meshwork. If PAS persisted, a Nagata GSL needle (Inami, Japan) was used for the same procedure. If PAS persisted despite the application of these measures, GSL was discontinued before goniodialysis happened.
Following surgery, patients were given a combination of fluorometholone or betamethasone 0.1% four times per day, moxifloxacin 0.5% three times per day, and bromfenac 0.1% twice per day, tapered over a month.
After the condition of the operated APAC eyes settled, the same surgery was performed on the fellow eyes to prevent APAC development.
Evaluation of the Effectiveness of Immediate Phacoemulsification
After the preoperative examination (Pre) and surgery, the patients were followed-up after 1 month (1m), 3 years (3y), and at the last visit for APAC eyes and their fellow eyes. We recorded the patients’ age, the follow-up period from phacoemulsification to the last visit, the time from APAC onset to surgery initiation, the time from arrival at the hospital to the start of surgery, surgery time, perioperative complications, BCVA, IOP, and the number of IOP-lowering medications at Pre, 1m, 3y, and at the last visit and the changes in the above values, number of corneal endothelial cells (CECs) at Pre and at more than 2 weeks after surgery, and the change in these values, and visual field mean deviation (MD) within 1 year after surgery and release of glaucoma attack and at the last visit, as well as the change in these values.
We performed the same evaluation on the fellow eyes as for the APAC eyes. We also examined the differences in all parameters between APAC eyes and fellow eyes for all periods.
Statistical Analysis
Continuous variables are presented as means ± standard deviations (range, minimum–maximum) for normally distributed variables. The BCVA was converted to the logarithm of the minimal angle of resolution. The Wilcoxon signed-rank test was used to compare BCVA, IOP, and the number of IOP-lowering medications at Pre, 1m, 3y, and at the last visit for the APAC and fellow eyes.
The Wilcoxon signed-rank test was used to compare visual field MD within 1 year after surgery and at the last visit, and the number of CECs between Pre and more than 2 weeks after surgery for APAC eyes and fellow eyes. The Wilcoxon signed-rank test was also used to compare follow-up periods, operation time, BCVA, IOP, number of CECs, IOP-lowering medications, and visual field MD between APAC eyes and fellow eyes, at all time-points.
Statistical significance was set at p < 0.05.
Statistical analyses were performed using R version 4.0.2 (The R Foundation for Statistical Computing, Vienna, Austria). Findings should be interpreted as exploratory because multiple comparisons leads to the potential increase in type 1 error.7 The statistics were checked by a biostatistician (YH) experienced in eye research.
Results
Patient Characteristics
Twenty-eight eyes of 14 patients were included in this study. Patient characteristics are presented in Table 1. The patients included two men (four eyes) and 12 women (24 eyes). Seven patients of 14 patients were administered IOP-lowering eye drops, oral acetazolamide, intravenous glycerol, or intravenous mannitol due to severe headache or nausea, but the other seven patients were not administered them. Two patients were administered four IOP-lowering medications, four patients were administered two IOP-lowering medications, and one patient was administered one IOP-lowering medication. One patient had pseudoexfoliation syndrome, without lens dislocation, in both eyes. With proper preoperative preparation, favorable outcomes can be achieved in cataract surgery in pseudoexfoliation syndrome.8 In addition, the design of our study is comparison of APAC eyes and fellow eyes, and both the eyes had pseudoexfoliation syndrome. That is why this comorbidity was not considered to have confounded our results significantly. All patients underwent phacoemulsification for APAC on the day of their initial visit to our hospital and patients were followed-up for a mean of more than 5 years.
 |
Table 1 Summary of Results for the Current Study |
The mean time from the initial visit to our hospital to phacoemulsification was 4.1 ± 5.8 (1–24) h for the APAC eyes and 284.0 ± 500.6 (19–1938) h for the fellow eyes. The mean time from onset to phacoemulsification was 54.5 ± 56.0 (7–175) h for the APAC eyes and 333.9 ± 494.7 (28–1949) h for the fellow eyes (Table 1).
An accurate and quantitative assessment of the degree and extent of PAS using gonioscopy during ophthalmic examination was not possible because of corneal edema and symptoms, such as headache or nausea.
Operation and Complications
Ten of the 14 eyes with APAC, but none of the fellow eyes, had corneal edema at the beginning of surgery. The operative time was significantly longer in the APAC eyes than in the fellow eyes (p = 0.007) (Table 1).
The IOL was inserted into the bag in all cases in both APAC and fellow eyes, and no severe adverse events were observed in either of the two groups. Small surgical complications included iris prolapse in three eyes and anterior chamber hemorrhage in one eye in the APAC group. On postoperative day 1, three APAC eyes had anterior chamber fibrin and one eye had anterior chamber hemorrhage, which improved over time. None of the APAC eyes required a reoperation during the follow-up period (Table 2). An accurate and quantitative assessment of the degree and extent of PAS using a Mori goniotomy lens during surgery was not possible because of the corneal edema in the APAC eyes. However, there were eight eyes, in which even a small extent of PAS was identified within the range visible with the lens. Five APAC eyes underwent GSL using only viscoelastic material and three APAC eyes underwent GSL using viscoelastic material and Nagata needle.
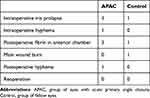 |
Table 2 Summary of Surgical Complications |
In the fellow eyes, small surgical complications included iris prolapse in one eye and main wound burn in one eye, which required suturing. On postoperative day 1, one fellow eye had anterior chamber fibrin that improved within a few days (Table 2). There were four eyes, in which even a small extent of PAS was identified within the range visible with the lens. Three fellow eyes underwent GSL using only viscoelastic material and one fellow eye underwent GSL using viscoelastic material and Nagata needle.
All the patients had deepening of the anterior chamber and opening of the angle in both eyes (Figure 1).
Changes in BCVA, IOP, Number of CECs, Medication, and MD
For the 14 APAC eyes, BCVA was significantly improved at 1m, 3y, and the last visit compared with that at Pre (p = 0.002, p < 0.001, and p = 0.002). IOP significantly decreased at 1m, 3y, and at the last visit compared to that at Pre (all p = 0.002). CECs did not differ significantly between Pre and more than 2 weeks after surgery (p = 0.945) (Figure 2), and the number of IOP-lowering medications decreased significantly at 1m (p = 0.020), but not at 3y or at the last visit (p = 0.052 and p = 0.052) as compared with that at Pre. There was no significant difference in the visual field MD at the last visit as compared with that within 1 year after surgery (p = 0.375) (Table 1; Figure 3).
For the 14 fellow eyes, there was no significant difference in BCVA at 1m, 3y, and last visit compared with that at Pre (p = 0.305, p = 0.138, and p = 0.476, respectively). IOP significantly decreased at 1m (p= 0.024), but not at 3y and at the last visit (p = 0.833 and p = 0.727) as compared to that at Pre. The number of CECs did not differ significantly between Pre and more than 2 weeks after surgery (p = 0.831) (Figure 2), and the number of IOP-lowering medications did not differ significantly at 1m, 3y, and at the last visit as compared with that at Pre (p = 1, p = 1, and p = 1, respectively). There was no significant difference in the visual field MD at the last visit compared with that within 1 year postoperatively (p = 0.625) (Table 1; Figure 3).
The results of the comparison of the APAC and fellow eyes were as follows:
BCVA was significantly different at Pre between the two groups, although it was not significantly different at 1m, 3y, and at the last visit (p = 0.001, 0.169, 0.726, and 0.593, respectively). IOP was significantly different at Pre between the two groups, although it was not significantly different at 1m, 3y, and at the last visit (p = 0.002, 0.133, 0.875, and 0.724, respectively). The number of CECs did not differ significantly between the two groups at Pre and more than 2 weeks after the operation (p = 0.820 and p = 0.765, respectively). The number of IOP-lowering medications was significantly different at Pre between the two groups, although this was not significantly different at 1m, 3y, and at the last visit (p = 0.039, p = not a number, p > 0.999, and p > 0.999, respectively). Visual field MD was not significantly different between the two groups within 1 year after treatment and at the last visit (p = 0.875 and p = 0.875, respectively; Table 1).
Discussion
In this longitudinal study, immediate phacoemulsification as a primary treatment for APAC led to visual improvement, good IOP control with prevention of visual field deterioration, and protection of the number of CECs, and phacoemulsification for the fellow eyes led to prevention of APAC development, good IOP control with prevention of visual field deterioration, and protection of the number of CECs over an extended period of time.
A few randomized control trials (RCTs) with more than 1 year of follow-up have reported on the clinical course after primary phacoemulsification without LPI.4,5,7 To the best of our knowledge, a 3-year follow-up period has been the longest follow-up period after primary phacoemulsification for APAC reported to date.7 Although our study was retrospective, no previous study has reported on the effect of primary phacoemulsification for APAC eyes and their fellow eyes in a case series with a mean follow-up period exceeding 5 years.
In addition, in terms of preoperative conditions, previous reports of long-term results on primary phacoemulsification for APAC differ from those of our study. All patients were medicated before phacoemulsification, the mean preoperative IOP was approximately 30 mmHg9 or less,4 or had their APAC resolved by medication before phacoemulsification.5
A previous review also compared APAC’s clinical course of phacoemulsification and LPI. Despite the surgical difficulty, phacoemulsification has been reported to be a better treatment option than LPI in terms of long-term IOP control and cost (Table 3); however, the appropriate timing for surgery remains unknown.10
 |
Table 3 Comparison Between Previous Reports About Phaco/IOL and Our Study |
The time from APAC onset to phacoemulsification in the previous studies ranged from approximately 0.1 to 10 days.3–6 In our study, the average time from APAC onset to phacoemulsification was approximately 2 days, and reoperation was not necessary until at least 3 years after surgery. Although the appropriate timing for phacoemulsification for APAC remains unknown,11 considering previous reports3–6 and the results of our study, phacoemulsification performed within 1–2 days can prevent irreversible Schlemm’s canal endothelial damage,12 Schlemm’s canal occlusion, and trabecular meshwork damage, and provide reasonable long-term IOP control. Therefore, we obtained an excellent clinical course of long-term IOP control and prevented the progression of glaucomatous visual field defects in APAC eyes as well as fellow eyes.
Many problems related to LPI have been reported. LPI can cause corneal endothelial damage.13,14 Between 1999 and 2001, bullous keratopathy (BK) related to LPI was the second most common form of BK, accounting for 23.4% of BK cases requiring total keratoplasties in Japan.15 The range of PAS increased after LPI for APAC.16 LPI tends to result in a long-term re-elevation of IOP, often requiring medications or reoperation to regulate the IOP,17–19 and can also cause long-term glaucomatous optic neuropathy.20 In addition, unoperated cataracts cause a decrease in visual acuity.20
One previous report had a similar study design to that of the present study and compared the 1-year follow-up period after phacoemulsification for eyes with APAC and fellow eyes.21 The main difference between our study and this previous report is that LPI was performed before phacoemulsification in all cases, and the time from APAC onset to phacoemulsification was longer than that in our study. In this previous report, the mean time from onset of APAC to phacoemulsification was 1.78 ± 1.5 weeks, and the mean time for fellow eyes was 3.5 ± 2.1 weeks, which were longer than these periods in our study. All eyes with APAC underwent LPI within a few days from onset, and the fellow eyes also underwent LPI before surgery, whereas the eyes in our study did not undergo LPI. They stated that a higher preoperative IOP resulted in a worse postoperative IOP control. They also stated that APAC eyes showed greater progression of visual field impairment than did the fellow eyes. Although the preoperative IOP of APAC eyes in our study was higher than that in the previous study, the APAC eyes achieved good postoperative IOP control, which was lower than 21 mmHg, and no worsening of visual field impairment was observed during the longer follow-up period. This may be attributed to the difference in the time from the onset of APAC to phacoemulsification, which is thought to be related to irreversible obstruction or damage to Schlemm’s canal11 and the trabecular meshwork, or because of the extent of PAS after LPI.15
In our study, although the surgery time in the APAC eyes was longer than that in the fellow eyes due to surgical difficulty, both groups achieved safe surgery, good BCVA, good IOP control, and prevention of visual field deterioration, without reoperation.
In our study, phacoemulsification was performed for the fellow eyes with shallow anterior chamber to prevent APAC development and achieved good clinical outcome. The previous report22 showed that phacoemulsification for primary angle closure disease, including primary angle closure glaucoma, primary angle closure, and primary angle closure suspect (PACS), had a long-term (>10 years) effect on IOP reduction. In fact, at 1 month after surgery, IOP was significantly lower than that before surgery in the fellow eye. Our study supports the positive effect of phacoemulsification for PACS.
This study had a number of limitations. A major limitation is that the current study was a retrospective, observational, small case series study. Moreover, two surgeons performed the phacoemulsification. Therefore, performance bias could affect internal validity in our study. Additionally, comparisons with other therapies, such as LPI, were not carried out. Furthermore, accurate measurement of the preoperative and postoperative PAS range and the impact of GSL were not possible because of perioperative corneal edema or the patients’ complaints, such as headache or nausea. Damage to the visual field and the optic nerve fiber layer was not thoroughly assessed before and after surgery. Additional RCTs are required to assess long-term surgical outcomes in a larger patient population.
Conclusion
This study revealed that in the long-term, immediate primary phacoemulsification for APAC eyes and phacoemulsification for the fellow eyes to prevent APAC development resulted in good visual improvement, protection of corneal endothelial cells, and good IOP control, with prevention of the visual field deterioration, although comparisons with LPI were not carried out.
Data Sharing Statement
The data presented in this study are available upon request from the corresponding author.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Shinseikai Toyama Hospital (approval number 230123-2; January 26, 2023).
Informed Consent Statement
The need to obtain informed patient consent was waived by the institutional review board of Shinseikai Toyama Hospital due to the retrospective nature of the study and the use of an opt-out consent process.
Acknowledgments
We would like to thank Editage for the English language editing. We would like to thank Yohei Hashimoto for collaboration on the statistical analysis.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study received no external funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
2. Burton MJ, Ramke J, Marques AP, et al. The lancet global health commission on global eye health: vision beyond 2020. Lancet Glob Health. 2021;9(4):e489–e551. doi:10.1016/S2214-109X(20)30488-5
3. Jacobi PC, Dietlein TS, Lüke C, Engels B, Krieglstein GK. Primary phacoemulsification and intraocular lens implantation for acute angle-closure glaucoma. Ophthalmology. 2002;109(9):1597–1603. doi:10.1016/s0161-6420(02)01123-5
4. Husain R, Gazzard G, Aung T, et al. Initial management of acute primary angle closure: a randomized trial comparing phacoemulsification with laser peripheral iridotomy. Ophthalmology. 2012;119(11):2274–2281. doi:10.1016/j.ophtha.2012.06.015
5. Lam DS, Leung DY, Tham CC, et al. Randomized trial of early phacoemulsification versus peripheral iridotomy to prevent intraocular pressure rise after acute primary angle closure. Ophthalmology. 2008;115(7):1134–1140. doi:10.1016/j.ophtha.2007.10.033
6. Imaizumi M, Takaki Y, Yamashita H. Phacoemulsification and intraocular lens implantation for acute angle closure not treated or previously treated by laser iridotomy. J Cataract Refract Surg. 2006;32(1):85–90. doi:10.1016/j.jcrs.2005.11.014
7. Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–46. doi:10.1097/00001648-199001000-00010
8. Belovay GW, Varma DK, Ahmed II. Cataract surgery in pseudoexfoliation syndrome. Curr Opin Ophthalmol. 2010;21(1):25–34. doi:10.1097/icu.0b013e328332f814
9. Azuara-Blanco A, Burr J, Ramsay C, et al. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet. 2016;388(10052):1389–1397. doi:10.1016/S0140-6736(16)30956-4
10. Chan PP, Pang JC, Tham CC. Acute primary angle closure-treatment strategies, evidences and economical considerations. Eye. 2019;33(1):110–119. doi:10.1038/s41433-018-0278-x
11. Wang N, Jia SB. Phacoemulsification with or without goniosynechialysis for angle-closure glaucoma: a global Meta-analysis based on randomized controlled trials. Int J Ophthalmol. 2019;12(5):826–833. doi:10.18240/ijo.2019.05.20
12. Hamanaka T, Kasahara K, Takemura T. Histopathology of the trabecular meshwork and Schlemm’s canal in primary angle-closure glaucoma. Invest Ophthalmol Vis Sci. 2011;52(12):8849–8861. doi:10.1167/iovs.11-7591
13. Lam DS, Lai JS, Tham CC, Chua JK, Poon AS. Argon laser peripheral iridoplasty versus conventional systemic medical therapy in treatment of acute primary angle-closure glaucoma: a prospective, randomized, controlled trial. Ophthalmology. 2002;109(9):1591–1596. doi:10.1016/s0161-6420(02)01158-2
14. Lai JS, Tham CC, Chua JK, et al. To compare argon laser peripheral iridoplasty (ALPI) against systemic medications in treatment of acute primary angle-closure: mid-term results. Eye. 2006;20(3):309–314. doi:10.1038/sj.eye.6701867
15. Shimazaki J, Amano S, Uno T, Maeda N, Yokoi N; Japan Bullous Keratopathy Study Group. National survey on bullous keratopathy in Japan. Cornea. 2007;26(3):274–278. doi:10.1097/ICO.0b013e31802c9e19
16. Moghimi S, Hashemian H, Chen R, Johari M, Mohammadi M, Lin SC. Early phacoemulsification in patients with acute primary angle closure. J Curr Ophthalmol. 2015;27(3–4):70–75. doi:10.1016/j.joco.2015.12.001
17. Aung T, Ang LP, Chan SP, Chew PT. Acute primary angle-closure: long-term intraocular pressure outcome in Asian eyes. Am J Ophthalmol. 2001;131(1):7–12. doi:10.1016/s0002-9394(00)00621-8
18. Lim LS, Aung T, Husain R, Wu YJ, Gazzard G, Seah SK. Acute primary angle closure: configuration of the drainage angle in the first year after laser peripheral iridotomy. Ophthalmology. 2004;111(8):1470–1474. doi:10.1016/j.ophtha.2004.01.036
19. Choong YF, Irfan S, Menage MJ. Acute angle closure glaucoma: an evaluation of a protocol for acute treatment. Eye. 1999;13(5):613–616. doi:10.1038/eye.1999.168
20. Aung T, Friedman DS, Chew PT, et al. Long-term outcomes in Asians after acute primary angle closure. Ophthalmology. 2004;111(8):1464–1469. doi:10.1016/j.ophtha.2003.12.061
21. Baek SU, Kim KH, Lee JY, Lee KW. Long-term intraocular pressure elevation after primary angle closure treated with early phacoemulsification. Korean J Ophthalmol. 2018;32(2):108–115. doi:10.3341/kjo.2017.0077
22. Sakai D, Yamamoto S, Yoshimizu S, et al. Ten-year outcomes of cataract surgery for glaucoma management in patients with primary angle-closure disease. Jpn J Ophthalmol. 2022;67(2):129–137. doi:10.1007/s10384-022-00971-8
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



