Back to Journals » Infection and Drug Resistance » Volume 15
The Utility of Nonroutine Intraocular Fluid Polymerase Chain Reaction for Uveitis in Indonesia
Authors Putera I, Riasanti M, Edwar L, Susiyanti M, Sitompul R, Aziza Y, Jessica P, Rukmana A, Yasmon A, La Distia Nora R
Received 25 January 2022
Accepted for publication 15 March 2022
Published 23 March 2022 Volume 2022:15 Pages 1219—1224
DOI https://doi.org/10.2147/IDR.S356030
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Ikhwanuliman Putera,1,2 Mei Riasanti,1 Lukman Edwar,1 Made Susiyanti,1 Ratna Sitompul,1 Yulia Aziza,1 Priscilla Jessica,1 Andriansjah Rukmana,3 Andi Yasmon,3 Rina La Distia Nora1,2,4
1Department of Ophthalmology, Faculty of MedicineUniversitas Indonesia – Cipto Mangunkusumo Kirana Eye Hospital, Jakarta, Indonesia; 2Department of Immunology, Erasmus Medical Center, Rotterdam, the Netherlands; 3Department of Microbiology, Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia; 4University of Indonesia Hospital (RSUI), Depok, West Java, Indonesia
Correspondence: Rina La Distia Nora, Department of Ophthalmology, Faculty of Medicine Universitas Indonesia – Cipto Mangunkusumo Kirana Eye Hospital, Jl. Kimia No. 8, Menteng, Central Jakarta, Jakarta, 10320, Indonesia, Tel +62811198910, Email [email protected]
Purpose: To investigate the utility of nonroutine polymerase chain reaction analysis of intraocular fluid to guide the diagnosis of infectious uveitis.
Patients and Methods: A retrospective cohort study was conducted by reviewing medical record data from intraocular fluid samples of uveitis patients who underwent single-plex real-time polymerase chain reaction analysis at the Department of Ophthalmology, Faculty of Medicine, Universitas Indonesia – Cipto Mangunkusumo Kirana Eye Hospital between January 2014 and December 2018.
Results: The positivity rate of nonroutine polymerase chain reaction analysis was 17.2%. The vitreous sample tended to show a higher positive outcome (28.6%) than the aqueous sample (16.2%), even though the outcome was not statistically significant. Mycobacterium tuberculosis and Toxoplasma gondii were the most frequently observed microorganisms in the polymerase chain reaction analysis among uveitis patients in our setting. The duration of symptoms, type of sample fluid (aqueous/vitreous), or presence of anterior chamber cells ≥ 2 were not significantly associated with polymerase chain reaction positivity (p > 0.05).
Conclusion: Nonroutine polymerase chain reaction analysis of intraocular fluid among a cohort of Indonesian patients demonstrated low positivity. The sensitivity and specificity of nonroutine single-plex polymerase chain reaction could not be estimated due to limitations such as lost to follow-up patients and incomplete monitoring data. The use of multiplex polymerase chain reaction in the future may be beneficial in our setting.
Keywords: aqueous humor, vitreous humor, infection, ocular inflammation, Mycobacterium tuberculosis, epidemiology
Introduction
Uveitis is a sight-threatening ocular inflammation with both infectious or non-infectious etiology. Infectious uveitis accounts for a higher proportion (often up to 50%) of uveitis cases in developing countries than in developed countries.1,2 Further, the causative organism varies by geographic location. In addition to Toxoplasma gondii (46%), the herpes simplex (HSV; 24%) and varicella-zoster (VZV; 30%) viruses were identified as the most frequent agents in the United States.3 A Thai study revealed that cytomegalovirus (CMV) was dominant because of a high proportion of anterior uveitis patients.4 In contrast, our previous report of a one-year study revealed that one-third of uveitis cases were classified as infectious uveitis with T. gondii and Mycobacterium tuberculosis as the common causes based primarily on corroborative evidence or clinical diagnosis.5
The diagnosis of infectious uveitis is typically based on clinical pattern recognition, and outcome depends on the appropriateness of the antimicrobial or antiviral treatment administered. Polymerase chain reaction (PCR) from intraocular aqueous or vitreous humor fluid samples is considered an adjunct modality to confirm an uncertain diagnosis.6 Even though a previous study has proposed that routine intraocular fluid PCR in suspected cases of infectious uveitis is beneficial because a clinical phenotype alone may be insufficient,7 not all facilities can provide this examination. In Indonesia, intraocular fluid PCR is not included in the national health service payment scheme, thus limiting its use in selected cases because many patients cannot afford the procedure. Given a lack of previously published data from Indonesia that specifically address the utility of PCR in infectious uveitis, this study aims to present results of intraocular fluid PCR analysis conducted in our center over five years.
Patients and Methods
Records of patients who underwent PCR testing of intraocular fluids (vitreous or aqueous) for suspected infectious uveitis at the Department of Ophthalmology, Faculty of Medicine, Universitas Indonesia - Cipto Mangunkusumo Kirana Eye Hospital between January 1st, 2014 and December 31st, 2018 were retrospectively reviewed. Cipto Mangunkusumo Kirana Eye Hospital is a government tertiary-care eye institution located in Jakarta. All patients with uveitis had undergone a tailored diagnostic work-up that included chest X-ray and various laboratory tests. Anatomical involvement was determined according to the Standardization of Uveitis Nomenclature system.8 Intraocular fluid PCR was performed in patients with active uveitis at presentation. The standard ocular PCR in our center is real-time probe-based, with a testing price range of Rp 500,000 to 700,000 (US $35–50) per pathogen. The pathogen tested was based on the clinical judgment of the attending ophthalmologist, as discussed with the patient. We prioritized patients with atypical presentation or recurrent uveitis with suspicion of infection for intraocular fluid PCR. In some patients, real-time PCR was performed as a part of another study, and thus the cost was covered by our institution.
Aqueous humor tap was performed in a procedural room. In the case of bilateral involvement, the eye with more severe inflammation based on presenting anterior chamber cells was chosen. Roughly 0.2 mL of aqueous sample was obtained using a 30-gauge needle on a 1 mL syringe while administering tetracaine topical anesthesia and topical 5% povidone-iodine solution. A solution containing hexamidine diisethionate 0.05% was used as another option for ocular surface disinfection.9 A vitreous sample was considered if the patient planned to undergo diagnostic vitrectomy in the operating theatre. Samples were transported immediately to the diagnostic laboratory (Department of Microbiology, Faculty of Medicine, Universitas Indonesia – Cipto Mangunkusumo General Hospital) within four hours.
DNA/RNA extraction of the aqueous or vitreous humor was then immediately initiated. The extraction was performed with the QIAamp DNA Mini Kit (Qiagen, Cat. No: 51304) or QIAamp Viral RNA Kit (Qiagen, Cat. No: 52904) according to the manufacturer’s protocol with final elution of 40 µL (DNA) and 60 µL (RNA), and was stored at −80°C for not more than 48 hours. The elution was used as a template for single-plex real-time PCR targeted to each Mycobacterium tuberculosis (primer: forward 5’- CCT GCG AGC GTA GGC GTC GG-3’, reverse 5’- CTC GTC CAG CGC CGC TTC GG - 3’), Toxoplasma gondii (primer: forward 5’- CTA GTA TCG TGC CGC AAT GTG - 3’, reverse 5’- GGC AGC GTC TCT TCC TCT TTT - 3’; probe: 5’-FAM-CCA-CCT-CGC-CTC-TTG-G-3’), CMV (primer: forward 5’- CAT GAA GGT CTT TGC CCA GTA C - 3’, reverse 5’- GGC CAA AGT GTA GGC TAC AAT AG - 3; probe: 5’-TGG CCC GTA GGT CAT CCA CAC TAG G-3’), HSV (primer: forward 5’- CCG TCA GCA CCT TCA TCG A - 3’, reverse 5’- CGC TGG ACC TCC GTG TAG TC - 3’; probe: 5’- CCA CGA GAT CAA GGA CAG CGG CC −3’), VZV (primer: forward 5’- TCT TTC ACG GAG GCA AAC AC −3’, reverse 5’- TCC AAG GCG GGT GCA TAT CT - 3’; probe: 5’-FAM-TAA CGT GGC TCG AGA ACG GTT TGG GTT T-3’), EBV (primer: forward 5’- CGG AAG CCC TCT GGA CTT C - 3’, reverse 5’- CCC TGT TTA TCC GAT GGA ATG - 3’; probe: 5’-TGT ACA CGC ACG AGA AAT GCG CC-3’), and Rubella (primer: forward 5’- CCT AHY CCC ATG GAG AAA CTC CT - 3’, reverse 5’- AAC ATC GCG CAC TTC CCA - 3’; probe: 5’- CCG TCG GCA GTT GG −3’). The PCR reaction mix was prepared according to the manufacturer’s instructions for each pathogen. In addition, a negative control with nucleic acid-free water was applied. A PCR result with cycle quantification < 40 was considered positive.
Results
Patient Characteristics
The medical records of 87 patients suspected of having infectious uveitis based on intraocular fluid PCR analysis were included. The proportion of patients with anterior, intermediate, posterior, and panuveitis was 12.6% (11), 3.4% (3), 39.1% (34), and 44.8% (39), respectively. Forty-two patients (48.3%) had visual acuity hand movement or worse, with 22 patients (out of 42; 52.4%) and 13 patients (out of 42; 31.0%) diagnosed with panuveitis and posterior uveitis, respectively. Positive test results were obtained in 15 patients (17.2%). Detailed patient characteristics are provided in Table 1. Among seven HIV-positive patients, only one had a positive PCR test. This was a 54-year-old male with bilateral panuveitis with exudative retinal detachment and a positive result for T. gondii. In addition, one non-HIV patient with posterior uveitis tested positive for both T. gondii and VZV.
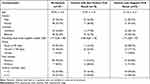 |
Table 1 Characteristics of Patients |
PCR Results
Overall, M. tuberculosis was the most-ordered PCR test, and five patients (6.9%) were positive for this agent. None of the samples showed a positive result for the Epstein-Barr virus (EBV). The percentage of PCR positivity for each microorganism is displayed in Table 2. Duration of symptoms, sample type (aqueous/vitreous), or the presence of anterior chamber cells ≥ 2+ were not significantly associated with PCR positivity (p > 0.05). Among the 15 patients with at least one pathogen identified with PCR, six (40%), six (40%), and three (20%) patients had posterior uveitis, panuveitis, and anterior uveitis, respectively. Finally, positive PCR results from 10/12 (83.33%) patients with panuveitis or posterior uveitis were based on aqueous humor analysis (Table 3).
 |
Table 2 Positivity of Intraocular PCR Based on Microorganism and Anatomical Involvement |
 |
Table 3 Positivity of Intraocular PCR Based on Anatomical Involvement and Fluid Sample Type |
Discussion
In general, the intraocular fluid PCR positivity rate that we observed is considered low. Nonroutine intraocular fluid PCR analysis in uveitis yielded 17.2% positivity in our population. Interestingly, analysis from the vitreous sample showed higher positivity (28.6%) compared to the aqueous sample (16.2%), even though the difference was not statistically significant. This finding is consistent with Dos Santos et al’s observation that a higher number of positive vitreous samples detected and identified infectious agents compared to aqueous humor samples.10 However, a multiple regression analysis by Balne et al revealed no significant association between positive PCR outcome and the type of sample (aqueous/vitreous) used.11 Another interesting study finding is that even in cases of posterior uveitis, aqueous fluid (17.2% positivity) analysis was still representative for diagnosing intraocular infection (compared to 20% positivity in vitreous fluid analysis). However, the positivity of vitreous fluid samples (50%) was considerably higher compared to aqueous samples (13.5%) in the context of panuveitis cases (Table 3). This finding is in line with a previous study that corroborates the usefulness of initial aqueous humor analysis in posterior uveitis,12 and with Oahalou et al finding that panuveitis and posterior uveitis were associated with an increased diagnostic yield of pars plana vitrectomy.13
M. tuberculosis and T. gondii were significant causative pathogens in our setting, especially in patients with atypical presentation. This may be attributed to the high proportion of patients with posterior uveitis or panuveitis. Our finding is consistent with results from our previous cohort, which indicated that 68% and 20% of all infectious uveitis was caused by toxoplasmosis and tuberculosis, respectively.5 The percentage of M. tuberculosis detected in vitreous analysis in our study (16.67%; 1/6) was higher than that found in aqueous analysis (6.1%; 4/66). This finding may be due to the microorganism’s localization in retinal pigment epithelium (RPE).14 Thus, the vitreous humor, which is anatomically closer to RPE than the aqueous humor, yielded more positive results. However, in the context of T. gondii, our study found positive results only in aqueous samples (3/33; 9.1% versus 0/4; 0% in vitreous samples). Although the previous study showed that parasites were more localized in the inner layers of the retina—mainly in the posterior pole of the eye15—and the DNA burden in the aqueous humor was considered low,16 Matos et al also revealed that PCR examination using the aqueous humor was precise in ocular toxoplasmosis, with a sensitivity of 75%.17
We found that the highest proportion of patients undergoing intraocular PCR analysis had panuveitis. As the ocular condition worsened, clinical pattern recognition alone was insufficient to guide appropriate diagnosis in significant panuveitis patients with visual acuity equal or worse than hand movement. In the Indonesian population, toxoplasmosis should be considered as a cause of atypical posterior uveitis or panuveitis.18 However, the timing of PCR analysis appeared to significantly affect the positivity of T. gondii PCR. De Groot-Mijnes et al observed that the positivity of T. gondii declined if samples were collected and analyzed at four weeks after onset. The authors observed that at a later time, the Goldmann–Witmer coefficient (GWC) was more accurate for guiding ocular toxoplasmosis diagnosis.19 Unfortunately, GWC examination is not available in our center, and patients inconclusive after PCR analysis could not be confirmed with the disease.
Geographical variation can also influence the causative pathogen of infectious uveitis. Given the continuing lack of consensus on when to perform intraocular PCR, our study setting is different than one in which intraocular PCR is routinely performed. Pathanapitoon et al’s study in the Thai population reported intraocular PCR positivity of 33%, nearly double that in our study. This may be due to a higher number of patients with anterior uveitis (41%) with positive CMV and to the routine performance of PCR in patients with an inconclusive initial work-up.4 In Africa, the positivity of intraocular PCR in suspected infectious posterior uveitis cases was roughly 16%, in line with our findings.7
As our study reported the PCR outcome on a nonroutine basis, the selection of the pathogen under examination may have affected the positivity rate of our result. In addition to the judgment of the attending ophthalmologist, patients’ ability to pay for PCR analysis determined the type and number of pathogen examined. In other words, the greater the number of pathogens examined, the higher the cost. Further, we could not compare the result of these PCR findings with the treatment response of individual patients. The study was also limited by loss to follow-up and incomplete monitoring data. Thus, sensitivity and specificity could not be estimated. Given our finding, the use of multiplex PCR in the future may be beneficial in our setting. Furthermore, we suggest conducting a robust prospective study for a comparative outcome evaluation—with a focus on cost-effectiveness in our population—with and without intraocular fluid PCR analysis in patients with suspected infection. Further studies to elucidate the diagnostic value of multiplex PCR and of affordable and accessible examinations to detect the causative pathogen of suspected infectious uveitis—together with their related clinical manifestations and treatment response—appear to be warranted in our setting.
Conclusion
Nonroutine PCR analysis of intraocular fluids from an Indonesian cohort demonstrated low positivity. The two most common causative microorganisms in infectious uveitis were M. tuberculosis and T. gondii. The sensitivity and specificity of nonroutine single-plex PCR could not be estimated due to limitations such as lost to follow-up patients and incomplete monitoring data. The use of multiplex PCR to detect the etiology of suspected infectious uveitis may be beneficial in our setting.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author, [RLDN]. Due to the privacy of research participants, names of individuals will be provided in the form of initials, and medical record numbers will not be provided.
Ethics Statement
Ethical approval was waived by the local Ethics Committee of the Faculty of Medicine, Universitas Indonesia – Cipto Mangunkusumo Hospital, Jakarta, Indonesia in view of the retrospective nature of the study, and all procedures performed were part of routine care.
Acknowledgments
We thank Gloria P. Usodo, MD, for her help in reviewing the patient medical records.
Author Contributions
All authors contributed to the study conception and design. Material preparation, acquisition of data and analysis were performed by Ikhwanuliman Putera, Rina La Distia Nora, and Priscilla Jessica. Clinical data were interpreted by Ikhwanuliman Putera, Lukman Edwar, Made Susiyanti, Ratna Sitompul, Yulia Aziza, and Rina La Distia Nora. PCR results were interpreted by Mei Riasanti, Andriansjah Rukmana, and Andi Yasmon. Final data interpretation and analysis were performed by all authors. The first draft and revised version of the manuscript were written by Ikhwanuliman Putera and Priscilla Jessica. All authors reviewed, revised, and approved all versions of the article before first submission and before re-submission of the revised manuscript. All authors agreed to submit the article to Infection and Drug Resistance. All authors agreed to take responsibility and be accountable for the contents of the article.
Funding
This study was supported by Riset Inovatif Produktif - Lembaga Pengelola Dana Pendidikan (RISPRO LPDP) [grant number RISPRO/KI/B1/KOM/5/15219/4/2020]. The funding source had no involvement in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the article for publication.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tsirouki T, Dastiridou A, Symeonidis C, et al. A focus on the epidemiology of uveitis. Ocul Immunol Inflamm. 2018;26:2–16. doi:10.1080/09273948.2016.1196713
2. Majumder PD, Ghosh A, Biswas J. Infectious uveitis: an enigma. Middle East Afr J Ophthalmol. 2017;24:2–10. doi:10.4103/meajo.MEAJO_252_16
3. De Groot-mijnes JDF, Rothova A, Van Loon AM, et al. Polymerase chain reaction and Goldmann-Witmer coefficient analysis are complimentary for the diagnosis of infectious uveitis. Am J Ophthalmol. 2006;141:313–318. doi:10.1016/j.ajo.2005.09.017
4. Pathanapitoon K, Kongyai N, Sirirungsi W, et al. The diagnostic value of intraocular fluid analysis by polymerase chain reaction in Thai patients with uveitis. Trans R Soc Trop Med Hyg. 2011;105:650–654. doi:10.1016/j.trstmh.2011.08.003
5. La Distia Nora R, Sitompul R, Bakker M, et al. Tuberculosis and other causes of uveitis in Indonesia. Eye. 2018;32:546–554. doi:10.1038/eye.2017.231
6. Chronopoulos A, Roquelaure D, Souteyrand G, et al. Aqueous humor polymerase chain reaction in uveitis - utility and safety. BMC Ophthalmol. 2016;16:1–7. doi:10.1186/s12886-016-0369-z
7. Scheepers MA, Lecuona KA, Rogers G, et al. The value of routine polymerase chain reaction analysis of intraocular fluid specimens in the diagnosis of infectious posterior uveitis. Sci World J. 2013;2013:545149. doi:10.1155/2013/545149
8. Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–516. doi:10.1016/j.ajo.2005.03.057
9. Pinna A, Donadu MG, Usai D, et al. In vitro antimicrobial activity of a new ophthalmic solution containing hexamidine diisethionate 0.05% (keratosept). Cornea. 2020;39:1415–1418. doi:10.1097/ICO.0000000000002375
10. Dos Santos FF, Commodaro AG, De Souza AV, et al. Real-time PCR in infectious uveitis as an alternative diagnosis. Arq Bras Oftalmol. 2011;74:258–261. doi:10.1590/s0004-27492011000400006
11. Balne PK, Modi RR, Choudhury N, et al. Factors influencing polymerase chain reaction outcomes in patients with clinically suspected ocular tuberculosis. J Ophthalmic Inflamm Infect. 2014;4:1–6. doi:10.1186/1869-5760-4-10
12. Dos Santos HNV, Ferracioli-Oda E, Barbosa TS, et al. Usefulness of aqueous and vitreous humor analysis in infectious uveitis. Clinics. 2020;75:1–6. doi:10.6061/clinics/2020/e1498
13. Oahalou A, Schellekens PAWJF, De Groot-mijnes JD, et al. Diagnostic pars plana vitrectomy and aqueous analyses in patients with uveitis of unknown cause. Retina. 2014;34:108–114. doi:10.1097/IAE.0b013e31828e6985
14. Chalam KV, Gupta SK, Vinjamaram S, et al. Tuberculous uveitis: distribution of mycobacterium tuberculosis in the retinal pigment epithelium. Arch Ophthalmol. 2006;119:409–410.
15. Greigert V, Bittich-Fahmi F, Pfaff AW. Pathophysiology of ocular toxoplasmosis: facts and open questions. PLoS Negl Trop Dis. 2020;14:1–18. doi:10.1371/journal.pntd.0008905
16. Garweg JG, De Groot-Mijnes JDF, Montoya JG. Diagnostic approach to ocular toxoplasmosis. Ocul Immunol Inflamm. 2011;19:255–261. doi:10.3109/09273948.2011.595872
17. Matos K, Muccioli C, Belfort R, et al. Correlation between clinical diagnosis and PCR analysis of serum, aqueous, and vitreous samples in patients with inflammatory eye disease. Arq Bras Oftalmol. 2007;70:109–114. doi:10.1590/S0004-27492007000100020
18. Kurniawan A, Sari IP, Harminarti N, et al. Toxoplasma gondii SAG2 type III in an atypical presentation of ocular toxoplasmosis in Indonesia. Int J Infect Dis. 2020;96:440–444. doi:10.1016/j.ijid.2020.05.017
19. De Groot-Mijnes JDF, Rothova A, Van Loon AM, et al. Polymerase chain reaction and goldmann-witmer coefficient analysis are complimentary for the diagnosis of infectious uveitis. Am J Ophthalmol. 2006;141:313–318. doi:10.1016/j.ajo.2005.09.017
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
