Back to Journals » Therapeutics and Clinical Risk Management » Volume 18
The Use of Muscle Relaxants and Reversal Agents in a Setting Without Cost Restrictions: Experience from a Tertiary Academic Hospital in the Netherlands
Authors Martini CH, Honing GHM, Bash LD, Olofsen E, Niesters M, van Velzen M , Dahan A , Boon M
Received 30 November 2021
Accepted for publication 12 March 2022
Published 8 April 2022 Volume 2022:18 Pages 379—390
DOI https://doi.org/10.2147/TCRM.S350314
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Chris H Martini,1 GH Maarten Honing,1 Lori D Bash,2 Erik Olofsen,1 Marieke Niesters,1 Monique van Velzen,1 Albert Dahan,1 Martijn Boon1
1Department of Anesthesiology, Leiden University Medical Center, Leiden, the Netherlands; 2Center for Observational and Real- World Evidence (CORE), Merck & Co., Inc, Kenilworth, NJ, USA
Correspondence: Chris H Martini, Department of Anesthesiology, Leiden University Medical Center, Albinusdreef 2, Leiden, 2333, ZA, the Netherlands, Tel +31 71 526 2301, Email [email protected]
Introduction: Muscle relaxants are often given during general anesthesia to facilitate endotracheal intubation. However lingering effects after anesthesia-end may lead to respiratory compromise in the PACU. Strategies to reduce these adverse events include monitoring neuromuscular block, the use of short-acting agents and active pharmacological reversal before extubation. At Leiden University Medical Center (LUMC), a tertiary care academic hospital in the Netherlands, various muscle relaxants and reversal agents are freely available to all clinicians without restrictions. In this setting, we intended to evaluate how patient and surgical characteristics impacted the use of these agents for a variety of non-cardiac surgeries.
Material and Methods: This is a retrospective database study of adult patients that had received elective, non-cardiac surgery and general anesthesia with endotracheal intubation between 2016 and 2020 at LUMC in the Netherlands. Exclusion criteria consisted of patients pharmacologically reversed with both sugammadex and neostigmine during the same procedure, diagnosed with myasthenia gravis, receiving pyridostigmine therapy, or with renal failure (eGFR < 30 mL.min.1.73m2).
Results: We retrieved 23,373 patient records of which 9742 were excluded because one or more exclusion criteria were met. The final cohort consisted of 13,631 cases. Rocuronium was the most commonly used muscle relaxant (88.5%); sugammadex was the most commonly used reversal agent (99.9% of those pharmacologically reversed). Of all cases that received rocuronium as muscle relaxant, 76.9% of patients were not reversed, while 23.1% were reversed with sugammadex. The odds of reversal increased with age, BMI, ASA class (1– 3) and shorter duration of surgery.
Conclusion: In an unrestricted clinical environment, rocuronium and sugammadex are the preferred agents for muscle relaxation and reversal. Pharmacologic reversal of neuromuscular block was uncommon overall, but more likely in older and obese patients, higher ASA classification and shorter lasting procedures. Sugammadex has largely replaced neostigmine for this purpose.
Keywords: neuromuscular blockade, muscle relaxants, sugammadex
Introduction
Muscle relaxants are routinely used during general anesthesia to facilitate endotracheal intubation and to maintain optimal surgical working conditions.1,2 However, the relatively long half-life of (non-depolarizing) muscle relaxants, poses patients at risk for residual neuromuscular block (NMB) after extubation and in the post-operative care unit,3,4 which is associated with complications such as atelectasis, pneumonia, pulmonary failure, and reintubation.5,6 To prevent residual NMB, clinicians may pharmacologically reverse neuromuscular block just before the end of anesthesia. This was traditionally accomplished with an acetylcholinesterase inhibitor, however sugammadex, a selective amino-steroidal relaxant binding agent,7 is gaining popularity due to its ability to reliably reverse both shallow and deep levels of neuromuscular block in a shorter period of time.8 In addition, sugammadex is devoid of major side-effects and especially lack cholinergic complications that often accompany cholinesterase inhibitors. Despite these advantages, financial considerations may limit the unrestricted use of sugammadex in many hospitals, because of the higher cost-base compared to acetylcholinesterase inhibitors.9 Although there are indications that sugammadex reduces the incidence of postoperative residual NMB,10 and possibly lowers the incidence of respiratory complications,11,12 effects on these outcomes remain controversial.13,14 In addition, many national and international anesthesia associations lack guidelines on perioperative NMB management. As such, there exists a wide variation in practices with regard to NMB management and reversal strategies. The goal of the current study is to leverage inpatient electronic medical records to describe the incidence of NMB and reversal agent utilization and factors impacting the choice of NMB reversal among patients in the inpatient setting, and specifically, identify factors which distinguish patients who are pharmacologically reversed from those who are not actively reversed. To this end, we conducted a retrospective analysis of patient data in a tertiary academic center in the Netherlands where sugammadex has been freely available since 2013. We hypothesize that use of sugammadex is associated with shorter lasting procedures and with patient characteristics related to postoperative complications, such as older age, higher ASA class, and higher BMI.
Materials and Methods
This was a single-center, retrospective observational study using a local electronic database to describe and assess the use of muscle relaxants and reversal agents at the Leiden University Medical Center (LUMC) at Leiden, The Netherlands. In this center, clinicians may freely choose between a variety of muscle relaxants and between neostigmine or sugammadex as reversal agent. Prior to start of the current study, the study protocol was approved by the local research board in June 2020, and by Merck in October 2020. This study was approved by the institutional review board (IRB) of the Departments of Anesthesiology and Intensive Care of the LUMC in June 2020 and the requirement for patient consent was waived as this study involved analysis of preexisting, deidentified data collected for clinical and operational purposes. All patient-related study data was collected in compliance with the Dutch Act on GRDP (General Data Protection Regulation) of 2016. Final data analyses were performed in March 2021 (end of study).
Data Extraction
Data of patients that received anesthesia from April 2016 to December 2020 in LUMC were retrieved from our electronic medical record database (Healthcare Information X-change, HiX, Chipsoft, The Netherlands). Data extraction was performed by CM with the aid of a local database manager. The research team (CM/MB) manually checked and validated the data for inconsistencies and accuracy. Cases were eligible if they had received general anesthesia for any type of elective surgical procedure requiring endotracheal intubation in patients aged 18 years and older. Exclusion criteria consisted of patients pharmacologically reversed with both sugammadex and neostigmine during the same procedure, diagnosed with myasthenia gravis, receiving pyridostigmine therapy, or with renal failure (eGFR <30 mL/min/1.73m2).
From the data, active reversal with sugammadex and spontaneous recovery were identified and compared with each other with respect to (1) patient-related characteristics, including age, gender, height, weight, body mass index (BMI) and American Society of Anesthesiologists (ASA) physical status classification; and (2) anesthesia and surgery related characteristics, including anesthesia type, surgery type, duration of surgery and hospital length of stay.
Procedures without procedure code, diagnostic procedures and procedures with less than 100 cases per specialty were removed. Final analyses focused on rocuronium cases (88.5% of total) and ASA 1 to 4 patients (sixteen ASA 5 patients were excluded).
Statistics
The main endpoint of our study was the utilization of neuromuscular blockade and reversal agent incidence in our hospital and the description of patient and procedure related characteristics. No a priori power analysis was conducted given the retrospective and descriptive study design.
Neuromuscular Monitoring Data and Reversal
In our hospital neuromuscular monitoring is available in every OR. All staff are well trained in the correct use of the monitoring equipment. In the case of a train-of-four (TOF-) ratio below 90% of its baseline value at the end of the surgical procedure, clinicians can either wait for the TOF-ratio to reach the 90% threshold spontaneously, or administer a reversal agent. Unfortunately, the neuromuscular monitoring data is not automatically logged into the electronic medical record database in a standardized manner and we rely on the manual, textual insertion of the data by the employees. After evaluation of the data, it was not suitable to quantitatively analyze for research purposes.
Descriptive statistics were used to analyze the frequency of NMB utilization and reversal agent by patient characteristics (age, gender, height, weight, BMI, ASA class), and procedure type (specialty, anesthesia type, duration of surgery, hospital length of stay). Covariates for reversal strategy were analyzed by stepwise univariate and multivariate logistic regression. All analyses were performed using IBM SPSS (version 25, Armonk NY USA). P-values < 0.05 were considered statistically significant. Data are presented as mean ± Standard Deviation (SD), min, max unless otherwise stated.
Results
Our search yielded 23,373 cases that were treated with a neuromuscular blocking agent. 7939 cases had to be excluded for various reasons. The final cohort consisted of 13,631 cases. Figure 1 shows a flow chart of the data selection process. Rocuronium was the most commonly used muscle relaxant (88.5%), followed by succinylcholine (10.4%), atracurium (1%) and mivacurium (0.1%), see Table 1. Though pharmacologic reversal was uncommon (approximately 23% of patients), sugammadex was used as reversal agent in 99.9% of these cases; in only 12 cases neostigmine was used as reversal agent (data not shown).
 |
Table 1 NMB Utilization Over Time |
 |
Figure 1 Flowchart of included cases. |
For our primary analysis, we focused on the cases where rocuronium was used as muscle relaxant. In this cohort, the only one case that was reversed with neostigmine was excluded from the analyses. As such, patients in this cohort were either allowed to recover spontaneously or were pharmacologically reversed with sugammadex. For a distribution of active versus spontaneous reversal of rocuronium induced NMB over time, see Table 2. There is a gradual increase of sugammadex use over time, ranging from nearly 19% in 2016 to 26% in 2020.
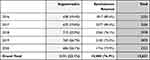 |
Table 2 Reversal of Rocuronium Induced NMB Over Time |
Table 3 displays the baseline characteristics of patients reversed with sugammadex versus spontaneous recovery of rocuronium induced NMB. Among all inpatients administered rocuronium in this period (N=13,631), patients were 55 years old on average, 55% were women, about a third underwent general surgery, with a median of 2 days in hospital stay. Nearly 15% of patients were missing ASA status, and nearly 44% were ASA 2.
 |  | 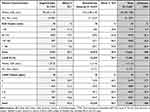 |
Table 3 Distribution of Patient Characteristics in Patients Reversed with Sugammadex versus Spontaneous Recovery of Rocuronium Induced Neuromuscular Block |
In this cohort, 77% were not pharmacologically reversed, while 23% had received at least one dose of sugammadex. The reversal percentage increased with increasing age (19.5% in patients 18–29 years old, to 27.3% in patients of 80+ years old); increasing ASA class from ASA 1 (18.4%) tot ASA 3 (30.6%) while patients of ASA class 4 (only 2.1% of the population) had a lower reversal rate (14.8%). Among patients that received inhalational (sevoflurane) anesthesia, 19.3% were reversed, compared to 24.3% of patients that had received total intravenous anesthesia. Procedures that were actively reversed were significantly shorter in duration compared to those which were spontaneously reversed (82 minutes versus 152 minutes respectively, p< 0.001). While overall, most procedures were not pharmacologically reversed, there was a wide range in reversal practice by surgery type (as often as 72% pharmacologically reversed among obstetrics, and as few as 3.6% reversed among endocrine procedures).
In the univariate logistic regression analysis, the following covariates yielded a higher probability of active reversal versus spontaneous recovery: older age (patient categories 70–79 and > 80 years were combined yielding a better fit of the logistic regression model), morbidly obese individuals (BMI > 35 kg.mg−2) and patient with underweight (BMI < 20 kg.m−2), ASA 2 (compared to ASA 1) and ASA 3 (compared to ASA 1 and 2), total intravenous anesthesia (TIVA), eye surgery, and shorter duration of surgery (Figure 2A). General surgery was used as reference category as it consisted of a large group of procedures (eg, endocrine, gastro-intestinal, trauma and vascular surgery) with an average reversal rate of 28% which was more or less similar to the population mean of 23%. In multivariate regression analysis the effects remained largely unchanged regarding direction and magnitude, except for anesthesia type (TIVA: univariate OR 1.27 versus multivariate OR 0.79, p=0.007) and eye surgery (univariate OR 1.31 vs multivariate OR 0.70, p=0.019). Other factors such as underweight, ASA class 1 and gynecologic procedures were not independently associated with reversal choices after adjusting for other perioperative characteristics. See Figure 2B and Table 4 for multivariate logistic regression results.
 |
Table 4 Characteristics of Multivariate Logistical Regression Analysis |
Discussion
This study presents data on the use of muscle relaxants and reversal agents in patients that received general anesthesia for a variety of non-cardiac surgical procedures that took place between 2016 and 2020 in a tertiary academic hospital in The Netherlands. In our hospital, sugammadex has been freely available since 2013 and choices regarding the use of muscle relaxants or reversal agents are not regulated (ie, are at the full discretion of the attending anesthesiologist). The data show that rocuronium was the preferred choice of muscle relaxant (88.5%) and sugammadex was the preferred reversal agent (99.9%). Of the patients that had received rocuronium, only 23% were actively reversed; the other 77% were allowed to recover spontaneously. Multivariate analysis showed that pharmacologic reversal was positively and independently associated with patients of advanced age (>70 years), ASA class 3 (compared to ASA 1 or 2) and elevated BMI >35 kg.m−2. In addition, anesthesia- and surgery related characteristics revealed a higher likelihood for reversal for shorter-lasting procedures, for cases that received sevoflurane anesthesia and for general surgery (compared to other types of surgery).
In our center, rocuronium was clearly the preferred muscle relaxant in daily practice. Rocuronium has a rapid onset and intermediate duration of action, which makes it suitable for many elective and emergency cases. Nevertheless, large inter-individual variation in duration mandates that clinicians monitor the level of NMB during anesthesia and decide on whether to pharmacologically reverse or not before the endotracheal tube is removed. Should residual NMB exist at this time, ie, the train-of-four (TOF-) ratio is below 90% of its baseline value, clinicians can either wait for the TOF-ratio to reach the 90% threshold spontaneously, or speed up the recovery by administering a reversal agent. The latter may be achieved with an acetylcholinesterase inhibitor, or sugammadex, in case an amino steroidal muscle relaxant such as rocuronium is used. Although both agents speed up the recovery of NMB, sugammadex, by directly encapsulating the muscle relaxant molecules, does this more predictably and effectively, with higher speed and without ceiling effect that limits the use of acetylcholinesterase inhibitors for reversal of deep NMB. Additionally, sugammadex has fewer side effects.15 However the higher cost-base may limit its use in settings where budgets are restricted. In our center, cost-implications of sugammadex do not restrict its clinical use. Therefore, we wished to study how this situation affects the use of muscle relaxants and reversal agents and what factors impacted these choices. Somewhat surprisingly, we observed in our population that in 77% of cases no reversal agent was used. This contrasts with the previous reports from the USA and Europe, where active reversal was performed in 50 to 80% of cases.16,17 In addition, a time related decrease in spontaneous recovery was noted in USA based hospitals since the approval of sugammadex.16 Intuitively, the absence of reversal would increase the risk for postoperative residual neuromuscular block, especially when neuromuscular monitoring is not used appropriately, although current literature does not support this hypothesis.17,18 In our center, neuromuscular monitoring is freely available in every OR, and it is possible that reversal in many of our patients was deemed unnecessary, however we are not informed on the depth of neuromuscular block at extubation as these data are not automatically logged into our electronic health record. Nevertheless, those patients that were actively reversed included patients of higher ASA class, BMI and age, which are characteristics that are generally regarded to increase the risk for residual NMB. A similar pattern was observed in recent studies using data from large US healthcare databases.16,19,20 This suggests that clinicians are aware of the risk factors for residual NMB and make an individual-based decision on whether to reverse or not based on these, and possibly other, risk factors. Among all factors, awareness of the risk of residual NMB and sufficient knowledge and education on how to prevent this, is probably the most important factor in preventing residual NMB; failure to do so has been demonstrated to negatively impact incidence of residual NMB, even when neuromonitoring and reversal agents are used.17
Our data also show that, in the setting where sugammadex is freely available, clinicians prefer to use sugammadex over neostigmine as reversal agent. This is broadly consistent with other reports showing that the use of sugammadex in many countries increases with time after regulatory approval for clinical use and hospital access granted.19–21 In this respect, our center may have had a head start because approval of sugammadex was granted in 2008 in The Netherlands versus 2015 in the USA. This may in part explain why the use of sugammadex in our center is higher (among those pharmacologically reversed) than what is reported in USA derived data. However, despite early approval of sugammadex in our country and many other European countries, differences between centers within and between EU countries exist. For instance, data from the POPULAR study, which was a European multi-center study, showed that neostigmine was still used in the majority of cases (77.4%).17 Although time progression since the conclusion of that study may have led to an ongoing gradual decrease in neostigmine use since then, we believe that the time component alone does not fully explain the differences between the POPULAR data and our data. Specifically, in our hospital, a deep neuromuscular block is applied for robotic surgery, retroperitoneal surgery and intravitreal eye surgery. Incidentally, a deep NMB needs reversal with sugammadex at the conclusion of a procedure which may have contributed to higher sugammadex use in our center. Still, most procedures in our center receive a single shot of muscle relaxant at the induction of anesthesia. Therefore, we contend that the choice of the use sugammadex was not primarily based on the depth of block alone, but rather on the merits of sugammadex itself.
Our study has several limitations. First, clinical variables that were not available in our dataset (such as categorized patient medical history, history of coded previous surgeries, neuromonitoring data, etc.) may have had an undetermined impact on the decision to reverse or not reverse a patient. These may include details of the perioperative care (eg, dosing information of medication and fluids), provider bias, surgeon preference, patient anthropometric data (eg, habitus or smoking status) and previous patient clinical events. When looking at associations we must interpret the current findings with caution considering unmeasured confounding and the potential impact these variables may have had on observed effects.
Conclusion
In conclusion, this study assessed the use of neuromuscular blocking agents and reversal strategy during anesthesia in a tertiary academic hospital in the Netherlands with unrestricted access to sugammadex. Of the patients that had received rocuronium, only 23% were actively reversed overall, with sugammadex as the preferred reversal agent (99.9% of reversals). The decision to actively reverse NMB with sugammadex in our cohort depended on patient age, BMI, ASA state, type of anesthesia and type and duration of surgery.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Merck Sharp & Dohme Corp, a subsidiary of Merck & Co, Inc, Kenilworth, NJ. The sponsors collaborated with the investigators in the design of the study, and preparation of the manuscript. Sponsors had no access to patient level data and took no part in data analysis.
Disclosure
Lori D Bash is a full-time employee of Merck Sharp & Dohme Corp, a subsidiary of Merck & Co, Inc, Kenilworth, NJ, USA which manufactures and distributes sugammadex, and may own stock and/or hold stock options in Merck & Co., Inc., Kenilworth, NJ. Marieke Niesters reports grants from Grunenthal, outside the submitted work. Albert Dahan reports grants and/or personal fees from MSD, MEDTRONIC, Trevena, Grunenthal, Medasense, AMO Pharma, ZonMW, and FDA, outside the submitted work. Dr Martijn Boon reports grants from MSD, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality of tracheal intubation: a randomized controlled trial. Anesthesiology. 2003;98(5):1049–1056. doi:10.1097/00000542-200305000-00005
2. Martini CH, Boon M, Bevers RF, Aarts LP, Dahan A. Evaluation of surgical conditions during laparoscopic surgery in patients with moderate vs deep neuromuscular block. Br J Anaesth. 2014;112(3):498–505. doi:10.1093/bja/aet377
3. Hayes AH, Mirakhur RK, Breslin DS, Reid JE, McCourt KC. Postoperative residual block after intermediate-acting neuromuscular blocking drugs. Anaesthesia. 2001;56(4):312–318. doi:10.1046/j.1365-2044.2001.01921.x
4. Debaene B, Plaud B, Dilly MP, Donati F. Residual paralysis in the PACU after a single intubating dose of nondepolarizing muscle relaxant with an intermediate duration of action. Anesthesiology. 2003;98(5):1042–1048. doi:10.1097/00000542-200305000-00004
5. Berg H, Roed J, Viby-Mogensen J, et al. Residual neuromuscular block is a risk factor for postoperative pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand. 1997;41(9):1095–1103. doi:10.1111/j.1399-6576.1997.tb04851.x
6. Murphy GS, Szokol JW, Marymont JH, Greenberg SB, Avram MJ, Vender JS. Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesth Analg. 2008;107(1):130–137. doi:10.1213/ane.0b013e31816d1268
7. Bom A, Bradley M, Cameron K, et al. A novel concept of reversing neuromuscular block: chemical encapsulation of rocuronium bromide by a cyclodextrin-based synthetic host. Angew Chem Int Ed Engl. 2002;41(2):266–270. doi:10.1002/1521-3773(20020118)41:2<265::aid-anie265>3.0.co;2-q
8. Jones RK, Caldwell JE, Brull SJ, Soto RG. Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology. 2008;109(5):816–824. doi:10.1097/ALN.0b013e31818a3fee
9. Rao Kadam V, Howell S. Unrestricted and restricted access to sugammadex and side effect profile in a teaching hospital centre for year 2014- database audit study. Anesth Pain Med. 2018;8(1):e63066. doi:10.5812/aapm.63066
10. Brueckmann B, Sasaki N, Grobara P, et al. Effects of sugammadex on incidence of postoperative residual neuromuscular blockade: a randomized, controlled study. Br J Anaesth. 2015;115(5):743–751. doi:10.1093/bja/aev104
11. Krause M, McWilliams SK, Bullard KJ, et al. Neostigmine versus sugammadex for reversal of neuromuscular blockade and effects on reintubation for respiratory failure or newly initiated noninvasive ventilation: an interrupted time series design. Anesth Analg. 2020;131(1):141–151. doi:10.1213/ANE.0000000000004505
12. Kheterpal S, Vaughn MT, Dubovoy TZ, et al. Sugammadex versus neostigmine for reversal of neuromuscular blockade and postoperative pulmonary complications (STRONGER): a multicenter matched cohort analysis. Anesthesiology. 2020;132(6):1371–1381. doi:10.1097/ALN.0000000000003256
13. Togioka BM, Yanez D, Aziz MF, Higgins JR, Tekkali P, Treggiari MM. Randomised controlled trial of sugammadex or neostigmine for reversal of neuromuscular block on the incidence of pulmonary complications in older adults undergoing prolonged surgery. Br J Anaesth. 2020;124(5):553–561. doi:10.1016/j.bja.2020.01.016
14. Li G, Freundlich RE, Gupta RK, et al. Postoperative pulmonary complications’ association with sugammadex versus neostigmine: a retrospective registry analysis. Anesthesiology. 2021;134(6):862–873. doi:10.1097/ALN.0000000000003735
15. Hristovska AM, Duch P, Allingstrup M, Afshari A. Efficacy and safety of sugammadex versus neostigmine in reversing neuromuscular blockade in adults. Cochrane Database Syst Rev. 2017;8:CD012763. doi:10.1002/14651858.CD012763
16. Bash LD, Turzhitsky V, Black W, Urman RD. Neuromuscular blockade and reversal agent practice variability in the US inpatient surgical settings. Adv Ther. 2021;38(9):4736–4755. doi:10.1007/s12325-021-01835-2
17. Kirmeier E, Eriksson LI, Lewald H, et al. Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicentre, prospective observational study. Lancet Respir Med. 2019;7(2):129–140. doi:10.1016/S2213-2600(18)30294-7
18. Grosse-Sundrup M, Henneman JP, Sandberg WS, et al. Intermediate acting non-depolarizing neuromuscular blocking agents and risk of postoperative respiratory complications: prospective propensity score matched cohort study. BMJ. 2012;345:e6329. doi:10.1136/bmj.e6329
19. Dubovoy TZ, Saager L, Shah NJ, et al. Utilization patterns of perioperative neuromuscular blockade reversal in the United States: a retrospective observational study from the multicenter perioperative outcomes group. Anesth Analg. 2020;131(5):1510–1519. doi:10.1213/ANE.0000000000005080
20. Bash LD, Black W, Turzhitsky V, Urman RD. Neuromuscular blockade and reversal practice variability in the outpatient setting: insights from US utilization patterns. Anesth Analg. 2021;133(6):1437–1450. doi:10.1213/ANE.0000000000005657
21. Ledowski T, Hillyard S, Kozman A, et al. Unrestricted access to sugammadex: impact on neuromuscular blocking agent choice, reversal practice and associated healthcare costs. Anaesth Intensive Care. 2012;40(2):340–343. doi:10.1177/0310057X1204000219
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

