Back to Journals » Journal of Asthma and Allergy » Volume 10
The US Food and Drug Administration’s drug safety recommendations and long-acting beta2-agonist dispensing pattern changes in adult asthma patients: 2003–2012
Authors Zhou EH, Seymour S, Goulding MR , Kang EM, Major JM, Iyasu S
Received 11 October 2016
Accepted for publication 23 December 2016
Published 16 March 2017 Volume 2017:10 Pages 67—74
DOI https://doi.org/10.2147/JAA.S124395
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Esther H Zhou,1 Sally Seymour,2 Margie R Goulding,1 Elizabeth M Kang,1 Jacqueline M Major,1 Solomon Iyasu1
1Division of Epidemiology, Office of Surveillance and Epidemiology, 2Office of New Drugs, Center for Drug Evaluation and Research, US Food and Drug Administration, Silver Spring, MD, USA
Background: Emerging safety issues associated with long-acting beta2-agonist (LABA) have led to multiple regulatory activities by the US Food and Drug Administration (FDA) since 2003, including Drug Safety Communications (DSCs) in 2010. These DSCs had three specific recommendations for the safe use of LABA products in adult asthma treatment.
Methods: We examined the initiation of LABA-containing products for adult asthma treatment using an intermittent time series approach in a claims database from 2003 to 2012. We assessed the alignment of dispensing patterns with the following 2010 FDA recommendations: 1) contraindicated use of single-ingredient (SI)-LABA without an asthma controller medication (ACM); 2) a LABA should only be used when asthma is not adequately controlled on inhaled corticosteroids (ICSs) or ACM; and 3) step-down asthma therapy (e.g., discontinue LABA) when asthma control is achieved.
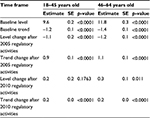
Results: There were 477,922 adults (18–64 years old) dispensed a new LABA during 2003–2012. Among LABA initiators, patients who initiated an SI-LABA and who did “not” have an ACM dispensed on the same date decreased from >9% in 2003 (the initial labeling change) to <2% post 2010 DSCs (p-value <0.0001 in the segmented regression model). The proportion of asthma patients dispensed an ICS in 6 months prior to initiating LABA treatment did not increase. The proportion of patients with longer than 4 months of continuous treatment did not decrease over the study period.
Conclusion: Although the decrease in SI-LABA initiation is consistent with FDA’s recommendations, low ICS dispensing before initiating a LABA and LABA continuation practices require further efforts to move toward the recommended safe practices.
Keywords: LABA, dispensing pattern, US FDA, regulatory activities
Introduction
Asthma, a chronic inflammatory respiratory disease, is highly prevalent in the US and associated with major health burden worldwide. The goal of therapy is to achieve long-term control of asthma symptoms while minimizing treatment side effects. Current guidelines recommend a stepwise approach to pharmacologic therapy with several classes of medications in which treatment is initiated and adjusted based on an ongoing assessment of the patient’s level of asthma control.1,2 long-acting beta2-agonist (LABAs) are bronchodilators that improve the airflow in patients with asthma. The US Food and Drug Administration (FDA)-approved LABA products for asthma include 1) fixed-dose combination (FDC) inhaled corticosteroids (ICSs) and LABA (FDC-ICS/LABA) products and 2) single-ingredient LABA (SI-LABA) products. A list of LABA products is provided in Supplementary materials, Table S1.
Safety concerns associated with LABA have led to FDA regulatory activities by the US FDA since 2003, including several Advisory Committee meetings, Drug Safety Communications (DSCs), and label changes. The FDA-approved label is the official description of a drug, including indication and safety information,3 and the DSC delivers updated information about medical products’ new safety issues.4 Key FDA regulatory activities include:
In 2003, a boxed warning was added to salmeterol product labels for severe asthma exacerbations and death, which were observed in the Salmeterol Multicenter Asthma Research Trial (SMART).5,6
In July 2005, a Pulmonary and Allergy Drugs Advisory Committee recommended that the boxed warning be expanded to include formoterol LABA products.7
Two more Advisory Committee meetings included discussions on LABA in November 2007 and December 2008. The committee stressed that the appropriate use of LABA is in combination with a long-term asthma controller medication (ACM).8
In 2010, the FDA issued two DSCs to patients and providers, providing new recommendations for the safe use of LABA (Box S1); and these recommendations were incorporated into the LABA product labels.9
These three recommendations in the FDA’s 2010 DSCs focused on ways to ensure the safe use of LABA products for adult asthma treatment: 1) contraindicated use of SI-LABA; 2) a LABA should only be used when asthma is not adequately controlled on ICS or ACM; and 3) discontinue LABA when asthma control is achieved. Previously, the FDA examined LABA dispensing patterns to see whether the FDA’s recommendations specifically targeted at young (<18 years old) asthma patients were being followed.10 This study examines the impact of multiple FDA LABA-related regulatory activities on the initiation of LABA-containing products for asthma treatment, particularly the impact of the three key FDA recommendations made in the 2010 DSCs, using 2003–2010 as baseline (pre-DSCs) dispensing patterns.
Methods
Data source
The IMS LifeLink™ Health Plan Claims database was used to construct a cohort of adult asthma patients from January 2002 through December 2012. This database consisted of medical and pharmaceutical claims for ~70 million de-identified patients, from more than 86 health plans across the US. The claims are captured from doctor’s offices, pharmacies, specialists, hospitalizations, emergency department (ED) visits, tests, procedures, and injections. The database is nationally representative of the commercially insured population of the US based on age and gender. The US FDA’s Research in Human Subjects Committee (RIHSC) approved the current retrospective study. The US FDA’s RIHSC deemed patient consent not necessary as patients are de-identified.
Study cohort
We identified adult asthma patients who had an incident dispensing of LABA between January 2003 and December 2012. “Incident LABA dispensing” is defined as having no LABA prescription filled in the 6 months prior to the initiation date (index date). Patients were included if they had continuous commercial insurance enrollment and had a diagnosis of asthma in the 12 months prior to the index date and were aged between 18 and 64 years. Asthma was defined by the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9 CM) code 493.xx, including an asthma-related ED visit or hospitalization. Since the DSCs and labeling changes targeted asthma patients, we excluded patients with diagnoses of chronic obstructive pulmonary disease (ICD-9-CM codes 491.xx, 492.xx, 496.xx), cystic fibrosis (ICD-9-CM code 277.0x), bronchiectasis (ICD-9-CM code 494.xx), pulmonary hypertension or embolism (ICD-9-CM codes 416.0, 415.1), bronchopulmonary dysplasia (ICD-9-CM code 770.7), or congestive heart failure (ICD-9-CM code 428.xx) during the 12 months prior to or on the index date (19% of patients were excluded). We further excluded patients where there was missing information on age, gender, days’ supply, and patients with >100 days’ supply for LABA prescription during the study period (5% of patients were excluded). The 100-day cutoff was used since many health insurance companies do not cover the cost of prescriptions that exceed 100 days’ supply in the US.
Design and outcome measures
We used a longitudinal new user cohort design to examine the changes in LABA dispensing patterns over a 10-year study period. To assess the alignment with FDA’s safe use recommendation I (i.e., contraindicated use of SI-LABA products), we calculated the proportion of incident SI-LABA dispensing among all incident LABA dispensings. For those who also had a non-LABA ACM dispensed on the same date as the incident LABA, we consider the dispensing consistent with the DSC recommendation for the adult asthma patient population. For patients who only initiated an SI-LABA or an SI-LABA together with an ACM dispensing on the same date, we determined the concurrent treatment status, as having overlapping days of SI-LABA treatment with any long-term non-LABA ACM, including ICS, leukotriene modifier, chromones, oral systemic corticosteroids, immunomodulators, and methylxanthines. The medication concurrency ratio (MCR) was calculated as the ratio of the number of days a patient was on concurrent medications to the total number of days that patient was on an SI-LABA treatment.
To assess FDA recommendation II (i.e., add-on therapy, a LABA should only be used when the asthma is not adequately controlled on ICSs or ACM), we identified patients with claims for an ICS or other ACM in 3 or 6 months prior to initiating LABA treatment. We also identified patients whose asthma was “poorly controlled” before they initiated LABA treatment. The criteria for identifying patients with “poorly controlled asthma” in claims data are constructed from a surrogate measure using prescriptions or asthma-related ED visits or hospitalizations. The details for these criteria are described in Figure 1.11–13
To assess FDA recommendation III (i.e., step-down strategy, discontinue LABA when asthma control is achieved), we calculated the duration of first “continuous treatment”, defined as starting from the index date of the LABA dispensing until there is a gap of >25% of the prior prescription days’ supply. For this analysis, after the assessment of “continuous treatment”, we excluded patients who initiated a LABA in 6 months prior to the end of the study period (i.e., July–December 2012) to ensure that episodes were not truncated by the end of the data collection period. We calculated mean and median duration (in days) of “continuous treatment” and then estimated the proportion of patients who had longer than 2 or 4 months of continuous treatment on a LABA.
Statistical analyses
We used interrupted time series (ITS) to model the changes in the levels and trends of LABA initiation associated with FDA regulatory activities. Seasonality and autocorrelation were controlled using autoregressive integrated moving average models.14 Since FDA regulatory activities and asthma treatment guideline changes were undertaken intermittently across different time points, the study time was divided into three segments: post first labeling change (2003–2004); post 2005 regulatory activities, pre 2010 DSCs (2005–2009); and post 2010 DSCs (2010–2012). The ITS models included these three periods. The estimation of the prior ACM dispensing and appropriate LABA initiation was also based on these three periods. Linear regression was used for trend analysis over the 10-year period. The Bonferroni method was used to adjust for multiple comparisons by dividing the overall α level by the number of implied comparisons. All analyses were performed using SAS v.9.4 software (SAS Institute, Inc., Cary, NC, USA).
Results
There were 477,922 adults with asthma who met the eligibility criteria for initiators of LABA treatment over the study period (2003–2012); 50% were 18–45 years old and 67.5% were female.
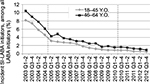
For recommendation I, among asthma patients who initiated any LABA treatment, the percentage of patients initiating an SI-LABA who did not have an ACM dispensed on the same date decreased. For 18–45 years old, the trend decreased from 9.6% (percentage points) in 2003 (the initial labeling change) to <1% post 2010 DSCs, with a baseline decreasing trend (−1.2% per 6 months [1.2% decreasing slope], p-value <0.0001 in the segmented regression model). There was a 1.1% significant decrease in SI-LABA initiation following 2005 regulatory activities (p-value <0.0001); then, the trend continuously decreased with a 0.3% decreasing slope after 2005 (the sum of the baseline trend, −1.2%, and the change in trend after 2005, 0.9%) and a 0.1% decreasing slope after 2010 regulatory activities. The decreasing trends and patterns were similar for the two age groups (Table 1 and Figure 2). In addition to the declining SI-LABA initiation (as a proportion of all LABA initiators among asthma patients) over the study period (2003–2012), we observed increased concurrent dispensing of ACM and SI-LABA therapy. In Table 2, the “SI-LABA” columns show the MCR for those who initiated an SI-LABA only (no other ACM dispensed on the same date) during the three time periods. The median MCR increased from 0% in 2003–2004, to 12.7% in 2005–2009 and to 33.3% in the 2010–2012 period. The proportion in the “high” concurrency category (MCR >75%) increased from 21.0% to 27.9%, and to 34.5% over the three time periods, respectively (p-value <0.001 for linear trend). The “SI-LABA and ACM” columns show the MCR for those who initiated an SI-LABA and had a dispensing of a non-LABA ACM on the same date. The MCRs were high (the median MCR was 100% for all the three periods) and the “high” concurrency category also increased over the three time periods (Table 2).
With regard to FDA’s safe use recommendation II, add-on therapy, Figure 1 illustrates the proportion of asthma patients who were dispensed an ACM (first three sets of bars) or who had poor asthma control (last set of bars), before initiating any LABA in the three periods: 2003–2004, 2005–2009, and 2010–2012. The proportion of these adult asthma patients who were dispensed an ICS in the 6 months before initiating a LABA decreased from 11.6% in 2003–2005, to 7.3% and 7.4% in the last two periods, respectively. Figure 1 shows that the proportion of patients with ≥1 dispensing of an ICS within 3 months was <10%. There were no statistically significant changes in the proportion of asthma patients dispensed an ACM product prior to initiating LABA treatment across the three time segments (40.1%, 39.4%, and 40.4%, respectively). The proportions of asthma patients dispensed an ACM did not increase much when using a 6- versus 3-month look-back window for identifying ICS or ACM dispensing prior to initiating any LABA treatment (the proportion with upward diagonal pattern). There were 34% of the LABA initiators identified as having poorly controlled asthma prior to initiating LABA treatment between 2003 and 2004, but this proportion was closer to 31% during 2005–2009 and 2010–2012.
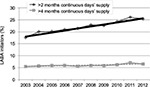
For FDA’s recommendation III, step-down strategy, the median for the first continuous LABA treatment was 30 days. There were >95% of patients who had a treatment duration shorter than 6 months over the 10-year period – 95% of patients had a duration shorter than 4 months in 2003 and 95% of patients had a duration shorter than 5.5 months in 2011 (Table S2). During the 10-year study period, the proportion of LABA initiators among asthma patients in each year who had longer LABA dispensing did not decrease (Figure 3). In fact, the proportion of LABA initiators who had longer than 2 months of continuous LABA treatment increased from 17.6% in 2003 to 25.4% in 2012; the proportion of LABA initiators increased from 5.4% in 2003 to 6.5% in 2012 with a 0.1% slope (p-value=0.009 for linear trend) for those with longer than 4 months of continuous days’ supply of a LABA dispensing (Figure 3).
Discussion
The most encouraging results of the current study are that the proportion of patients starting SI-LABA declined significantly over the 10-year study period and the new SI-LABA initiators had significantly increased concurrent ACM–LABA use. These findings align with FDA’s safe use recommendation I. However, the evidence on adherence to recommendation II (LABA only as add-on therapy) and recommendation III (step-down strategy) is not as encouraging. We observed low proportions of new LABA users having prior ICS or ACM use; and the proportions of incident LABA users with longer continuous LABA treatment increased over the 10-year period.
Recommendation I, contraindicated use of SI-LABA products. The 2003 boxed warning and results from SMART may have contributed to the sharp decline of the initiation of SI-LABA after 2003, and then the trend continuously declined over the 10-year study period. Similar patterns were also reported in the Mini-Sentinel LABA study using different data sets with a shorter study period, 2005–2011.15 In addition, the new SI-LABA users had significantly increased concurrent ACM–LABA use over the study period. These findings align with FDA’s multiple regulatory activities and asthma treatment guidelines.2,9
For recommendation II, the low proportions of new LABA users having prior ICS or ACM dispensing (~7% and 40%, respectively, throughout 2003–2012) in the 6 months prior to initiating LABA treatment in the adult population were also observed in other studies. Friedman et al16 reported that only 6.3% of LABA initiators had received an ICS, and 30% of new LABA users had either pre-index ICS use or an indication of moderate or severe asthma when using a different US commercial insurance database. Even though Hartung et al17 reported a small increase in the proportion of new LABA users having prior ACM within 3 months before initiating a LABA, after the FDA’s 2010 DSC, the overall proportion remained <40% over the entire study period (July 2008–December 2012). Similar results were also seen in the Mini-Sentinel LABA study.15 The low prevalence of ICS/ACM dispensing prior to LABA initiation suggests that many patients were prescribed a LABA without a trial of ICS/ACM.
We also identified only one-third of the patients aged 18–64 years with LABA initiation having evidence of preceding poorly controlled asthma (Figure 1, last set of bars). Similar low proportions of patients who had poorly controlled asthma were reported: 39.2% among study patients aged 12–64 years by Blanchette et al12 and 37.6% among study patients aged >12 years by Ye et al.13 These results may portray a prescribing behavior in the US that is inconsistent with recommendation II of the FDA 2010 DSCs.
For recommendation III (step-down therapy in asthma treatment), it is less measurable in the available claims data. The LABA duration was constructed by linking the days’ supply of subsequent prescriptions for the same patient if there was no big gap (<25% of the prior days’ supply). Our finding provided some evidence that most of the patients (95%) did not stay on a LABA for >6 months. However, the proportions of incident LABA users with longer continuous LABA treatment (>4 months) increased over the 10-year period. We do not know whether patients discontinued LABA because they had achieved good control over their asthma symptoms or for other reasons. For confirmation of appropriate step-down therapy, more granular clinical data (e.g., symptoms and pulmonary function and safety outcomes) and careful evaluation of long-term stability are needed;18–21 however, these data were not available in this current US claims database.
Overall, risk communications of medical products are important for patients using the products as well as for physicians prescribing them, yet such communications are rarely fully evaluated.22,23 There are many factors that could have had an impact on the LABA dispensing patterns in adult asthma patients over the 10-year study period. There were multiple important FDA LABA regulatory activities, worldwide asthma treatment guideline modifications, and relevant research publications during this time period. Clinical practice and patient preferences could have been influenced by these factors and others, such as overall ACM effectiveness, adverse event experience, medication formulary changes, product advertising, insurance coverage, over-the-counter availability, out-of-pocket, and overall cost.24–28 Of note, the cost of asthma medications is increasing dramatically in the US over the years;29,30 and the Centers for Disease Control and Prevention found that 15% of the population under the age of 65 years was uninsured during the first quarter of 2014 in the US.31 The high cost might be a barrier to choose asthma drugs and compliance with treatment guidelines and recommendations. Studies of LABA-related safety outcomes as well as how to achieve effective long-term asthma control may worth further investigation.20,32 In view of this multitude of potentially influential factors during the study period, we evaluated the segmented temporal trends with the expectation of continuous changes during the study period.
Limitations of the current study include the following points. First, this commercially insured claims data in the US capture dispensing as a surrogate for patients’ medication use; actual medication intake is unknown; no information on clinical details, such as asthma severity; and the same person could gain and lose insurance coverage. Therefore, the data and methodology were more robust for evaluating the first DSC recommendation, but less robust for the second and third recommendations. Second, even though the data are nationally representative of the commercially insured population of the US, this is still a small proportion of the population that is affected by the FDA’s recommendations, and the results may not be generalizable to the uninsured or publically insured population. Third, physicians may provide patients with “doctors’ samples” (provided by pharmaceutical companies) in the US. Studies have shown that physicians who provide samples are more likely to prescribe the drug that may be more expensive and not the first-line therapy drugs.33,34 Claims data do not capture these “samples”, which may lead to an incomplete asthma drug dispensing. However, there is no evidence that these “samples” would have systematic change over the years. Finally, the data cover the prescriptions dispensed between 2002 and 2012. Newer data may reveal more recent changes and impact on prescriber practice; therefore, continuous LABA monitoring is needed.
Conclusion
The results of this study are mixed, and only partly encouraging. The significant decrease in SI-LABA initiation is consistent with FDA’s regulatory activities and asthma treatment guidelines. However, the low ICS and ACM dispensing, as well as the low proportion of patients having poorly controlled asthma before LABA initiation, are not consistent with FDA’s LABA safe use recommendations. Additional analyses from the perspective of patients and prescribers may provide useful insight into the reasons for the low ACM use.22 For the assessment of step-down therapy, more granular clinical data are needed. Such future studies could inform approaches to improve adherence with the latest LABA safe use recommendations for asthma patients.
Acknowledgments
An abstract and a poster of this study were presented at the 31st International Conference on Pharmacoepidemiology & Therapeutic Risk Management, August 23–26, 2015, Boston, MA, USA. This study also contributed to the “Joint Meeting of the Pulmonary Allergy Drugs Advisory Committee (PADAC) and the Drug Safety and Risk Management Advisory Committee (DSARM)”, March 19, 2015, and can be found at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Pulmonary-AllergyDrugsAdvisoryCommittee/UCM438379.pdf. The authors gratefully acknowledge Judy A Staffa, PhD, RPh, Associate Director for Public Health Initiatives, Office of Surveillance and Epidemiology, for the thoughtful comments and suggestions. We thank Tracy Pham, Pharm. D. and Grace Chai, Pharm.D., Deputy Director for Drug Use, Division of Epidemiology II, Office of Surveillance and Epidemiology, for their assistance in acquiring the data and communicating with the data vendor. No internal or external funding was secured for this study.
Disclosure
All the authors were employees of the US FDA at the time of manuscript completion. The views expressed are those of the authors and not necessarily those of the US FDA. The authors report no other conflicts of interest in this work.
References
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention 2015 (revision). Available from: http://ginasthma.org/wp-content/uploads/2016/01/GINA_Report_2015_Aug11-1.pdf. Accessed January 21, 2017. | ||
National Heart, Lung, and Blood Institute. National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Full Report 2007. Available from: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf. Accessed Aug 17, 2016. | ||
FDA [webpage on the Internet]. Drugs@FDA Glossary of Terms. Available from: http://www.fda.gov/Drugs/InformationOnDrugs/ucm079436.htm#L. Accessed August 17, 2016. | ||
Food and Drug Administration [webpage on the Internet]. Drug Safety Communications. Available from: http://www.fda.gov/Drugs/DrugSafety/ucm199082.htm. Accessed August 17, 2016. | ||
Perera BJ. Salmeterol multicentre asthma research trial (SMART): interim analysis shows increased risk of asthma related deaths. Ceylon Med J. 2003;48:99. | ||
Wooltorton E. Salmeterol (Serevent) asthma trial halted early. CMAJ. 2003;168:738. | ||
2005 Pulmonary-Allergy Drugs Advisory Committee [webpage on the Internet]. Available from: http://www.fda.gov/ohrms/dockets/ac/cder05.html#PulmonaryAllergy. Accessed August 17, 2016. | ||
2008 Joint Meeting with Drug Safety, Risk Management Advisory Committee and the Pediatric Advisory Committee [webpage on the Internet]. Available from: http://www.fda.gov/ohrms/dockets/ac/cder08.html#PulmonaryAllergy. Accessed August 17, 2016. | ||
FDA Drug Safety Communication [webpage on the Internet]. Drug labels now contain updated recommendations on the appropriate use of long-acting inhaled asthma medications called Long-Acting Beta-Agonists (LABAs). Available from: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm213836.htm. Accessed August 17, 2016. | ||
Zhou EH, Kang EM, Seymour S, Iyasu S. Long-acting beta-adrenergic agonist use in pediatric and adolescent asthma patients, 2003-2011. J Asthma. 2014;51(10):1061–1067. | ||
Kaplan S, Zhou EH, Iyasu S. Characterization of long-actingbeta2-adrenergic agonists utilization in asthma patients. J Asthma. 2012;49:1079–1085. | ||
Blanchette CM, Culler SD, Ershoff D, Gutierrez B. Association between previous health care use and initiation of inhaled corticosteroid and long acting beta2-adrenergic agonist combination therapy among US patients with asthma. Clin Ther. 2009;31:2574–2583. | ||
Ye X, Gutierrez B, Zarotsky V, Nelson M, Blanchette CM. Appropriate use of inhaled corticosteroid and long-acting beta(2)-adrenergic agonist combination therapy among asthma patients in a US commercially insured population. Curr Med Res Opin. 2009;25(9):2251–2258. | ||
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. | ||
Butler MG, Zhou EH, Zhang F, et al. Changing patterns of asthma medication use related to FDA LABA Regulation from 2005-2011. J Allergy Clin Immunol. 2016;137(3):710–717. | ||
Friedman H, Wilcox T, Reardon G, Crespi S, Yawn BP. A retrospective study of the use of fluticasone propionate/salmeterol combination as initial asthma controller therapy in a commercially insured population. Clin Ther. 2008;30:1908–1917. | ||
Hartung DM, Middleton L, Markwardt S, Williamson K, Ketchum K. Changes in long-acting β-agonist utilization after the FDA’s 2010 drug safety communication. Clin Ther. 2015;37(1):114–123. | ||
Ahmad S, Kew KM, Normansell R. Stopping long-acting beta2-agonists (LABA) for adults with asthma well controlled by LABA and inhaled corticosteroids. Cochrane Database Syst Rev. 2015;19(6):CD011306. | ||
Horiuchi K, Kasahara K, Kuroda Y, Morohoshi H, Hagiwara Y, Ishii G. Step-down therapy in well-controlled asthmatic patients using salmeterol xinafoate/fluticasone propionate combination therapy. J Asthma Allergy. 2016;9:65–70. | ||
Patel M, Pilcher J, Beasley R. Combination ICS/fast-onset LABA inhaler as maintenance and reliever therapy: the future for uncontrolled adult asthma? Expert Rev Respir Med. 2013;7(5):451–454. | ||
Obase Y, Ikeda M, Kurose K, et al. Step-down of budesonide/formoterol in early stages of asthma treatment leads to insufficient anti-inflammatory effect. J Asthma. 2013;50(7):718–721. | ||
Kesselheim AS, Campbell EG, Schneeweiss S, et al. Methodological approaches to evaluating the impact of FDA drug safety communications. Drug Saf. 2015;38(6):565–575. | ||
Dusetzina SB, Higashi AS, Dorsey ER, et al. Impact of FDA drug risk communications on health care utilization and health behaviors: a systematic review. Med Care. 2012;50(6):466–478. | ||
Milgram LJ. Asthma medications should be available for over-the-counter use: con. Ann Am Thorac Soc. 2014;11(6):975–979. | ||
Dickinson BD, Altman RD, Deitchman SD, Champion HC. Safety of over-the-counter inhalers for asthma: report of the council on scientific affairs. Chest. 2000;118(2):522–526. | ||
Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94(10):1782–1787. | ||
Anarella J, Roohan P, Balistreri E, Gesten F. A survey of Medicaid recipients with asthma: perceptions of self-management, access, and care. Chest. 2004;125(4):1359–1367. | ||
Altawalbeh SM, Thorpe JM, Thorpe CT, Smith KJ. Cost-Utility Analysis of Long-Acting Beta Agonists versus Leukotriene Receptor Antagonists in Older Adults with Persistent Asthma Receiving Concomitant Inhaled Corticosteroid Therapy. Value Health. 2016;19(5):537–543. | ||
Kesselheim AS, Avorn J, Sarpatwari A. The high cost of prescription drugs in the United States: origins and prospects for reform. JAMA. 2016;316(8):858–871. Review. | ||
Chiu S, Kelton CML, Guo JJ, Wigle PR, Lin AC, Szeinbach SL. Utilization, spending, and price trends for short- and long-acting beta-agonists and inhaled corticosteroids in the medicaid program, 1991–2010. Am Health Drug Benefits. 2011;4(3):140–149. | ||
Cohen RA, Martinez ME. Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, January–March 2014; 2014. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Available from: http://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201409.pdf. Accessed December 7, 2016. | ||
FDA Drug Safety Communication [webpage on the Internet]. FDA requires post-market safety trials for Long-Acting Beta-Agonists (LABAs). Available from: http://www.fda.gov/Drugs/DrugSafety/ucm251512.htm. Accessed December 7, 2016. | ||
Hurley MP, Stafford RS, Lane AT. Characterizing the relationship between free drug samples and prescription patterns for acne vulgaris and rosacea. JAMA Dermatol. 2014;150(5):487–493. | ||
Adair RF, Holmgren LR. Do drug samples influence resident prescribing behavior? A randomized trial. Am J Med. 2005;118(8):881–884. |
Supplementary materials
  | Table S1 LABA products approved for asthma in the US before 2010 Abbreviation: LABA, long-acting beta2-adrenergic agonist; HFA, hydrofluoroalkane. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.