Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
The role of NOS2A -954G/C and vascular endothelial growth factor +936C/T polymorphisms in type 2 diabetes mellitus and diabetic nonproliferative retinopathy risk management
Authors Porojan MD, Cătană A, Popp R, Dumitrascu D, Bala C
Received 27 July 2015
Accepted for publication 6 October 2015
Published 27 November 2015 Volume 2015:11 Pages 1743—1748
DOI https://doi.org/10.2147/TCRM.S93172
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Mihai Dumitru Porojan,1 Andreea Cătană,2 Radu A Popp,2 Dan L Dumitrascu,1 Cornelia Bala3
1Department of Internal Medicine, 2Department of Molecular Sciences, 3Department of Diabetes, Nutrition and Metabolic Diseases, Iuliu Hatieganu, University of Pharmacy and Medicine, Cluj Napoca, Romania
Abstract: Type 2 diabetes mellitus (T2DM) remains one of the major health problems in Europe. Retinopathy is one of the major causes of morbidity in T2DM, strongly influencing the evolution and prognosis of these patients. In the last 2 decades, several studies have been conducted to identify the possible genetic susceptibility factors involved in the pathogenesis of the disease. However, there is little data related to the involvement of vascular endothelial growth factor (VEGF) and nitric oxide synthase (NOS) gene polymorphisms in the T2DM Caucasian population. The objective of this study was to identify a possible connection between NOS2A -954G/C (rs2297518) and VEGF +936C/T (rs3025039) polymorphisms and the risk of developing T2DM and nonproliferative diabetic retinopathy in a Caucasian population group. We investigated 200 patients diagnosed with T2DM and 208 controls. Genotypes were determined by multiplex polymerase chain reaction-restriction fragment length polymorphism. Statistical and comparative analyses (Fisher’s exact test) for dominant and recessive models of NOS2A -954G/C and VEGF +936C/T polymorphisms revealed an increased risk of T2DM (χ2=8.14, phi =0.141, P=0.004, odds ratio [OR] =2.795, 95% confidence interval [CI] =1.347–5.801; χ2=18.814, phi =0.215, P<0.001, OR =2.59, 95% CI =1.675–4.006, respectively). Also, comparative analysis for the recessive model (using Pearson’s chi-square test [χ2] and the phi coefficient [phi]) reveals that the variant CC genotype of NOS2A gene is more frequently associated with T2DM without retinopathy (χ2=3.835, phi =-0.138, P=0.05, OR =0.447, 95% CI =0.197–1.015). In conclusion, the results of the study place VEGF +936C/T polymorphisms among the genetic risk factor for T2DM, whereas NOS2A -954G/C polymorphisms act like a protective individual factor for nonproliferative retinopathy.
Keywords: type 2 diabetes mellitus, T2DM, retinopathy, +936C/T variant of VEGF gene, -954G/C of NOS2A gene
Introduction
Type 2 diabetes mellitus (DM) is a major public health problem, being one of the most common metabolic disorders.1,2 Even if the hyperglycemic status has a hereditary component with dominant expression in the phenotype, diabetes is considered as a multifactorial disease in which there is an imbalance associated with hereditary and environmental factors.3,4 Over the last 2 decades, genome-wide association studies, linkage analysis, candidate gene approach, and combined analysis of these candidate loci led to the identification of several molecular markers associated with the pathogenesis of T2DM and its complications.5–7
Diabetic retinopathy (DR) is one of the major complications in diabetic adults and considered as the major cause of new-onset blindness in these patients. This microvascular complication occurs rapidly in some patients, whereas it occurs in the late stages of diabetic evolution or does not develop at all in other patients.8–10
Vascular endothelial growth factor (VEGF) is a potent angiogenic and vascular permeability factor; therefore, this gene and its polymorphic variants seem to play an important role in DR characterized by impaired vascular permeability, tissue ischemia, and neoangiogenesis.11–13 The human VEGF gene is located on chromosome 6 (6p21.3) and highly polymorphic, with at least 30 single-nucleotide polymorphisms described in the literature.14–16 The particular +936C/T in the 3′-untranslated region of VEGF gene is one of the most common gene variants related to lower levels of plasma lipopolysaccharide-stimulated VEGF protein production in peripheral blood mononuclear cells in healthy individuals.17,18
Human gene encoding for nitric oxide synthase (NOS) is located on chromosome 17 (17q11.2-12)19 and consists of a highly reactive intercellular signaling molecule, with antithrombogenic and antiplatelet regulatory activities, produced in the Muller cells and the retinal pigment epithelium20 and highly expressed in retinal vessels, where it plays a major role in the regulation of vascular tone and macrophage remodeling.21 Although there is a sufficient evidence that endothelial NOS isoform is linked to diabetes and complications, such as retinopathy, inducible nitric oxide synthase (iNOS) remains unknown in terms of its association with DR. A pentanucleotide (CCTTT)n polymorphism was already proved to be associated with DR, although it is still questionable whether -954G/C polymorphism in the promoter region that affects the expression level of iNOS is also linked to DR.19
The objective of this study was to evaluate the possible association of +936C/T variant of VEGF gene and -954G/C of NOS2A gene in relationship with type 2 diabetes and nonproliferative retinopathy in a Caucasian of origin Eastern European population group.
Materials and methods
Patients and controls
The study was conducted according to the Declaration of Helsinki and was approved by the Ethics Committee of the “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania. Written informed consent was obtained from all subjects included in this study.
A group of 408 individuals, all Caucasians, were included in this prospective case–control study; among those, 200 patients with T2DM were included in the study group without a medical history of high blood pressure or dyslipidemia (independent risk factor for retinopathy). For both groups, fasting blood glucose, total serum cholesterol, high-density lipoprotein and low-density lipoprotein cholesterol, triglyceride level, weight, body mass index, abdominal circumference, and systolic and diastolic blood pressure were determined. For the study group, glycosylated hemoglobin (HbA1c) levels were determined in addition. Also, ophthalmological assessment with binocular indirect ophthalmoscopy and a standard fundus retinography (Visucam Lite; Carl Zeiss Meditec AG, Jena, Germany) was carried out in all diabetic subjects. We mention that in this study, only diabetic patients without retinopathy or with incipient, early-stage nonproliferative retinopathy were included. The controls consisted of 208 healthy, nondiabetic volunteers, with negative chronic ophthalmological illnesses.
Genotypic analyses of NOS2A -954G/C (rs2297518) and VEGF +936C/T (rs3025039)
DNA samples were obtained from 400 μL peripheral blood, using Wizard Genomic DNA Purification Commercial Kit (Promega Corporation, Fitchburg, WI, USA). Genotyping was based on polymerase chain reaction (PCR)-restriction fragment length polymorphism technique. For specific DNA amplification, a total amount of 100 ng of genomic purified DNA was amplified in a volume of 25 μL reaction mixture containing 12.5 μL of PCR mastermix, a premixed, ready-to-use solution containing Taq DNA polymerase, deoxynucleotide triphosphates, MgCl2, and reaction buffers (Promega Corporation); 7.5 μL free nuclease water; 1 μL of bovine serum albumine; 1 μL of each primer; and 1 μL of water suspended DNA. The amplification products were submitted to enzyme digestion (Fermentas; Thermo Fisher Scientific, Waltham, MA, USA) and analyzed by electrophoresis agarose gel (MetaPhor®; FMC BioProducts, Rockland, ME, USA), allowing detection by ethidium bromide staining of the corresponding genotypes. Specific thermocycling conditions and resulting DNA fragments are presented in Table 1. The genotypic analyses of NOS2A −954G/C (rs2297518) and VEGF +936C/T (rs3025039) were done in accordance with the studies of Kun et al22 and Guan X et al.23
Statistical analysis
Statistical analysis was carried out using SPSS 18.0 for Windows software (SPSS Inc., Chicago, IL, USA). Demographic and clinical data were compared using the Pearson’s chi-square test (χ2) and the phi coefficient. The distribution of genotype and allele frequency of each NOS2A -954G/C (rs2297518) and VEGF +936C/T (rs3025039) polymorphisms between different groups was compared by the Fisher’s exact test, followed by comparative analysis according to dominant and recessive models. For estimation of the relative risk and strength of association, we calculate odds ratio (OR) at 95% confidence interval (CI). A P-value <0.05 is considered to be statistically significant.
Results
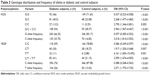
Demographic characteristic and clinical data of the diabetic subjects and controls are presented in Table 2. The average disease duration was 7.2±5.4 years. Statistical analysis did not reveal any differences between subjects and controls as sex distribution (χ2=1.370, phi =0.058, P=0.242), body mass index (P=0.219), weight (P=0.943), abdominal circumference (P=0.731), systolic blood pressure (P=0.312), and diastolic blood pressure (P=0.341). Although average mean age in control group is lower compared with the study group (P<0.001), this has no influence on the genetic polymorphisms, because they are present in individuals, without being age related.
None of the subjects from the control group or the study group had high cholesterol or triglycerides level.
Genotype distribution and frequency of alleles of NOS2A -954G/C and VEGF +936C/T polymorphisms in patients with diabetes and controls are presented in Table 3.
Comparative analysis (Fisher’s exact test) for dominant and recessive models of NOS2A -954G/C and VEGF +936C/T polymorphisms was performed.
Comparative analysis to assess the diabetes risk in the study group with that of the control group for -954G/C of NOS2A gene variant carriers (Fisher’s exact test analysis – ORs for dominant model) does identify a statistically increased risk value (χ2=8.14, phi =0.141, P=0.004, OR =2.795, 95% CI =1.347–5.801). The statistical analysis according to Fisher’s exact test – ORs for the recessive model – also reveals significant differences among patients and controls (χ2=27.712, phi =0.261, P<0.001, OR =2.965, 95% CI =1.967–4.468).
Comparative analysis to evaluate the diabetes risk in the study group with that of the control group for +936C/T polymorphism of VEGF gene carriers (Fisher’s exact test analysis – ORs for dominant model) does identify a statistically increased risk value (χ2=18.814, phi =0.215, P<0.001, OR =2.59, 95% CI =1.675–4.006); the same statistically significant differences were highlighted by using Fisher’s exact test – ORs for the recessive model (χ2=10.506, phi =0.160, P=0.001, OR =4.161, 95% CI =1.650–10.493).
DR was also assessed by using the same Fisher’s exact test – ORs. Comparative analysis for the dominant model to analyze DR in relation to the variant genotype for -954G/C of NOS2A gene did not reveal any statistically significant differences (χ2=1.661, phi =-0.091, P=0.197, OR 0.685, 95% CI =0.385–1.219), whereas comparative analysis for the recessive model highlighted that the variant CC genotype is more frequently associated with diabetes without retinopathy (χ2=3.835, phi =-0.138, P=0.05, OR =0.447, 95% CI =0.197–1.015).
Comparative analysis to analyze the diabetic nonproliferative retinopathy in relation to the variant genotype +936C/T of VEGF gene did not reveal any statistically significant differences for neither the dominant nor the recessive models (χ2=0.215, phi =0.033, P=0.643 OR =1.147, 95% CI =0.642–2.052 and χ2=1.316, phi =0.081, P=0.251, OR =1.769, 95% CI =0.661–4.739, respectively).
Nonproliferative DR assessed in relationship with HbA1c, and variant genotypes of both investigated polymorphisms also found no statistical differences (χ2=5.750, phi =0.182, P=0.016, OR =2.171, 95% CI =1.146–4.113 for -954G/C of NOS2A variant and χ2=5.288, phi =0.143, P=0.021, OR =3, 95% CI =1.158–7.772 for +936C/T of VEGF variant).
Discussion
Over the past 2 decades, the number of people diagnosed with T2DM has more than doubled globally, making it one of the major public health challenges to all developed countries. DR is the most common vascular complication of T2DM characterized by hemostatic abnormalities, increased vascular permeability, and tissue ischemia followed by neoangiogenesis, and it occurs in ~75% of patients within 15 years of evolution.24 As this complication is one of the major causes of blindness in general population, the etiopathogenesis of this complication has been extensively studied in recent years.
However, only some of the diabetics develop this retinopathy, and this proves that there are a series of individual genetic factors involved in the long-term outcome of microvascular diabetic complications. Therefore, it is important to identify the genetic susceptibility factors for DR, which could help us to clarify the pathogenesis, evolution, and adopt adequate treatment.25
The risk factors for DR include disease’s length (period of time), fasting glucose, HbA1c, and in addition high blood pressure, lipid serum levels, and genetic factors. The genetic risk factors remain a new, innovative field, requiring clear more scientific data that are involved in developing DR. We decided screening the subjects without high blood pressure and dyslipidemia and with a satisfactory glycemic control of the diabetes, especially for showing the role of genetic factors in DR.
Although NOS2A -954G/C and VEGF +936C/T polymorphisms and their relevance with diabetes and DR were studied in several different studies4,5 in the last years, there are few data regarding the distribution and importance of these two genetic variants in Caucasian population with diabetes.
Genetic variants of VEGF with dysregulated expression are implicated in many chronic proliferative disorders, with markedly elevated protein levels in the vitreous and aqueous fluids in the eyes of patients with diabetes.24 As VEGF may play an important role in the pathogenesis of DR, several polymorphisms have been studied in the VEGF gene. A meta-analysis found significant associations between +936C/T (rs3025039) and DR susceptibility in Asian populations;16 in accordance with other research group, a meta-analysis found that +936C/T polymorphism of VEGF gene was related to DR in Korean populations;26 however, another study on Asian population demonstrated no significant association of this polymorphism with diabetes and associated retinopathy.27 Our results come in agreement with these studies, placing +936C/T variant of VEGF gene among the genetic risk factors involved in the pathogenesis of type 2 diabetes and associated retinopathy.
Even if there are valid data regarding the distribution of this variant in the general population, it is still not clear whether there is a conclusive evidence for an association of this polymorphism with diabetes and retinopathy in East European Caucasian population.
It is well known that functional hyperemia in diabetic patients is severely decreased. The loss of this vascular response could starve the retina for oxygen and glucose, putting neurons at risk, and therefore contributing to retinal pathology.28 Neuronal or glial retinal dysfunction observed in early stages of DR is associated with altered neurovascular signaling, leading to the loss of functional hyperemia. Because functional hyperemia is reduced and iNOS expression is increased, genetic polymorphisms of NOS2A gene are the suitable candidate molecular markers for the study of DR. Also, chronic inflammation has been proposed to be involved in the pathogenesis of obesity-related insulin resistance and type 2 diabetes,29 and also a new study has shown that iNOS plays an important role in the pathogenesis of insulin resistance in vivo.30 Another proof that iNOS may be involved in DR is that restoring functional hyperemia by inhibiting iNOS may slow the progression of the disease.28
To our knowledge, there are no valid data regarding the assessment and relationship of -954G/C NOS gene polymorphism and diabetes in Caucasian population. -954G/C NOS was reported as a genetic risk variant in the inflammatory bowel disease in Spanish population or gastric cancer in the Chinese population.19 The results of our study show that variant CC genotype of -954G/C NOS gene is associated with T2DM but is less commonly found in subjects with DR. Most of the late studies focused on the study of the pentanucleotide (CCTTT)n repeat polymorphism in iNOS gene, result suggesting that this particular genetic variant seems to act like a protective factor against retinopathy in patients with T2DM.19,30 Although our study is among the first case–control study focused on the association of NOS2A -954G/C and VEGF +936C/T genetic polymorphisms with the risk of T2DM and DR in the eastern European population, our study still has some limitations due to the relatively small sample size and lack of information regarding the evolution of retinopathy in these diabetic patients.
Conclusion
In this study, +936C/T polymorphism of VEGF gene is highly associated with DR; therefore, this genetic variant is confirmed to be an independent genetic risk factor for nonproliferative retinopathy. As for -954G/C polymorphism of NOS gene, there is evidence that the variant genotype acts like a protective factor against retinopathy in patients with type 2 diabetes.
Studied genetic polymorphisms may play an important role in genetic predisposition to DR. This finding suggests the need for interventional approaches to identify asymptomatic patients at risk of developing retinopathy, which can benefit from an aggressive prevention of DR.
Acknowledgment
This article was published under the frame of the European Social Fund, Human Resources Development Operational Programme 2007–2013, project number POSDRU/159/1.5/S/138776.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Global Health Estimates: Deaths by Cause, Age, Sex and Country. Health Statistics and Information Systems. Geneva: World Health Organization; 2014. Available from: http://apps.who.int/healthinfo/statistics/mortality/whodpms/. Accessed July 16, 2015. | ||
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. | ||
Sun X, Yu W, Hu C. Genetics of type 2 diabetes: insights into the pathogenesis and its clinical application. Biomed Res Int. 2014;2014:926713. | ||
Morris AP, Voight BF, Teslovich TM, et al. Large scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet. 2012;44(9):981–990. | ||
Dupuis J, Langenberg C, Prokopenko I, et al. New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet. 2010;42(2):105–116. | ||
Voight BF, Scott LJ, Steinthorsdottir V, et al. Twelve type 2 diabetes susceptibility loci identified through large-scale association analysis. Nat Genet. 2010;42(7):579–589. | ||
Guo X, Cui J, Jones MR. Insulin clearance: confirmation as a highly heritable trait, and genome-wide linkage analysis. Diabetologia. 2012;55(8):2183–2192. | ||
Klein R, Lee KE, Gangnon RE, Klein BE. The 25-year incidence of visual impairment in type 1 diabetes mellitus: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Ophthalmology. 2010;117:63–70. | ||
The ACCORD Study Group and ACCORD Eye Study Group. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med. 2010;363:233–244. | ||
Ng PKD. Human genetics of diabetic retinopathy: current perspectives. J Ophthalmol. 2010;2010:172593. | ||
Ribatti D. The crucial role of vascular permeability factor/vascular endothelial growth factor in angiogenesis: a historical review. Br J Haematol. 2005;128(3):303–309. | ||
Chun MY, Hwang HS, Cho HY, et al. Association of vascular endothelial growth factor polymorphisms with nonproliferative and proliferative diabetic retinopathy. J Clin Endocrinol Metab. 2010;95(7):3547–3551. | ||
Yang X, Deng Y, Gu H, et al. Polymorphisms in the vascular endothelial growth factor gene and the risk of diabetic retinopathy in Chinese patients with type 2 diabetes. Mol Vis. 2011;17:3088–3096. | ||
Bleda S, De Haro J, Varela C, Esparza L, Ferruelo A, Acin F. Vascular endothelial growth factor polymorphisms are involved in the late vascular complications in type II diabetic patients. Diab Vasc Dis Res. 2012;9(1):68–74. | ||
Qiu M, Xiong W, Liao H, Li F. VEGF -634G>C polymorphism and diabetic retinopathy risk: a meta-analysis. Gene. 2013;518(2):310–315. | ||
Han L, Zhang L, Xing W, et al. The associations between VEGF gene polymorphisms and diabetic retinopathy susceptibility: a meta-analysis of 11 case-control studies. J Diabetes Res. 2014;2014:805801. | ||
Zhao T, Zhao J. Association between the -634C/G polymorphisms of the vascular endothelial growth factor and retinopathy in type 2 diabetes: a meta-analysis. Diabetes Res Clin Pract. 2010;90(1):45–53. | ||
Wróbel T, Mazur G, Dzietczenia J, Gębura K, Kuliczkowski K, Bogunia-Kubik K. VEGF and bFGF gene polymorphisms in patients with non-Hodgkin’s lymphoma. Biomed Res Int. 2013;2013:159813. | ||
Qidwai T, Jamal F. Inducible nitric oxide synthase (iNOS) gene polymorphism and disease prevalence. Scand J Immunol. 2010;72(5):375–387. | ||
Yoshida A, Pozdnyakov N, Dang L, Orselli SM, Reddy VN, Sitaramayya A. Nitric oxide synthesis in retinal photoreceptor cells. Vis Neurosci. 1995;12(3):493–500. | ||
Uthra S, Raman R, Mukesh BN, et al. Diabetic retinopathy: validation study of ALR2, RAGE, iNOS and TNFB gene variants in a south Indian cohort. Ophthalmic Genet. 2010;31(4):244–251. | ||
Kun JF, Mordmüller B, Perkins DJ, et al. Nitric oxide synthase 2Lambaréné (G-954C), increased nitric oxide production, and protection against malaria. J Infect Dis. 2001;184(3):330–336. | ||
Guan X, Yin M, Wei Q, et al. Genotypes and haplotypes of the VEGF gene and survival in locally advanced non-small cell lung cancer patients treated with chemoradiotherapy. BMC Cancer. 2010;16(10):431. | ||
Gong JY, Sun YH. Association of VEGF gene polymorphisms with diabetic retinopathy: a meta-analysis. PLoS One. 2013;8(12):e84069. | ||
Patel S, Chen H, Tinkham NH, Zhang K. Genetic susceptibility of diabetic retinopathy. Curr Diab Rep. 2008;8:257–262. | ||
Awata T, Inoue K, Kurihara S, et al. A common polymorphism in the 5′-untranslated region of the VEGF gene is associated with diabetic retinopathy in type 2 diabetes. Diabetes. 2002;51(5):1635–1639. | ||
Mandecka A, Dawczynski J, Blum M, et al. Influence of flickering light on the retinal vessels in diabetic patients. Diabetes Care. 2007;30(12):3048–3052. | ||
Perreault M, Marette A. Targeted disruption of inducible nitric oxide synthase protects against obesity-linked insulin resistance in muscle. Nat Med. 2001;7(10):1138–1143. | ||
Fujimoto M, Shimizu N, Kunii K, Martyn JA, Ueki K, Kaneki M. A role for iNOS in fasting hyperglycemia and impaired insulin signaling in the liver of obese diabetic mice. Diabetes. 2005;54(5):1340–1348. | ||
Kumaramanickavel G, Sripriya S, Vellanki RN, et al. Inducible nitric oxide synthase gene and diabetic retinopathy in Asian Indian patients. Clin Genet. 2002;61(5):344–348. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.