Back to Journals » Clinical Ophthalmology » Volume 17
The Role of Early Nd:YAG Laser Capsulotomy in Improving Visual Performance in Mild to Moderately Symptomatic Trifocal Patients
Authors LoBue SA , Martin CR, Benson KK, Trosclair KB, Shelby CL, Coleman III WT
Received 20 November 2023
Accepted for publication 12 December 2023
Published 22 December 2023 Volume 2023:17 Pages 3991—4000
DOI https://doi.org/10.2147/OPTH.S448784
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Stephen A LoBue,1 Curtis R Martin,1 Krysta K Benson,1 Krystle B Trosclair,2 Christopher L Shelby,1 Wyche T Coleman III1
1Department of Ophthalmology, Willis-Knighton Medical Center, Shreveport, LA, USA; 2Department of Graduate Medical Education, Statistics, Willis-Knighton Medical Center, Shreveport, LA, USA
Correspondence: Wyche T Coleman III, Department of Ophthalmology, Willis-Knighton Medical Center, Bert Kouns Industrial Loop, Suite 116, Shreveport, LA, 71118, USA, Tel +1-318-212-5901, Email [email protected]
Purpose: To determine the effect of early Nd:YAG (neodymium:yttrium-aluminum-garnet) laser capsulotomy on objective and subjective visual quality in symptomatic trifocal intraocular lens (IOL) patients.
Methods: A single-center, prospective study examined symptomatic patients after bilateral cataract extraction with trifocal IOL implantation. A ten-question survey was conducted one month after surgery. Study endpoints included the assessment of monocular and binocular uncorrected distance visual acuity (UDVA), uncorrected near visual acuity (UNVA), contrast sensitivity (CS), and subjective visual quality before and after Nd:YAG capsulotomy prior to 4 months after cataract surgery.
Results: A total of 38 eyes from 21 patients were included with a TFAT00 (n = 23) or TFAT30-60 (n = 15). Overall satisfaction with the IOL was 8.55 ± 1.77 (range 5– 10). A Nd:YAG capsulotomy was performed at 55 ± 26 days. Monocular UDVA and UNVA > 20/25 before Nd:YAG were 53.0% and 42.0%, which improved post-Nd:YAG to 63.0% and 66.0%, respectively (P = 0.41, P = 0.051). Binocular UDVA and UNVA > 20/25 before Nd:YAG were 82.0% and 63.0%, which increased to 97% and 97%, respectively (P < 0.05, P < 0.001). CS increased in all post-Nd:YAG capsulotomies (P < 0.01). The presence of glare was documented at 74% pre-Nd:YAG, which decreased to 41% post-Nd:YAG (P < 0.01). Glare which limited activities was documented at 24%, which decreased to 5% post-Nd:YAG (P = 0.21).
Conclusion: Early treatment of posterior capsule opacities in mild to moderately dissatisfied trifocal IOL patients may be beneficial in improving CS, visual quality, and reducing the presence and severity of dysphotopsias.
Keywords: trifocal IOL, posterior capsule opacification, Nd:YAG laser capsulotomy, visual performance, dysphotopsias, symptomatic patients
Introduction
The advancement of cataract surgery has progressed into lens-based refractive surgery as patients’ expectations continue to rise. Eliminating refractive error is not enough, as patients are now seeking spectacle independence at all distances with presbyopia-correcting intraocular lenses (IOL). Advances in presbyopia-correcting IOLs have led to the development of a trifocal diffractive IOL (AcrySof Panoptix, Alcon, Fort Worth, Texas, USA), enabling improved distance, intermediate, and near vision.1 However, the multiple concentric rings on the diffractive IOL cause an increased rate of dysphotopsia (eg, glare, haloes, starbursts) and reduction of contrast sensitivity which becomes problematic in a select group of patients.2
Apart from the optical properties of the intraocular lenses, capsular wrinkling is a well-known finding of cataract surgery that can lead to visual disturbances, including glare and haloes.3,4
In our practice, we anecdotally noticed that a majority of symptomatic trifocal IOL patients had subtle posterior capsule opacification (PCO) early in the postoperative period often with 20/25 or better uncorrected visual acuity. In these patients, overall visual satisfaction improved after neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy earlier in the postoperative period.
Thus, this prospective study was aimed at studying the effect of Nd:YAG laser capsulotomy prior to 4 months after cataract surgery with symptomatic trifocal IOL patients to examine the effects on subjective and objective visual performance as well as contrast sensitivity (CS).
Methods
Study Design
A prospective study was conducted at Willis-Knighton Eye Institute in Shreveport, Louisiana. The study was approved by the Institutional Review Board at Willis-Knighton Medical Center and was conducted according to the tenets of the Declaration of Helsinki. All patients provided verbal and written informed consent before participating in the study.
Patients
Patients included in the study involved men and women over 18 years of age who underwent planned bilateral cataract or clear lens extraction with posterior chamber IOL implantation. Only symptomatic patients with visual complaints were included in the study.
Patients were excluded from the study if they did not receive a trifocal IOL or were treated with Nd:YAG laser capsulotomy after 4 months from cataract surgery. Patients were also excluded if contrast sensitivity was not performed after cataract surgery prior to Nd:YAG laser capsulotomy.
IOL Description
The AcrySof PanOptix Trifocal IOL, model TFAT00 vs TFAT30-60 was the primary lens used in the study. This trifocal IOL has a biconvex optic containing an aspheric design and 26 diffractive rings on the anterior surface. Multiple concentric rings on the IOL allow for a range of vision including distance, intermediate, and near.
Procedures and Assessments
Femtosecond laser-assisted cataract surgery (FLACS) was performed using the LenSx platform (Alcon, Fort Worth, TX, USA) to create a 5mm anterior capsulotomy and fragmentation of the nucleus. The main incision and paracentesis were created manually. All phacoemulsification was performed with the Centurion vision system (Alcon, Fort Worth, TX) using topical anesthesia. Optiwave refractive analysis (ORA, Alcon Fort Worth, TX) was used after cataract extraction to verify or modify pre-operative IOL selection. A soft polymer irrigation/aspiration tip was used to polish the posterior capsule. Cataract extraction was uncomplicated and completed in all patients with the placement of a trifocal TFAT00 vs TFAT30-60 IOL.
Visual acuity was measured using the Snellen chart, and the total number of letters read was recorded and converted to logMAR for analyses. Distance measurements for binocular and monocular uncorrected distance visual acuity (UDVA) were tested at 6.1 m under 100% contrast photopic conditions with ambient room lighting. All binocular and monocular uncorrected near visual acuity (UNVA) were tested between 40cm and 33cm at the patient’s comfortable reading distance with photopic conditions with a Rosenbaum near chart with ambient room lighting.
PCO Grading
Grading was performed by one ophthalmologist according to Congdon’s study.5 A grade 0 was no central opacity with or without opacities on the peripheral capsule. Grade 1 involved wrinkling or opacity of the central capsule limited in a circle 4 mm diameter without impairing the view of the posterior retina. Grade 2 involved central or paracentral opacity worse than grade 1 which slightly affected the view of the posterior pole. Grade 3 involved a central or paracentral opacity worse than grade 2, impairing the view of the posterior pole and making the cup/disc ratio difficult to ascertain. Lastly, a grade 4, central or paracentral opacity severely hindered the view of posterior retina, making very difficult or impossible to see key structures.5
Nd:YAG Laser Capsulotomy
The eye was dilated with 2.5% phenylephrine and 1% tropicamide topical drops. The patient was then positioned at the Nd:YAG laser. Topical proparacaine was placed in the patient’s eye followed by the insertion of a capsulotomy lens with viscous eye gel (Genteal tears, Alcon, Fort Worth, TX). Nd:YAG laser was aligned with a view of the opacified capsule in the visual axis. A series of 10–20 laser pulses of approximately 1.8–2.4 millijoules of power per shot was used to create a diamond-shaped 4.5 mm opening of the posterior capsule.
The CSV-2000 contrast sensitivity test (Vector Vision, Greenville, OH, USA) was employed to assess distance contrast sensitivity (CS) monocularly at 2.5 m, under photopic (85 cd/m2) conditions. This test consists of a backlit translucent chart presenting four sine-wave stimuli corresponding to spatial frequencies of 3, 6, 12, and 18 cycles per degree with eight levels of contrast. A total of 5 minutes were given to the patient to adapt to each illumination level. CS testing was conducted with the best manifest refraction.
Patients were followed on postoperative day one, month one, and three months. Final refraction was performed between the first and third months. Manifest refractions were performed using the maximum plus refraction technique with plus cylinder. A ten-question survey was conducted one month after surgery (Table 1). Symptomatic patients complaining of worsening quality of vision after surgery were evaluated at the slit lamp. If a posterior capsule opacity was documented, CS was performed followed by Nd:YAG laser capsulotomy. Vision, contrast sensitivity, and the ten-question survey were repeated on a follow-up visit two weeks later.
 |
Table 1 Subjective Visual Performance Questionnaire |
Endpoint
The study endpoints included the assessment of monocular and binocular UDVA, UNVA, CS, and subjective vision quality evaluated with a questionnaire before and after Nd:YAG laser capsulotomy prior to 4 months of cataract surgery.
Statistical Analysis
SPSS (IBM, Armonk, New York, USA) was used for statistical comparisons of each group. When possible, the data groups are presented as mean ± standard deviation. Independent t-tests for numeric variables and Chi-square tests for categorical variables were utilized for statistical comparisons. Significance was set at p < 0.05.
Results
A total of 38 eyes from 21 patients were included in the study from July 2022 to July 2023. Two patients did not receive bilateral trifocal implantation secondary to high spherical aberration in one eye. A total of 68% were female with an average age of 68.6 ± 7.4. IOL selection included a TFAT00 (n = 23) or TFAT30-60 (n = 15) implanted in the capsular bag. The average axial length was 23.4 ± 0.89 mm, K1 43.6 ± 1.44, K2 44.5 ± 1.83, internal anterior chamber depth (ACD) 2.58 ± 0.29 mm, and total corneal spherical aberration 0.42 ± 0.15 µm. All patients had visual complaints (eg, blurry/foggy/waxy vision, glare, haloes) with 1+ PCO associated with or without capsular wrinkles (Figure 1). The time of onset of Nd:YAG laser capsulotomy from initial cataract surgery was 55 ± 26 days (Table 2). Macular optical coherence tomography (OCT) performed pre and post Nd:YAG laser capsulotomy demonstrated no significant change in central subfield thickness (CST).
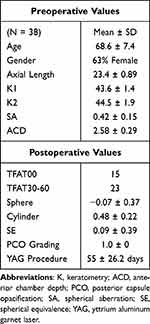 |
Table 2 Preoperative and Postoperative Data of All Patients Included in the Study |
 |
Figure 1 Early postoperative posterior capsule opacification (PCO) in symptomatic trifocal patients. (A) Grade 1+ PCO without capsular wrinkles. (B) Grade 1+ PCO with prominent capsular wrinkles. |
Objective Outcomes
Patients included in the study had a low residual refractive error. Among all patients, the cumulative visual acuity of 20/25 or better for binocular UDVA compared to CDVA was 92% vs 97% (Figure 2A). Binocular UDVA was the same or better than CDVA in 71% (Figure 2B). A total of 92% of UDVA was within 1 line of CDVA (Figure 2B). Postoperative spherical equivalence was within 0.5D for 87% compared to 1.00D for 100% of patients (Figure 2C). Residual refractive cylinder was ≤0.5D for 92% and ≤1.00D for 97% (Figure 2D).
The average monocular UDVA and UNVA before Nd:YAG capsulotomy was 0.095 ± 0.105 and 0.086 ± 0.091 which improved post-Nd:YAG to 0.05 ± 0.08 and 0.037 ± 0.55, respectively (P = 0.06, P < 0.001, Figure 3A). The average binocular UDVA and UNVA before Nd:YAG capsulotomy was 0.018 ± 0.083 and 0.045 ± 0.063 improved post-Nd:YAG to −0.032 ± 0.063 and 0.004 ± 0.026, respectively (P < 0.01, P < 0.001, Figure 3A).
The percentage of eyes with monocular UDVA and UNVA > 20/25 before Nd:YAG capsulotomy was 53.0% and 42.0% which improved post-Nd:YAG to 63.0% and 66.0%, respectively (P = 0.41, P = 0.051, Figure 3B). A larger increase in binocular UDVA and UNVA >20/25 before Nd:YAG capsulotomy was noted, demonstrating 82.0% and 63.0% which increased to 97% and 97%, respectively (P < 0.05, P < 0.001, Figure 3C).
Monocular contrast sensitivity significantly increased at 3, 6, 12, and 18 cycles per degree (CPD) from pre-Nd:YAG at 0.57 ± 0.19, 0.48 ± 0.20, 0.40 ± 0.24, and 0.33 ± 0.29 to post-Nd:YAG at 0.67 ± 0.15, 0.65 ± 0.19, 0.61 ± 0.20, and 0.58 ± 0.23, respectively (P < 0.01, P < 0.001, P < 0.001, P < 0.001, Figure 4).
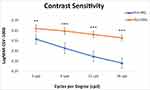 |
Figure 4 Monocular contrast sensitivity significantly increased at 3, 6, 12, and 18 cycles per degree (CPD) from pre-Nd:YAG to post-Nd-YAG (**P < 0.01, ***P < 0.001). |
Subjective Outcomes
The visual performance questionnaires with questions 1–10 were performed one month after cataract surgery and two weeks after Nd:YAG laser capsulotomy. All enrolled patients completed the survey prior to and after the Nd:YAG capsulotomy (n = 38).
Questions 1–3 involving the quality of distance, intermediate, and near vision without glasses increased after Nd:YAG capsulotomy. The quality of distance vision improved from 8.26 ±1.64 to 9.00 ± 1.68 (P = 0.056, Figure 5A). The quality of intermediate vision improved from 8.92 ± 1.22 to 9.50 ± 0.83 (P = 0.018, Figure 5A). The quality of near vision improved from 8.84 ± 1.20 to 9.39 ± 1.03 (P = 0.034, Figure 5A) The level of glasses independence (question 4) and quality of vision meeting expectations (question 5) increased from 9.55 ± 1.00 and 8.58 ± 1.93 pre-Nd:YAG to 9.66 ± 1.14 and 9.26 ± 1.57 post-Nd:YAG, respectively (P > 0.05, Figure 5A). The overall satisfaction with the lens and physician (questions 6 and 7) before Nd:YAG capsulotomy was 8.55 ± 1.77 and 9.82 ± 1.45 which increased post-Nd:YAG to 9.42 ± 0.39 and 9.95 ± 0.23, respectively (P = 0.022, P = 0.079, Figure 5A).
Patients stating that they would choose the same lens again were documented in 89% of patients pre-Nd:YAG which increased to 95% post-Nd:YAG (P = 0.39, Figure 5B). The presence of glare was documented at 74% pre-Nd:YAG which decreased to 41% post-Nd:YAG capsulotomy (P = 0.007, Figure 5C). Glare which limited activities (eg, night driving) was documented at 24% (n = 9) which decreased to 5% (n = 2) post-Nd:YAG capsulotomy (P = 0.21, Figure 5D).
Discussion
Overall patient satisfaction with trifocal IOL in our practice is generally very high. The high rate of success may be due to several factors including optimal lens position over the visual axis, minimal residual refractive error, low corneal aberration, and appropriate preoperative patient selection. Utilizing pentacam Scheimpflug imaging (Oculus, Wetzlar, Germany) we avoid asymmetric astigmatism or suspicious tomography consistent with ectatic disorders (eg, keratoconus) as well as total corneal spherical aberration greater than 0.7 µm. Significant pathology involving the cornea, macula, and optic nerve is also excluded as well as pilots or truck drivers seeking excellent night vision.
Regardless of strict patient selection and excellent refractive outcomes, a select number of patients will be unhappy with the quality of their vision and the level of diffractive dysphotopsias early in the postoperative period. Diffractive IOLs, such as trifocal IOL, are well known to cause starbursts, halos, and glare which can improve over 6 months with neuroadaptation.6 Nevertheless, we noticed that subtle PCOs were associated with increased visual complaints in these patients within the first few months after cataract surgery.
A PCO is the most common complication of cataract surgery, which results in secondary capsule opacification and wrinkling from the migration, proliferation, and normal or abnormal differentiation of lens epithelial cells (LECs).7,8
In addition to the established and accepted mechanism of PCO formation outlined above, we suggest an alternative mechanism involving capsular contraction around a smaller, synthetic IOL. The average axial diameter of a cataractous lens is approximately 5mm compared to a 0.5 mm synthetic IOL.9 In the process of scaring and contracting around the much thinner IOL, some wrinkling must occur. Thus, we suggest that every patient who undergoes uncomplicated cataract surgery will inevitably have some degree of PCO or capsular wrinkling.
Significant PCOs typically present six months to years following uncomplicated cataract surgery, causing decreased vision, increased glare/halos, reduced contrast, and impaired near vision.10,11 However, in a recent study of 1039 subjects with hydrophilic acrylic IOL implantation, 29% of individuals developed a PCO within 3 months, a majority of which were grade 1.12
In our prospective study, we performed Nd:YAG laser capsulotomy as early as 29 days postoperatively with an average of 55 days post-cataract surgery. Nd:YAG laser capsulotomy resulted in a significantly improved objective visual acuity among all patients. Specifically, binocular UDVA and UNVA had the greatest improvement post-Nd:YAG capsulotomy with 97% of patients seeing >20/25 compared to 82.0% and 63.0% pre-Nd:YAG, respectively (P < 0.05, P < 0.001, Figure 2C). The significant increase in objective visual performance is likely due to the improvement in contrast sensitivity. Contrast sensitivity significantly increased at all cycles per degree after Nd:YAG laser capsulotomy. Improvement in binocular vision at all parameters compared to monocular vision is likely due to the summation of vision between eyes, supporting the benefit of bilateral trifocal implantation.
It is well documented that MIOL implantation results in decreased CS in comparison to monofocal IOL.13–15 Additionally, a subtle, central PCO will further decrease CS, which is demonstrated in our study. Thus, we hypothesize that a large number of symptomatic patients with MIOL, especially trifocal IOLs, may be exacerbated by subtle opacities or wrinkles in the posterior capsule, increasing light scatter and diffractive dysphotopsias.
Our data support this hypothesis as post-Nd:YAG patients had a decrease in the amount and severity of dysphotopsias. The presence of glare was documented at 74% pre-Nd:YAG which decreased to 41% post-Nd:YAG capsulotomy (P = 0.007, Figure 4C). Glare that limited activities (eg, night driving) was documented at 24% (N = 9) which decreased to 5% (N = 2) post-Nd:YAG laser capsulotomy (P = 0.21, Figure 4D). Although a decrease in limiting dysphotopsia was not significant, the reduction is clinically meaningful and may be limited due to the small sample size.
CS is a better measure of vision quality and functional vision in a real-world setting compared to a Snellen chart.16 As a result, patients in our study also had a subjective increase in visual quality paralleling increased CS. Specifically, subjective intermediate and near vision had the most significant increase post-Nd:YAG, (P < 0.05, Figure 4A). Overall visual quality also significantly increased (P < 0.05, Figure 4A) supported by improvement in subjective and objective visual performance.
Limiting dysphotopsia, improving CS, and enhancing near vision to obtain spectacle independence are essential for MIOL success. A case series of 50 eyes who underwent explantation of MIOL found that the most common complaint for IOL removal involved waxy vision, glare/haloes, blurry vision at distance, intermediate, or near.17 In the above study, the most common reason for IOL explantation was decreased CS.17 Thus, the ability to perform a Nd:YAG laser capsulotomy early in the postoperative period has the potential to benefit symptomatic MIOL patients by increasing CS, decreasing dysphotopsias, and improving visual performance.
Although a safe procedure, Nd:YAG capsulotomies are not without risk and may result in a temporary increase in intraocular pressure, cystoid macular edema (CME), and rare cases of retinal detachment.8,18 Refractive errors including hyperopic shifts can occur with large posterior capsulotomies.11,13,14 These risks are reduced by minimizing laser energy and not extending the capsulotomy beyond 5 mm.10 All Nd:YAG capsulotomies performed in the study were performed with low levels of total energy with an approximate 4.5 mm posterior capsulotomy, extending just beyond the center diffractive rings. In general, treating early PCOs requires less power and number of shots, resulting in less total energy within the eye and potentially minimizing ocular complications.
Nevertheless, most surgeons are hesitant on performing Nd:YAG capsulotomies on MIOL patients, especially severely symptomatic patients early in the postoperative period as lens exchange becomes more challenging.19 Others believe that hyperopic shifts are greater earlier in the postoperative period, stating Nd:YAG capsulotomies should be performed after one year.20
Our cohort involved mild-to-moderate dissatisfied patients with a documented overall satisfaction rating of 8.55 ± 1.77 (range 5–10). Thus, caution should be given in performing a Nd:YAG capsulotomy in severely symptomatic patients. However, our study demonstrates that early Nd:YAG capsulotomy can have a significant improvement in objective and subjective visual quality on appropriate trifocal IOL candidates with a minimal refractive error. Thus, we do not delay Nd:YAG laser capsulotomies for mild to moderately symptomatic patients, especially individuals who are not willing to lose near vision with a lens exchange.
The main limitation of the study is the small sample size and lack of a placebo control. Larger prospective studies with an appropriate control are needed to be carried out to verify our findings. Additionally, other lenses need to be examined to determine if other types of MIOL have a similar effect with early Nd:YAG laser capsulotomy.
Conclusion
A PCO is the most common complication of cataract surgery, causing decreased vision, increased glare, and reduced CS. Mild-to-moderate symptomatic trifocal IOL patients in our study were associated with subtle capsular opacities and wrinkles less than 4 months post-cataract surgery. Early intervention with Nd:YAG laser capsulotomy between 1 and 4 months post-cataract surgery resulted in significant improvement in binocular UDVA, UNVA, and CS. Subjective visual quality also improved overall with a decrease in the amount and severity of dysphotopsias. Our study supports that even subtle PCOs early within the postoperative period can have a significant effect on subjective and objective visual quality, warranting early intervention in selected patients.
Acknowledgment
Presented as a paper discussion at the American Society of Cataract and Refractive Surgeons (ASCRS) annual meeting in San Diego in May, 2023.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hovanesian JA, Jones M, Allen Q. The PanOptix Trifocal IOL vs the ReSTOR 2.5 Active Focus and ReSTOR 3.0-add multifocal lenses: a study of patient satisfaction, visual disturbances, and uncorrected visual performance. Clin Ophthalmol Auckl NZ. 2021;15:983–990. doi:10.2147/OPTH.S285628
2. Pieh S, Weghaupt H, Skorpik C. Contrast sensitivity and glare disability with diffractive and refractive multifocal intraocular lenses. J Cataract Refract Surg. 1998;24(5):659–662. doi:10.1016/s0886-3350(98)80261-7
3. Holladay JT, Bishop JE, Lewis JW. Diagnosis and treatment of mysterious light streaks seen by patients following extracapsular cataract extraction. J Am Intra Ocul Implant Soc. 1985;11(1):21–23. doi:10.1016/s0146-2776(85)80108-7
4. Posterior capsular folds creating a Maddox rod effect following cataract surgery. Available from: https://webeye.ophth.uiowa.edu/eyeforum/cases/191-maddox-rod-effect.htm.
5. Congdon N, Fan H, Choi K, et al. Impact of posterior subcapsular opacification on vision and visual function among subjects undergoing cataract surgery in rural China: study of Cataract Outcomes and Up-Take of Services (SCOUTS) in the Caring is Hip Project, report 5. Br J Ophthalmol. 2008;92(5):598–603. doi:10.1136/bjo.2007.126714
6. Modi S, Lehmann R, Maxwell A, et al. Visual and patient-reported outcomes of a diffractive trifocal intraocular lens compared with those of a monofocal intraocular lens. Ophthalmology. 2021;128(2):197–207. doi:10.1016/j.ophtha.2020.07.015
7. Wormstone IM. Posterior capsule opacification: a cell biological perspective. Exp Eye Res. 2002;74(3):337–347. doi:10.1006/exer.2001.1153
8. Apple DJ, Solomon KD, Tetz MR, et al. Posterior capsule opacification. Surv Ophthalmol. 1992;37(2):73–116. doi:10.1016/0039-6257(92)90073-3
9. Khan A, Pope JM, Verkicharla PK, Suheimat M, Atchison DA. Change in human lens dimensions, lens refractive index distribution and ciliary body ring diameter with accommodation. Biomed Opt Express. 2018;9(3):1272–1282. doi:10.1364/BOE.9.001272
10. Pandey SK, Apple DJ, Werner L, Maloof AJ, Mb E, Milverton EJ. Posterior capsule opacification: a review of the aetiopathogenesis, experimental and clinical studies and factors for prevention. Indian J Ophthalmol. 2004;52(2):99.
11. Hayashi K, Hayashi H, Nakao F, Hayashi F. Correlation between posterior capsule opacification and visual function before and after Neodymium:YAG laser posterior capsulotomy. Am J Ophthalmol. 2003;136(4):720–726. doi:10.1016/S0002-9394(03)00425-2
12. Gu X, Chen X, Jin G, et al. Early-onset posterior capsule opacification: incidence, severity, and risk factors. Ophthalmol Ther. 2022;11(1):113–123. doi:10.1007/s40123-021-00408-4
13. Martínez Palmer A, Gómez Faiña P, España Albelda A, Comas Serrano M, Nahra Saad D, Castilla Céspedes M. Visual function with bilateral implantation of monofocal and multifocal intraocular lenses: a prospective, randomized, controlled clinical trial. J Refract Surg Thorofare NJ. 2008;24(3):257–264. doi:10.3928/1081597X-20080301-07
14. Cillino S, Casuccio A, Pace FD, et al. One-year outcomes with New-generation multifocal intraocular lenses. Ophthalmology. 2008;115(9):1508–1516. doi:10.1016/j.ophtha.2008.04.017
15. Maurino V, Allan BD, Rubin GS, et al. Quality of vision after bilateral multifocal intraocular lens implantation: a randomized trial--AT LISA 809M versus AcrySof ReSTOR SN6AD1. Ophthalmology. 2015;122(4):700–710. doi:10.1016/j.ophtha.2014.10.002
16. Ginsburg AP. Contrast sensitivity and functional vision. Int Ophthalmol Clin. 2003;43(2):5–15. doi:10.1097/00004397-200343020-00004
17. Fernández-Buenaga R, Alio JL, Pérez-Ardoy AL, et al. Late in-the-bag intraocular lens dislocation requiring explantation: risk factors and outcomes. Eye. 2013;27(7):795–802. doi:10.1038/eye.2013.95
18. Kim JW, Eom Y, Yoon EG, et al. Comparison of Nd:YAG laser capsulotomy rates between refractive segmented multifocal and multifocal toric intraocular lenses. Am J Ophthalmol. 2021;222:359–367. doi:10.1016/j.ajo.2020.09.046
19. Sachdev GS, Sachdev M. Optimizing outcomes with multifocal intraocular lenses. Indian J Ophthalmol. 2017;65(12):1294–1300. doi:10.4103/ijo.IJO_1072_17
20. Lee CY, Lu TT, Meir YJJ, et al. Refractive changes following premature posterior capsulotomy using neodymium:yttrium-aluminum-garnet laser. J Pers Med. 2022;12(2):272. doi:10.3390/jpm12020272
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



