Back to Journals » Clinical Ophthalmology » Volume 16
The Role of Automated Peripheral Iridectomy Combined with Phacoemulsification and Mini Ex-PRESS Shunt Implantation in Patients with Chronic Angle Closure Glaucoma
Authors Samir A , Abdelrahman Elsayed AM , Deiaeldin YA , Al-Naimy MA
Received 4 April 2022
Accepted for publication 28 July 2022
Published 19 August 2022 Volume 2022:16 Pages 2699—2703
DOI https://doi.org/10.2147/OPTH.S367509
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Supplementary video of "Phacoemulsification and ExPress shunt implantation" [ID 367509].
Views: 386
Ahmed Samir,1,2 Ayman M Abdelrahman Elsayed,1 Yasmine A Deiaeldin,1 Mohammed A Al-Naimy1
1Department of Ophthalmology, Zagazig University, Zagazig, Sharkia, Egypt; 2Magrabi Eye Hospital, Jeddah, Kingdom Saudi Arabia
Correspondence: Ahmed Samir, Tel +966 594988779, Email [email protected]
Purpose: To evaluate the role of automated peripheral iridectomy as an adjunctive tool combined with phacoemulsification and ExPRESS shunt implantation in management of cases with chronic angle closure glaucoma.
Setting: Magrabi eye hospital.
Methods: This prospective study included 22 eyes of 22 patients with chronic angle closure glaucoma and cataract who underwent Ex-PRESS shunt implantation, cataract extraction and surgical peripheral iridectomy at the site of shunt implantation in the period between January 2018 and April 2020.
Results: After surgery, the mean IOP was 11.3± 1.2 mm Hg, 14.5± 1.6 mm Hg, 14.8± 2.1 mm Hg, 15.3± 1.9 mm Hg and 17.4± 1.8 mm Hg at 7 days, 1 month, 3 months, 6 months and 12 months, respectively. All postoperative IOP was significantly lower compared with preoperative IOP (P = 0.001). There was a significant decrease in the number of medications required after surgery. The baseline mean number of medications was 3.4± 0.02 (range from 1 to 4), while postoperatively the mean number of medications decreased to 0.7± 0.01 at 12 months (P < 0.01). The qualified success rate was 6/22 eyes, and the complete success rate was 16/22 (72.7%) at 12 months, respectively.
Conclusion: The combined phacoemulsification and Ex-PRESS shunt implantation with automated peripheral iridectomy is an effective and safe procedure to treat chronic angle closure glaucoma.
Keywords: Ex-PRESS shunt, chronic angle closure glaucoma, iridectomy
Introduction
Glaucoma is the leading cause of irreversible blindness. Primary open-angle glaucoma is three times more common than angle-closure glaucoma, although angle closure is responsible for 50% of blindness caused by glaucoma because of the greater morbidity of this disease.1 The primary risk factors for angle-closure include older age, female gender, and race.1
Surgical management of chronic angle-closure glaucoma includes filtering surgery with a high rate of complications, such as shallow anterior chamber, hypotony, choroidal detachment, choroidal hemorrhage, and aqueous misdirection with significant visual impairment.2 Other surgical treatments have been investigated, including phacoemulsification alone or combined with other procedures such as goniosynechiolysis, surgical iridectomy, endocyclophotocoagulation and glaucoma drainage devices.3,4
Ex-PRESS shunt has been introduced as an alternative to trabeculectomy in controlling IOP. The implant is a non-valved stainless-steel device which is implanted under a scleral flap to drain aqueous humor from the anterior chamber to the subconjunctival space, creating a filtration bleb.5 Fewer complications, such as hyphema, encapsulated bleb, blockage by the iris and, more rarely, migration into the anterior chamber, have been reported with this procedure.5
Ex-PRESS shunt was indicated initially for open-angle glaucoma but has been implanted in other types of glaucomas, including neovascular glaucoma, uveitic glaucoma and post-penetrating keratoplasty glaucoma with satisfactory results.6
Ex-PRESS shunt is not suitable for PACG patients because they have shallow peripheral anterior chamber. This is because the shunt may be relatively too thick and could accidently contact either the cornea or the iris, resulting in endothelial cells and iris damage.7 The device needs an adequate space in the anterior chamber angle and so it is not suitable in acute or chronic angle-closure glaucoma unless concomitant cataract surgery is planned.7,8
This study evaluated the role of phacoemulsification combined with Ex-PRESS shunt implantation with adjunctive surgical peripheral iridectomy (SPI) in treating cases with combined cataract and chronic angle closure glaucoma.
Patients and Methods
This prospective study included 22 eyes of 22 patients with chronic angle-closure glaucoma and cataract who underwent Ex-PRESS shunt implantation (Supplementary Video S1), cataract extraction and surgical peripheral iridectomy at the site of shunt implantation in the period between January 2018 and April 2020. The model used in this study was P50 (Ex-PRESS P50, Alcon Laboratories, Fort Worth, Texas, USA). All included patients were treated by the same surgeon (A.S.).
The study protocol was approved by the Magrabi Eye Hospital Research Committee and the study was adherent to the tenets of the Declaration of Helsinki. The procedure and the follow up were disclosed to all patients and informed written consent was obtained.
Cases included in this study are patients with chronic angle closure glaucoma, with peripheral anterior synechia (PAS) more than 180 degrees and coexisting cataract. The indication for glaucoma filtering surgery was based on uncontrolled IOP or progressive visual field defect despite maximum anti-glaucoma medications.
Eyes with angle closure that was secondary to other ocular abnormalities, previous incisional ocular surgery, concurrent retinal or optic neuropathy other than glaucoma were excluded.
A comprehensive ophthalmic examination was performed before surgery at one week as well as at 1, 3, 6 and 12 months after surgery. Examinations included Snellen distance best corrected visual acuity (BCVA), IOP measurement with Goldmann applanation tonometer, fundus examination and gonioscopy.
Surgical Procedure
All patients were operated on under local anesthesia. After phacoemulsification and IOL implantation, intracameral miostat is injected and after miosis an automated peripheral iridectomy was done at the site of Ex-PRESS shunt implantation using a 23-gauge vitrectomy cutter of the phacoemulsification machine (cutting rate 100 cpm and vacuum of 300 mm Hg were used). This aimed to create roomy space in the anterior chamber to avoid iris touch and clogging the inner opening of the Ex-PRESS shunt. A 6-0 silk traction suture was placed in the upper cornea. A fornix-based conjunctival periotomy and a dissection of a 4 × 4 mm half-thickness rectangular scleral flap was fashioned. For the application of MMC, a 2×2 mm cellulose sponge saturated with 0.2 mg/mL solution of MMC was applied under the conjunctiva and scleral flap for 3 minutes. The surgical site was then irrigated with 20 mL of balanced salt solution. A stab incision into the anterior chamber parallel to the iris was made using a 25-G needle, then the Ex-PRESS miniature glaucoma implant was inserted into the anterior chamber under the scleral flap. The scleral flap and conjunctiva were closed with 10-0 nylon sutures. The OVD was aspirated at the end of the operation and intracameral antibiotic was injected.
Postoperatively, all patients were treated with topical broad spectrum antibiotic drops (moxifloxacin) four times per day, topical prednisolone acetate four times per day and topical NSAID drops once a day. The topical antibiotic and NSAID were stopped after two weeks and the topical steroid was tapered over four weeks
The primary outcome measures were the intraocular pressure (IOP) at the end of follow-up period and number of medications used postoperatively to maintain IOP < 21 mmHg while the secondary outcome measures were best corrected visual acuity (BCVA) at the end of follow-up period and occurrence of complications.
Surgery was considered a complete success when postoperative IOP was <21 mmHg without medication. Qualified success was defined as IOP < 21 mmHg with medication. Surgery was considered a failure when IOP was higher than 21 mmHg despite medication and/or further glaucoma surgery was required.
Data were statistically analyzed using procedure of SPSS (2012) according to the following model: Yij = µ + Ti + eij, where µ = the overall mean, Ti = the fixed effect of operative (1 = pre-operative IOP, pre-operative BCVA and pre-operative number of medications, 2 = postoperative IOP, postoperative BCVA and postoperative number of medications and eij = residual error).
Results
Twenty-two eyes of 22 patients were included in this study. Table 1 shows preoperative data of the patients.
 |
Table 1 Pre-operative Data of the Patients |
The mean age of the patients was 58.5±1.76 years (range from 39–73 years). Mean pre-operative IOP was 28.2±2.16 mm Hg. Mean pre-operative BCVA was 0.43±0.02. The mean number of pre-operative anti-glaucoma medications was 3.4±0.2 drugs.
After surgery, the mean IOP was 11.3±1.2 mm Hg, 14.5 ±1.6 mm Hg, 14.8±2.1 mm Hg, 15.3±1.9 mm Hg and 17.4±1.8 mm Hg at 7 days, 1 month, 3 months, 6 months and 12 months, respectively, as shown in Figure 1. All postoperative IOP was significantly lower compared with pre-operative IOP (P = 0.001).
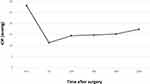 |
Figure 1 Mean IOP before surgery and at each follow-up period. |
There was a significant decrease in the number of medications required after surgery. The baseline mean number of medications was 3.4±0.02 (range from 1 to 4), while postoperatively the mean number of medications decreased to 0.7±0.01 at 12 months (P < 0.01).
The qualified success rate was (6/22 eyes), and the complete success rate was (16/22) at 12 months, respectively.
The mean pre-operative BCVA 0.4±0.28 (range from 0.05 to 1.0) increased to 0.5±0.25 (range 0.05 to 1.0) at 12 months.
There were no postoperative complications in the form of flat anterior chamber, hypotony, choroidal detachment or bleb leak. Fifteen patients needed Argon laser suturelysis. Posterior capsular opacification occurred following cataract surgery, and Nd:YAG laser capsulotomy was performed in 5 eyes to restore visual acuity.
Discussion
Ex-PRESS is usually not recommended for PACG treatment due to the shallow peripheral anterior chamber. However, this concept has changed as recent studies have shown that the depth of the central and peripheral regions of the anterior chamber increases after phacoemulsification plus IOL implantation in PACG which is wide enough to accommodate the Ex-PRESS shunt.8–10
However, some studies reported Ex-PRESS shunt contact with the iris with or without being blocked, which may need re-intervention to readjust the shunt.10
Kanner11 reported that the most common Ex-PRESS shunt-related complication was blockage of the lumen of the device; however, we did not observe any in our case series. There was a significant decrease in the number of medications required after surgery. This matches with Li et al,13 who reported that the number of medications decreased from 2.47±1.89 pre-operatively to 0.21±0.74 postoperatively.
The qualified success rate was 6/22eyes and the complete success rate (IOP < 21 mm Hg without medication) in our study was 16/22 eyes (73%) at 12 months, which is comparable to previous studies on the same patients. Tsai et al12 reported that the complete success rate for PACG eyes undergoing phaco-trabeculectomy was about 75% at one year after surgery. Wang et al13 reported that the success rate (IOP < 21 mm Hg without medication) was 88% for PACG undergoing phaco-trabeculectomy after 10 months follow-up. Poon et al14 showed the complete success rate (IOP < 15 mm Hg without medication) of phaco-trabeculectomy was 74% in PACG in the two years follow-up. The success rate reported by Li et al8 was 90.9%, which is higher than our study, may be due to the higher ratio of postoperative scleral flap argon suture lysis and 5-FU injection.
Ex-PRESS implantation generally had no everlasting impact on visual acuity when compared with the baseline. The mean pre-operative BCVA 0.4±0.28 increased to 0.5±0.25 at 12 months, which was insignificant. However, BCVA improved in 11 eyes (50%) of our patients. No change was recorded in 11 eyes (50%). All these results indicated that Ex-PRESS is a safe procedure for PACG patients with cataracts.
In other similar studies the reported complication rates of Ex-PRESS shunts were low, in the form of hypotony (4% to 22%), shallow anterior chamber (3% to 20%), suprachoroidal effusion (4% to 24%), bleb leakage (2.5% to 29%) and hyphema (1%to 8%).15,16
In this study only two cases (5.8%) showed transient hypotony and shallow anterior chamber. A case with hyphaema was observed in the first postoperative day, but resolved spontaneously within 3 days.
In our study no postoperative complications in the form of flat anterior chamber, choroidal detachment or bleb leak were encountered in the postoperative period. Fifteen patients needed Argon laser suturelysis. Posterior capsular opacification occurred in 5 eyes and Nd:YAG laser capsulotomy was performed to restore visual acuity. No intraoperative complications occurred during cataract surgery.
In conclusion, this prospective study demonstrates that Ex-PRESS implantation is associated with a lower rate of postoperative complications. Adjunctive intra-operative SPI gives more space to the shunt and prevents iris blockage; it is therefore more effective and safer in the management of PACG accompanied with cataract.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Nicolai M, Franceschi A, Pelliccioni P, Pirani V, Mariotti C. EX-PRESS glaucoma filtration device: management of complications. Vision. 2020;4(3):39. doi:10.3390/vision4030039
2. Tian T, Li M, Pan Y, Cai Y, Fang Y. The effect of phacoemulsification plus goniosynechialysis in acute and chronic angle closure patients with extensive goniosynechiae. BMC Ophthalmol. 2019;19(1):65. doi:10.1186/s12886-019-1070-9
3. Izquierdo Villavicencio JC, Agudelo Arbelaez N, Lastra BR, et al. Primary outcomes of patients with chronic angle-closure glaucoma treated with combined phacoemulsification, viscogoniosynechialysis, and endocyclophotocoagulation. J Ophthalmol. 2019;2019:6378489. doi:10.1155/2019/6378489
4. Bayliss JM, Ng WS, Waugh N, Azuara-Blanco A. Laser peripheral iridoplasty for chronic angle closure. Cochrane Database Syst Rev. 2021;3(3):CD006746. doi:10.1002/14651858.CD006746.pub4
5. Altinel MG, Kanra AY, Karadag R, Bayramlar H. Ex-PRESS implantation for different types of glaucoma. Int J Ophthalmol. 2019;12(8):1290–1297. doi:10.18240/ijo.2019.08.09
6. Wagdy FM, Zaky AG. Comparison between the express implant and transscleral diode laser in neovascular glaucoma. J Ophthalmol. 2020;2020:3781249. doi:10.1155/2020/3781249
7. Ledesma-Gil J, Alvarez-Guzman C, Navas A, Ahmed I. Late-onset spontaneous EX-PRESS shunt dislocation into anterior chamber. Can J Ophthalmol. 2021;56(2):e58–e59. doi:10.1016/j.jcjo.2020.07.008
8. Nie L, Fang A, Pan W, et al. Prospective study on Ex-PRESS implantation combined with phacoemulsification in primary angle-closure glaucoma coexisting cataract: 3-year results. Curr Eye Res. 2018;43(8):1045–1051. doi:10.1080/02713683.2018.1464196
9. Dada T, Mohan S, Bali SJ, Bhartiya S, Sobti A, Panda A. Ultrasound biomicroscopic assessment of angle parameters in patients with primary angle closure glaucoma undergoing phacoemulsification. Eur J Ophthalmol. 2011;21:559–565. doi:10.5301/EJO.2011.6287
10. Hayashi K, Hayashi H, Nakao F, Hayashi F. Changes in anterior chamber angle width and depth after intraocular lens implantation in eyes with glaucoma. Ophthalmology. 2000;107:698–703. doi:10.1016/S0161-6420(00)00007-5
11. Kanner EM, Netland PA, Sarkisian SR, Du H. Ex-PRESS miniature glaucoma device implanted under a scleral flap alone or combined with phacoemulsification cataract surgery. J Glaucoma. 2009;18:488–491. doi:10.1097/IJG.0b013e31818fb44e
12. Tsai HY, Liu CJ, Cheng CY. Combined trabeculectomy and cataract extraction versus trabeculectomy alone in primary angle-closure glaucoma. Br J Ophthalmol. 2009;93:943–948. doi:10.1136/bjo.2008.151803
13. Wang M, Fang M, Bai YJ, et al. Comparison of combined phaco-trabeculectomy with trabeculectomy only in the treatment of primary angle-closure glaucoma. Chin Med J. 2012;125:1429–1433.
14. Poon LY, Lai IC, Lee JJ, Tsai JC, Lin PW, Teng MC. Comparison of surgical outcomes after phacotrabeculectomy in primary angle-closure glaucoma versus primary open-angle glaucoma. Taiwan J Ophthalmol. 2015;5:28–32. doi:10.1016/j.tjo.2015.01.001
15. Marzette L, Herndon LW. A comparison of the Ex-PRESS mini glaucoma shunt with standard trabeculectomy in the surgical treatment of glaucoma. Ophthalmic Surg Lasers Imaging. 2011;42:453–459. doi:10.3928/15428877-20111017-03
16. Seider MI, Rofagha S, Lin SC, Stamper RL. Resident-performed Ex-PRESS shunt implantation versus trabeculectomy. J Glaucoma. 2012;21:469–474. doi:10.1097/IJG.0b013e3182182bfb
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
