Back to Journals » Infection and Drug Resistance » Volume 15
The Risk of Emerging Resistance to Trimethoprim/Sulfamethoxazole in Staphylococcus aureus
Authors Sato T , Ito R, Kawamura M , Fujimura S
Received 13 June 2022
Accepted for publication 17 August 2022
Published 23 August 2022 Volume 2022:15 Pages 4779—4784
DOI https://doi.org/10.2147/IDR.S375588
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Takumi Sato, Ryota Ito, Masato Kawamura, Shigeru Fujimura
Division of Clinical Infectious Diseases & Chemotherapy, Tohoku Medical and Pharmaceutical University, Sendai, Japan
Correspondence: Takumi Sato, Division of Clinical Infectious Diseases & Chemotherapy, Tohoku Medical and Pharmaceutical University, 4-4-1 Komatsushima, Aoba-ku, Sendai, 981-8558, Japan, Tel/Fax +81227270176, Email [email protected]
Objective: Due to the spread of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA), the demand for trimethoprim/sulfamethoxazole (SXT) is increasing in the world. It is not clear whether the resistant strain emerges by overuse of SXT. We investigated here the emergent risk of the SXT-resistant mutant in S. aureus by an in vitro SXT exposure experiment.
Methods: A total of 40 S. aureus clinical isolates (20 MSSA and 20 MRSA isolates) were exposed to sub-MIC of SXT for consecutive days, and MIC of SXT was determined every day. In addition, the dfrB DNA sequencing was performed to detect the mutation in the SXT-resistant strain.
Results: The SXT-resistant strain began to emerge on the eighth day and accounted for 45% (18/40 clinical isolates) after 14 days. Moreover, one half of these resistant strains showed F98Y mutation in DfrB to retain SXT-resistance without selective pressure.
Conclusion: The emergent risk was SXT exposure of 14 days or more.
Keywords: Staphylococcus aureus, antimicrobial resistance, trimethoprim/sulfamethoxazole, dfrB
Introduction
Community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) is spreading worldwide.1–3 As a therapeutic option other than antibiotic agents, essential oil is considered4–6 against drug-resistant S. aureus such as MRSA; however, clinical evidence is limited. In actual clinical setting, trimethoprim/sulfamethoxazole (SXT) has been used to treat skin and soft tissue infections and bone and joint infections because the majority of S. aureus isolates, including CA-MRSA, are susceptible to this drug.7,8 However, there are some cases of failure and/or recurrence by the drug-resistant acquisition.9,10 S. aureus shows resistance to SXT due to the mutation of dfr gene where dihydrofolate reductase becomes the target of trimethoprim.11 We investigate here the emergence risk of the SXT-resistant mutants through in vitro exposure of SXT.
Materials and Methods
Bacterial Strains
A total of 40 SXT-susceptible S. aureus clinical isolates, consisting of 20 MSSA and 20 MRSA isolates, were used. These strains were isolated, as a part of standard hospital protocol, from 16 general hospitals in the Tohoku region in Japan, their origins are as follows: sputum, 30%; pus, 20%; otorrhea, 13%; nasal cavity, 10%; and other, 27%. These isolates are collected and stocked by Tohoku Infectious Diseases society, and we received from them. In addition, these strains have confirmed not harbor mobile genetic elements including dfrA, dfrK, and/or dfrG by the conventional PCR method.12
Antimicrobial Susceptibility Testing and in vitro SXT Challenge
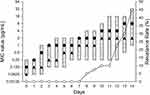
MIC of SXT was determined by the broth microdilution method according to the guideline of the Clinical and Laboratory Standard Institute,13 with resistance being in accordance with M100-S28.14 The SXT challenge to inoculate sub-MIC surviving strain into another dilution series was performed for a total of 14 days (Figure 1).15 Moreover, to investigate whether acquired resistance was maintained, strains were subsequently incubated using drug-free Mueller-Hinton broth (MHB) (Day 28). Then, these strains were re-challenged with SXT for 7 days (Day 35).
 |
Figure 1 Experimental design. Allow indicated days of incubation with or without trimethoprim/sulfamethoxazole. |
DNA Sequencing of dfrB Gene
The DNA sequence of the dfrB gene in the SXT-resistant strain was determined by the Dye Terminator Cycle Sequencing method using Genomelab GeXP and Quick Start Kit (Beckman Coulter Inc., CA, US) and the previously described primer.16
Growth Ability Assay
Further, to determine the growth ability of each strain, bacterial counts were measured.17 Briefly, the bacterial solution was inoculated into MHB following incubation for 48 hours. While the incubation, the bacterial amount was counted by plating each 0-, 3-, 6-, 9-, 12-, 24-, 36- and 48-hours later.
Statistical Analysis
The data were calculated as the mean and standard deviation per experimental group, and compared by an unpaired t-test. Statistical significance was set at P <0.05. All experiments were performed in duplicate on another day.
Results
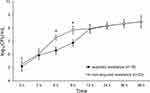
The first SXT-resistant strain was confirmed after 8 days; then a total of 18 strains (45%) had acquired resistance after 14 days (Figure 2). These 18 strains were confirmed as DfrB mutation, and the previously reported F98Y mutation was 11 out of 18 mutants (61%) (Table 1). In addition, previously unreported mutations L40I, F92L, T96I, and L141P were confirmed. The growth ability of 18 DfrB mutants after 6 hours was significantly low compared with the other 22 strains (P <0.05) (Figure 3). Moreover, seven of the 18 strains recovered susceptibility by the incubation without the drug and lost mutation (Day 28 in Table 1). The growth ability of these 7 mutants had decreased more than its parental strains (P <0.05) (Figure 4). Then, 7 strains that showed the same mutation by the second challenge of SXT (Day 35) acquired resistance again. In contrast, the other 11 strains-maintained resistance by the drug-free incubation. All mutations of DfrB in these 11 strains were F98Y, and they were maintained after 14 days of incubation (Day 28) (Table 1).
 |
Table 1 MIC and DfrB Mutation Point in 18 Isolates of Trimethoprim/Sulfamethoxazole-Resistant S. aureus |
Discussion
Despite the SXT-resistance rate indicating approximately 1% in the United States and Japan,18,19 45% of strains acquired resistance in this in vitro study. This was because the SXT challenge was performed at 14 days in vitro. SXT administration is generally completed from 5 to 7 days in skin infections caused by S. aureus, and therefore, DfrB mutation may not occur. Moreover, it is difficult to isolate the causative organism in the bone and joint infection for which SXT is administered for a long period of time.20 Therefore, these resistant strains might not be detected.
Because the 18 strains that acquired resistance in this study had significantly low growth ability 12 hours later, it is suggested that the initial stationary phase in the growth of the bacteria process was long. Trimethoprim has mutation inductivity,21 and its influence is dependent on the amount of exposure in the stationary phase.22 It was considered that the mutation was more likely to occur in the 18 strains because of continued SXT exposure in the long stationary phase. In addition, despite approximately 40% of DfrB mutants having recovered susceptibility, those showed resistance again by the second SXT challenge. Generally, the growth rate of the resistant strain is slower than that of the susceptible strain, which is the result of a gene mutation.23 In fact, the growth ability of the susceptibility to recovery strain was significantly decreased compared with its parental strain (P <0.05) (Figure 3). The resistant mutant will become dominant by the antibiotic selective pressure because only a mutant can survive. Moreover, as the wild type grows quickly if the selective pressure disappears, thus it seems to have recovered susceptibility.24 However, caution is recommended as hetero-resistant strains can become easily resistant.
The SXT-resistance rate is high in some regions (eg, Taiwan, Nigeria, and a few towns in Africa),25–27 and it is involved in spreading the strain harboring the dfrA, dfrG, and/or dfrK gene via companion and livestock animals.12,28–30 At the moment, the human-derived strain is rarely reported in the United States and Japan, but it will be necessary to monitor it closely. Furthermore, we reported that SXT-resistant small colony variants lurk in community strains,31 and these cannot be detected by a general bacterial test. These strains should also be kept in mind.
Conclusion
Forty-five percent of S. aureus clinical isolates became SXT-resistant through the 2-week in vitro challenge, and these strains have DfrB mutation. Thus, these mutants may be selected if SXT is administered over a 2-week period for S. aureus infection. To define these clinical problems, further clinical studies and trials including population analysis and AUC studies are required.
Ethical Approval
Not required, according to the Research Ethics Statement of the Ministry of Health, Labour and Welfare of Japan, because this study is basic research that used bacterial isolates only. Clinical isolates that were used in this study were collected and stocked by the Tohoku Infectious Diseases Society; therefore, we cannot access patient information.
Acknowledgment
We thank Dr. Akira Watanabe of Tohoku Infectious Disease Society, for he gifted S. aureus clinical isolates.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded internally.
Disclosure
All authors have no conflict of interest to declare.
References
1. DeLeo FR, Otto M, Kreiswirth BN, Chambers HF. Community-associated methicillin-resistant Staphylococcus aureus. Lancet. 2010;375:1557–1568. doi:10.1016/S0140-6736(09)61999-1
2. David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev. 2010;23:616–687. doi:10.1128/CMR.00081-09
3. Algammal AM, Hetta HF, Elkelish A, et al. Methicillin-Resistant Staphylococcus aureus (MRSA): one health perspective approach to the bacterium epidemiology, virulence factors, antibiotic-resistance, and zoonotic impact. Infect Drug Resist. 2020;13:3255–3265. doi:10.2147/IDR.S272733
4. Spengler G, Gajdács M, Donadu MG, et al. Evaluation of the antimicrobial and antivirulent potential of essential oils isolated from Juniperus oxycedrus L. ssp. macrocarpa aerial parts. Microorganisms. 2022;10(4):758. doi:10.3390/microorganisms10040758
5. Mazzarello V, Gavini E, Rassu G, et al. Clinical assessment of new topical cream containing two essential oils combined with tretinoin in the treatment of acne. Clin Cosmet Investig Dermatol. 2020;13:233–239. doi:10.2147/CCID.S236956
6. Bua A, Usai D, Donadu MG, et al. Antimicrobial activity of Austroeupatorium inulaefolium (H.B.K.) against intracellular and extracellular organisms. Nat Prod Res. 2018;32:2869–2871. doi:10.1080/14786419.2017.1385014
7. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52:e18–e55. doi:10.1093/cid/ciq146
8. Spellberg B, Lipsky BA. Systemic antibiotic therapy for chronic osteomyelitis in adults. Clin Infect Dis. 2012;54:393–407. doi:10.1093/cid/cir842
9. Paul M, Bishara J, Yahav D, et al. Trimethoprim-sulfamethoxazole versus vancomycin for severe infections caused by meticillin resistant Staphylococcus aureus: randomised controlled trial. BMJ. 2015;350:h2219. doi:10.1136/bmj.h2219
10. Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection. Ann Emerg Med. 2010;56:283–287. doi:10.1016/j.annemergmed.2010.03.002
11. Dale GE, Broger C, D’Arcy A, et al. A single amino acid substitution in Staphylococcus aureus dihydrofolate reductase determines trimethoprim resistance. J Mol Biol. 1997;266:23–30. doi:10.1006/jmbi.1996.0770
12. Nurjadi D, Olalekan AO, Layer F, et al. Emergence of trimethoprim resistance gene dfrG in Staphylococcus aureus causing human infection and colonization in sub-Saharan Africa and its import to Europe. J Antimicrob Chemother. 2014;69:2361–2368. doi:10.1093/jac/dku174
13. Clinical and Laboratory Standards Institute. Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria. CLSI Guideline M45.
14. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. CLSI Supplement M100.
15. Berti AD, Wergin JE, Girdaukas GG, Hetzel SJ, Sakoulas G, Rose WE. Altering the proclivity towards daptomycin resistance in methicillin-resistant Staphylococcus aureus using combinations with other antibiotics. Antimicrob Agents Chemother. 2012;56:5046–5053. doi:10.1128/AAC.00502-12
16. Dale GE, Then RL, Stüber D. Characterization of the gene for chromosomal trimethoprim-sensitive dihydrofolate reductase of Staphylococcus aureus ATCC 25923. Antimicrob Agents Chemother. 1993;37:1400–1405. doi:10.1128/AAC.37.7.1400
17. Saito M, Katayama Y, Hishinuma T, et al. “Slow VISA”, a novel phenotype of vancomycin resistance, found in vitro in heterogeneous vancomycin-intermediate Staphylococcus aureus strain Mu3. Antimicrob Agents Chemother. 2014;58:5024–5035. doi:10.1128/AAC.02470-13
18. Sader HS, Mendes RE, Streit JM, Flamm RK. Antimicrobial susceptibility trends among staphylococcus aureus isolates from U.S. hospitals: results from 7 years of the ceftaroline (AWARE) surveillance program, 2010 to 2016. Antimicrob Agents Chemother. 2017;61:e01043–17. doi:10.1128/AAC.01043-17
19. Watanabe S, Ohnishi T, Yuasa A, et al. The first nationwide surveillance of antibacterial susceptibility patterns of pathogens isolated from skin and soft-tissue infections in dermatology departments in Japan. J Infect Chemother. 2017;23:503–511. doi:10.1016/j.jiac.2017.05.006
20. Kavanagh N, Ryan EJ, Widaa A, et al. Staphylococcal osteomyelitis: disease progression, treatment challenges, and future directions. Clin Microbiol Rev. 2018;31:e00084–17. doi:10.1128/CMR.00084-17
21. Song LY, Goff M, Davidian C, et al. Mutational consequences of ciprofloxacin in Escherichia coli. Antimicrob Agents Chemother. 2016;60:6165–6172. doi:10.1128/AAC.01415-16
22. Ward WO, Swartz CD, Hanley NM, DeMarini DM. Transcriptional characterization of Salmonella TA100 in log and stationary phase: influence of growth phase on mutagenicity of MX. Mut Res. 2010;692:19–25. doi:10.1016/j.mrfmmm.2010.07.010
23. Holmes AH, Moore LS, Sundsfjord A, et al. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet. 2016;387:176–187. doi:10.1016/S0140-6736(15)00473-0
24. Durão P, Balbontín R, Gordo I. Evolutionary mechanisms shaping the maintenance of antibiotic resistance. Trends Microbiol. 2018;26:677–691.
25. Aires de Sousa M, Crisóstomo MI, Sanches IS, et al. Frequent recovery of a single clonal type of multidrug-resistant Staphylococcus aureus from patients in two hospitals in Taiwan and China. J Clin Microbiol. 2003;41:159–163. doi:10.1128/JCM.41.1.159-163.2003
26. Breurec S, Fall C, Pouillot R, et al. Epidemiology of methicillin-susceptible Staphylococcus aureus lineages in five major African towns: high prevalence of Panton-Valentine leukocidin genes. Clin Microbiol Infect. 2011;17:633–639. doi:10.1111/j.1469-0691.2010.03320.x
27. Olalekan AO, Schaumburg F, Nurjadi D, et al. Clonal expansion accounts for an excess of antimicrobial resistance in Staphylococcus aureus colonising HIV-positive individuals in Lagos, Nigeria. Int J Antimicrob Agents. 2012;40:268–272. doi:10.1016/j.ijantimicag.2012.05.016
28. Coelho C, de Lencastre H, Aires-de-Sousa M. Frequent occurrence of trimethoprim-sulfamethoxazole hetero-resistant Staphylococcus aureus isolates in different African countries. Eur J Clin Microbiol Infect Dis. 2017;36:1243–1252. doi:10.1007/s10096-017-2915-x
29. Donadu MG, Ferrari M, Mazzarello V, et al. No correlation between biofilm-forming capacity and antibiotic resistance in environmental Staphylococcus spp. In Vitro Results Pathogens. 2022;11:471. doi:10.3390/pathogens11040471
30. Giacinti G, Carfora V, Caprioli A, et al. Prevalence and characterization of methicillin-resistant Staphylococcus aureus carrying mecA or mecC and methicillin-susceptible Staphylococcus aureus in dairy sheep farms in central Italy. J Dairy Sci. 2017;100:7857–7863. doi:10.3168/jds.2017-12940
31. Sato T, Kawamura M, Furukawa E, Fujimura S. Screening method for trimethoprim/sulfamethoxazole-resistant small colony variants of Staphylococcus aureus. J Glob Antimicrob Resist. 2018;15:1–5. doi:10.1016/j.jgar.2018.05.008
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.