Back to Journals » Clinical Epidemiology » Volume 10
The right combination – treatment outcomes among HIV-positive patients initiating first-line fixed-dose antiretroviral therapy in a public sector HIV clinic in Johannesburg, South Africa
Authors Hirasen K , Evans D , Maskew M, Sanne IM, Shearer K, Govathson C, Malete G, Kluberg SA , Fox MP
Received 10 July 2017
Accepted for publication 8 September 2017
Published 18 December 2017 Volume 2018:10 Pages 17—29
DOI https://doi.org/10.2147/CLEP.S145983
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Henrik Sørensen
Kamban Hirasen,1 Denise Evans,1 Mhairi Maskew,1 Ian M Sanne,1–3 Kate Shearer,1 Caroline Govathson,1 Given Malete,1 Sheryl A Kluberg,4 Matthew P Fox1,4,5
1Health Economics and Epidemiology Research Office, Department of Internal Medicine, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; 2Right to Care, Johannesburg, South Africa; 3Clinical HIV Research Unit, Department of Internal Medicine, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; 4Department of Global Health, Boston University School of Public Health, Boston, MA, USA; 5Department of Epidemiology, Boston University School of Public Health, Boston, MA, USA
Background: Long-term antiretroviral therapy (ART) adherence is critical for achieving optimal HIV treatment outcomes. Fixed-dose combination (FDC) single-pill regimens, introduced in South Africa in April 2013, has simplified pill taking. We evaluated treatment outcomes among patients initiated on a FDC compared to a similar multi-pill ART regimen in Johannesburg, South Africa.
Methods: We conducted a retrospective cohort study of ART-naïve HIV-positive non-pregnant adult (≥18 years) patients without tuberculosis who initiated first-line ART on tenofovir and emtricitabine or lamivudine with efavirenz at Themba Lethu Clinic in Johannesburg, South Africa. We compared those initiated on a multi-pill ART regimen (3–5 pills/day; September 1, 2011–August 31, 2012) to those initiated on a FDC ART regimen (one pill/day; September 1, 2013–August 31, 2014). Treatment outcomes included attrition (combination of lost to follow-up and mortality), missed medical visits, and virologic suppression (viral load <400 copies/mL) by 12 months post-ART initiation. Cox proportional hazards models and Poisson regression were used to estimate the association between FDCs vs multiple pills and treatment outcomes.
Results: We included 3151 patients in our analysis; 2230 (70.8%) patients initiated multi-pill ART and 921 (29.2%) patients initiated on a FDC. By 12 months post-initiation, attrition (adjusted hazard ratio: 0.98; 95% CI: 0.77–1.24) was similar across regimen types (FDC vs multi-pill). Although not significant, patients on a FDC were marginally more likely to achieve viral suppression by 6 (adjusted relative rate [aRR]: 1.10; 95% CI: 0.99–1.23) and 12 months (aRR: 1.12; 95% CI: 0.92–1.36) on ART. Patients initiated on a FDC were significantly less likely to miss medical visits during the first 12 months of treatment (aRR: 0.66; 95% CI: 0.52–0.83).
Conclusion: Our results suggest FDCs may have a role to play in supporting patient adherence and medical monitoring through improved medical visit attendance. This may potentially improve treatment outcomes later on in treatment.
Keywords: antiretroviral therapy, fixed-dose combination, attrition, virologic suppression, adherence, South Africa
Introduction
Long-term adherence to antiretroviral therapy (ART) is critical for achieving optimal clinical outcomes among people living with HIV, as well as reducing the risk of transmission to uninfected partners.1–4 Regimen complexity, characterized by multiple pills, differing dosing times, as well as varying dosing instructions have been shown to be important factors contributing to suboptimal adherence.5,6 In turn, people with poor adherence have been identified to be at an increased risk for incomplete virologic suppression, development of drug resistance, disease progression, and death.7,8
While regimen complexity has been noted as a barrier to adherence, the introduction of fixed-dose combinations (FDCs) where one pill contains multiple active drugs has simplified pill taking. This is achieved through a reduction in pill burden in combination with simpler scheduling (once daily).9 Introduced to resource-limited settings in the early 2000s, FDCs were initially a combination of two active antiretroviral (ARV) drugs administered as one pill (e.g., Truvada®; Gilead Sciences, Inc., Foster City, CA, USA; emtricitabine (FTC) and tenofovir disoproxil fumarate [TDF]).9 Although not in widespread use at the onset, numerous clinical trials and observational cohort studies report improved patient satisfaction, quality of life, adherence and virologic suppression through these simplified regimens (both two and three active drugs administered in a FDC).10–12 While the immunologic and virologic effects of FDCs appear positive, there is still limited data on the effects of FDCs administered to individuals at scale, under routine clinical conditions.4
In April 2013, South Africa began initiating eligible first-line patients on a once-daily, single-tablet FDC ARV regimen of TDF, FTC, and efavirenz (EFV).13 To evaluate the impact of this policy change, we compared treatment outcomes among patients who initiated this FDC ARV regimen ≥5 months after FDCs became available, to patients who initiated a TDF, lamivudine (3TC), and EFV multi-pill ART regimen prior to FDC introduction at a large public sector HIV clinic in Johannesburg, South Africa.
Methods
Study design, site, and population
We conducted a retrospective cohort study of non-pregnant, non-tuberculosis (TB) patients initiating first-line ART at Themba Lethu Clinic, located at Helen Joseph Hospital in Johannesburg, South Africa.
At Themba Lethu, demographic, laboratory, and clinical data were captured on an electronic patient management system called TherapyEdge-HIV™ (Advanced Biological Laboratories, SA, Luxembourg).14 HIV care and treatment at Themba Lethu followed the South African ART Guidelines.15–19 After treatment initiation, patients were typically scheduled for medical follow-up visits at 1, 3, 6, and 12 months and then 6-monthly thereafter.16,20 During the study period, ART eligibility was based on a CD4 cell count ≤350 cells/mm³.17,18 Since the implementation of the 2010 national treatment guidelines, monitoring laboratory tests such as viral load tests are performed at 6 and 12 months post-initiation, and annually thereafter. Additionally, CD4 cell count tests are performed 12 months following ART initiation, and annually thereafter. Complete blood counts, hemoglobin, creatinine clearance, and liver function tests are performed at least annually.
Study population
The study population consisted of HIV-positive non-pregnant, non-TB, ART-naïve adults (≥18 years) initiating a triple combination, TDF-based regimen. We compare two groups: an unexposed multi-pill group who initiated TDF/3TC/EFV with 3–5 pills per day between September 1, 2011 and August 31, 2012, prior to the introduction of FDCs; and an exposed group who initiated a single-pill per day regimen (TDF/FTC/EFV) from September 1, 2013 to August 31, 2014, ≥5 months after the introduction of FDCs to allow for the clinic to transition and implement the policy change. Both groups were followed-up until 12 months post-ART initiation.
Study variables
We compared the multi-pill and FDC groups with respect to the following outcomes: 1) attrition (a combination of lost to follow-up [LTFU], defined as being >3 months late for the last scheduled visit with no subsequent visit and all-cause mortality/death, determined by family and/or hospital report as well as linkage to the South African National Vital Registration System in August 2014 for patients with a valid South African national identification number;21,22 2) missing a medical visit (0 vs ≥1) defined as being >7 days late for a scheduled medical visit;23 and 3) virologic suppression defined as a viral load <400 copies/mL at 6 and 12 months post-ART initiation (+/–3 months). Due to the relatively small number of patients having experienced LTFU or mortality across respective regimen types by 12 months, these outcomes were not assessed separately; instead LTFU and mortality were combined into attrition by 12 months (LTFU + all-cause mortality). For primary outcomes, person-time accrued from ART initiation to the earliest of: 1) attrition; 2) transfer out to another facility; 3) completed 12 months of follow-up, and when reporting total follow-up time, to the close of dataset (April 5, 2016).
Statistical analysis
Baseline demographic and clinical characteristics of all patients included in the cohorts were presented using medians with corresponding interquartile ranges (IQRs) for continuous variables, while categorical variables were presented as simple proportions along with a count of missing data. Primary outcomes were assessed using complete case analysis. Attrition and missed visits were measured by 12 months post-ART initiation, while virologic suppression was measured at both 6 and 12 months post-ART initiation (+/–3 months). Due to the variation in time to outcome (LTFU/mortality), Cox proportional hazards models were used to evaluate the relationship between FDCs vs multiple pills and attrition. Poisson regression was used to estimate the association between FDCs vs multiple pills for both missed medical visits and virologic suppression. Proportions and relative rates (RRs) of virologic suppression were calculated among only those with viral load tests at respective time points. Additionally, we conducted a sensitivity analysis to identify the impact of missing data. At both time points of viral load measurement, patients alive and in care with missing viral load tests were categorized as having suppressed and unsuppressed viral loads in two respective Poisson regression models. All baseline characteristics which resulted in a ≥±10% change in the primary exposure effect were included in the respective adjusted models. Additionally, potential confounders known through prior knowledge or hypothesized to be associated with respective outcomes were included in the adjusted models. Demographic and clinical characteristics considered a priori included; age, sex, CD4 cell count, and World Health Organization (WHO) stage (according to national guidelines, CD4 cell count and WHO stage are characteristics which determine ART initiation across regimen types and were consequently considered as a priori). Due to the setting of the clinic site (high altitude), hemoglobin levels were first adjusted down by 0.65 g/dL, and defined per sex for males as 1) no anemia (Hb ≥13 g/dL), 2) mild anemia (10< Hb <13 g/dL), 3) moderate anemia (8≤ Hb ≤10 g/dL), and 4) severe anemia (Hb <8 g/dL); and for females as 1) no anemia (Hb ≥12 g/dL), 2) mild anemia (10< Hb <12 g/dL), 3) moderate anemia (8≤ Hb ≤10 g/dL), and 4) severe anemia (Hb <8 g/dL).
Ethical approval
Ethical approval for the use of data was provided by the Human Research Ethics Committee (Medical) of the University of the Witwatersrand (M140201). The study protocol was reviewed by the Institutional Review Board of the University of the Witwatersrand who approved the collection of the data without informed consent and the use of an anonymous analytical data set.
Results
Demographic and clinical characteristics
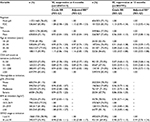
We included 3151 patients in our analysis. Overall, 2230 (70.8%) patients initiated multi-pill ART (September 1, 2011–August 31, 2012) and 921 (29.2%) patients initiated on a FDC (September 1, 2013–August 31, 2014). Table 1 presents the demographic and clinical characteristics of patients on each regimen type at initiation. The proportion of females was similar between patients taking multiple pills and those on FDCs (61.1 vs 54.3%) as was the median age at initiation (37.8 years for both groups) and median hemoglobin at initiation (11.7 vs 11.9 g/dL). Patients on a multi-pill regimen presented a marginally higher median CD4 cell count at ART initiation compared to those on a FDC (175.5 vs 158.0 cells/mm³), while a lower proportion of the former initiated with CD4 cell counts >350 cells/mm³ (4.3 vs 10.8%). Levels of creatinine clearance, body mass index (BMI), and WHO clinical stage were similar across groups. By 12 months post-ART initiation, more than 75% of patients were still alive in care. Lost to follow-up, mortality, and transfer-out were 12, 6, and 7%, respectively. Overall, 16% of patients missed one or more medical visits by 12 months on ART, while more than 75% of patients suppressed their viral load by 6 and 12 months, respectively.
Attrition by 12 months on ART
By 12 months on ART, the overall incidence of attrition was 17.5% (552/3151) (11.9% were LTFU and 5.6% had died). The attrition rate within the first year of ART was 20.3/100 person-years. This was lower among those on FDCs (17.6/100 person-years) compared to those taking multiple pills (21.5/100 person-years). Table 2 shows the crude hazard ratio (HR) and adjusted HR (aHR) estimates of attrition by 12 months post-ART initiation. While those on FDCs had a reduced risk of attrition in crude analyses (HR: 0.82; 95% CI: 0.68–1.00), aHRs reveal that patients on FDCs have approximately the same risk of attrition by 12 months compared to those on multi-pills (aHR: 0.98; 95% CI: 0.77–1.24). Males (aHR: 1.49; 95% CI: 1.17–1.90), those with a lower CD4 cell count (0–50 vs ≥201 cells/mm³, aHR: 2.29; 95% CI: 1.69–3.12 and 51–100 vs ≥201 cells/mm³, aHR: 1.48; 95% CI: 1.01–2.16), patients with advanced anemia (moderate vs none, aHR: 1.71; 95% CI: 1.22–2.39) and (severe vs none, aHR: 2.42; 95% CI: 1.56–3.75), as well as those with low BMI (<18.5 vs 18.5–24.9 kg/m2, aHR: 1.42; 95% CI: 1.07–1.87) were more likely to be lost from care or die. In contrast, patients with higher BMI were protected from attrition (≥30 vs 18.5–24.9 kg/m2, aHR: 0.57; 95% CI: 0.33–0.96).
Additionally, when looking specifically at LTFU by 12 months on treatment, no significant effects were observed across regimen types (FDC vs multi-pill, aHR: 1.02; 95% CI: 0.76–1.36) (Table S1). Similarly, no significant effects across regimen types were noted for all-cause mortality by the same time point (FDC vs multi-pill, aHR: 0.97; 95% CI: 0.65–1.45) (Table S2).
Missed medical visits by 12 months on ART
Table 3 shows the crude RR and adjusted RR (aRR) estimates of missed medical visits by 12 months on ART. At this time point, a smaller proportion of those taking FDCs (11.3%) missed at least one medical visit compared to those taking multiple pills (17.5%). Similarly, in adjusted analyses, patients initiated on a FDC had a lower risk of missing at least one medical visit (aRR: 0.66; 95% CI: 0.52–0.83). Compared to their female counterparts, males were ~30% more likely to miss visits (aRR: 1.31; 95% CI: 1.07–1.60). The risk of missing visits in the first 12 months on treatment reduced with increasing age as older patients were less likely to miss at least one medical visit (≥55 vs 18–24, aRR: 0.42; 95% CI: 0.21–0.83).
When looking specifically at ARV pick-up visits during the first 12 months on treatment, a similar protective effect of FDCs in missing visits was observed (aRR: 0.57; 95% CI: 0.47–0.70) (Table S3).
Viral load suppression at 6 and 12 months
Table 4 shows the crude and aRR estimates of viral load suppression at 6 and 12 months post-ART initiation. At 6 months, 70% (647/921) of those who initiated FDC treatment vs 66% (1465/2230) of the multi-pill group had viral load tests. At this time point, virologic suppression was marginally higher among those taking FDCs (83 vs 77%; aRR: 1.10; 95% CI: 0.99–1.23). While not significant in the multivariate analysis, compared to females, males were less likely to achieve virologic suppression earlier in treatment (75.1 vs 80.8%; aRR: 0.93; 95% CI: 0.84–1.04). In relation to age group, older patients were more likely to have suppressed their viral load by 6 months on treatment (≥55 vs 18–24, aRR: 1.16; 95% CI: 0.85–1.59). Additionally, patients with lower CD4 cell counts were less likely to have suppressed viral loads at this time (0–50 vs ≥201, aRR: 0.90; 95% CI: 0.77–1.05), (51–100 vs ≥201, aRR: 0.89; 95% CI: 0.75–1.06), and (101–200 vs ≥201, aRR: 0.93; 95% CI: 0.82–1.06).
At 12 months, 31% (220/717) of those taking FDCs vs 33% (553/1657) of those taking multiple pills had viral load tests. Similar to viral load suppression at 6 months, patients on a FDC were marginally more likely to achieve viral suppression by 12 months on treatment (aRR: 1.12; 95% CI: 0.92–1.36). Young and middle-aged patients were less likely to suppress at this time point (25–34 vs 18–24, aRR: 0.93; 95% CI: 0.59–1.47) and (35–54 vs 18–24, aRR: 0.92; 95% CI: 0.59–1.43), respectively. As observed in the first 6 months, by 12 months patients with lower CD4 cell counts were also less likely to have suppressed their viral load (0–50 vs ≥201, aRR: 0.88; 95% CI: 0.68–1.14), (51–100 vs ≥201, aRR: 0.83; 95% CI: 0.60–1.14), and (101–200 vs ≥201, aRR: 0.90; 95% CI: 0.73–1.12)
Sensitivity analyses revealed a significant difference in suppression at 6 months among patients on a FDC, missing viral loads categorized as “suppressed”, aRR: 1.07; 95% CI: 0.97–1.18 vs “unsuppressed”, aRR: 1.15; 95% CI: 1.03–1.28 (Table S4). However, no difference was observed by 12 months, missing viral loads categorized as “suppressed”, aRR: 1.04; 95% CI: 0.94–1.15 vs “unsuppressed”, aRR: 1.01; 95% CI: 0.83–1.23.
Discussion
Currently, there are a limited number of studies focusing specifically on the effects of active ARV drugs administered as separate pills compared to those same active drugs administered in a FDC.9 Thus, the current study helps fill a critical gap in literature. In this study, we followed two groups of patients initiated on either a multi-pill or FDC regimen and assessed treatment outcomes 12 months post-ART initiation.
While the crude rate of attrition was somewhat lower among patients on a FDC, adjusted analyses revealed no significant differences in the risk of this outcome across regimen types 12 months post-ART initiation. Thereafter, compared to traditional multi-pill regimens, FDCs may not have a noticeable effect on patients’ ability to remain alive and in care during the first 12 months of treatment. This early phase of treatment may be considered important as the behavioral challenges associated with starting a life-long treatment program are assumed to be at their highest. While adverse drug reactions (ADRs), treatment tolerability, clinic attendance, development of coinfections, concomitant treatments, and treatment/pill fatigue have been identified as barriers to adherence, cumulative time on treatment has also been associated with decreases in adherence levels.5,6,9,24–26 It is at this time, later on in treatment, where a simplified, single-pill per day regimen may be more effective than a multi-pill regimen (each with varying dosing instructions serving to increase patient burden). Conversely, a FDC may be restrictive in its ability to form part of a holistic treatment plan which addresses coinfections. Limitations in single-drug substitutions may limit the use of FDCs later on in treatment, either periodically, when substitutions are needed, or more permanently.
As with attrition, there were no significant differences in the risk of virologic suppression among patients on a FDC compared to those on multi-pills. This was observed at both 6 and 12 months where patients on a FDC presented marginally higher rates of suppression with no discernible differences in risk (FDCs: 10 and 12% more likely to suppress at 6 and 12 months, respectively). Although numerous studies and randomized controlled trials (RCTs) evaluating the effects of FDCs (either partial or full) on virologic suppression (varying definitions/thresholds and durations of follow-up) have documented higher rates of suppression among patients on FDCs compared to those on multi-pill regimens,27 many of these studies examined virologic suppression across two non-identical regimens or among treatment-experienced patients, including those who switched to a FDC after initiating multi-pill therapy. Therefore, among treatment-naïve patients, comparing regimens similar in structure and dose in routine clinical care, the effects of pill number may not be a strong indication/predictor of virologic suppression.
During the study period (throughout enrolment of the multi-pill and FDC cohorts), improvements in adherence counseling and tracing initiatives among other interventions may have facilitated increasing levels of adherence and declining rates of LTFU. Specifically, during the enrolment of the FDC cohort, an automated pharmacy dispensing system was introduced at the study site. Although the impact of this system on patient treatment outcomes was not directly assessed, patient waiting times during medication collection were noticeably reduced. This may have contributed specifically to the reduction in missed ARV visits among patients on a FDC regimen (Table S3). However, even when looking specifically at missed medical visits in the first 12 months of treatment, compared to the multi-pill cohort, patients on a FDC were 30% less likely to miss this type of visit. While the direct mechanism/s through which a reduced pill count may facilitate improved clinical/medical visit attendance need to be further explored, the benefits of increased monitoring among FDC patients may in turn lead to improved treatment outcomes later on in treatment.
Although focusing on more direct and indirect measures (pill counts, self-report) of adherence rather than proxy measures (missed visits), numerous studies have documented increases in adherence associated with FDCs.12,28,29 Additionally, randomized trials have also documented the benefits of FDCs in adherence to ART including improvements in correct dosing and timing.30
Therefore, reduced pill counts and simplified pill taking, which improve treatment adherence, may ensure prolonged first-line treatment as well as prevent treatment failure and switching to more expensive and potentially limited second- and third-line regimens in the future.
Limitations
Previous studies focusing on ART medication simplification tend to report adherence levels as a primary outcome. These often include self-report measures and unannounced pill counts. Unfortunately, these data are not routinely collected at the treatment site and could not be included as a potential outcome. We use missed medical visits as a proxy of adherence and are unable to provide a robust and reliable measure of this outcome. Follow-up studies examining the effects of FDCs on more direct adherence measures as well as the mechanisms through which a reduced pill count may improve clinic attendance are needed. Additionally, we were unable to comment on patient preferences, experiences, and quality of life with regard to regimen type. However, accurate measurements of treatment outcomes may serve as a strong indicator of the effects of FDCs.
While we were unable to compare the outcomes of patients on regimens with identical active drugs (TDF/FTC/EFV [3–5 pills per day] vs TDF/FTC/EFV [1 pill per day]),10 the documented interchangeability of FTC and 3TC assures the clinical validity of reported outcomes.13 In turn, this ensures that the observed effects may be attributed to the difference in pill count and dosing instructions opposed to significant variation of active agents across respective regimen types (multi-pill vs FDC).
Patients enrolled in the FDC and multi-pill cohorts were enrolled in two mutually exclusive time periods. This aspect of the study design was a function of the national treatment guideline changes between the study time periods and ensured two distinct treatment groups. While the non-overlapping nature of our respective cohorts may allow direct regimen comparisons, it may create confounding through changes or improvements in programmatic conditions between time periods. Programmatic changes (e.g., tracing initiatives, automated pharmacy dispensing, etc.) could have potentially impacted treatment outcomes investigated here.
Lastly, in this study, we were only able to observe treatment outcomes within the first 12 months of ART initiation. Critical to treatment success, adherence is a fluid process, influenced by a multitude of factors including socioeconomic status, health and treatment-related elements as well as behavioral tendencies.31,32 Consequently, a larger cohort with longer follow-up time is needed to identify longer-term outcomes which may differ from the initial effects of treatment initiation up to 1 year on treatment.
Conclusion
FDC ART may be seen as a major advancement in the treatment of HIV-positive individuals. At the center of this simplified regimen is the facilitation of a reduced pill burden which has documented far reaching impacts, not only on clinical treatment outcomes but also on patient-centered outcomes such as quality of life. While the findings from this study may not, for the most part, illustrate these well-documented positive impacts of FDCs on HIV treatment outcomes identified in current literature, it is one of the first studies in Africa, particularly South Africa, which effectively examines the difference in outcomes between patients initiated on a single tablet first-line ART regimen compared to patients on a similar regimen administered as multiple drugs. We find that under programmatic conditions, FDCs do not significantly decrease rates of attrition or support noteworthy increases in virologic suppression compared to a multi-pill regimen. At the very least, these outcomes are similar regardless of the regimen type. However, FDCs may have a role to play in supporting patient adherence and monitoring through improved clinic attendance via medical visits. We find patients initiating ART on a FDC to be significantly less likely to miss medical visits in the first 12 months on treatment.
Acknowledgments
This study was made possible by the generous support of the American people through cooperative agreement AID 674-A-12-00029 from the United States Agency for International Development (USAID) South Africa. The contents of the article are the responsibility of the authors and do not necessarily reflect the views of USAID or the US Government. The funders had no role in the study design, collection, analysis, and interpretation of the data; in the writing of the report; approval of the manuscript; or in the decision to submit the paper for publication.
KH, DE, MM, IMS, KS, CG, GM, SAK, and MPF were supported through USAID cooperative agreement number 674-A-12-00029 to the Health Economics and Epidemiology Research Office. Additional support to KS was provided by the National Institutes of Health (T32AI102623).
Author contributions
IMS conceived the study. GM, CG, KS, and KH were responsible for data management (data access and cleaning). KH and DE designed the analysis while KH performed statistical analysis and wrote respective drafts of the manuscript. MM and IMS helped with the clinical interpretation of results. DE, MM, IMS, KS, CG, GM, SAK, and MPF critically reviewed the analysis and edited the manuscript. All the authors read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Attia S, Egger M, Muller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS (London, England). 2009;23(11):1397–1404. | ||
Cohen MS, McCauley M, Gamble TR. HIV treatment as prevention and HPTN 052. Current opinion in HIV and AIDS. 2012;7(2):99–105. | ||
De Cock KM, Gilks CF, Lo YR, Guerma T. Can antiretroviral therapy eliminate HIV transmission? Lancet (London, England). 2009;373(9657):7–9. | ||
Sax PE, Meyers JL, Mugavero M, Davis KL. Adherence to antiretroviral treatment and correlation with risk of hospitalization among commercially insured HIV patients in the United States. PloS one. 2012;7(2):e31591. | ||
Stone VE, Jordan J, Tolson J, Miller R, Pilon T. Perspectives on adherence and simplicity for HIV-infected patients on antiretroviral therapy: self-report of the relative importance of multiple attributes of highly active antiretroviral therapy (HAART) regimens in predicting adherence. J Acquir Immune Defic Syndr. 2004;36(3):808–816. | ||
van Galen KA, Nellen JF, Nieuwkerk PT. The effect on treatment adherence of administering drugs as fixed-dose combinations versus as separate pills: systematic review and meta-analysis. AIDS Res Treat. 2014;2014:967073. | ||
Fielden SJ, Rusch ML, Yip B, et al. Nonadherence increases the risk of hospitalization among HIV-infected antiretroviral naive patients started on HAART. J Int Assoc Physicians AIDS Care (Chic). 2008;7(5):238–244. | ||
Mitiku H, Abdosh T, Teklemariam Z. Factors affecting adherence to antiretroviral treatment in harari national regional state, Eastern Ethiopia. ISRN AIDS. 2013;2013:960954. | ||
Ramjan R, Calmy A, Vitoria M, et al. Systematic review and meta-analysis: patient and programme impact of fixed-dose combination antiretroviral therapy. Trop Med Int Health. 2014;19(5):501–513. | ||
Airoldi M, Zaccarelli M, Bisi L, et al. One-pill once-a-day HAART: a simplification strategy that improves adherence and quality of life of HIV-infected subjects. Patient Prefer Adherence. 2010;4:115–125. | ||
Bangsberg DR, Ragland K, Monk A, Deeks SG. A single tablet regimen is associated with higher adherence and viral suppression than multiple tablet regimens in HIV+ homeless and marginally housed people. AIDS. 2010;24(18):2835–2840. | ||
Sterrantino G, Santoro L, Bartolozzi D, Trotta M, Zaccarelli M. Self-reported adherence supports patient preference for the single tablet regimen (STR) in the current cART era. Patient Prefer Adherence. 2012;6:427–433. | ||
Clinicians Society SH. Fixed-dose combination for adults accessing antiretroviral therapy. 2013;14(1):41–43. | ||
Fox MP, Maskew M, MacPhail AP, et al. Cohort profile: the Themba Lethu Clinical Cohort, Johannesburg, South Africa. Int J Epidemiol. 2013;42(2):430–439. | ||
National Department of Health Republic of South Africa. National Antiretroviral Treatment Guidelines. 1st edn. Pretoria, South Africa, 2004. | ||
National Department of Health Republic of South Africa. Clinical Guidelines for the Management of HIV & AIDS in Adults and Adolescents. South Africa, 2010. | ||
National Department of Health Republic of South Africa. Circular on New Criteria for Initiating Adults on ART at CD4 Count of 350 cells/mL and Below. South Africa, 2011. | ||
National Department of Health Republic of South Africa. The South African Antiretroviral Treatment Guidelines. South Africa, 2013. | ||
National Department of Health Republic of South Africa. National Consolidated Guidelines – For the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults. South Africa, 2015. | ||
Brennan AT, Shearer K, Maskew M, Long L, Sanne I, Fox MP. Impact of choice of NRTI in first-line antiretroviral therapy: a cohort analysis of stavudine vs. tenofovir. Trop Med Int Health. 2014;19(5):490–498. | ||
Brennan AT, Maskew M, Sanne I, Fox MP. The interplay between CD4 cell count, viral load suppression and duration of antiretroviral therapy on mortality in a resource-limited setting. Trop Med Int Health. 2013;18(5):619–631. | ||
Shearer K, Maskew M, Ajayi T, et al. Incidence and predictors of herpes zoster among antiretroviral therapy-naive patients initiating HIV treatment in Johannesburg, South Africa. Int J Infect Dis. 2014;23:56–62. | ||
Brennan AT, Maskew M, Sanne I, Fox MP. The importance of clinic attendance in the first six months on antiretroviral treatment: a retrospective analysis at a large public sector HIV clinic in South Africa. J Int AIDS Soc. 2010;13(1):1. | ||
Li H, Marley G, Ma W, et al. The role of ARV associated adverse drug reactions in influencing adherence among HIV-infected individuals: a systematic review and qualitative meta-synthesis. AIDS Behav. 2017;21(2):341–351. | ||
Lima VD, Harrigan R, Bangsberg DR, et al. The combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality over time. J Acquir Immune Defic Syndr (1999). 2009;50(5):529. | ||
Shuper PA, Joharchi N, Irving H, et al. Differential predictors of ART adherence among HIV-monoinfected versus HIV/HCV-coinfected individuals. AIDS care. 2016;28(8):954–962. | ||
Hodder SL, Mounzer K, DeJesus E, et al. Patient-reported outcomes in virologically suppressed, HIV-1–infected subjects after switching to a simplified, single-tablet regimen of Efavirenz, Emtricitabine, and Tenofovir DF. AIDS Patient Care STDs. 2010;24(2):87–96. | ||
Cocohoba JM, Murphy P, Pietrandoni G, Guglielmo BJ. Improved antiretroviral refill adherence in HIV-focused community pharmacies. J Am Pharmacists Assoc. 2012;52(5):e67–73. | ||
Manfredini V, Vigano A, Murri R et al. One-pill once a day HAART: Simplification strategy maintaining adherence, efficacy and improving physical and psychological outcomes in a cohort of HIV-infected adolescents and youths. Italian Conference on AIDS and Retroviruses, Italy 27-29 March 2011. | ||
Maitland D, Jackson A, Osorio J, Mandalia S, Gazzard BG, Moyle GJ. Switching from twice-daily abacavir and lamivudine to the once-daily fixed-dose combination tablet of abacavir and lamivudine improves patient adherence and satisfaction with therapy. HIV Med. 2008;9(8):667–672. | ||
Kleeberger CA, Phair JP, Strathdee SA, Detels R, Kingsley L, Jacobson LP. Determinants of heterogeneous adherence to HIV-antiretroviral therapies in the Multicenter AIDS Cohort Study. J Acquir Immune DeficSyndr. 2001;26(1):82–92. | ||
Vervoort SC, Borleffs JC, Hoepelman AI, Grypdonck MH. Adherence in antiretroviral therapy: a review of qualitative studies. Aids. 2007;21(3):271–281. |
Supplementary materials
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.