Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 14
The Relevance of Regenerating Gene 1a Polymorphisms to Radiation Sensitivity and Survival of Nasopharyngeal Carcinoma Receiving Radiotherapy in a Southern Chinese Population
Authors Xing HJ , Chen XD, Sun HX, Dai YZ, Han YF, Chen HB, Liu F
Received 7 July 2021
Accepted for publication 28 September 2021
Published 6 November 2021 Volume 2021:14 Pages 1403—1413
DOI https://doi.org/10.2147/PGPM.S328285
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Martin H Bluth
Hai-Jie Xing,1,*,2 Xiang-Dong Chen,3,* Hong-Xia Sun,4,* Yao-Zhang Dai,5,* Yao-Feng Han,6,* Hai-Bo Chen,7,* Feng Liu8,9,*
1Department of Otorhinolaryngology, Head and Neck Surgery, University of Chinese Academy of Sciences, Shenzhen Hospital, Shenzhen, 518106, People’s Republic of China; 2Department of Otorhinolaryngology Head and Neck Surgery, Affiliated Xinhua Hospital of Hainan Medical Colleage, Haikou, 570311, People’s Republic of China; 3Department of Otolaryngology, Head and Neck Surgery, Affiliated General Hospital of Shenzhen University, Shenzhen, 518106, People’s Republic of China; 4Wuhan Medical Science Research Institution, Wuhan, 430013, People’s Republic of China; 5Department of Throat, Head and Neck Surgery, Affiliated Otolaryngological Hospital, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, 450052, People’s Republic of China; 6Department of Epidemiology, Public Health College of Xiamen University, Xiamen, 361005, People’s Republic of China; 7Clinical Laboratory, Affiliated Xinhua Hospital of Hainan Medical Colleage, Haikou, 570311, People’s Republic of China; 8Department of Endocrine Oncology, University of Chinese Academy of Sciences, Shenzhen Hospital, Shenzhen, 518106, People’s Republic of China; 9Department of Medical Imaging Centre, The First Affiliated Hospital, Jinan University, Guangzhou, 510630, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hai-Jie Xing
Department of Otorhinolaryngology, Head and Neck Surgery, University of Chinese Academy of Sciences, Shenzhen Hospital, Shenzhen, 518106, People’s Republic of China
Tel/Fax +86-755-27548815
Email [email protected]
Xiang-Dong Chen
Department of Otolaryngology, Head and Neck Surgery, Affiliated General Hospital of Shenzhen University, Shenzhen, 518106, People’s Republic of China
Tel/Fax +86-755-27548815
Email [email protected]
Objective: Gene polymorphism is closely related to tumor development, therapeutic response and prognosis. The relationship between regenerating gene 1A (Reg1A) polymorphism and nasopharyngeal carcinoma (NPC) is unclear. This retrospective study aimed to analyze the association between Reg1a polymorphisms and metastasis, radiation sensitivity and survivals in patients with NPC.
Methods: A total of 308 patients who had received radiotherapy at the Affiliated Xinhua Hospital, Hainan Medical College, between January 2010 and December 2018 with NPC, were enrolled for assessment of Reg1a polymorphisms through direct DNA sequencing.
Results: In the polymorphism of gene REG1A, patients with rs10165462 20CC genotype had later T stages (OR = 4.051, 95% CI: 1.775– 9.244, P = 0.001), whereas carriers with rs12072 2922CC genotype had earlier T stages (OR = 1.891, 95% CI: 1.018– 3.514, P = 0.044) after adjustments for age and gender, respectively. Among rs10165462 20 C/T polymorphism, 20TT wild-type was associated with better radiation response (P = 0.0019), and multivariate analysis showed that it was the only genotype of polymorphism that was significantly associated with better radiation response (OR = 0.265, 95% CI: 0.096– 0.727, P = 0.01). Patients with the 20TT wild-type had a better five-year overall survival (60.9%) rate and five-year progression-free survival (60.8%) than those with the 20CC genotype (41.8% and 39.4%, P = 0.01 and P = 0.004, respectively). Patients with variant alleles (CC + CT) had significantly poorer OS (45.2%) and PFS (41.8%) compared with wild-type (TT) carriers (60.9% and 60.8%; P = 0.037 and P = 0.015, respectively). As for rs12072, patients with variant alleles (TT + TC) had significantly adverse OS and PFS compared with wild-type (CC) carriers (62.5% vs 44.8% and 62.5% vs 42.9%; P = 0.024 and P = 0.027, respectively). Cox regression showed that rs10165462 20CT was the only prognostic factor for OS (HR = 1.642, 95% CI 1.038– 2.598, P = 0.034) and PFS (HR = 1.705, 95% CI 1.080– 2.692, P = 0.022).
Conclusion: Reg1a polymorphisms may be a predictor of radiation response, local invasion, OS and PFS in patients with NPC who undergo radiotherapy treatment.
Keywords: regenerating gene 1a, polymorphisms, radiation, sensitivity, nasopharyngeal, survival
Introduction
Nasopharyngeal carcinoma (NPC) is the most common cancer of the head and neck in the south of China.1 More than 90% of NPC cases are diagnosed histologically as undifferentiated carcinoma. The five-year overall survival (OS) rate for NPC is around 70%. Recurrence and metastasis result from radiation resistance and are the main barriers to survival.2 Although treatment (radiotherapy with or without chemotherapy)3,4 is based on a patient’s TNM stage rather than their genetic composition, significant inter-individual variability has been observed in radiation sensitivity and prognosis, which suggests that genetic susceptibility plays a role, and that the identification of the biomarkers of NPC may be useful for individual radiotherapy.5,6 Since research into novel biomarkers could help predict the curability of individual radiotherapy, it is, therefore, of vital importance.
Growing evidence suggests that genetic polymorphisms, most often single nucleotide polymorphisms (SNPs), influence individual sensitivity to radiotherapy and prognosis in a variety of tumors, although the underlying mechanisms are unclear.7,8 P53 polymorphism may influence individual responsiveness to chemo-radiotherapy (CRT) for advanced head and neck cancer, ovarian cancer, and cervical cancer.9 DNA repair gene (X-ray repair cross-complementing 1, XRCC1; breast cancer susceptibility gene 1, BRCA1; and excision repair cross-complementing group 1, ERCC1) polymorphisms could alter DNA repair capacity and are, therefore, associated with CRT response and survival in lung cancer.10 The variant alleles of XRCC1 Arg399Gln are significantly associated with poor survival rates and the absence of pathologic complete response (pCR).11,12 ERCC1 (rs11615) C118T and C allele, for example, could predict the response to radiotherapy and chemotherapy as a basis for the individualized therapy of advanced esophageal cancer.13–16 They could also be used to help identify a subgroup of alleles that suggests patients with NPC who receive either radiotherapy (RT) or cisplatin plus RT have an excellent prognosis.17
Other studies have shown a close relationship between genotype and therapeutic response. For example, a polymorphism within the promoter of the transforming growth factor-β (TGF-β) gene has been found to increase radiation sensitivity in lung cancer,18 and coronin-2A rs1985859 and the putative marker FAM101A rs7955740 have been used to predict radiation sensitivity to preoperative chemo-radiotherapy (pCRT) in rectal cancer patients.19 In addition, ataxia telangiectasia-mutated gene (ATM) polymorphisms in the heterozygote state have been found to heighten clinical radiation sensitivity and clinical radioprotection in breast cancers.20 The same result was also found in other studies.21–23
In a recent study, polymorphisms in the promoter region of miR-34b/c rs4938723 significantly affected the CRT efficacy for locally advanced ESCC.24 It is clear that SNPs and SNP sets contribute to radiation sensitivity, so genetic variants hold promise as markers of individual radiation sensitivity.25
The regenerating gene (Reg) was originally isolated in a study that regenerated rats’ pancreatic islets and examined the acute phase reactants, lectins, anti-apoptotic factors, and growth factors for pancreatic β-islet cells and epithelial cells in the digestive system.26 Reg1a is a member of the human Reg1 family (Reg I–IV). Initial studies indicated that it is involved in inflammatory diseases27 and gastroenterological carcinogenesis.28 Further studies demonstrated that Reg1a expression is associated with CRT response in patients with ESCC.29 Our previous research showed that overexpression of Reg1a led to variations in the local progression and poor prognosis of NPC;30 moreover, Reg1a (rs12072) polymorphisms have been found to increase the risk of developing NPC.31 Therefore, we hypothesized that there might be a link between the functional variants in the Reg1a gene and radiation sensitivity and prognosis in patients with NPC. The present research details a retrospective study that was conducted to verify the association between Reg1a polymorphisms, radiation sensitivity, and survival in southern Chinese patients with NPC. It is hoped that the findings of the study can provide a greater understanding of genetic biomarkers for radiation sensitivity.
Patients and Methods
Patients
A total of 308 patients with previously untreated, non–distant metastatic, newly histologically confirmed NPC who had received radiotherapy at the Affiliated Xinhua Hospital, Hainan Medical College, between January 2010 and December 2018 were enrolled in this retrospective study. The median age was 49.2 years (range 22–74 years) and the median follow-up time was 39.1 months (range 9.8–99.96 months). Staging and grading were employed according to current standard classifications.32,33 Table 1 summarizes the patient and clinical baseline data.
 |
Table 1 Clinical and Pathological Characteristics, Responses to Radiotherapy, and Genotyping Analysis of Enrolled Patients |
Clinical follow-up data were obtained through patients’ medical records, for which we obtained written informed consent from each patient or an immediate family member. The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of the Affiliated Xinhua hospital of Hainan Medical Colleage and informed consent was taken from all the patients.
Treatment
All patients received radical radiotherapy through three-dimensional conformal intensity modulated radiation therapy (3DCRT). The median radiation dose was 72 Gy (range 70–78 Gy) at the primary site and 64.20 Gy (range 60–72 Gy) for lymph node metastasis, dosed at a daily fraction of 1.8 to 2 Gy five times per week. All patients were followed up for more than three months and underwent computerized tomography (CT) scans and nasopharyngeal/neck and nasopharyngeal endoscopies in order to evaluate treatment response during follow-up. Response was assessed three months after completion of radiotherapy.
Response Evaluation
Tumor response was defined, based on the new Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1) from the World Health Organization (WHO), as complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD). The objective response rate was defined by CR.
DNA Extraction and Genotyping
Based on the DNA sequences (GenBank ID: 5967) of the human Reg1a gene, six pairs of specific polymerase chain reaction (PCR) primers, covering the six exons, were designed using Primer Premier v5.0 software to amplify the exons (see Table 2). DNA extraction and genotyping was performed as previously described.31 In brief, genomic DNA was extracted from pre-treatment paraffin-embedded NPC tissue for genotyping by direct sequencing.
 |
Table 2 Primer Sequences of PCR for the Reg1α Gene |
Amplification and Sequencing
The first PCR reaction was carried out with 2.5 μL of 10 × Good’s buffer (Applied Biosystems, USA), 200 μM of dNTP, 1.5 μM of primer, 1.25 U of AmpliTaq GoldTM Polymerase (Applied Biosystems, USA), and about 20 ng of DNA (25 μL total volume). Thermal cycling was performed in a Veriti system (Applied Biosystems, USA) and consisted of an initial 5-minute denaturation step at 95°C, 35 cycles of 30 seconds at 95°C, 30 seconds at 58°C, and a 40-second extension step followed by 5 minutes at 72°C. The second PCR was the same as the first except that about 2 μL product of the first amplification was used instead of 20 ng of DNA. The final PCR products were cleaned up and sequenced.
Statistical Analysis
Genotype and minor allele frequency for Reg1a were counted, and the genotyped data were analyzed using the PLINK statistical package (http://pngu.mgh.harvard.edu/~purcell/plink), version 1.07.34 The genotypes in the control and case groups were tested for deviation from the Hardy-Weinberg equilibrium (HWE) using Fisher’s exact test, and the odds ratio (OR) for each genotype was calculated. Analysis of single markers was performed using the PLINK toolset. The associations between SNP genotype and different clinic-pathological characteristics and radiation response were analyzed using a chi-square test or Fisher’s exact test. Univariate and multivariate logistic regressions were conducted to evaluate the association of T stage and radiation response rate with variant genotypes (unconditional or after adjustment for clinic-pathological characteristics) and presented as odds ratio (OR) and 95% confidence interval (CI). Linkage disequilibrium (LD) analyses, haplotype analyses and LD block construction were carried out using Haploview version 3.32 (Daly Lab, Broad Institute, MA, USA).35
The primary endpoint was progression-free survival (PFS), and the secondary endpoint was OS. The duration of time to loco-regional relapse was measured from the date of the start of radiotherapy until the failure of documented treatment. PFS was assessed from the start of treatment to the first defined event of failure, ie, loco-regional relapse and/or distant metastasis in patients who completely responded to radiation therapy, as well as definite progression of disease in patients who partially responded. The duration of OS was calculated from the start of radiotherapy until death due to any cause or until the date of the last follow-up visit for patients who are still alive.
A Kaplan–Meier curve and Log rank test were used to compare OS and PFS in Reg1a SNPs. Cox proportional hazards modeling was conducted to evaluate prognostic factors for OS and PFS. Two-sided P values < 0.05 were considered statistically significant. The statistical analysis was performed using SPSS 19.0 (IBM, Armonk, NY, USA).
Results
Recurrence, Metastasis and Progression During the Follow-Up Period
During the follow-up period, recurrence and metastasis occurred in 17 (16.88%) cases (local relapse 4 cases, regional relapse 3 cases, local-regional relapse 4 cases, and distant metastasis 6 cases), and 27 cases that were assessed with resistance to radiotherapy were regarded as a progression of the disease. Analysis was not performed due to the small size of this category.
Detection of Reg1a Polymorphisms
Rs10165462 (20C/T; exon 1), rs117580393 (369G/T; exon 2), rs768985544 (1201A/G; exon 3), and rs12072 (2922T/C; exon 6) were detected in the Reg1a gene. Their distribution among the 308 patients is shown in Table 1. The test showed that the Reg1a allele and genotype frequencies in each paired group conformed to the Hardy–Weinberg equilibrium; all were P > 0.05 (see Supplementary Tables 1–5). Linkage disequilibrium (LD) was not observed.
Association Between Reg1a Polymorphisms and Clinical Characteristics
Reg1a variant genotypes were detected in the patients. rs10165462 20C/T existed in 54 (CC), 88 (CT), and 45 (TT) cases and rs12072 2922T/C existed in 20 (TT), 77 (TC), and 90 (CC) cases in local early-stage patients (T1–T2); rs10165462 20C/T existed in 18 (CC), 67 (CT), and 36 (TT) cases, while rs12072 2922T/C existed in 18 (TT), 67 (TC), and 36 (CC) cases corresponding in local advanced-stage patients (T3–T4). There was a significant difference between local early-stage patients and advanced-stage patients at both loci (P = 0.018 and P = 0.0059, respectively). These results show that rs10165462 20C/T and rs12072 2922T/C variant genotypes are associated with local invasion in NPC.
Stratified analysis found that occurrence of the rs10165462 20CC genotype was significantly different compared with CT and TT (P < 0.01 respectively), and that patients with the 20CC genotype had a later T stage than those with CT and TT (OR = 3.652, 95% CI: 1.623–8.217, P = 0.002) and (OR = 4.051, 95% CI: 1.775–9.244, P = 0.001) after adjusting for age and gender. Conversely, carriers with the rs12072 2922CC genotype tended to have earlier T stages than TC and TT (P < 0.05 respectively), (OR = 2.020, 95% CI: 1.106–3.692, P = 0.022) and (OR = 1.891, 95% CI: 1.018–3.514, P = 0.044) after adjusting for age and gender. These results indicate that the rs10165462 20CC genotype and the rs12072 2922CC genotype are contributors to and independent predictors of local invasion in NPC.
No association was found between the rs10165462 20C/T and rs12072 2922T/C variant genotypes and other clinical characteristics (all P > 0.05). Moreover, no statistically significant association was observed when comparing other Reg1a SNPs, including rs117580393 369G/T and rs768985544 1201A/G, with different clinical characteristics (all P > 0.05) (see Supplementary Tables 1–5).
Association of Reg1a Polymorphisms with Radiation Sensitivity
In this study, 281 cases were assessed as radiation sensitive, and 27 cases (including 17 PR cases, 6 SD cases, and 4 PD cases) were assessed as resistant three months after complete treatment. The total sensitivity rate was 91.23% (281/308) and the resistance rate was 8.77% (27/308) (see Table 1).
Variant genotypes of rs10165462 20C/T existed as follows: in radiation-sensitive patients there were 63 CC cases (22.42%), 150 CT cases (53.38%), and 68 TT cases (24.20%); in radiation-resistant patients there were 9 CC cases (33.33%), 5 CT cases (18.52%), and 13 TT cases (48.15%). Analysis of these results showed that Reg1a rs10165462 20C/T polymorphisms were significantly associated with radiation response (X2 = 13.410, P = 0.0019). Stratified analysis results showed that occurrence of the rs10165462 20CT genotype was significantly different when compared with occurrence of the CC, TT, and CC + TT genotypes (all P < 0.01). Patients with the Reg1a rs10165462 20C/T CT genotype experienced significantly more frequent radiation response (OR = 0.275, 95% CI: 0.102–0.739, P = 0.01). Multivariate logistic regression analysis showed that the Reg1a rs10165462 20C/T genotype was also significantly associated with radiation response (OR = 0.265,95% CI: 0. 096–0.727, P = 0.01) after adjusting for other clinical-pathological factors, such as age, gender, T stage, N stage, pathology, and other Reg1a polymorphisms.
No statistically significant association was observed when comparing the other Reg1a variant genotypes with radiation response (all P > 0.05). Therefore, the Reg1a rs10165462 20C/T genotype was the only predictor for radiation response in NPC (see Supplementary Tables 6 and 7).
Association of Reg1a Polymorphisms with OS and PFS
The five-year OS and PFS rates of the patients was 49.5% and 47.1%, respectively (see Supplementary Figure 1). The five-year OS rate of patients with the rs10165462 20C/T variant genotype was 41.8% for the CC genotype, 53.6% for the CT genotype and 60.9% for the TT genotype (log-rank = 8.110, P = 0.017). Patients with the 20TT genotype had a better five-year OS rate than those with the 20CC genotype (P = 0.01). Individuals with variant alleles (CC + CT) (45.2%) had significantly poorer OS compared with wild-type (TT) carriers (60.9%) (log-rank = 4.340, P = 0.037).
The five-year PFS rate was 39.4% for CC, 48.4% for CT, and 60.8% for TT (log-rank = 8.510, P = 0.014); patients with the 20TT genotype had a better five-year PFS than those with the CC genotype (P = 0.004). Carriers with variant alleles (CC + CT (41.8%) had significantly poorer PFS compared with wild-type (TT) carriers (60.8%) (log-rank = 5.963, P = 0.015). These results indicate that patients with NPC who carried the TT genotype had better five-year OS and PFS rates than those who carried the CC or CT genotypes (see Figure 1).
Similarly, the five-year OS rates of patients with the rs12072 2922C/T variant genotype were 67.1% for the CC genotype; 43.3% for the CT genotype, and 48.3% for the TT genotype (log-rank = 5.846, P = 0.054); however, patients with the CC genotype had a better OS rate than those with the CT genotype (P = 0.017). Patients with variant alleles (TT + TC) (44.8%) had significantly adverse OS rates compared with wild-type (CC) carriers (log-rank = 5.115, P = 0.024).
The five-year PFS rates of patients with the rs12072 2922C/T variant genotype were 62.5% for the CC genotype, 41.8% for the CT genotype, and 45.9% for the TT genotype. No significant difference was found when comparing the genotypes in the rs12072 2922C/T variant genotype (log-rank = 5.431, P = 0.066). Interestingly, patients with the CC genotype had a higher PFS rate than those with the CT genotype (P = 0.022). In addition, a significant difference was observed between those with the CC genotype and those with the TT + TC genotype (62.5% vs 42.9%) (log-rank = 4.919, P = 0.027). Patients with variant alleles (TT + TC) had a negative prognosis outcome compared with those with wild-type (CC) carriers (see Supplementary Figure 2). No statistically significant association with OS and PFS was observed in other Reg1a SNPs, including rs117580393 369G/T and rs768985544 1201A/G (all P > 0.05). This indicates that patients carrying the 20C/T and 2922T/C wild-type genotypes tend to have longer OS and PFS compared with those carrying other variant genotypes (P < 0.05).
Multivariate analysis showed that T stage (T1–2 vs T3–4) and rs10165462 20CT genotype were independent prognostic factors for OS (HR = 0.384, 95% CI 0.256–0.575, P = 0.0001 and HR = 1.642, 95% CI 1.038–2.598, P = 0.034, respectively) and for PFS (HR = 0.401, 95% CI 0.269–0.599, P = 0.0001 and HR = 1.705, 95% CI 1.080–2.692, P = 0.022, respectively) when clinic-pathological characteristics, including age, gender, T stage, N stage, pathology, radiation sensitivity, rs10165462 20C/T, rs117580393 369G/T, rs768985544 1201A/G, and rs12072 2922T/C variant genotypes were entered into the Cox proportional hazards model. This suggests an association between Reg1a rs10165462 20C/T and OS and PFS and indicates that patients carrying the rs10165462 20CT genotype had significantly longer OS and PFS compared with those carrying the 20CC and 20TT genotypes (see Table 3).
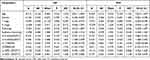 |
Table 3 Multivariate Cox Regression Analyses of OS and PFS |
Discussion
Accumulating evidence indicates that genetic variations are strongly associated with cell proliferation, disease progression, treatment response, and survival in various types of solid tumors.10,36 Previous studies have also observed an association between Reg1a polymorphisms and human cancers. Current research, however, is limited to the possible role of regulatory variants and some coding regions in the Reg1a gene in the development and progression of several types of pancreatic disease.37 Our previous study showed that the Reg1a rs10702 2922C/T variant genotype increased the risk of developing NPC in a Cantonese population.31 The results of the present study indicate that Reg1a gene polymorphisms are not only involved in local invasion but also in treatment response and survival of patients with NPC.
Liu et al reported that patients with NPC who carried the TC genotype and T-allele had a later T stage (T3–T4) than those who did not.38 Hao et al suggested that IFN-γ 13-CA-repeat polymorphism impacted the metastasis of NPC and contributed to an increased risk of lymph node metastasis and distant metastasis.39 Guo et al observed that two loci in the AKT1 gene (rs3803300 and rs2494738 alone or combined) were associated with reduced risk of distant failure, especially in N2–3 patients carrying at least one variant allele.40 Another study that explored the contribution of NOS3 variants to NPC progression revealed that NOS3 T-786C can reduce the development of regional lymph node metastasis.41 The results of the present study found that carriers of the Reg1a rs10165462 20CC genotype had a later T stage (T1–2 vs T3–4), while those with the Reg1a rs10702 2992CC genotype had an earlier T stage than those with other genotypes (rs10165462 20 CT + TT and rs10702 2992 CT + TT, alone or combined).
Two loci, rs10165462 and rs10702, are related to local invasion in NPC. Our previous research indicated that the overexpression of the Reg1a protein could accelerate this local invasion and stimulate T-stage progression from early to advanced,30,31 suggesting that the rs10165462 20CC and rs12072 2992CC genotypes may play a role in the local invasion of NPC. Further investigation is still needed to unravel the functional significance of these polymorphisms.
Gene polymorphism is strongly related to individual variations in radiation sensitivity in various tumors.42 Alsbeih et al reported that MDR1 G2677T and C3435T polymorphisms can be used to assess the response to radiotherapy of patients with NPC.8 The wide genotype GG of XRCC1 rs25489 and the wide genotype CC of 8-oxoguanine DNA glycosylase (OGG1) rs1052133 were positively and negatively associated, respectively, with the efficacy of radiotherapy on primary tumors.43 Meanwhile, ERCC1 Cys8092Ala, HDM2 promoter T/G rs2279744 and T/A rs1196333, XRCC1 Codon399 Gln/Gln allele, and cyclin-dependent kinase inhibitor gene CDKN2A rs3088440 polymorphism have all been identified as independent predictors of response to radiotherapy on the primary tumor and cervical lymph node in NPC.44,45
Alsbeih et al used polygenic polymorphism to predict radiation sensitivity and identified six SNPs that were more accurate than a single SNP as biomarkers to assess the efficiency of radiotherapy.8 The same result was observed in the catenin beta 1 genes (CTNNB1) rs1880481 and rs3864004 and glycogen synthase kinase 3-beta gene (GSK3β) rs3755557 polymorphisms, which were significantly associated with poorer efficacy of radiotherapy in patients with NPC.46 A later study suggested that a sequence polymorphism in miR-608 could predict the local recurrence rate in patients with NPC undergoing radiotherapy.47 Our data showed that the total radiation response rate in patients with NPC was 91.23%, and that, associated with REG1a rs10165462 20C/T heterozygous genotype alone, carriers of the REG1A rs10165462 20CT genotype had a higher response rate than carriers of the 20CC or 20TT genotype or a combination of the two (CT vs CC + TT, all P < 0.01). This result is consistent with previous findings and indicates that the rs10165462 20CT genotype in Reg1a might stimulate a potential signaling pathway to modulate the radiotherapy response of patients with NPC.
Tumor load influences the efficacy of radiotherapy, regardless of local lesion or metastasis. Here, we identified the role of the rs10165462 20CC genotype in facilitating local progression and reducing radiotherapy efficacy in NPC patients. The rs10165462 genetic variations were significantly correlated with radiation response. Moreover, multivariate analysis showed that the rs10165462 20CT genotype was the only influencing factor for radiation sensitivity after adjustments for other clinic-pathological factors. Therefore, rs10165462 20CT may be a potential regulator for moderating radiotherapy efficacy and could be used as a biomarker for radiation sensitivity. The rs10165462 20CT genotype, rather than other genotypes and SNPs in the Reg1a gene, plays a key role in the NPC progression and the efficacy of radiotherapy. Therefore, the C allele of rs10165462 20C/T is implicated as a potential marker for personalized medicine, and a patient that carries it may require more aggressive radiotherapy.
A high risk of disease progression and poor radiation sensitivity both contribute to the negative prognosis and survival of patients with NPC. There is growing evidence that gene polymorphisms that help identify patients with different risks for prognosis are strongly associated with treatment outcome.48 CXCL12 rs1801157 polymorphism has been significantly associated with distant metastasis-free survival and PFS.3 In the current study, the five-year OS and PFS rates were 49.5% and 47.1%, respectively. The rs10165462 20C/T and rs10702 2992C/C variant genotypes had different OS and PFS rates, and these differences were significant. The C allele in rs10165462 20C/T and the T allele in rs10702 2992C/C can influence the OS and PFS rates of patients with NPC. These results are in accordance with the observations of previous studies and indicate that Reg1a SNPs are associated with the efficacy of radiotherapy and survival in patients with NPC, although the mechanism itself remains unclear.
In the multivariate analysis, it was observed that rs10165462 20 CT and T stage were associated with OS and PFS rates, and, therefore, could be used as independent predictors of survival. This provides extremely strong evidence that Reg1a plays a crucial role in NPC prognosis, with the double effect of Reg1a gene polymorphisms enhancing local invasion and regulating radiation sensitivity; this finding provides new insight into the genetic basis of tumor cellular response to radiation. Reg1a gene polymorphisms may be used as pre-treatment biomarkers for identifying highly radiosensitive patients with NPC, leading to the customization of treatment protocols and improved treatment outcomes.
Our data suggest that Reg1a gene variation is closely related to radioresponsiveness and survival of nasopharyngeal carcinoma. The potential molecular biological mechanism may be that the change of bases at polymorphic sites of REG1A gene leads in turn to the variation of the gene sequence and function, and the latter responds to radiation differently through different functional pathways in cells, manifested as proliferation or apoptosis of tumor cells, thus affecting the survival and prognosis of NPC patients. Further study with larger samples and exploration of the molecular mechanism are both needed for more accurate assessment.
The current study has some limitations. Firstly, the patient sample was small, and the candidate genetic predictors require more definitive validation in an independent cohort. Larger population-based studies in different ethnic groups are necessary to further validate the role and mechanism of Reg1a SNPs. Secondly, a single gene was identified rather than a set of genes or pathways of Reg1a involved in NPC, and, as we know, radiation sensitivity may be the result of the combined effects of genes involved in different cellular pathways. Lastly, the mechanism by which Reg1a SNPs influence the efficacy of radiotherapy and survival in patients with NPC could not be fully understood, although doing so was beyond the scope of this study. In addition, the application of CT, inferior to Magnetic resonance imaging (MRI) in soft tissue resolution, may affect the accuracy of the assessment of radiation response in this study.
Conclusion
In conclusion, our study verified that Reg1a SNPs have a reliable association with local progression, radiation response, and treatment outcome in NPC in a southern Chinese population. Reg1a rs10165462 is a significant risk factor for local invasion and serves as a potential predictor of radiation response and prognosis in patients with NPC who are being treated with radiotherapy.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
This study was funded by: Shenzhen Science and Technology Innovation Fund Project (No. JCYJ20160428174605066 and JCYJ20170302153015013) and Nature Science Foundation from the Sci-Tech Department of Hainan Province (No.310162). Shenzhen Guangming District Science and Technology Innovation Bureau fund project (No.2020R01057 and 2021R01018).
Disclosure
The authors declare that they have no competing interests.
References
1. Kamran SC, Riaz N, Lee N. Nasopharyngeal carcinoma. Surg Oncol Clin N Am. 2015;24(3):547–561. doi:10.1016/j.soc.2015.03.008
2. Zhang Y, Chen M, Chen C, Kong L, Lu JJ, Xu B. The efficacy and toxicities of intensive induction chemotherapy followed by concurrent chemoradiotherapy in nasopharyngeal carcinoma patients with N3 disease. Sci Rep. 2017;7(7):3668. doi:10.1038/s41598-017-03963-8
3. Forman D, Bray F, Brewster DH, et al. Cancer Incidence in Five Continents, Vol. X. IARC Scientific Publication No. 164. Lyon: International Agency for Research on Cancer; 2014.
4. Chen R, Xu Y, Du X, et al. CXCL12 genetic variants as prognostic markers in nasopharyngeal carcinoma. Onco Targets Ther. 2015;8:2835–2842. doi:10.2147/OTT.S90430
5. Chen L, Mao YP, Xie FY, et al. The seventh edition of the UICC/AJCC staging system for nasopharyngeal carcinoma is prognostically useful for patients treated with intensity-modulated radiotherapy from an endemic area in China. Radiother Oncol. 2012;104(3):331–337. doi:10.1016/j.radonc.2011.10.009
6. Hornhardt S, Rossler U, Sauter W, et al. Genetic factors in individual radiation sensitivity. DNA Repair. 2014;16:54–65. doi:10.1016/j.dnarep.2014.02.001
7. Mertens AC, Mitby PA, Radloff G, et al. XRCC1 and glutathione-S-transferase gene polymorphisms and susceptibility to radiotherapy-related malignancies in survivors of Hodgkin disease. Cancer. 2004;101(6):1463–1472. doi:10.1002/cncr.20520
8. Alsbeih G, El-Sebaie M, Al-Rajhi N, et al. Among 45 variants in 11 genes, HDM2 promoter polymorphisms emerge as new candidate biomarker associated with radiation toxicity. 3 Biotech. 2014;4(2):137–148. doi:10.1007/s13205-013-0135-3
9. Ishikawa H, Mitsuhashi N, Sakurai H, Maebayashi K, Niibe H. The effects of p53 status and human papillomavirus infection on the clinical outcome of patients with stage IIIB cervical carcinoma treated with radiation therapy alone. Cancer. 2001;91(1):80–89. doi:10.1002/1097-0142(20010101)91:1<80::aid-cncr11>3.0.co;2-e
10. Kelsey CR, Jackson IL, Langdon S, et al. Analysis of single nucleotide polymorphisms and radiation sensitivity of the lung assessed with an objective radiologic endpoin. Clin Lung Cancer. 2013;14(3):267–274. doi:10.1016/j.cllc.2012.10.006
11. Wu X, Gu J, Wu TT, et al. Genetic variations in radiation and chemotherapy drug action pathways predict clinical outcomes in esophageal cancer. J Clin Oncol. 2006;24(23):3789–3798. doi:10.1200/JCO.2005.03.6640
12. Grimminger PP, Brabender J, Warnecke-Eberz U, et al. XRCC1 gene polymorphism for prediction of response and prognosis in the multimodality therapy of patients with locally advanced rectal cancer. J Surg Res. 2010;164(1):e61–e66. doi:10.1016/j.jss.2010.08.002
13. Yu X, Xiao H, Zhao B, Zhang X, Wang G. DNA repair gene ERCC1 C118T polymorphism predicts sensitivity of recurrent esophageal cancer to radiochemotherapy in a Chinese population. Thorac Cancer. 2015;6(6):741–748. doi:10.1111/1759-7714.12251
14. Li F, Xie X, Ren X, Zhang J. A meta-analysis identifies ERCC1 gene polymorphism as a predictor of better patient response to treatment with radiochemotherapy. Cancer Chemother Pharmacol. 2016;77(6):1183–1191. doi:10.1007/s00280-016-3015-9
15. Bollschweiler E, Hölscher AH, Herbold T, et al. Molecular markers for the prediction of minor response to neoadjuvant chemoradiation in esophageal cancer: results of the prospective Cologne Esophageal Response Prediction (CERP) Study. Ann Surg. 2016;264(5):839–846. doi:10.1097/SLA.0000000000001911
16. Metzger R, Warnecke-Eberz U, Alakus H, et al. Neoadjuvant radiochemotherapy in adenocarcinoma of the esophagus: ERCC1 gene polymorphisms for prediction of response and prognosis. J Gastrointest Surg. 2012;16(1):26–34. doi:10.1007/s11605-011-1700-x
17. Hui EP, Ma BB, Chan KC, et al. Clinical utility of plasma Epstein-Barr virus DNA and ERCC1 single nucleotide polymorphism in nasopharyngeal carcinoma. Cancer. 2015;121(16):2720–2729. doi:10.1002/cncr.29413
18. Kelsey CR, Jackson L, Langdon S, et al. A polymorphism within the promoter of the TGFβ1 gene is associated with radiation sensitivity using an objective radiologic endpoint. Int J Radiat Oncol Biol Phys. 2012;82(2):e247–e255. doi:10.1016/j.ijrobp.2011.02.064
19. Kim JC, Ha YJ, Roh SA, et al. Novel single-nucleotide polymorphism markers predictive of pathologic response to preoperative chemoradiation therapy in rectal cancer patients. Int J Radiat Oncol Biol Phys. 2013;86(2):350–357. doi:10.1016/j.ijrobp.2012.12.018
20. Angèle S, Romestaing P, Moullan N, et al. ATM haplotypes and cellular response to DNA damage: association with breast cancer risk and clinical radiosensitivity. Cancer Res. 2003;63(24):8717–8725.
21. Yang J, Wang X, Zou SM, et al. [Genetic variations in MLH3 and MSH2 genes are associated with the sensitivity and prognosis in locally advanced rectal cancer patients receiving preoperative chemoradiotherapy]. Zhonghua Zhong Liu Za Zhi. 2018;40(6):433–440. Chinese. doi:10.3760/cma.j.issn.0253-3766.2018.06.007
22. Qiao Y, Hu CX, Song DA, Li SQ, Zhou LH, Jiang XD. [High throughput-targeted sequencing panel for exploring radiosensitivity associated genes in esophageal squamous cell carcinoma]. Zhonghua Zhong Liu Za Zhi. 2017;39(8):584–588. Chinese. doi:10.3760/cma.j.issn.0253-3766.2017.08.005
23. Wang C, Nie H, Li Y, et al. The study of the relation of DNA repair pathway genes SNPs and the sensitivity to radiotherapy and chemotherapy of NSCLC. Sci Rep. 2016;6:26526. doi:10.1038/srep26526
24. Bulibu J, Wang W, Tang Y, Li N, Saifuding K. Association between polymorphisms in the promoter region of microRNA-34b/c and the chemoradiotherapy efficacy for locally advanced esophageal squamous cell carcinoma in Chinese Han Population. Pathol Oncol Res. 2019;25(1):421–427. doi:10.1007/s12253-017-0366-4
25. Baijer J, Déchamps N, Perdry H, et al. TNFSF10/TRAIL regulates human T4 effector memory lymphocyte radiosensitivity and predicts radiation-induced acute and subacute dermatitis. Oncotarget. 2016;7(16):21416–21427. doi:10.18632/oncotarget.7893
26. Fujimura T, Fujimoto T, Itaya-Hironaka A, et al. Significance of interleukin-6/STAT pathway for the gene expression of REG Iα, a new autoantigen in sjögren’s syndrome patients, in salivary duct epithelial cells. Clin Rev Allergy Immunol. 2017;52(3):351–363. doi:10.1007/s12016-016-8570-7
27. Kiyayama Y, Fukui H, Hara K, et al. Role of regenerating gene I in claudin expression and barrier function in the small intestine. Transl Res. 2016;173:92–100. doi:10.1016/j.trsl.2016.03.007
28. Planas R, Pujol-Autonell I, Ruiz E, et al. Regenerating gene Iα is a biomarker for diagnosis and monitoring of celiac disease: a preliminary study. Transl Res. 2011;158(3):140–145. doi:10.1016/j.trsl.2011.04.004
29. Hayashi K, Motoyama S, Koyota S, et al. REG I enhances chemo- and radiosensitivity in squamous cell esophageal cancer cells. Cancer Sci. 2008;99(12):2491–2495. doi:10.1111/j.1349-7006.2008.00980.x
30. Xing H, Chen X, Han Y. Role of regenerating gene IA expression on local invasion and survival in nasopharyngeal carcinoma. Biol Res. 2017;50(1):37. doi:10.1186/s40659-017-0142-7
31. Xing H, Chen X, Sun H, Han Y, Ding L, Chen X. Association of regenerating gene 1A single-nucleotide polymorphisms and nasopharyngeal carcinoma susceptibility in southern Chinese population. Eur Arch Otorhinolaryngol. 2020;277(1):221–226. doi:10.1007/s00405-019-05645-9
32. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131(6):803–820. doi:10.1007/s00401-016-1545-1
33. Edge SB, Compton CC. The American joint committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. doi:10.1245/s10434-010-0985-4
34. Purcell S, Neale B, Todd-Brown K, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81(3):559–575. doi:10.1086/519795
35. Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21(2):263–265. doi:10.1093/bioinformatics/bth457
36. Ho-Pun-Cheung A, Assenat E, Bascoul-Mollevi C, et al. A large-scale candidate gene approach identifies SNPs in SOD2 and IL13 as predictive markers of response to preoperative chemoradiation in rectal cancer. Pharmacogenomics J. 2011;11(6):437–443. doi:10.1038/tpj.2010.62
37. Mahurkar S, Bhaskar S, Reddy DN, Rao GV, Chandak GR. Comprehensive screening for reg1alpha gene rules out association with tropical calcific pancreatitis. World J Gastroenterol. 2007;13(44):5938–5943. doi:10.3748/wjg.v13.i44.5938
38. Liu Y, Cai H, Liu J, et al. A miR-151 binding site polymorphism in the 3ʹ-untranslated region of the cyclin E1 gene associated with nasopharyngeal carcinoma. Biochem Biophys Res Commun. 2013;432(4):660–665. doi:10.1016/j.bbrc.2013.02.024
39. Hao K, Yan Z, Shuang Y, et al. Association between interferon gamma 13-CA-repeats polymorphism and metastasis of nasopharyngeal carcinoma in a population of Northern China. Int J Clin Exp Pathol. 2015;8(6):7409–7414.
40. Guo Q, Lu T, Chen Y, et al. Genetic variations in the PI3K-PTEN-AKT-mTOR pathway are associated with distant metastasis in nasopharyngeal carcinoma patients treated with intensity-modulated radiation therapy. Sci Rep. 2016;6:37576. doi:10.1038/srep37576
41. Aouf S, Laribi A, Gabbouj S, et al. Contribution of nitric oxide synthase 3 genetic variants to nasopharyngeal carcinoma risk and progression in a Tunisian population. Eur Arch Otorhinolaryngol. 2019;276(4):1231–1239. doi:10.1007/s00405-019-05333-8
42. Guo C, Huang Y, Yu J, et al. The impacts of single nucleotide polymorphisms in genes of cell cycle and NF-kB pathways on the efficacy and acute toxicities of radiotherapy in patients with nasopharyngeal carcinoma. Oncotarget. 2017;8(15):25334–25344. doi:10.18632/oncotarget.15835
43. Wang J, Guo C, Gong X, et al. The impacts of genetic polymorphisms in genes of base excision repair pathway on the efficacy and acute toxicities of (chemo)radiotherapy in patients with nasopharyngeal carcinoma. Oncotarget. 2017;8(45):78633–78641. doi:10.18632/oncotarget.20203
44. Jin H, Xie X, Wang H, et al. ERCC1 Cys8092Ala and XRCC1 Arg399Gln polymorphisms predict progression-free survival after curative radiotherapy for nasopharyngeal carcinoma. PLoS One. 2014;9(7):e101256. doi:10.1371/journal.pone.0101256
45. Zhai XM, Hu QC, Gu K, Wang JP, Zhang JN, Wu YW. Significance of XRCC1 Codon399 polymorphisms in Chinese patients with locally advanced nasopharyngeal carcinoma treated with radiation therapy. Asia Pac J Clin Oncol. 2016;12(1):e125–e132. doi:10.1111/ajco.12117
46. Yu J, Huang Y, Liu L, et al. Genetic polymorphisms of Wnt/β-catenin pathway genes are associated with the efficacy and toxicities of radiotherapy in patients with nasopharyngeal carcinoma. Oncotarget. 2016;7(50):82528–82537. doi:10.18632/oncotarget.12754
47. Zheng J, Deng J, Xiao M, et al. A sequence polymorphism in miR-608 predicts recurrence after radiotherapy for nasopharyngeal carcinoma. Cancer Res. 2013;73(16):5151–5162. doi:10.1158/0008-5472.CAN-13-0395
48. Liu H, Qi B, Guo X, et al. Genetic variations in radiation and chemotherapy drug action pathways and survival in locoregionally advanced nasopharyngeal carcinoma treated with chemoradiotherapy. PLoS One. 2013;8(12):e82750. doi:10.1371/journal.pone.0082750
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

