Back to Journals » Risk Management and Healthcare Policy » Volume 15
The Relationship Between the Neutrophil to Lymphocyte Ratio, The Platelet to Lymphocyte Ratio, and Cardiac Syndrome X
Authors Cao GY, Li JC, Wang WJ, Wu HB
Received 19 October 2021
Accepted for publication 10 December 2021
Published 9 March 2022 Volume 2022:15 Pages 427—433
DOI https://doi.org/10.2147/RMHP.S359733
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kent Rondeau
Guang-Yun Cao,1 Jian-Chao Li,1,2 Wen-Jing Wang,1 Hai-Bo Wu1
1Department of Cardiology, Hebei General Hospital, Shijiazhuang, Hebei Province, 050051, People’s Republic of China; 2HeBei North University, Zhangjiakou, Hebei Province, 050051, People’s Republic of China
Correspondence: Hai-Bo Wu, Department of Cardiology, Hebei General Hospital, 348 Heping West Road, Shijiazhuang, Hebei Province, 050051, People’s Republic of China, Tel +86 15128138630, Email [email protected]
Objective: This study aims to investigate the relationship between the neutrophil to lymphocyte ratio (NLR), the platelet to lymphocyte ratio (PLR), and cardiac syndrome X (CSX).
Methods: A total of 102 patients with CSX who were hospitalized in the Cardiology Department of our hospital from December 2018 to December 2020 were enrolled in the CSX group, and 102 subjects who underwent physical examinations during the same period were included in the control group. An automatic blood cell analyzer was adopted to detect the neutrophil count (NC), lymphocyte count (LC), and number of platelets (PLT) in the whole blood of the subjects in both groups, and the NLR and PLR were calculated. Electrocardiography was conducted on the subjects in both groups to detect whether any abnormality existed in the ST segment. The receiver operating curve (ROC) was used to evaluate the diagnostic value of each indicator of CSX, and multivariate logistic regression analysis was adopted for the analysis of the influencing factors.
Results: No significant differences existed in age, gender, smoking history, or family history of diabetes mellitus, hypertension, and tumors between the two groups (p > 0.05). When compared with the control group, the NC, PLT, NLR, PLR, and rate of abnormality of the ST segment on the electrocardiogram were significantly higher, and the LC was significantly lower in the CSX group (p < 0.05). Multivariate logistic regression analysis showed that the ST-segment abnormality (3.95 [2.10∼ 7.41]; NLR > 2.21, 3.46 [1.87∼ 6.39]; and PLR > 119.77, 3.66 [1.99∼ 6.73]) was a correlated risk factor for the occurrence of CSX (p < 0.05).
Conclusion: Both the NLR and PLR in patients with CSX were significantly elevated, and both have a certain predictive value for the occurrence of CSX and are expected to be effective biomarkers for CSX.
Keywords: cardiac syndrome X, neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, correlation analysis, inflammation
Introduction
Cardiac Syndrome X (CSX), also known as microvascular angina pectoris, is characterized by no typical exercise-induced angina, ST-segment changes during an exercise stress test, objective ischemia recorded on myocardial perfusion imaging, or epicardial coronary artery stenosis or vasospasm.1 Currently, various pathophysiological mechanisms have been proposed for CSX, including endothelial dysfunction, altered autonomic status, and vascular inflammation, but the exact mechanism remains unclear.2 Previously, CSX was considered a benign condition, but recent studies have shown that it is correlated with persistent chest pain, decreased quality of life, angiographic recurrence, and increased cardiovascular morbidity and mortality.3 Although long-term survival is generally high in patients with CSX, mortality may increase in those with an ischemic response during exercise.4
Inflammation plays a key role in the development and progression of cardiovascular disease. The neutrophil to lymphocyte ratio (NLR) has been introduced as a marker of inflammation in various pathological conditions, including diabetes, thyroiditis, ulcerative colitis, functional bowel diseases, Covid-19 infection, thyroid conditions, and cancers,5–11 and it has recently emerged as a potential marker in the identification of inflammation in cardiac and non-cardiac disease.12 Platelets are also thought to play an important role in the pathogenesis of atherosclerosis.13 The platelet to lymphocyte ratio (PLR) is also associated with many disorders, such as diabetes, malignant thyroid nodules, irritable bowel syndrome, Covid-19 infection, and thyroid conditions.10,14–16 It is also correlated with morbidity in patients with acute myocardial infarction.17 The NLR and PLR can be cost-effective predictors of inflammation and cardiovascular complications.18 However, the changes in and clinical value of the NLR and PLR in CSX have not been reported.
In the present study, the NLR and PLR, which are correlated indicators for reflecting the degree of inflammation in an organism, were selected as observation indicators to explore their changes in and diagnostic value for CSX to provide a reference for the clinical prevention and treatment of CSX.
Materials and Methods
Study Subjects
A total of 102 patients with CSX including 58 males and 44 females aged 35–83 y (61.25 ± 12.17 y) who were hospitalized in our Cardiology Department from December 2018 to December 2020 were selected as the study subjects (CSX group). The coronary angiography of the CSX group showed no vascular stenosis. Another 102 subjects with no previous history of allergy including 61 males and 41 females aged 34–82 y (61.03 ± 11.92 y) who underwent healthy physical examinations were enrolled in the control group. There were no significant differences in age and gender between the two groups (p > 0.05), and the data were comparable. Informed consent was obtained from the patients and their families, and the study was approved by the Medical Ethics Committee of the Hebei Provincial People’s Hospital.
Inclusion and Exclusion Criteria
(1) Inclusion criteria for patients with CSX: (a) met the diagnostic criteria for CSX,19 which are typical symptoms of exertional angina pectoris with positive exercise plate test results and no cavity stenosis or irregular wall lesions on the coronary angiography together with the exclusion of a coronary spasm and (b) complete clinical data.
(2) Exclusion criteria: (a) other types of heart disease, such as angina pectoris; (b) severe cardiac, cerebral, pulmonary, renal, or other vital organ dysfunction; (c) malignant tumors; (d) other disorders that may affect NLR or PLR, such as diabetes, thyroiditis, ulcerative colitis, functional bowel diseases, Covid-19 infection, and thyroid conditions; and (e) lost during follow-up.
Electrocardiography Detection
Electrocardiography was performed when the patient complained of precordial discomfort. An electrocardiograph (Shenzhen Ribbon Precision Instruments Co., Ltd.) was used to detect abnormal changes in the ST segment of the study subjects before admission, including elevation, depression, extension, and shortening.
Liver and Kidney Function Index, Neutrophil and Lymphocyte Count, and Platelet Assay
Early on the day of hospitalization, 6 mL of fasting peripheral venous blood (3 mL in a non-anticoagulant tube and 3 mL in an ethylenediaminetetraacetic acid anticoagulant tube) was taken from the subjects. Serum creatinine, alanine aminotransferase, aspartate aminotransferase, triglyceride, whole blood neutrophil count (NC), lymphocyte count (LC) and platelet count (PLT) numbers in CSX group and control group were measured by an AU automatic biochemical analyzer (Bio-Rad Laboratories, Hercules, CA) and automatic blood cell analyzer (Bio-Rad Laboratories) The following equations were adopted to calculate the NLR and PLR: NLR = NC ÷ LC and PLR = PLT ÷ LC.
Statistical Analysis
The SPSS 23.0 software was adopted for the input and analysis of all data. The Shapiro–Wilk test was used to determine the normality of the data. The normally distributed continuous data were described as mean ± standard deviation ( ) and tested using the t-test. The non- normally distributed continuous data were expressed as median and interquartile range (M [Q1, Q3]) and compared using the Mann–Whitney U-test. The countable data were expressed as a number (%) and tested using the chi-squared test. The receiver operating curve (ROC) was used to assess the diagnostic value of each indicator of CSX, and logistic regression analysis was adopted for risk factor analysis. P < 0.05 was considered to be statistically significant.
) and tested using the t-test. The non- normally distributed continuous data were expressed as median and interquartile range (M [Q1, Q3]) and compared using the Mann–Whitney U-test. The countable data were expressed as a number (%) and tested using the chi-squared test. The receiver operating curve (ROC) was used to assess the diagnostic value of each indicator of CSX, and logistic regression analysis was adopted for risk factor analysis. P < 0.05 was considered to be statistically significant.
Results
Comparison of the General Characteristics
A total of 204 study subjects were included in the present study, 102 in the CSX group and 102 in the control group. No significant differences existed between the CSX and the control groups in terms of age; gender; smoking history; or family history of diabetes mellitus, hypertension, and tumor (p > 0.05; see Table 1).
 |
Table 1 Comparison of General Data Between the Two Groups[n (%)] |
Comparison of the Electrocardiogram Results Between the Two Groups
When compared with the electrocardiogram (ECG) results of the control group, the rate of ST-segment abnormality in the ECG results of the CSX group was significantly higher (p < 0.05; see Table 2).
 |
Table 2 Comparison of ECG Results Between the Two Groups[n (%)] |
The Comparison of the NC, LC, PLT, NLR, and PLR in the Peripheral Blood Between the Two Groups
When compared with the control group, the NC, PLT, NLR, and PLR were significantly higher and the LC was significantly lower in the CSX group (p < 0.05; see Table 3).
 |
Table 3 Comparison of NC, LC, PLT, NLR and PLR in Peripheral Blood Between the Two Groups ( |
Analysis of Diagnostic Value
The results of the ROC analysis showed that the area under the curve for the NLR and PLR was 0.727 and 0.887, respectively. The sensitivity of the NLR and PLR for the diagnosis of CSX was 75.1% and 88.7%, and the specificity was 72.5% and 85.2%, respectively (see Figure 1).
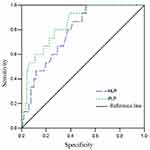 |
Figure 1 The receiver operating curve for the diagnosis of cardiac syndrome X by each indicator. |
Multivariate Logistic Regression Analysis of the Influencing Factors of CSX
Multivariate logistic regression analysis was conducted using the occurrence of CSX as the dependent variable (no = 0 and yes = 1) and the variables that were significant in the univariate analysis as the independent variables. The results showed that ST-segment abnormalities, NLR > 2.21, and PLR > 119.77 were risk factors correlated with the occurrence of CSX (p < 0.05; see Table 4).
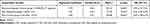 |
Table 4 Multivariate Logistic Regression Analysis of CSX Influencing Factors |
Discussion
The present study included a total of 204 study subjects (102 patients with CSX and 102 healthy subjects). The existing research data have shown that coronary heart disease, hypertension, and other diseases are closely correlated with the onset of CSX and are risk factors for CSX. In this study, in order to ensure the reliability and comparability of the results, we performed initial tests on the two groups of subjects to identify differences in general demographic characteristics. No statistically significant differences were found in age, gender, smoking habits, the presence of diabetes or high blood pressure, family history of tumor, or liver and kidney function indexes.
The ECG is a routine examination that is performed when patients are admitted to hospital, and abnormal ECG results coupled with abnormalities in the related indicators in the body can reflect the cardiac health status of the patient. The 12-lead ECG is the most common cardiac test, and the results are of great importance for patients with cardiac symptoms, including chest pain, dyspnea, palpitations, and syncope.20 In the present study, all the study subjects were examined using an electrocardiograph, and it was found that the rate of ST-segment abnormalities was significantly higher in the CSX group than in the control group, indicating that the occurrence of CSX may lead to both abnormalities in the ECG results and chest pain.
The NLR is an inexpensive indicator of systemic inflammation, is correlated with the prognosis of various diseases, eg, acute coronary syndrome and acute pancreatitis, and is useful in predicting subclinical atherosclerosis in patients with psoriasis.21–23 The NLR can be used to predict survival after coronary intervention in non-ST-segment elevation and ST-segment elevation myocardial infarction.24,25 Several reports have suggested the role of inflammation in the regulation of coronary microvascular responses in patients with CSX.26 In addition, an elevated NLR may be correlated with persistent inflammation and asymptomatic atherosclerosis in the pathophysiology of CSX, which is strongly confirmed by the results of the present study.27 The PLR has been considered as another indicator of systemic inflammation due to growing evidence that platelets play an early role in the process of inflammation and tissue repair,28 although it has been studied less frequently than the NLR.29 Platelets work closely with all types of leukocytes, and chemotactic substances secreted by the activated platelets, accelerating the binding of leukocytes to the endothelial surface and causing subsequent extravasation, and they may affect the inflammatory response of leukocytes in both a stimulatory and an inhibitory manner. Chronic low-grade inflammation may lead to an elevated PLR, and an increase in the PLR may be a sign of ongoing inflammation, which ultimately increases the risk of various diseases, including coronary artery disease, solid organ tumors, and autoimmune diseases.30 Based on the above studies, we speculate that the NLR and PLR may have a certain application value in CSX diseases. In the present study, an automatic blood cell analyzer was used to detect the NC, LC, and PLT in all subjects, and the NLR and PLR were subsequently calculated. When compared with the control group, the NC, PLT, NLR, and PLR were significantly higher and the LC was significantly lower in the CSX group, suggesting that the incidence of inflammatory response was significantly higher in the CSX group than in the control group and that the occurrence of CSX may lead to an abnormal inflammatory response in the organism, which would result in a disturbance of the balance of the NC, PLT, and LC, thus causing an imbalance in the NLR and PLR. This also verifies that the development of CSX may be closely correlated with an inflammatory response in the organism. In the present study, the diagnostic value of each indicator was analyzed using an ROC, and the results of the ROC analysis showed that both the NLR and PLR have excellent diagnostic value for CSX. In addition, multivariate logistic regression analysis was used to analyze the influencing factors of CSX, and it was found that ST-segment abnormalities, NLR > 2.21, and PLR > 119.77 are risk factors correlated with the occurrence of CSX. Therefore, close attention should be paid to patients with these indicators to prevent the development of CSX. Although NLR and PLR are not included in the current diagnostic indicators for CSX, in the early stage of the disease, abnormal changes in blood indicators often precede the appearance of clinical symptoms, so NLR and PLR have the potential to become auxiliary diagnostic indicators for CSX.
Some limitations existed in the present study. First, the limited sample size led to some discrepancies in the comparison of disease history and other information between patients in the present study and existing studies. Second, since the present study verified the existence of a relationship between the pathogenesis of CSX and inflammation, the pathogenesis of CSX could be explored in terms of immunity in patients.
Conclusion
NLR and PLR were abnormally elevated in the peripheral blood of patients with CSX. The abnormal elevation of these parameters may indicate dysregulated inflammatory responses in CSX. Therefore, inhibiting excessive inflammatory response may be a therapeutic strategy for the clinical treatment of CSX. Whether these parameters are related to the clinical prognosis of CSX patients will be analyzed in future studies.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Hebei General Hospital. A written informed consent was obtained from all participants.
Funding
Hebei Provincial Administration of Traditional Chinese Medicine Foundation Project No. 2019140.
Disclosure
All authors declare that the work is original and has not been submitted or published elsewhere. None of the authors have any financial disclosure or conflicts of interest.
References
1. Jovanovic I, Tesic M, Giga V, et al. Impairment of coronary flow velocity reserve and global longitudinal strain in women with cardiac syndrome X and slow coronary flow. J Cardiol. 2020;76(1):1–8. doi:10.1016/j.jjcc.2020.02.005
2. Kanar BG, Sünbül M. Cardiac syndrome X: an important cause of microvascular angina. Turk Kardiyol Dern Ars. 2018;46(6):437–438. doi:10.5543/tkda.2018.31050
3. Lutfi MF. Anxiety level and cardiac autonomic modulations in coronary artery disease and cardiac syndrome X patients. PLoS One. 2017;12(1):86–95. doi:10.1371/journal.pone.0170086
4. Masoudkabir F, Vasheghani-Farahani A, Hakki E, et al. Novel scoring system for prediction of cardiac syndrome X in women with typical angina and a positive exercise tolerance test. Tex Heart Inst J. 2018;45(1):5–10. doi:10.14503/THIJ-16-5906
5. Duman TT, Aktas G, Atak BM, et al. Neutrophil to lymphocyte ratio as an indicative of diabetic control level in type 2 diabetes mellitus. Afr Health Sci. 2019;19(1):1602–1606. doi:10.4314/ahs.v19i1.35
6. Aktas G, Sit M, Dikbas O, et al. Elevated neutrophil-to-lymphocyte ratio in the diagnosis of Hashimoto’s thyroiditis. Rev Assoc Med Bras. 2017;63(12):1065–1068. doi:10.1590/1806-9282.63.12.1065
7. Posul E, Yilmaz B, Aktas G, Kurt M. Does neutrophil-to-lymphocyte ratio predict active ulcerative colitis? Wien Klin Wochenschr. 2015;127(7–8):262–265. doi:10.1007/s00508-014-0683-5
8. Aktas G, Duman TT, Atak BM, et al. Irritable bowel syndrome is associated with novel inflammatory markers derived from hemogram parameters. Fam Med Prim Care Rev. 2020;22(2):107–110. doi:10.5114/fmpcr.2020.95311
9. Khalid A, Ali Jaffar M, Khan T, et al. Hematological and biochemical parameters as diagnostic and prognostic markers in SARS-COV-2 infected patients of Pakistan: a retrospective comparative analysis. Hematology. 2021;26(1):529–542. doi:10.1080/16078454.2021.1950898
10. Afsin H, Aktas G. Platelet to Lymphocyte and Neutrophil to Lymphocyte Ratios are useful in differentiation of thyroid conditions with normal and increased uptake. Ethiop J Health Dev. 2021;35(3):1–5.
11. Sit M, Aktas G, Erkol H, et al. Neutrophil to lymphocyte ratio is useful in differentiation of malign and benign thyroid nodules. P R Health Sci J. 2019;38(1):60–63.
12. Zahorec R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy. 2021;122(7):474–488. doi:10.4149/BLL_2021_078
13. Kounis NG, Koniari I, Plotas P, et al. Inflammation, thrombosis, and platelet-to-lymphocyte ratio in acute coronary syndromes. Angiology. 2021;72(1):6–8. doi:10.1177/0003319720946213
14. Atak B, Aktas G, Duman TT, et al. Diabetes control could through platelet-to-lymphocyte ratio in hemograms. Rev Assoc Med Bras. 2019;65(1):38–42. doi:10.1590/1806-9282.65.1.38
15. Atak B, Bakir Kahveci G, Bilgin S, et al. Platelet to lymphocyte ratio in differentiation of benign and malignant thyroid nodules. Exp Biomed Res. 2021; 4(2):148–153. doi:10.30714/j-ebr.2021267978
16. Aktas G. Hematological predictors of novel Coronavirus infection. Rev Assoc Med Bras. 2021;67Suppl 1(Suppl 1):1–2. doi:10.1590/1806-9282.67.Suppl1.20200678
17. Larmann J, Handke J, Scholz AS, et al. Preoperative neutrophil to lymphocyte ratio and platelet to lymphocyte ratio are associated with major adverse cardiovascular and cerebrovascular events in coronary heart disease patients undergoing non-cardiac surgery. BMC Cardiovasc Disord. 2020;20(1):230. doi:10.1186/s12872-020-01500-6
18. Ezhumalai B, Ananthakrishnapillai A, Selvaraj RJ, et al. Cardiac syndrome X: clinical characteristics revisited. Indian Heart J. 2015;67(4):328–331. doi:10.1016/j.ihj.2015.04.022
19. Hornick J, Costantini O. The electrocardiogram: still a useful tool in the primary care office. Med Clin North Am. 2019;103(5):775–784. doi:10.1016/j.mcna.2019.04.003
20. Adamstein NH, Ridker PM. The neutrophil-lymphocyte ratio: considerations for clinical application. Eur Heart J. 2021;42(22):2216–2217. doi:10.1093/eurheartj/ehab166
21. Balta I, Balta S, Demirkol S, et al. Neutrophil-to-lymphocyte ratio may predict subclinical atherosclerosis in patients with psoriasis. Echocardiography. 2014;31(9):1166–1167. doi:10.1111/echo.12668
22. Grenader T, Pavel ME, Ruszniewski PB, et al.; CLARINET Study Group. Prognostic value of the neutrophil/lymphocyte ratio in enteropancreatic neuroendocrine tumors. Anticancer Drugs. 2020;31(3):216–222. doi:10.1097/CAD.0000000000000909
23. Pinheiro Machado G, Araujo GN, Carpes CK, et al. Elevated neutrophil-to-lymphocyte ratio can predict procedural adverse events in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis. 2019;30(1):20–25. doi:10.1097/MCA.0000000000000671
24. Fan Z, Li Y, Ji H, Jian X. Prognostic utility of the combination of monocyte-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio in patients with NSTEMI after primary percutaneous coronary intervention: a retrospective cohort study. BMJ Open. 2018;8(10):e023459. doi:10.1136/bmjopen-2018-023459
25. Long M, Huang Z, Zhuang X, et al. Association of inflammation and endothelial dysfunction with coronary microvascular resistance in patients with cardiac syndrome X. Arq Bras Cardiol. 2017;109(5):397–403. doi:10.5935/abc.20170149
26. Okyay K, Yilmaz M, Yildirir A, et al. Relationship between neutrophil-to-lymphocyte ratio and impaired myocardial perfusion in cardiac syndrome X. Eur Rev Med Pharmacol Sci. 2015;19(10):1881–1887.
27. Wang N, Li C, Yang Y, et al. The use of platelet/lymphocyte ratio and cancer antigen 125 combined with magnetic resonance diffusion-weighted imaging in diagnosis of recurrent ovarian cancer and neuropathic pain. World Neurosurg. 2021;149:502–510. doi:10.1016/j.wneu.2020.11.117
28. Etulain J. Platelets in wound healing and regenerative medicine. Platelets. 2018;29(6):556–568. doi:10.1080/09537104.2018.1430357
29. Dasgupta R, Atri A, Jebasingh F, et al. Platelet-lymphocyte ratio as a novel surrogate marker to differentiate thyrotoxic patients with graves disease from subacute thyroiditis: a cross-sectional study from South India. Endocr Pract. 2020;26(9):939–944. doi:10.4158/EP-2020-0086
30. Ozdemir E, Safak O, AltIn MP, et al. Correlation between the severity of coronary artery ectasia and monocyte/lymphocyte, platelet/lymphocyte, and HDL/LDL ratios. J Coll Physicians Surg Pak. 2020;30(3):235–239. doi:10.29271/jcpsp.2020.03.235
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

