Back to Journals » Journal of Pain Research » Volume 16
The Relationship Between Pain Intensity and Pain-Related Activity Patterns in Older Adults with Chronic Musculoskeletal Pain: Mediating Roles of Pain Resilience and Pain Catastrophizing
Authors Gong Y, Wang Y , Wu W, Li L, Li Y, Song J , Jiang L, Hu S , Yang J, Wang A
Received 13 October 2022
Accepted for publication 25 February 2023
Published 10 March 2023 Volume 2023:16 Pages 797—807
DOI https://doi.org/10.2147/JPR.S393359
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jonathan Greenberg
Yan Gong,1 Yonghua Wang,2 Wei Wu,3 Ling Li,2 Yunming Li,4 Jie Song,2 Lingli Jiang,5 Shibei Hu,1 Juan Yang,1 Aihua Wang1
1School of Nursing, Chengdu Medical College, Chengdu, People’s Republic of China; 2Department of Nursing, The General Hospital of Western Theater Command, Chengdu, People’s Republic of China; 3Department of Anesthesiology and Pain Medicine, The General Hospital of Western Theater Command, Chengdu, People’s Republic of China; 4Department of Information, Medical Support Center, The General Hospital of Western Theater Command, Chengdu, People’s Republic of China; 5Department of Neurosurgery, The General Hospital of Western Theater Command, Chengdu, People’s Republic of China
Correspondence: Yonghua Wang, Department of Nursing, The General Hospital of Western Theater Command, No. 270 Tianhui Road, Rongdu Avenue, Chengdu, 610083, People’s Republic of China, Tel +86-18180720869, Email [email protected]
Purpose: To explore the relationship between pain intensity, pain resilience, pain catastrophizing, and pain-related activity patterns in older adults with chronic musculoskeletal pain (CMP).
Patients and Methods: A total of 220 elderly Chinese with chronic musculoskeletal pain were recruited from a tertiary general hospital. Participants completed several measures including a demographic questionnaire, Brief Pain Inventory (BPI), Pain Resilience Scale (PRS), Pain Catastrophizing Scale (PCS), and Patterns of Activity Measure-Pain (POAM-P). Moreover, Process version 3.5 plug-in SPSS26 was used to test the mediation effect between variables.
Results: The scores of POAM-P in older adults with CMP from high to low were: avoidance (27.39 ± 8.10), pacing (24.25 ± 9.48), and overdoing (16.65 ± 10.95). Mediation analysis revealed that pain resilience and pain catastrophizing mediated the relationship between pain intensity and pain-related activity patterns (avoidance and pacing) in older adults with CMP.
Conclusion: These results provide evidence for the role of pain resilience and pain catastrophizing in the relationship between pain intensity and pain-related activity patterns. Interventions targeting these factors should be included in activity management programs for elderly CMP patients. It may be possible to reduce the negative impact of pain intensity on activity patterns by improving pain resilience and reducing pain catastrophizing.
Keywords: older adults, chronic musculoskeletal pain, avoidance, pacing, overdoing
Introduction
Chronic musculoskeletal pain (CMP) refers to pain that occurs in muscles, bones, joints, tendons, or soft tissue and lasts more than 3 months.1 It is commonly associated with chronic primary neck pain, low back pain, osteoporosis, lumbar disc herniation, etc.2,3 The prevalence of CMP increases with age and is more prevalent in older women.4,5 CMP is persistent and easy to relapse. It is not only a simple bad feeling of pain, but also affects physical function, leading to a decreased level of physical activity, dyskinesia, weakness, falls, and decreased sleep quality, which is the most important cause of disability in the elderly.1,6,7 Chronic pain also hurts mental health. In the elderly population, chronic pain increases the risk for depression between 2.5 and 4.1 times.8 The World Health Organization (WHO) reported that musculoskeletal health posed a threat to healthy aging and might pose a significant socio-economic burden.9 With the aggravation of aging in China.10 CMP has become an urgent medical problem in China.
Patients with chronic pain usually change their activity patterns to minimize the intensity of pain and maximize physical function.11 The activity pattern refers to the way how individuals organize their daily activities,12 which plays an important role in the development and maintenance of chronic pain.13 Three activity patterns have been distinguished among individuals with chronic pain: Avoidance is characterized by the patient’s intentional avoidance of pain-related activities and results in reduced activity levels.14 Overdoing means that patients ignore their conditions and persist in longer or more intensive activities, which is characterized by high or fluctuating activity levels.14 Pacing includes task decomposition, combining work and rest, maintaining a steady pace, moderating activity levels, and alternating activity or rest on time rather than according to pain intensity. Its purpose is to save energy for valuable activities and improve activity endurance, and reduce pain intensity and disability level.15,16 Studies have reported higher levels of avoidance were associated with poorer psychological and physical function, and more severe pain interference,11,14 and older adults with CMP have less physical activity.17 Research examining the relationship between overdoing and function has also yielded inconsistent results, pacing was associated with better physical and psychological function.11,14,18
Pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.19 Several studies found reduced activity in elderly patients with musculoskeletal pain.20,21 In addition, the study of Larsson et al22 suggested that pain intensity was associated with kinesiophobia. Kindermans et al15 pointed out that pain intensity of CMP patients was positively correlated with the pacing. Pan et al16 found that pain intensity of patients with chronic pain was positively correlated with overdoing.
As a part of positive psychology, resilience is the process and outcome of successfully adapting to difficult or challenging life experiences, especially through mental, emotional, and behavioral flexibility and adjustment to external and internal demands.23 Patients with higher resilience would more actively take advantage of environmental or their strengths to cope with stressors and mitigate the adverse effects of stress, resulting in higher levels of physical and mental health.24,25 Thompson et al26 detected a negative correlation between pain intensity and pain resilience in adults with or at risk for knee osteoarthritis. Resilience affects an individual’s perception of negative events, which indirectly affects a patient’s behavior.27 The work of Resnick et al28 noted resilience was significantly correlated with physical activity.
Pain catastrophizing is conceptualized as a set of exaggerated and negative cognitive-affective responses to actual or anticipated pain.29 It is considered to be the most significant psychological factor related to pain and can participate in regulating pain behavioral responses.30,31 The study suggested that pain intensity was positively correlated with pain catastrophizing in patients with frozen shoulder.32 In a survey of older adults with osteoarthritis, pain catastrophizing was found to predict reduced physical activity and increased sedentary behavior.33 The study of Peñacoba et al34 suggested the moderating role of helplessness (as a dimension of pain catastrophizing) between some activity patterns (avoidance and overdoing) and function in women with fibromyalgia. Moreover, pain catastrophizing was positively correlated with pacing in women with fibromyalgia when pain acceptance was low.35
A study suggested that pain resilience was negatively related to pain catastrophizing in patients with coronary heart disease.24 The survey of patients with back pain showed that the predictive power of the fear-avoidance model of pain increased when individual differences in pain catastrophizing and pain resilience were considered.36 In conclusion, pain intensity was strongly correlated with pain resilience, which in turn was significantly related to pain catastrophizing, and pain catastrophizing was related to pain-related activity patterns.
Based on previous studies, the study tried to explore the following:
Hypothesis 1: Pain intensity will significantly predict pain-related activity patterns. Hypothesis 2: Pain resilience will mediate the association between pain intensity and pain-related activity patterns relationships. Hypothesis 3: Pain catastrophizing will mediate the association between pain intensity and pain-related activity patterns relationships. Hypothesis 4: Pain resilience and pain catastrophizing will act as a chain mediator between pain intensity and pain-related activity patterns.
Materials and Methods
Participants and Procedure
The minimum sample size of this study was determined by G*Power 3.1.9.7.37 This study required at least 119 participants to achieve a medium size effect (f2 = 0.15) with a power of 0.95 and 0.05 significance level. The cross-sectional study was conducted from December 2021 to August 2022. We recruited 220 older adults with CMP from a tertiary hospital in Chengdu, China. They all received treatment (such as medication, physical therapy, and Chinese medicine). The inclusion criteria were: (1) aged 60 and older; (2) CMP that lasted more than 3 months; (3) met the diagnostic criteria of CMP in ICD-11 for Mortality and Morbidity Statistics (coded as MG30.02 and MG30.3)38 and Chinese Expert Consensus on the Management of Chronic Musculoskeletal Pain in Elderly Patients (2019);4 (4) normal cognitive and communication skills, able to complete the questionnaire independently or with the help of researchers; (5) informed consent to participate in this study. The exclusion criteria were: (1) patients with other types of chronic pain (such as chronic neuropathic pain, chronic visceral pain, chronic headache, or orofacial pain); (2) patients with tumors; (4) patients with severe mental illness. This study was approved by the Ethics Committee of The General Hospital of Western Theater Command (2021EC5-123), and it was conducted based on the principles in the Declaration of Helsinki.
The researcher explained the purpose and significance of the survey to the patients and obtained their informed consent before distributing questionnaires for completion. In the process of investigation, unified instruction was used to explain the filling methods and precautions of the questionnaire. The researcher would read the questionnaire items and record the selected answers for those who had difficulty filling in due to limited education or poor vision.
Measures
A self-made demographic questionnaire based on a review of relevant literature and expert consultation was utilized to collect the characteristics of participants, including age, gender, place of residence, living with family, duration of pain, number of comorbidity, and types of pain area.
Pain Intensity
The Brief Pain Inventory (BPI) was developed by Cleeland et al39 and the Chinese version was applied and verified by Wang et al.40 The BPI was used to assess the patient’s pain intensity, including four items (most, least, average, and current pain), each of which was scored on a scale of 0 to 10, with higher scores indicating more severe pain. The average score of the four items was taken as the pain intensity score of the patients. The Cronbach’s α of the scale was 0.894.
Pain Resilience
The Pain Resilience Scale (PRS) was developed by Slepian et al41 and the Chinese version was translated by Dong.24 The scale has 14 items over three metrics: behavioral perseverance, cognitive, and affective positivity. This instrument was scored on a 5-point Likert scale; the total score for PRS ranges from 0 to 56. Higher scores indicate higher levels of pain resilience. The Cronbach’s α for the PRS was 0.821.
Pain Catastrophizing
The Pain Catastrophizing Scale (PCS) was originally designed by Sullivan et al31 and the Chinese version was applied and verified by Yap et al.42 The scale has 13 items over three metrics: rumination, magnification, and helplessness. This instrument was scored on a 5-point Likert scale; the total score for PCS ranges from 0 to 52. Higher scores indicate higher levels of pain catastrophizing. The Cronbach’s α for the PCS was 0.927.
Pain-Related Activity Patterns
The Patterns of Activity Measure-Pain (POAM-P) was developed by Cane et al14 and was translated by Pan.16 The scale consists of 30 items grouped into three subscales: avoidance, overdoing, and pacing. This instrument was scored on a 5-point Likert scale; the total score for each subscale ranges from 0 to 40. The Cronbach’s α of the three subscales was 0.95, 0.79, and 0.86, respectively.
Statistical Analysis
All statistical analyses were performed using SPSS 26.0 (IBM, Armonk, NY, USA). Continuous variables that were normally distributed were expressed as means and standard deviations, while categorical variables were expressed as numbers or percentages. Pearson correlation analysis was used to identify relationships among variables. In the mediation analysis, the total effect (c) is the effect of pain intensity on pain-related activity patterns (avoidance and pacing) after controlling the covariates and excluding the mediating variables (pain resilience and pain catastrophizing). The total effect includes direct effects (a1b1, a1a3b2, a2b2) and indirect effect (c’). The Process V3.5 in SPSS was used to analyze single and serial multiple mediating effects. The bootstrap method was used to estimate the 95% confidence interval with 5000 repeated sampling, and Two-sided inspection level α= 0.05.
Results
Participants’ Characteristics
The demographic characteristics of older adults with CMP (n=220) were shown in Table 1. The average age of the patients was 67.63 years (SD =6.92, ranging from 60 to 92 years). A large proportion of patients were female (68.6%), lived in towns (57.3%), and lived with family (85.5%). The most prevalent pain area was lower limb (40.40%), followed by upper limb (33.80%), and lower back (15.50%).
 |
Table 1 Baseline Characteristics of CMP in Older Adults (N=220) |
Correlation Analysis
We performed Pearson’s correlation analysis to explore relationships among pain intensity, pain resilience, pain catastrophizing, and pain-related activity patterns. Means, standard deviations, and correlation coefficient for each variable were shown in Table 2.
 |
Table 2 Correlation Analysis of Study Variables |
Multiple Mediation Analysis
The results of the multiple mediation analysis were presented in Figure 1A. First, the standardized regression coefficient (β) was significant in each path (ps < 0.01), controlling for the covariates (gender, living place, and number of comorbidity). The total effect of pain intensity on avoidance was significant (β= 0.462, p < 0.001). When controlling for the mediating variables, the direct effect remained significant (β = 0.233, p < 0.001).
Next, as shown in Table 3, the results analyzing pain intensity → pain resilience → avoidance, and pain intensity → pain catastrophizing → avoidance indicated the bootstrap 95% CIs did not contain 0; therefore, the independent mediating effects of pain resilience and pain catastrophizing were significant, accounting for 33.57% and 8.10% of the total effect respectively. Furthermore, pain intensity → pain resilience → pain catastrophizing → avoidance remained significant, indicating that pain resilience and pain catastrophizing had a chain mediating effect between pain intensity and avoidance, accounting for 7.90% of the total effect.
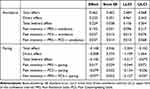 |
Table 3 Mediation Analysis of Relationship Between Pain Intensity and Pain-Related Activity Patterns (Avoidance and Pacing) |
The results of the multiple mediation analysis were presented in Figure 1B. The results showed the total effect of pain intensity on pacing was significant (β = −0.148, p < 0.05). However, the direct effect was not significant (β = −0.008, p >0.05) after the inclusion of mediating variables.
As shown in Table 3, the results analyzing pain intensity → pain resilience → pacing indicated the bootstrap 95% CIs contained 0; therefore, the indirect effect of pain intensity on pacing through pain resilience was not significant. However, the results analyzing pain intensity → pain catastrophizing → pacing and pain intensity → pain resilience → pain catastrophizing → pacing indicated the bootstrap 95% confidence intervals did not include 0; therefore, the indirect effect of pain intensity on pacing through pain catastrophizing was significant, and the chain mediating effect of pain resilience and pain catastrophizing was also significant.
Discussion
The present study examined the mediating role of pain resilience and pain catastrophizing between pain intensity and pain-related activity patterns (avoidance and pacing) in older adults with CMP. According to our results: (1) Avoidance had the highest score, followed by overdoing, and pacing had the lowest score; (2) Pain resilience and pain catastrophizing partially mediated between pain intensity and avoidance; (3) The relationship between pain intensity and the pacing pattern was mediated by pain catastrophizing or the chain mediating effect of pain resilience and pain catastrophizing. The current findings add to the literature by providing evidence for the role of pain resilience and pain catastrophizing in the relationship between pain intensity and pain-related activity patterns (avoidance and pacing).
In this study, the score of avoidance was 27.39 ± 8.10, overdoing was 16.41 ± 11.09, and pacing was 24.25 ± 9.48. This result was consistent with another study43 reporting that the score of overdoing was lower than those of the other two activity patterns. However, in patients with fibromyalgia, avoidance had the highest score, followed by overdoing, and pacing had the lowest score.11 To sum up, the score of avoidance was the highest among patients in different countries and types of pain. It was possible that for patients with pain, reducing the amount of activity can reduce pain intensity to a certain extent. However, several studies11,14 have shown that avoidance was positively correlated with poor physical and mental function. Therefore, older adults should engage in physical activity to the extent that their functional capacity allows, and adjust their physical activity effort to their fitness level.44
In the present study, pain intensity could predict avoidance in older adults with CMP, and hypothesis 1 was supported, which strengthens the relationship between pain intensity and decreased physical activity of patients.45 A study of older adults with chronic pain showed that patients with more severe pain have higher levels of kinesiophobia.22 And kinesiophobia caused patients to have an excessive and irrational fear of activities or movements, thus avoiding activities and leading to reduced activity.46,47 This suggested that activity avoidance in elderly patients with CMP can be reduced by relieving pain intensity.
Furthermore, pain resilience had a mediating effect on the association between pain intensity and avoidance, and hypothesis 2 was supported. Tanner et al48 showed that pain intensity was negatively correlated with pain resilience in patients with CMP. Similar results were found in this study. In the case of long-term pain, patients with a high level of pain resilience could maintain behavioral participation and the ability to regulate emotion and cognition,49 which had a positive effect on patients’ reasonable arrangement of activities, thus reducing the avoidance of activities. At the same time, the exercise of the elderly would increase with the improvement of pain resilience.50 Therefore, it is suggested that nurses should pay attention to the positive psychological status of patients and improve the level of pain resilience by reducing pain intensity, to reduce the avoidance of activities.
We found that pain catastrophizing mediates the relationship between pain intensity and avoidance, and hypothesis 3 was supported. The more severe the pain intensity, the more likely the patient is to over-focus and exaggerate the impact of pain, resulting in catastrophic thinking. Hirata et al32 showed that pain intensity improved the level of pain catastrophizing by reducing the self-efficacy of patients with frozen shoulder, indicating that pain intensity is closely related to pain catastrophizing. The study33 suggested that on mornings when older adults with osteoarthritis catastrophized more than usual about their pain in the day ahead, they spent more time in sedentary behavior and less time in physical activity that day. Meanwhile, higher levels of pain catastrophizing were positively correlated with reduced physical activity in people with knee osteoarthritis.51 The results of this study were supported by the fear-avoidance model,52 that is, pain experience leads to catastrophic thinking and pain-related fear, which in turn leads to avoidance behavior. Therefore, activity avoidance can be avoided by reducing the level of pain catastrophizing in older patients with CMP.
Another important finding was the chain mediating effect of pain resilience and pain catastrophizing in the relationship between pain intensity and avoidance of older adults with CMP, and hypothesis 4 was supported. Pain intensity indirectly affects pain resilience through cognitive, emotional, and other factors, so the individuals with more severe pain intensity were susceptible to negative emotional distress and were more inclined to adopt negative coping styles, thus reducing their pain resilience.53 The lower the level of resilience, the less effective it was to regulate negative emotions and alleviate catastrophic thinking. Compared with chronic pain patients with higher resilience, patients with lower resilience reported a higher level of pain catastrophizing.54 Also, the more severe the degree of pain catastrophizing, the more severe the fear-avoidance beliefs,55 leading to patients being more prone to avoid activities. It can be concluded that pain resilience and pain catastrophizing are important intermediate links between pain intensity and avoidance, indicating that the overall concept needs to be established in clinical work to comprehensively evaluate the physical and mental state of older CMP patients.
Our study findings showed that pain catastrophizing was positively correlated with overdoing (r=0.191, p<0.01), which was consistent with the results of a previous study,34 indicating that pain catastrophizing might have a potential impact on overdoing patterns. Overdoing was related to poor physical and mental function.56 Therefore, it is recommended that nurses should pay attention to the level of pain catastrophizing in patients. In the future, we should actively explore the variables related to overdoing to help understand the formation mechanism of the pattern.
We found that pain intensity negatively predicted the pacing pattern in elderly patients with CMP, and hypothesis 1 was supported. However, after adding two mediating variables, pain resilience and pain catastrophizing, the direct effect of pain intensity on the pacing pattern was not significant, indicating that the effect of pain intensity on the pacing pattern could only be achieved through pain resilience and pain catastrophizing. In the present study, pain resilience could not mediate the relationship between pain intensity and the pacing pattern, and hypothesis 2 was not supported by the findings. This may be because the effect of resilience on health behaviors is its joint effect with family care and social support.57 Therefore, resilience has not yet played a separate mediating role between pain intensity and pacing. We also found that pain catastrophizing mediates the relationship between pain intensity and pacing, and hypothesis 3 was supported. A study16 showed that pain catastrophizing is negatively correlated with activity pacing in chronic pain patients, which means that the lower the level of pain catastrophizing, the more patients tend to choose activity pacing. Activity pacing was considered to be adaptive.58 Therefore, multidisciplinary rehabilitation, exercise training, progressive relaxation therapy, and cognitive behavioral therapy can be adopted to reduce the level of pain catastrophizing,59 to promote older adults with CMP to choose activity pacing.
We also found that the chain mediating effect of pain resilience and pain catastrophizing in the relationship between pain intensity and activity pacing in older adults with CMP, and hypothesis 4 was supported. Among women experiencing chronic pain, the lower the pain intensity of patients, the higher the level of pain resilience, thus showing higher pain acceptance and self-regulatory efficacy beliefs,60 which has a certain buffer effect on reducing pain catastrophizing. In addition, the higher the pain resilience, the better the self-efficacy, and the more cognitive strategies of attention transfer and neglect could be adopted to get rid of the attention of pain-related information.61 Pan et al62 showed that lower levels of pain catastrophizing were associated with better physical and mental functioning, which enabled patients to better cope with chronic pain, and to choose adaptive activity patterns to ensure a balance between activity participation and pain relief.
The current study has the following important contributions: theoretically, the results of this study better clarify the role of the relationship between the four study variables and provide an important theoretical basis for how to help manage pain-related activity patterns in older adults with CMP. Practically, the study inspired nurses to consider not only reducing pain intensity but also improving cognitive-emotional responses to pain when managing activity patterns in elderly CMP patients, focusing on those with low levels of pain resilience and high levels of pain catastrophizing.
This study has some limitations. First, this study used self-report questionnaires, and the responses given by participants may not be consistent with the actual situation. Second, the cross-sectional design of this study could not explain the causal relationship between pain-related activity patterns and other variables in older patients with CMP. Longitudinal studies should be carried out to explore this issue in the future. Third, this study was conducted in a tertiary hospital in China, the sample size was not large enough and the participants consisted only of older adults with CMP, so the results may not be generalizable to other populations. Finally, the results of this study are limited because there is no data on the pre-existing pain-related activity patterns in the Chinese elderly population and the psychological attributes of the participants are not known.
Conclusion
To sum up, older adults with CMP often chose the avoidance activity mode. This study demonstrated the relationship between pain intensity and pain-related activity patterns, and the chain mediating effect of pain resilience and pain catastrophizing on pain intensity and pain-related activity patterns. Specifically, pain intensity was positively correlated with activity avoidance and negatively correlated with activity pacing. Pain resilience and pain catastrophizing played an important role in the relationship between pain intensity and activity patterns. Interventions targeting these factors should be included in activity management programs for elderly CMP patients. It may be possible to reduce the negative impact of pain intensity on activity patterns by improving pain resilience and reducing pain catastrophizing.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Lv Y, Cheng J, Fan B, et al. ICD-11 classification of chronic pain Chinese compiled version. Chin J Pain Med. 2018;24(11):801–805. doi:10.3969/j.issn.1006-9852.2018.11.001
2. Pain Department Branch of Chinese Physicians Association, National Key Clinical Specialties China-Japan Hospital Pain Specialist Medical Association, Beijing Pain Treatment Quality Control and Improvement Center. Expert consensus on drug therapy of chronic musculoskeletal pain (2018). Chin J Pain Med. 2018;24(12):881–887. doi:10.3969/j.issn.1006-9852.2018.12.001
3. Mao P, Lin X, Li Y, Wu Y. Chronic secondary musculoskeletal pain. Chin J Pain Med. 2021;27(5):323–326. doi:10.3969/j.issn.1006-9852.2021
4. Ji Q, Yi R, Wang J, Jian Z. Chinese expert consensus on the management of chronic musculoskeletal pain in elderly patients (2019). Chin J Geriatrics Res. 2019;6(2):28–34. doi:10.3877/cma.j.issn.2095-8757.2019.02.002
5. Woo J, Leung J, Lau E. Prevalence and correlates of musculoskeletal pain in Chinese elderly and the impact on 4-year physical function and quality of life. Public Health. 2009;123(8):549–556. doi:10.1016/j.puhe.2009.07.006
6. Treede RD, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19–27. doi:10.1097/j.pain.0000000000001384
7. Blyth FM, Noguchi N. Chronic musculoskeletal pain and its impact on older people. Best Pract Res Clin Rheumatol. 2017;31(2):160–168. doi:10.1016/j.berh.2017.10.004
8. Zis P, Daskalaki A, Bountouni I, Sykioti P, Varrassi G, Paladini A. Depression and chronic pain in the elderly: links and management challenges. Clin Interv Aging. 2017;12:709–720. doi:10.2147/cia.s113576
9. Briggs AM, Cross MJ, Hoy DG, et al. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 World Health Organization World Report on ageing and health. Gerontologist. 2016;56(Suppl 2):S243–S255. doi:10.1093/geront/gnw002
10. China Government Network [homepage on the Internet]. Notice on the issuance of the “14th Five-Year Plan” for healthy aging; 2022. Available from: http://www.gov.cn/zhengce/zhengceku/2022-03/01/content_5676342.htm.
11. Racine M, Galán S, de la Vega R, et al. Pain-related activity management patterns and function in patients with fibromyalgia syndrome. Clin J Pain. 2018;34(2):122–129. doi:10.1097/ajp.0000000000000526
12. Bendixen HJ, Kroksmark U, Magnus E, Jakobsen K, Alsaker S, Nordell K. Occupational pattern: a renewed definition of the concept. J Occupat Sci. 2006;13(1):3–10. doi:10.1080/14427591.2006.9686565
13. Van Damme S, Kindermans H. A self-regulation perspective on avoidance and persistence behavior in chronic pain: new theories, new challenges? Clin J Pain. 2015;31(2):115–122. doi:10.1097/ajp.0000000000000096
14. Cane D, Nielson WR, McCarthy M, Mazmanian D. Pain-related activity patterns: measurement, interrelationships, and associations with psychosocial functioning. Clin J Pain. 2013;29(5):435–442. doi:10.1097/AJP.0b013e31825e452f
15. Kindermans HPJ, Roelofs J, Goossens MEJB, Huijnen IPJ, Verbunt JA, Vlaeyen JWS. Activity patterns in chronic pain: underlying dimensions and associations with disability and depressed mood. J Pain. 2011;12(10):1049–1058. doi:10.1016/j.jpain.2011.04.009
16. Pan L. Adaption of Patterns of Activity Measure-Pain and the effect of Chronic Pain-Related Activity Patterns on the Functioning in Patients with Spine Degenerative Disease [dissertation]. China: Tianjin Medical University; 2019. doi:10.27366/d.cnki.gtyku.2019.000548
17. Stubbs B, Binnekade TT, Soundy A, Schofield P, Huijnen IPJ, Eggermont LHP. Are older adults with chronic musculoskeletal pain less active than older adults without pain? A systematic review and meta-analysis. Pain Med. 2013;14(9):1316–1331. doi:10.1016/j.jpain.2011.04.009
18. Racine M, Sánchez-Rodríguez E, de la Vega R, et al. Pain-related activity management patterns as predictors of treatment outcomes in patients with fibromyalgia syndrome. Pain Med. 2020;21(2):e191–e200. doi:10.1093/pm/pnz259
19. Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–1982. doi:10.1097/j.pain.0000000000001939
20. Stubbs B, Patchay S, Soundy A, Schofield P. The avoidance of activities due to fear of falling contributes to sedentary behavior among community-dwelling older adults with chronic musculoskeletal pain: a multisite observational study. Pain Med. 2014;15(11):1861–1871. doi:10.1111/pme.12570
21. Karttunen N, Lihavainen K, Sipilä S, Rantanen T, Sulkava R, Hartikainen S. Musculoskeletal pain and use of analgesics in relation to mobility limitation among community-dwelling persons aged 75 years and older. Eur J Pain. 2012;16(1):140–149. doi:10.1016/j.ejpain.2011.05.013
22. Larsson C, Ekvall Hansson E, Sundquist K, Jakobsson U. Kinesiophobia and its relation to pain characteristics and cognitive affective variables in older adults with chronic pain. BMC Geriatr. 2016;16:128. doi:10.1186/s12877-016-0302-6
23. American Psychological Association [homepage on the Internet]. The road to resilience: what is resilience? 2011. Available from: http://www.apa.org/helpcenter/road-resilience.aspx.
24. Dong W. Study on Pain Resilience and Associated Factors in Patients with Coronary Heart Disease [dissertation]. China: Tianjin Medical University; 2019. doi:10.27366/d.cnki.gtyku.2019.000663
25. Dai J, Shen C. Research progress of psychological resilience in patients with hypertension. Chin J Mod Nurs. 2021;27(4):548–551. doi:10.3760/cma.j.cn115682-20200608-03813
26. Thompson KA, Bulls HW, Sibille KT, et al. Optimism and psychological resilience are beneficially associated with measures of clinical and experimental pain in adults with or at risk for knee osteoarthritis. Clin J Pain. 2018;34(12):1164–1172. doi:10.1097/ajp.0000000000000642
27. Deshields TL, Heiland MF, Kracen AC, Dua P. Resilience in adults with cancer: development of a conceptual model. Psychooncology. 2016;25(1):11–18. doi:10.1002/pon.3800
28. Resnick B, Hebel JR, Gruber-Baldini AL, et al. The impact of body composition, pain and resilience on physical activity, physical function and physical performance at 2 months post Hip fracture. Arch Gerontol Geriatr. 2018;76:34–40. doi:10.1016/j.archger.2018.01.010
29. Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9(5):745–758. doi:10.1586/ern.09.34
30. Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122–131. doi:10.1016/j.amjsurg.2010.02.007
31. Sullivan M, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7(4):524–532.
32. Hirata J, Tomiyama M, Koike Y, Yoshimura M, Inoue K. Relationship between pain intensity, pain catastrophizing, and self-efficacy in patients with frozen shoulder: a cross-sectional study. J Orthop Surg Res. 2021;16(1):542. doi:10.1186/s13018-021-02693-y
33. Zhaoyang R, Martire LM, Darnall BD. Daily pain catastrophizing predicts less physical activity and more sedentary behavior in older adults with osteoarthritis. Pain. 2020;161(11):2603–2610. doi:10.1097/j.pain.0000000000001959
34. Peñacoba C, Pastor-Mira M, Suso-Ribera C, Catalá P, Nardi-Rodríguez A, López-Roig S. Activity patterns and functioning. A contextual-functional approach to pain catastrophizing in women with fibromyalgia. Int J Environ Res Public Health. 2021;18(10):5394. doi:10.3390/ijerph18105394
35. Ecija C, Catala P, López-Roig S, Pastor-Mira M, Gallardo C, Peñacoba C. Are pacing patterns really based on value goals? Exploring the contextual role of pain acceptance and pain catastrophizing in women with fibromyalgia. J Clin Psychol Med Settings. 2021;28(4):734–745. doi:10.1007/s10880-021-09762-8
36. Slepian PM, Ankawi B, France CR. Longitudinal analysis supports a fear-avoidance model that incorporates pain resilience alongside pain catastrophizing. Ann Behav Med. 2020;54(5):335–345. doi:10.1093/abm/kaz051
37. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi:10.3758/bf03193146
38. World Health Organization [homepage on the Internet]. ICD-11 for mortality and morbidity statistics (Version:02/2022); 2022. Available from: https://icd.who.int/browse11/l-m/en#.
39. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23(2):129–138.
40. Wang XS, Mendoza TR, Gao SZ, Cleeland CS. The Chinese version of the Brief Pain Inventory (BPI-C): its development and use in a study of cancer pain. Pain. 1996;67(2–3):407–416. doi:10.1016/0304-3959(96)03147-8
41. Slepian PM, Ankawi B, Himawan LK, France CR. Development and initial validation of the pain resilience scale. J Pain. 2016;17(4):462–472. doi:10.1016/j.jpain.2015.12.010
42. Yap JC, Lau J, Chen PP, et al. Validation of the Chinese Pain Catastrophizing Scale (HK-PCS) in patients with chronic pain. Pain Med. 2008;9(2):186–195. doi:10.1111/j.1526-4637.2007.00307.x
43. Burrus C, Vuistiner P, Léger B, Rivier G, Hilfiker R, Luthi F. Task-contingent persistence is related to better performance-based measures in patients with chronic musculoskeletal pain. Pain Res Manage. 2020;2020:1765456. doi:10.1155/2020/1765456
44. World Health Organization [homepage on the Internet]. WHO guidelines on physical activity and sedentary behaviour; 2020. Available from: https://www.who.int/publications/i/item/9789240015128.
45. Yoshimoto T, Fujii T, Oka H, Kasahara S, Kawamata K, Matsudaira K. Pain status and its association with physical activity, psychological stress, and telework among Japanese workers with pain during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(11):5595. doi:10.3390/ijerph18115595
46. Aydemir B, Huang CH, Foucher KC. Strength and physical activity in osteoarthritis: the mediating role of kinesiophobia. J Orthop Res. 2022;40(5):1135–1142. doi:10.1002/jor.25151
47. Alpalhão V, Cordeiro N, Pezarat-Correia P. Kinesiophobia and fear avoidance in older adults: a scoping review on the state of research activity. J Aging Phys Act. 2022;1–10. doi:10.1123/japa.2021-0409
48. Tanner JJ, Johnson AJ, Terry EL, et al. Resilience, pain, and the brain: relationships differ by sociodemographics. J Neurosci Res. 2021;99(5):1207–1235. doi:10.1002/jnr.24790
49. Ankawi B, Slepian PM, Himawan LK, France CR. Validation of the pain resilience scale in a chronic pain sample. J Pain. 2017;18(8):984–993. doi:10.1016/j.jpain.2017.03.013
50. Yang J, Ren Y, Li Y, Tang S. The influence of physical exercise on the spiritual well-being of the elderly: the mediator role of psychological resilience. Chin J Clin Psychol. 2021;29(1):191–194+208. doi:10.16128/j.cnki.1005-3611.2021.01.039
51. Uritani D, Kasza J, Campbell PK, Metcalf B, Egerton T. The association between psychological characteristics and physical activity levels in people with knee osteoarthritis: a cross-sectional analysis. BMC Musculoskelet Disord. 2020;21(1):269. doi:10.1186/s12891-020-03305-2
52. Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. doi:10.1016/s0304-3959(99)00242-0
53. Sturgeon JA, Zautra AJ. Resilience: a new paradigm for adaptation to chronic pain. Curr Pain Headache Rep. 2010;14(2):105–112. doi:10.1007/s11916-010-0095-9
54. Ong AD, Zautra AJ, Reid MC. Psychological resilience predicts decreases in pain catastrophizing through positive emotions. Psychol Aging. 2010;25(3):516–523. doi:10.1037/a0019384
55. Shim EJ, Hahm BJ, Go DJ, et al. Modeling quality of life in patients with rheumatic diseases: the role of pain catastrophizing, fear-avoidance beliefs, physical disability, and depression. Disabil Rehabil. 2018;40(13):1509–1516. doi:10.1080/09638288.2017.1300691
56. Andrews NE, Strong J, Meredith PJ. Activity pacing, avoidance, endurance, and associations with patient functioning in chronic pain: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2012;93(11):2109–2121.e7. doi:10.1016/j.apmr.2012.05.029
57. Sun T, Liu W, Zhao H, Li X, Bai J, Ye H. A study on the correlation between self-management behavior and psychological status in elderly patients with type 2 diabetes mellitus. Qilu Nurs J. 2022;28(11):68–71. doi:10.3969/j.issn.1006-7256.2022.11.020
58. Luthi F, Vuistiner P, Favre C, Hilfiker R, Léger B. Avoidance, pacing, or persistence in multidisciplinary functional rehabilitation for chronic musculoskeletal pain: an observational study with cross-sectional and longitudinal analyses. PLoS One. 2018;13(9):e0203329. doi:10.1371/journal.pone.0203329
59. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2017;166(7):514–530. doi:10.7326/m16-2367
60. Brittain DR, Gyurcsik NC, Cary MA, Moser EN, Davis LS. Differences in resilience mechanisms and physical activity among women experiencing chronic pain with higher or lower resilience. Womens Health Issues. 2022;32(3):309–316. doi:10.1016/j.whi.2021.11.004
61. Ling Y, Chen H, Jackson T. The effect of pain resilience on pain-related self-efficacy, coping and pain adaptation. Chin J Pain Med. 2021;27(6):449–454. doi:10.3969/j.issn.1006-9852.2021.06.009
62. Pan L, Sun Y, Li Y, Cao H, Li Y, Shi B. Relationship between catastrophic thinking and functional status among elderly patients with chronic degenerative low back pain: the mediating effect of pain acceptance. Chin Nurs Res. 2019;33(24):4247–4251. doi:10.12102/j.issn.1009-6493.2019.24.011
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

