Back to Journals » Psychology Research and Behavior Management » Volume 16
The Relationship Between Fear and Anxiety Among Chinese Uninfected Residents During the Pandemic: A Conditional Process Analysis
Received 5 May 2023
Accepted for publication 29 September 2023
Published 6 October 2023 Volume 2023:16 Pages 4095—4104
DOI https://doi.org/10.2147/PRBM.S420047
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Zhaoliang Li,1 Fanglin Wang,1 Yang Sun2
1College of Philosophy and Sociology, Jilin University, Changchun, People’s Republic of China; 2Psychological Institute and Network Aging Research, Ruprecht Karls University of Heidelberg, Baden-Württemberg, Germany
Correspondence: Yang Sun, Psychological Institute and Network Aging Research, Ruprecht Karls University of Heidelberg, Bergheimer Str. 20, Heidelberg, 69115, Germany, Email [email protected]
Background: This study aimed to explore the relationship between residents’ COVID-19 fear and anxiety, consider whether this relationship is mediated through obsessions and the moderating role of self-efficacy on this mediating pathway.
Methods: This study used an online questionnaire to obtain and assess fear, obsession, anxiety and self-efficacy in 1589 Chinese COVID-19 uninfected residents. A conditional process model was used to examine the relationships between variables.
Results: Higher levels of fear were positively associated with obsession and anxiety. In addition, obsession was positively associated with anxiety, while self-efficacy attenuated the effect of fear on obsession and further mitigated the indirect effect of fear on anxiety through obsession.
Conclusion: During the COVID-19 outbreak, uninfected residents suffered varying degrees of psychological distress. COVID-19 fear may have an effect on anxiety in COVID survivors through obsession, and self-efficacy as a protective factor for individual mental health partially attenuates the effect of COVID-19 fear on obsession and the indirect effect of fear on anxiety.
Keywords: fear, anxiety, obsession, self-efficacy, prevention, Chinese COVID-19 uninfected residents
Introduction
Although the COVID-19 pandemic may have ended, we still need to pay attention to the adverse effects of prolonged isolation and fear of the virus on mental health.1 A significant body of research reports that the after-effects of this pandemic (such as post-traumatic stress disorder) may persist for several years.2,3 Some previous survey results indicate that rates of depression, anxiety, and suicidal tendencies have continued to rise globally in the two years following the COVID-19 outbreak.4–7 In China alone, a study conducted during the pandemic revealed that 53.8% of respondents reported moderate to severe impacts on their mental health due to the outbreak.8 It is important to note that the psychological impact of the pandemic has shown significant differences across different countries and subgroups. Some studies suggest that residents in developing countries experience higher levels of anxiety, depression, and stress.9,10
On the other hand, other research points out that younger individuals (<30 years old), individuals living alone, and individuals with pre-existing mental health conditions seemed to suffer more psychological distress during this pandemic.11–14 The reasons for these variations can be considered at the societal and individual levels. At the societal level, a country’s level of development and the government’s response to the pandemic can indirectly influence individuals’ mental health.11,15 At the individual level, factors such as age, education level, and medical history may directly impact an individual’s mental health.7,11,12,16 However, these factors have not been comprehensively examined, which hinders the effective development of tailored psychological prevention and intervention measures based on individual and regional differences.
An increasing number of psychologists and psychiatrists are calling for a comprehensive examination of the impact of the pandemic, with reducing residents’ psychological distress as one of the main objectives in rebuilding their mental health in the post-pandemic era and preventing the potential impact of future crises.17 Previous research on the psychological distress caused by the COVID-19 pandemic has mainly focused on front-line healthcare workers or infected individuals, with limited exploration of the relationship between the psychological distress experienced by COVID-19 survivors and their negative emotions.18,19 However, some of the latest results suggest that due to prolonged lockdowns, and uncertainty over the spread and impact of the virus, residents who were not infected during the COVID-19 outbreak also suffered from different levels of psychological distress, and some residents even experienced a significant increase in anxiety and depression in a short period of time.20 Previous studies have indicated a significant association between these negative emotions resulting from lockdown measures and heightened suicidal tendencies, prompting the attention and concern of mental health experts.21 Therefore, in order to provide reference for subsequent regional or global public health events and improve the effectiveness and adaptability of public health response policies and reduce the harm of the COVID-19 pandemic to individual mental health, it is very important to pay attention to and explore the relationship between the negative emotions of uninfected residents, and to explore and verify the role of different psychological protection mechanisms.
Fear and anxiety are the first observed negative emotions during the COVID-19 pandemic, and there is a strong correlation between them.22–24 Fear and anxiety are considered necessary to maintain the unity and integrity of the individual’s self. Although for a long time, researchers believed that fear and anxiety were indistinguishable and overlapped on a subjective level. But the latest neurobiological findings suggest that fear and anxiety are triggered by distinct neurobiological networks designed to respond to different evolutionary needs.25,26 Fear is often a direct response to harm or threat, whereas anxiety is an individual’s assessment of their coping abilities when faced with a challenge.26 The global pandemic outbreak is the primary source of fear for everyone at this stage, and how to deal with this uncertainty crisis has undoubtedly increased the anxiety of individuals to a large extent. Some previous studies have shown that anxiety levels increase as individuals become more fearful.27 After the outbreak of the pandemic, fear and anxiety have generally appeared in the public, and statistics show that high levels of fear are often accompanied by high anxiety.24,28,29 However, there is still a lack of research to explore and verify their relationship and the possible mediating and regulatory mechanisms.30 Therefore, this study will mainly focus on and explore the relationship between COVID-19 fear and anxiety in COVID-19 survivors during the pandemic, assuming that COVID-19 fear positively predicts individual coronavirus anxiety.
Obsessive-compulsive thoughts, one of the main symptoms of obsessive-compulsive disorder, are recurring, persistent, uncontrollable thoughts or urges in an individual, usually about harm, threat, and risk, that tend to trigger anxiety and are associated with intrusiveness.31,32 Previous multi-country studies have consistently shown that individuals experience varying degrees of compulsive thinking or compulsive behaviors due to the COVID-19 pandemic, regardless of whether they have ever been diagnosed with OCD.33,34 And the pandemic’s uncertainty, unpredictability, fear and stress are the main reasons for the high prevalence of new compulsive thinking and compulsive behavior.32,35 However, to our knowledge, current research does not explicitly explore the relationship between fear, obsessions, and anxiety. Therefore, based on the above findings, we explore and hypothesize that obsession is a mediating factor between fear and anxiety in this study, and fear increases an individual’s risk of developing anxiety to a certain extent through obsessions.
Lockdowns have proven to be the best way to deal with the rapid spread of the virus, and various levels of lockdowns have been adopted around the world after the outbreak of COVID-19. On the one hand, these measures have blocked the spread of the virus; on the other hand, they have had a specific impact on individual psychology. While some studies have indicated that government responses to COVID-19 have partially alleviated depression symptoms in some populations,15 more research results suggest that prolonged lockdowns have hindered individuals from engaging in regular social interactions and accessing psychological support from their previously stable social networks. In such circumstances, individuals are left to rely on their internal psychological resources to cope with the psychological distress caused by the pandemic and lockdown measures.20,36 Self-efficacy is people’s beliefs about their ability to cope with and control negative events and is an essential internal psychological resource for individuals.37 According to social cognitive theory, in the face of sudden stressful events, an individual’s self-efficacy can positively influence them to produce more positive coping strategies and behaviors by influencing motivation, emotion, and cognitive evaluation.38 Bandura believes that self-efficacy is negatively related to stress-related negative emotions and positively related to psychological resources such as resilience and perseverance, indicating that it positively affects negative situations.39 This view has also been confirmed in studies related to the COVID-19 pandemic, such as a newly published longitudinal study on the impact of self-efficacy shows that individuals with high self-efficacy tend to be able to maintain stable positive emotions and lower levels of negativity after prolonged lockdowns.40 Based on social cognitive theory and the above findings, we hypothesized that self-efficacy could moderate the effect of fear on obsession, and this moderating effect further influences the indirect effect of fear on anxiety through obsession.
In conclusion, this study examines the relationship between fear and anxiety among uninfected residents during the COVID-19 outbreak and the conditional process model that may exist between the two relationships. The purpose is to make up for the current lack of attention to the impact of COVID-19 on the mental health of uninfected people, as well as the insufficient understanding of the relationship between fear and anxiety. We developed the following three assumptions and plotted the conditional process model (Figure 1).
Hypothesis 1 (H1): The higher the fear of COVID-19, the more anxious the survivor of COVID-19; Hypothesis 2 (H2): Obsession mediates the relationship between COVID-19 fear and anxiety in uninfected residents; Hypothesis 3 (H3): Higher self-efficacy attenuates the effect of COVID-19 fear on obsession and further attenuates the indirect effect of fear on anxiety through obsession.
 |
Figure 1 Fear-Obsession-Anxiety Hypothesis Test Model. |
Materials and Methods
Participants
Early in the COVID-19 pandemic outbreak (May 2020), we conducted a cross-sectional survey study recruiting participants in Jilin Province, China, using a convenient sampling approach. Recruiting was based on adult residents aged 18 and older, without cognitive impairment, who could use a smartphone for independent operation and were not infected with the coronavirus. To avoid exposure to infection, the researchers distributed electronic questionnaires to participants through a social platform (WeChat). Before the study, we informed all participants of the purpose and use of this anonymous study and their rights. All participants signed an informed consent form before answering the questions. A total of 1713 residents participated in this study. After excluding those who did not meet the inclusion criteria (<18 years old) and invalid responses (missing questions or answering less than 3 minutes), we obtained 1589 valid data, with a data recovery rate of 92.8%. The age range of participants in the final sample was 18–75 years (M=34.34, SD=12.37), and 1080 (68%) were female.
Assessment and Measurement
Independent Variable
Residents’ fear of the COVID-19 pandemic is measured using the COVID Fear Scale.41 The scale consists of 7 items, and each is scored on a 5-point scale. The overall score is between 0–35, with higher scores indicating higher fear of COVID-19. The Cronbach’s alpha for the scale in this study was 0.92.
Dependent Variable
Participants’ anxiety caused by coronavirus-related information and thoughts over the past two weeks was measured using the 5-term Coronavirus Anxiety Scale (CAS).42 The scale uses a 5-point Likert scale from 0 to 4, with a total score between 0 and 25, with higher scores indicating higher anxiety levels. The Cronbach’s alpha measured in this study was 0.88.
Mediating Variable
To measure residents’ obsession with COVID-19, we used The Obsession with COVID-19 Scale (OCS).43 The scale OCS includes a total of 4 items, and the items are rated on a 5-point Likert scale, with a total score ranging from 0 to 20. The score indicates the frequency and degree of obsessive thinking about content that respondents have experienced in the past two weeks due to the COVID-19 pandemic. In this study, the Cronbach’s alpha for this scale was 0.79.
Moderator
Residents’ self-efficacy was measured using the Chinese version of the General Self-Efficacy Scale (GSES), which contains 10 questions, all 4-point Likert scales.44,45 The total self-efficacy score is the sum of the scores of 10 items. The score forecast indicates that the stronger the respondents’ self-efficacy, the more confident they are. In this study, Cronbach’s alpha for this scale was 0.93.
Covariates
In this study, participants primarily reported the following demographic information: age, gender (1=male; 2=female), and living alone during the COVID-19 pandemic (yes/no).
Statistical Analysis
First, we performed a standard method bias test on the data using SPSS 24.0 and performed descriptive and Pearson correlation analyses of the main study variables and covariates. Secondly, we used the PROCESS macro 3.3 written by Hayes46 to carry out the verification analysis of the mediation model and the conditional process model (the regulated mediation model) successively. This macro is one of the most widely used statistical tools to detect whether the mediator effect value is adjusted. According to the suggestion of Preacher et al47 and Edwards & Lambert,48 when the bootstrap method is used to simulate the repeated sampling of the sample (n=1589), the confidence interval of the 95% deviation of the value obtained does not contain zero. In the further simple slope analysis results, there is a difference in the mediating effect value under one standard deviation of the moderator variable. The mediation pathway can be considered to be regulated.
The bootstrap analysis used in the data analysis of this study is to obtain 95% bias-corrected confidence intervals by simulating 5000 repeated samplings. An effect is significant if the upper and lower bounds of the confidence interval (CI) for an effect do not include zero.
Results
Common Method Bias Test
Since the data in this study are all from questionnaires, we require respondents to answer the questionnaire anonymously to reduce the possible errors caused by a single self-report method. Statistically, Harman’s univariate test was used to test whether the data involved in this study had common method bias. The results show that there are 3 factors with eigenvalues greater than 1 involved in this study, and the variance explanation rate of the first factor is 28.44% (< 40%), indicating that there is no serious common method bias in this study.49
Initial Analysis
Descriptive statistics and bivariate correlations between all study variables and covariates are shown in Table 1. According to the scoring criteria proposed by Lee,42,43 8.8% of respondents in this study reported high levels of coronavirus anxiety (CAS ≥ 9), and 11.1% reported excessive obsession with COVID-19 (COS ≥ 7). In addition, the correlation matrix showed that fear was significantly positively correlated with obsession and anxiety and negatively correlated with self-efficacy; obsession was significantly positively correlated with anxiety. On the other hand, the covariate age was significantly and positively correlated with the study variables (fear, obsession, anxiety, and self-efficacy); Gender is positively correlated with fear and negatively correlated with self-efficacy; Living alone was negatively correlated with both fear and anxiety. It is necessary to include the above covariates in further mediation analysis and conditional process model testing.
 |
Table 1 Descriptive Statistics and Bivariate Correlations Between All Study Variables and Covariates |
Mediating Effect Analysis
The SPSS macro PROCESS developed by Hayes46 was used to verify the mediating dictation of obsession in the relationship between residents’ fear and anxiety (Model 4). The results showed that the indirect effect of fear on anxiety through obsession was significant, the mediating effect index was 0.29 (95% CI = [0.24, 0.17], p <0.01), and the mediating effect accounted for 63.69% of the total effect. Fear had a certain direct effect on anxiety (β = 0.17, t = 8.04, 95% CI = [0.13, 0.21], p<0.01). Therefore, residents’ fear of COVID-19 is an influencing factor of coronavirus anxiety, and this effect is mediated by obsession, and the results support hypothesis (H1, H2).
Conditional Process Model Analysis
Table 2 shows the results based on the above research results of further conditional process model analysis using the SPSS macro PROCESS. Specifically, after controlling for covariates (age, sex, and living alone), we examined whether the first half of the mediating pathway of fear-obsessed anxiety was mediated by self-efficacy. The first regression equation results show that residents’ fear has a significant effect on obsession (β = 0.47, t = 20.46, 95% CI = [0.43, 0.52], p<0.01); The interaction of fear and self-efficacy significantly negatively affects obsession (β=−0.06, t=−3.00, 95% CI = [−0.10, 0.02], p < 0.01). Regression Equation 2 shows that both fear and obsession have an effect on anxiety (β=0.17 and 0.62, t=8.04 and 30.92, 95% CI = [0.13, 0.21] and [0.58, 0.66], p < 0.001).
 |
Table 2 Results of Further Conditional Process Model Analysis |
Further bias-corrected bootstrapping analysis showed that the indirect effects of fear on anxiety through obsession were different at different levels of self-efficacy. As shown in Table 3, regardless of whether the self-efficacy is low or high, the indirect effect of fear on anxiety is significant. The difference is that the indirect effect of fear on anxiety is stronger with low self-efficacy (−1 SD), and the indirect effect of fear on anxiety was partially attenuated by high self-efficacy (+1 SD).
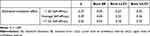 |
Table 3 Estimated Conditional Indirect Effect Fear → Obsession→ Anxiety at Different Values of Self-Efficacy |
The above findings suggest that obsession among uninfected residents during the COVID-19 pandemic mediates the relationship between fear and anxiety. This mediating effect of obsession was negatively moderated by self-efficacy (first-stage moderation), supporting hypothesis (H3).
Discussion
The purpose of this study is to focus on and explore the impact of this global pandemic on the mental health of COVID-19 survivors (fear, anxiety and obsession), to examine the direct and indirect effects of COVID-19 on anxiety through obsessions and whether these effects are mediated by self-efficacy. On the one hand, we found through a large sample survey study that the high rate of anxiety and excessive obsession among uninfected residents during the COVID-19 pandemic reached 8.8% and 11.1% respectively. This result is higher than that in Korea during the same period (N = 329, CAS = 3.3%, OCS = 5.5%)50 and Turkey (N = 763, CAS = 3.8%).51 Survey data obtained using the same scale in adults demonstrate the importance and necessity of paying attention to the negative emotions of Chinese COVID-19 survivors.
The psychological responses of individuals to the pandemic are influenced by various demographic factors such as gender and age.52 The results of this study indicate that, during the current pandemic, the age of uninfected residents in China is significantly correlated with anxiety and obsession. Compared to younger individuals, older adults have experienced more negative effects during this pandemic, displaying higher levels of anxiety and obsession. Surprisingly, in this study, participants’ gender was not significantly associated with their anxiety and obsession, contrary to previous research conducted in other countries such as Italy and France.53,54 This discrepancy may be attributed to differences in sample characteristics and sociocultural backgrounds. Future research should involve larger cross-cultural samples to explore the underlying reasons for these differences. Furthermore, there is a need for further research that comprehensively examines the influence of participants’ demographic factors and environmental factors on individuals’ psychological well-being during major stress events like pandemics. Such research will provide a more robust theoretical foundation for the development of targeted prevention and intervention measures.
On the other hand, the results of this study support our main hypothesis. First, the findings establish a positive association between COVID-19 fear and anxiety. This means that individuals with high fear tend to be accompanied by high anxiety levels, which is consistent with previous findings in other groups.30 While the current cross-sectional study results cannot infer whether there is a causal relationship between fear and anxiety. However, from a statistical point of view, the results of regression tests are directional. Therefore, our findings somewhat support the hypothesis that fear positively affects anxiety (H1).
Moreover, the findings again underscore the significance and necessity of preventing and alleviating residents’ fears during pandemics, which play a crucial role in further interventions and mitigating the psychological distress caused by such outbreaks. Second, after controlling for age, gender and whether they lived alone, the direct effect of fear on anxiety and the indirect effect through obsession was significant. We validated our previous hypothesis that obsession mediates the relationship between fear and anxiety (H2). Previous research findings were mainly about the pairwise relationship between fear and obsession, obsession and anxiety, and fear and anxiety, with limited exploration of their comprehensive relationship. Our study results partially address this gap in the field and provide a solid theoretical foundation for future preventive and intervention efforts. Finally, our findings show that self-efficacy negatively moderates the effects of fear on obsession, and this moderating effect further influences the indirect effect of fear on anxiety through obsession, validating and supporting our proposed conditional process model (H3). Specifically, individuals with high self-efficacy were more able to maintain emotional stability during the pandemic and fewer obsessions and anxiety due to fear of COVID-19. The results of this study validate the social cognitive theory38 and self-efficacy models.55,56 The effectiveness during the COVID-19 outbreak supports previous research conclusions that self-efficacy as a protective factor for individual psychology can effectively alleviate the psychological distress caused by the COVID-19 pandemic.57
The above findings not only reiterate the significant impact of the current pandemic on residents’ mental health but also highlight the vulnerability of residents’ psychological resilience during crises, emphasizing the necessity of developing a nationwide psychological intervention plan. Cognitive Behavioral Therapy (CBT) has been widely used in various psychological interventions during this pandemic, and numerous empirical studies have demonstrated its significant effectiveness in reducing negative emotions and insomnia associated with COVID-19.58 Internet-delivered Cognitive Behavioral Therapy (I-CBT) has been extensively applied in countries like China and Singapore during lockdown periods, overcoming limitations of time and location, and its efficacy has been well-established through multiple validations.58–61 These successful cases provide valuable insights for future intervention plans to address the psychological distress caused by crises. Governments and relevant agencies should prioritize the role of CBT in crisis psychological interventions and leverage emerging technologies such as the Internet to develop more widespread, convenient, and efficient psychological intervention programs for the public.
As mentioned earlier, some limitations of this study as a cross-sectional study should be considered when discussing and evaluating the above findings. First, since our findings came from a cross-sectional study, we cannot make any causal inferences about the relationship between fear and anxiety among Chinese residents infected with COVID-19. Therefore, further follow-up investigations are needed to verify and expand the conditional process model proposed in this study. Second, since the study was conducted during a large-scale outbreak of COVID-19, research limited by public distancing measures of the COVID-19 pandemic, participants can only be recruited through social networks by convenience sampling. Although a large sample size was obtained, this sampling method may not cover all populations (for example, older people without mobile phones, etc.), limiting the sample’s representativeness and diversity to some extent. Finally, survey research using only self-report methods is often subject to potential bias (eg, participant volatility may be influenced by factors such as social expectations). We suggest that methods such as a combination of others and self-reports can be used in future research to reduce this bias.
Despite these limitations, the results of this study are robust and support the use of fear as a related factor for anxiety in residents uninfected by COVID-19. And these results found that obsession may serve as a potential mechanism for fear and anxiety. In addition, the results of this study further reveal that the mediating effect of obsession is mediated by self-efficacy. It is suggested that maintaining a high level of self-efficacy in the face of public health emergencies can often weaken the direct and indirect effects of fear on anxiety. The above findings have both theoretical and practical significance for preventing and reducing the harm of the COVID-19 pandemic to individual psychology.
Conclusion
This article explores and describes the effect of fear on anxiety among uninfected residents during the covid-19 outbreak. The results suggest that residents’ fear of COVID-19 increases the risk of developing anxiety through obsession, and the level of individual self-efficacy moderated this mediating effect. Therefore, health departments need to pay attention to the negative emotions of COVID-19 survivors, intervene in a timely manner, release timely and effective information, carry out relevant popular science activities, etc. Raise residents’ scientific awareness of the pandemic and reduce public fears about COVID-19. In addition, at the individual level, residents should recognize that improving self-efficacy is conducive to maintaining positive emotions, reducing and alleviating the positive effects of individual obsessions and anxiety caused by fear of COVID-19, and consciously increasing self-efficacy. At the societal level, facing possible future public health emergencies, we should focus more on individuals with low self-efficacy and implement intervention measures to alleviate their potential psychological distress. Finally, in the post-pandemic new normal era, comprehensively understanding and mitigating “COVID-19 psychological after-effects” is one of the main tasks. Some issues, such as COVID-19 burnout,62 have severely impacted the recovery of social production, and more research is needed to characterize and develop intervention programs to address these sequelae.
Ethical Approval
This study was reviewed and approved by the Ethics Committee of Jilin University. The study followed the principles of the Declaration of Helsinki. All participants were requested to read and sign the informed consent form before starting this study.
Funding
This study was supported by the National Social Science Foundation of China (15BSH087). Yang Sun completed the writing and revision of the manuscript during her PhD, which was funded by the China Scholarship Council (No.202106170007).
Disclosure
The authors report no potential conflicts of interest in this work.
References
1. Zhou X, Chen Y, Zhu L, An Z, Zhang J, Ge J. The association between group identity and post-traumatic growth in the post COVID-19 era: the mediating Effect of social-emotional competence. Psychol Res Behav Manag. 2023;16:2869–2882. doi:10.2147/PRBM.S419484
2. Ceban F, Ling S, Lui LMW, et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: a systematic review and meta-analysis. Brain Behav Immun. 2022;101:93–135. doi:10.1016/j.bbi.2021.12.020
3. Tan W, Hao F, McIntyre RS, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. doi:10.1016/j.bbi.2020.04.055
4. Luo Y, Chua CR, Xiong Z, Ho RC, Ho CSH. A systematic review of the impact of viral respiratory epidemics on mental health: an implication on the Coronavirus disease 2019 pandemic. Front Psychiatry. 2020;11:565098. doi:10.3389/fpsyt.2020.565098
5. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi:10.1016/j.jad.2020.08.001
6. Brown SM, Doom JR, Lechuga-Peña S, Watamura SE, Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl. 2020;110(Pt 2):104699. doi:10.1016/j.chiabu.2020.104699
7. Ceban F, Nogo D, Carvalho IP, et al. Association between mood disorders and risk of COVID-19 infection, hospitalization, and death: a systematic review and meta-analysis: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(10):1079–1091. doi:10.1001/jamapsychiatry.2021.1818
8. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi:10.3390/ijerph17051729
9. Kola L, Kohrt BA, Hanlon C, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. 2021;8(6):535–550. doi:10.1016/S2215-0366(21)00025-0
10. Wang C, Chudzicka-Czupała A, Tee ML, et al. A chain mediation model on COVID-19 symptoms and mental health outcomes in Americans, Asians and Europeans. Sci Rep. 2021;11(1):6481. doi:10.1038/s41598-021-85943-7
11. Wang C, Tee M, Roy AE, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PLoS One. 2021;16(2):e0246824. doi:10.1371/journal.pone.0246824
12. Ren Z, Xin Y, Wang Z, Liu D, Ho RCM, Ho CSH. What factors are most closely associated with mood disorders in adolescents during the COVID-19 pandemic? A cross-sectional study based on 1771 adolescents in Shandong province, China. Front Psychiatry. 2021;12:728278. doi:10.3389/fpsyt.2021.728278
13. Hao F, Tam W, Hu X, et al. A quantitative and qualitative study on the neuropsychiatric sequelae of acutely ill COVID-19 inpatients in isolation facilities. Transl Psychiatry. 2020;10(1):355. doi:10.1038/s41398-020-01039-2
14. Hao F, Tan W, Jiang L, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–106. doi:10.1016/j.bbi.2020.04.069
15. Lee Y, Lui LMW, Chen-Li D, et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J Affect Disord. 2021;290:364–377. doi:10.1016/j.jad.2021.04.050
16. Ren Z, Xin Y, Ge J, et al. Psychological impact of COVID-19 on college students after school reopening: a cross-sectional study based on machine learning. Front Psychol. 2021:12. doi:10.3389/fpsyg.2021.641806
17. Devaraj S, Patel PC. Change in psychological distress in response to changes in reduced mobility during the early 2020 COVID-19 pandemic: evidence of modest effects from the U.S. Soc Sci Med. 2021;270(113615):113615. doi:10.1016/j.socscimed.2020.113615
18. Xu F, Wang X, Yang Y, et al. Depression and insomnia in COVID-19 survivors: a cross-sectional survey from Chinese rehabilitation centers in Anhui province. Sleep Med. 2022;91:161–165. doi:10.1016/j.sleep.2021.02.002
19. Holder JM, Jolley D. Forced relocation between nursing homes: residents’ health outcomes and potential moderators. Rev Clin Gerontol. 2012;22(4):301–319. doi:10.1017/s0959259812000147
20. Rehman U, Yıldırım M, Shahnawaz MG. A longitudinal study of depression, anxiety, and stress among Indians during COVID-19 pandemic. Psychol Health Med. 2023;28(1):60–68. doi:10.1080/13548506.2021.2023751
21. Ambrosetti J, Macheret L, Folliet A. Psychiatric emergency admissions during and after COVID-19 lockdown: short-term impact and long-term implications on mental health. BMC Psychiatry. 2021;21(1). doi:10.1186/s12888-021-03469
22. Chen JH, Tong KK, Su X, Yu EWY, Wu AMS. Measuring COVID-19 related anxiety and obsession: validation of the Coronavirus Anxiety Scale and the obsession with COVID-19 Scale in a probability Chinese sample. J Affect Disord. 2021;295:1131–1137. doi:10.1016/j.jad.2021.08.104
23. Giesbrecht GF, Rojas L, Patel S, et al. Fear of COVID-19, mental health, and pregnancy outcomes in the pregnancy during the COVID-19 pandemic study: fear of COVID-19 and pregnancy outcomes. J Affect Disord. 2022;299:483–491. doi:10.1016/j.jad.2021.12.057
24. Şimşir Z, Koç H, Seki T, Griffiths MD. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. 2022;46(3):515–523. doi:10.1080/07481187.2021.1889097
25. LeDoux J, Daw ND. Surviving threats: neural circuit and computational implications of a new taxonomy of defensive behaviour. Nat Rev Neurosci. 2018;19(5):269–282. doi:10.1038/nrn.2018.22
26. Porcelli P. Fear, anxiety and health-related consequences after the covid-19 epidemic. Clin Neuropsychiatry. 2020;17(2):103–111. doi:10.36131/CN20200215
27. McLean CP, Anderson ER. Brave men and timid women? A review of the gender differences in fear and anxiety. Clin Psychol Rev. 2009;29(6):496–505. doi:10.1016/j.cpr.2009.05.003
28. Lee SA, Mathis AA, Jobe MC, Pappalardo EA. Clinically significant fear and anxiety of COVID-19: a psychometric examination of the Coronavirus Anxiety Scale. Psychiatry Res. 2020;290(113112):113112. doi:10.1016/j.psychres.2020.113112
29. Millroth P, Frey R. Fear and anxiety in the face of COVID-19: negative dispositions towards risk and uncertainty as vulnerability factors. J Anxiety Disord. 2021;83(102454):102454. doi:10.1016/j.janxdis.2021.102454
30. Costanza A, Macheret L, Folliet A, et al. COVID-19 related fears of patients admitted to a psychiatric Emergency Department during and post-lockdown in Switzerland: preliminary findings to look ahead for tailored preventive mental health strategies. Medicina. 2021;57(12):1360. doi:10.3390/medicina57121360
31. Nissen JB, Hojgaard D, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020;20(1). doi:10.1186/s12888-020-02905
32. Ornell F, Braga DT, Bavaresco DV, et al. Obsessive-compulsive disorder reinforcement during the COVID-19 pandemic. Trends Psychiatry Psychother. 2021;43(2):81–84. doi:10.47626/2237-6089-2020-0054
33. Alhujaili N, Alghamdi A, Abo Talib T, Alhaqbani M, Alfelali M, Alghamdi W. The impact of COVID-19 pandemic on obsession and compulsion symptoms in Saudi Arabia. Cureus. 2021;13(11):e20021. doi:10.7759/cureus.20021
34. Davide P, Andrea P, Martina O, Andrea E, Davide D, Mario A. The impact of the COVID-19 pandemic on patients with OCD: effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. 2020;291(113213):113213. doi:10.1016/j.psychres.2020.113213
35. Tanir Y, Karayagmurlu A, Kaya İ, et al. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. 2020;293(113363):113363. doi:10.1016/j.psychres.2020.113363
36. Ramiz L, Contrand B, Rojas Castro MY, et al. A longitudinal study of mental health before and during COVID-19 lockdown in the French population. Global Health. 2021;17(1):29. doi:10.1186/s12992-021-00682-8
37. Bandura A, Adams NE, Hardy AB, Howells GN. Tests of the generality of self-efficacy theory. Cognit Ther Res. 1980;4(1):39–66. doi:10.1007/bf01173354
38. Bandura A. Regulation of cognitive processes through perceived self-efficacy. Dev Psychol. 1989;25(5):729–735. doi:10.1037/0012-1649.25.5.729
39. Bandura A. On the functional properties of perceived self-efficacy revisited. J Manage. 2012;38(1):9–44. doi:10.1177/0149206311410606
40. Marle JL, Parmentier C, Vinchon F, Storme F, Borteyrou M, Lubart X. Evolution and impact of self-efficacy during French COVID-19 confinement: a longitudinal study. J Gen Psychol. 2021;148(3):360–381. doi:10.1080/00221309.2021.1904815
41. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2022;20(3):1537–1545. doi:10.1007/s11469-020-00270-8
42. Lee SA. Coronavirus Anxiety Scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44(7):393–401. doi:10.1080/07481187.2020.1748481
43. Lee SA. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain Behav Immun. 2020;51. doi:10.1016/j.bbi.2020.04.067
44. Schwarzer R, Mueller J, Greenglass E. Assessment of perceived general self-efficacy on the internet: data collection in cyberspace. Anxiety Stress Coping. 1999;12(2):145–161. doi:10.1080/10615809908248327
45. Caikang W. Evidences for reliability and validity of the Chinese Version of General SelfEfficacy Scale. Chin J Appl Psychol. 2001;7(1):37–40.
46. Hayes AF. PROCESS: a versatile computational tool for observed variable mediation, moderation, and conditional process modeling; 2012. Available from: http://www.afhayes.com/public/process2012.pdf.
47. Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivariate Behav Res. 2007;42(1):185–227. doi:10.1080/00273170701341316
48. Edwards JR, Lambert LS. Methods for integrating moderation and mediation: a general analytical framework using moderated path analysis. Psychol Methods. 2007;12(1):1–22. doi:10.1037/1082-989X.12.1.1
49. Malhotra NK, Kim SS, Patil A. Common method variance in IS research: a comparison of alternative approaches and a reanalysis of past research. Manage Sci. 2006;52(12):1865–1883. doi:10.1287/mnsc.1060.0597
50. Choi E, Lee J, Lee SA. Validation of the Korean version of the obsession with COVID-19 scale and the Coronavirus anxiety scale. Death Stud. 2022;46(3):608–614. doi:10.1080/07481187.2020.1833383
51. Evren C, Evren B, Dalbudak E, Topcu M, Kutlu N. Measuring anxiety related to COVID-19: a Turkish validation study of the Coronavirus Anxiety Scale. Death Stud. 2022;46(5):1052–1058. doi:10.1080/07481187.2020.1774969
52. Koch M, Park S. Do government responses impact the relationship between age, gender and psychological distress during the COVID-19 pandemic? A comparison across 27 European countries. Soc Sci Med. 2022;292(114583):114583. doi:10.1016/j.socscimed.2021.114583
53. Wathelet M, Duhem S, Vaiva G, et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3(10):e2025591. doi:10.1001/jamanetworkopen.2020.25591
54. Amerio A, Bertuccio P, Santi F, et al. Gender differences in COVID-19 lockdown impact on mental health of undergraduate students. Front Psychiatry. 2021;12:813130. doi:10.3389/fpsyt.2021.813130
55. Bayraktar S, Jiménez A. Self-efficacy as a resource: a moderated mediation model of transformational leadership, extent of change and reactions to change. J Organ Chang Manag. 2020;33(2):301–317. doi:10.1108/jocm-12-2018-0368
56. Schwarzer R, Boehmer S, Luszczynska A, Mohamed NE, Knoll N. Dispositional self-efficacy as a personal resource factor in coping after surgery. Pers Individ Dif. 2005;39(4):807–818. doi:10.1016/j.paid.2004.12.016
57. Bidzan M, Bidzan-Bluma I, Szulman-Wardal A, Stueck M, Bidzan M. Does self-efficacy and emotional control protect hospital staff from COVID-19 anxiety and PTSD symptoms? Psychological functioning of hospital staff after the announcement of COVID-19 Coronavirus pandemic. Front Psychol. 2020;11:552583. doi:10.3389/fpsyg.2020.552583
58. Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of Coronavirus disease 2019 (COVID-19) beyond paranoia and panic. Ann Acad Med Singapore. 2020;49(3):155–160. doi:10.1111/wvn.12439
59. Soh HL, Ho RC, Ho CS, Tam WW. Efficacy of digital cognitive behavioural therapy for insomnia: a meta-analysis of randomised controlled trials. Sleep Med. 2020;75:315–325. doi:10.1016/j.sleep.2020.08.020
60. Zhang MWB, Ho RCM. Moodle: the cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technol Health Care. 2017;25(1):163–165. doi:10.3233/THC-161261
61. Chen Y, Zhou X, Liu J, et al. Effect of internet-delivered cognitive behavioral therapy on insomnia in convalescent patients with COVID-19: protocol for a systematic review and meta-analysis. PLoS One. 2022;17(6):e0269882. doi:10.1371/journal.pone.0269882
62. Lau SSS, Ho CCY, Pang RCK, et al. Measurement of burnout during the prolonged pandemic in the Chinese zero-COVID context: COVID-19 burnout views scale. Front Public Health. 2022;10:1039450. doi:10.3389/fpubh.2022.1039450
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
