Back to Journals » Clinical Ophthalmology » Volume 15
The Relationship Between Dry Eye in Adults with Indications for Kidney Transplantation and Influence Factors
Authors Le Trung N , Quoc Toan P , Thang LV , Ngan ND , Chien Thang N, Van Cuong N, Van Dam N, Tuan Anh H, Thi Hang V, Kien Trung N, Nhu Binh D , Anh Tuan V
Received 25 August 2021
Accepted for publication 19 October 2021
Published 28 October 2021 Volume 2021:15 Pages 4327—4332
DOI https://doi.org/10.2147/OPTH.S335989
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nguyen Le Trung,1,2 Pham Quoc Toan,1,3 Le Viet Thang,1,3 Nguyen Dinh Ngan,1,2 Nguyen Chien Thang,1,2 Nguyen Van Cuong,1,2 Nguyen Van Dam,1,2 Hoang Tuan Anh,1,2 Vo Thi Hang,1,2 Nguyen Kien Trung,4 Do Nhu Binh,1,5 Vu Anh Tuan6
1Vietnam Military Medical University, Hanoi, 12108, Vietnam; 2Vietnam Department of Opthalmology, Military Hospital 103, Hanoi, 12108, Vietnam; 3Vietnam Department of Nephrology, Military Hospital 103, Hanoi, 12108, Vietnam; 4Vietnam National Eye Hospital, Hanoi, 11613, Vietnam; 5Vietnam Department of Infectious Diseases, Military Hospital 103, Hanoi, 12108, Vietnam; 6Vietnam Hanoi Medical University, Hanoi, 11601, Vietnam
Correspondence: Vu Anh Tuan Email [email protected]
Purpose: Patients with end-stage renal failure are susceptible to dry eye disease. This study explores the relationship between dry eye disease and influence factors.
Patients and Methods: The control group consisted of 57 healthy subjects who were kidney donors. They were of the same age and sex as the kidney transplant recipients. The outcome variable was the dry eye condition of the participants. The Schirmer test confirmed dry eye disease, TBUT (breakup time test), and the Eye Surface Disease Index (OSDI) questionnaire, using linear regression to evaluate the association.
Results: The total number of subjects was 146 (89 kidney recipients and 57 kidney donors). When univariate analysis found the level of visual acuity, the age group involved was statistically significant, while the other factors were not statistically significant. In multivariable logistic regression analysis, age (odds ratio: 2.8, p< 0.05), smoking history (odd ratio: 0.1, p< 0.05), corneal conjunctival calcification (odd ratio: 0.2, p< 0.05); central corneal thickness (odd ratio: 1.02, p< 0.05) is considered to be an influence factor for disease progression.
Conclusion: Age group, smoking history, corneal central thickness, and conjunctival calcification are factors for dry eye disease in patients preparing to receive a kidney. These results reinforce the evidence for multifactorial dry eye disease in patients with renal impairment.
Keywords: dry eye, renal failure, renal transplant, Hanoi Vietnam
Introduction
Dry eye is a common disorder characterized by ocular surface disease. They are characterized by tear film instability and associated ocular symptoms, including tear film instability and the tear film’s increased osmolarity. Neurosensory abnormalities play a role in tears, inflammation, and damage to the ocular surface.1 Dry eyes are familiar in all ages and social backgrounds, but those at high risk are the elderly, postmenopausal women, or people with autoimmune and chronic diseases.2,3 Classification of dry eyes includes three causes: dehydration, increased evaporation, combined dehydration, and increased evaporation. The classification tables have been shown that the cause of increased evaporation accounts for a more significant proportion than the lack of water, accounting for about 70%.3–5
Dry eye is one of the most frequently stated problems with the patient who often has end-stage chronic renal failure.6–8 Dry eye has existed as a health problem for many years. Therefore, dry eye disease is one of the reasons why patients with end-stage renal failure have to visit regular eye exams, causing considerable costs in terms of treatment costs and reducing the quality of life.
Although some research has been carried out in Vietnam on dry eye, no studies have found which dry eye in renal failure patients with indications for kidney transplantation and the correlated factors. This paper aims to explore “The relationship between dry eye in adults with indications for kidney transplantation and influence factors”.
Patients and Methods
Ethical approval was obtained according to Decision No. 467/GCN-HDDDNCSYHN-ĐHYHN dated 04/05/2021, Hanoi Medical University, Vietnam. All patients provided written informed consent, and that this study was conducted following the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The formula for calculating sample size uses the formula for determining the sample size of a proportion of the World Health Organization.9
The participants were divided into two groups based on the study group included 89 patients with end-stage renal failure with an indication for kidney transplantation; the control group consisted of 57 kidney donors who had undergone health screening and were eligible for surgery, they are the same age and sex as the recipients. We chose to analyze the results in the left eye.
Inclusion Criteria
Patients diagnosed with renal failure grade 3 to 4 indicated for kidney transplantation with glomerular filtration rate < 60 mL/min/173m2 according to the formula of KDIGO (Kidney Disease Improving Global Outcomes 2012).10 Chronic kidney disease includes chronic glomerulonephritis and other reasons such as hypertension, polycystic kidney, chronic pyelonephritis, lupus, gout, diabetes. Sex, the age at the time of the study was over 18, and the time of disease detection was different were studied.
Exclusion Criteria
Acute systemic comorbidities such as sepsis, respiratory failure, pneumonia, stroke. In the eyes, there are inflammatory diseases of the ocular surface, acute and chronic glaucoma, chronic uveitis, degenerative eye disease, keratoconjunctivitis, history of surgical eye, contact lens wear, diagnosis, and previous treatment.
Variables
The main study variable was dry eye disease in all subjects. The diagnostic criteria for dry eye are based on three methods, including the Schirmer test, TBUT (time break-up test), and OSDI (Ocular surface disease index) questionnaire.11 Systemic factors include age (years), sex (male or female), body nutritional status as calculated by BMI = weight /(height/100)2 in three levels of ≤ 18.5, 18.5–25, and ≥ 25.12 Age groups were divided into three age groups: ≤ 30 years old, 31–40 years old, and ≥ 41 years old. Previous smoking habits were noted as a predisposing factor. Blood samples were collected to determine serum calcium as measured by the enzymatic method on an Olympus AU 680 (Tokyo, Japan). Serum calcium as measured by the enzymatic method on an Olympus AU 680 (Tokyo, Japan).
Protocol
All participants responded to an OSDI (Ocular Surface Disease Index) questionnaire to assess dry eye disease functional symptoms. This questionnaire is reliable for assessing dry eye symptoms.11 Perform the Schirmer I test (without anesthetic) to quantify tear secretion with a 35 x 5mm filter paper strip, which is used to measure the number of tears produced over 5 minutes. After five minutes of the Schirmer I test, we conducted a test to measure the break-up time of the tear film TBUT (test break-up time). We use the sterile fluorescent dye Fluorescein. The participants look upward, and the fluorescein paper was gently touched to the lower eyelid conjunctiva and then removed. Participants blinked three times and then looked straight ahead without blinking. The tear film was observed under the cobalt blue filter light of a slit lamp biological microscope, and the time interval between the last blink and the appearance of the first dry spot in seconds was accepted as TBUT. The eye is diagnosed as dry when the Schirmer value is less than 10 mm, the TBUT is less than 10 seconds, or the total OSDI score is > 35 points.12
Best-corrected visual acuity using the Snellen electronic table at a distance of 5m, in logMAR units, divided into three levels: group reaching maximum visual acuity 0.0, group achieving visual acuity 0.1, and group 3 remaining visible acuity levels. Apply one drop of Alkain 0.1% (Alcon) to each eye, Goldmann tonometer Fluorescein stain, model BQ-900 (Haag-Streit; Haag Streit, Bern Switzerland) to obtain IOP readings from each eye. Evaluation of the anterior segment, including cornea, anterior chamber, iris, pupil, and vitreous by CSO microscope (Italy). Mydrin-P pupil dilation evaluates the posterior segment, including vitreous, optic disc, central retina.
Data Processing
Data entry was completed using EpiData software 3.1 (EpiData, Odense, Denmark). Statistical analysis and data cleaning with STATA 16.0 (Stata Corp, College Station, TX, USA). Quantitative data are presented as mean and standard deviation, and qualitative data are presented as absolute values and percentages. Test of normal distribution, compare the mean of two groups by t-student test, of many groups by ANOVA test. For non-normal distribution, test the mean of two independent groups using the Wilcoxon-Mann–Whitney test and the mean of more than two separate groups using the Kruskal–Wallis test. Compare two proportions of one group by Chi-square test, two independent groups by Fisher test with qualitative variables. Using logistic regression equation to evaluate the relationship between dry eye disease with several independent variables in the system and eyes.
Results
We compared the sign of dry eye status and factors that may affect the dry eye in patients with renal failure and healthy participants. The differences between the transplant group and donor group are highlighted in Table 1.
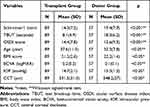 |
Table 1 Some Characteristics of the Disease Group and the Control Group |
We used the Schirmer1 test, TBUT tear film break time, and OSDI scores to assess the degree of dry eye in the kidney transplant group (Figure 1).
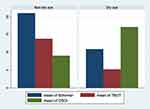 |
Figure 1 Distribution of mean values of dry eye tests in the kidney transplant group. |
As Figure 1 shows, there is a significant difference between the dry and non-dry groups (p<0.05, Wilcoxon signed-rank test) (Table 2).
 |
Table 2 Single-Variable Correlation Between Dry Eye Tests with Some Factors in the Kidney Transplant Group |
The correlational analysis results show a negative correlation between the Schirmer test and visual acuity grade, TBUT test with age group, and visual acuity group in Table 2. There was a positive correlation between OSDI score and age group and visual acuity group (p < 0.05) (Table 3).
 |
Table 3 Prevalence of Dry Eye with Some Factors in Renal Failure Group: Logistic Regression |
The data featured in this table is the regression coefficient between the incidence of dry eye disease with age group, previous smoking habits, conjunctival calcification, and corneal central thickness in patients with end-stage renal failure were statistically significant (p < 0.05).
Discussion
It is the first study conducted on renal failure patients with indications for kidney transplantation in Vietnam. The study results showed that the incidence of dry eye disease was significant with age, smoking history, and central corneal thickness. This study provides evidence on the prevalence of dry eye disease and, at the same time, indicates some related factors, thereby providing guidelines for the treatment of dry eye disease in these patients.
Prior studies have noted the importance of the relationship between dry eye disease and age.13–15 This phenomenon is due to the decline in the endocrine, leading to disorders of the accessory tear glands. In patients with end-stage renal failure, in addition to age, renal failure also increases the degree of damage to the tear glands.6 Urea concentration increases in tears, decreased tear secretion after dialysis causes an increase in tear osmolarity. This phenomenon stimulates epithelial cell inflammation, inflammatory cytokines, and background metalloproteinases (MMPs) cause damage to the ocular surface, loss of goblet cells, and loss of mucin cells, resulting in lacrimal instability.16 Prolonged kidney failure, along with aging, makes dry eyes worse.
A strong relationship between dry eye and secondhand smoke has been reported in the literature.17 Secondhand smoke irritates the surface of the ocular, which, when prolonged, continuously activates T cells. This process, in turn, triggers the call of other T cells, causing local inflammation. Cytokines are released in tears as subsequent inflammation irritates the ocular surface and blocks sensory signals from the ocular surface to the lacrimal gland, resulting in decreased tear secretion and the development of dry eye syndrome.18 Our study found that smoking habits, although at the time of examination, patients with renal failure were no longer using them, were still a risk factor for dry eye disease. This information is recommended for patients with renal failure of all stages.
The current study found that dry eyes can cause calcium deposition in the conjunctiva.16 In contrast, calcified deposit on the conjunctiva in patients with renal failure on dialysis results from the accumulation of toxic materials in the systemic and metabolic changes that disrupt the stability of tear film, disrupting the regular distribution of tears across the cornea. Calcium deposition induces inflammatory responses and increases tear permeability. In our study, the correlation between dry eye and corneal calcification was significant. This finding was also reported by Aktas’s study.12 This outcome was contrary to Ozdemir et al, who found no relationship between conjunctival calcification and dry eye.19 This difference is probably due to different criteria for evaluating dry eyes. The author used additional measures of Rose-Bengal staining to assess the degree of dry eyes and two standards, Schirmer and TBUT.
Szczotka-Flynn et al showed that vision loss is more pronounced in patients with dry eyes than decreased contrast sensitivity.20 This differs from the findings presented here in our study; the visual acuity level of patients with renal failure was not affected by dry eye. A possible explanation for this might be that the dry eye condition in our study group is still not enough to affect the visual acuity and the vision loss is due to other damage factors in the eye.
The results of Liu’s study showed a thinning of the cornea with dry eye.21 This sign occurs because chronic inflammation activates the immune system to damage corneal endothelial cells, especially in patients with renal failure on dialysis. This study confirms that dry eye is associated with central corneal thickness.
Our finding contradicts previous studies, which have suggested that serum calcium levels are significant in dry eye disease. When serum calcium levels decrease, dry eye disease worsens.22 In our study, calcium concentration did not correlate with the degree of the patient’s dry eye. The constant serum calcium levels could explain this in patients with renal failure undergoing hemodialysis, so serum calcium levels are unstable.
Our study’s limitation is that the case-control study’s design requires a review of several factors in the past, leading to repeat errors and some retroactive elements that cannot be performed in the control group. In addition, in our research, the Rose-Bengal test could not be performed to diagnose dry eye and could not be compared with other authors.
Conclusion
The main objective of the present study was to determine the association between dry eye disease and influence factors in renal failure patients preparing for kidney transplantation. Previous smoking habits, age, corneal central thickness, conjunctival calcification emerged as reliable predictors of dry eye in renal failure patients. The evidence from this study suggests that eye health care should be taken into account for patients before and after kidney transplantation.
Abbreviation
TBUT, test break-up time; OSDI, ocular surface disease index; BMI, body mass index; BCVA, best-corrected vision acuity; IOP, intraocular pressure; CCT, central corneal thickness.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. If you have concerns about sharing the data, please contact [email protected].
Ethical Statements
All participants were dispensed with written informed consents, and the protocol was approved by the Ethical Review Committee of the Hanoi Medical University, Vietnam (Decision no. 467/GCN-HDDDNCSYHN-DHYHN dated 05/04/2021). All patients provided written informed consent, and that this study was conducted following the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for Publication
I understand that the Clinical Opthalmology journal may be available in print and the internet and will be available to a broader audience through marketing channels and other third parties. Therefore, anyone can read material published in the journal. I understand that readers may include medical professionals, scholarly researchers and journalists, and general public members. If you have any queries, please contact [email protected].
Acknowledgments
We thank all the Department of Opthalmology and Department of Nephrology staff, and the Director board of Military Hospital 103 for supporting this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bron AJ, de Paiva CS, Chauhan SK, et al. Tfos dews ii pathophysiology report. Ocul Surf. 2017;15(3):438–510.
2. Sullivan DA, Rocha EM, Aragona P, et al. TFOS DEWS II sex, gender, and hormones report. Ocul Surf. 2017;15(3):284–333.
3. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.008
4. Grenon SM, Jans JM, Hutchinson JW, et al. System for Inner Eyelid Treatment of Meibomian Gland Dysfunction. Google Patents; 2016.
5. Perry HD, Donnenfeld ED. Dry eye diagnosis and management in 2004. Curr Opin Ophthalmol. 2004;15(4):299–304. doi:10.1097/00055735-200408000-00004
6. Diaz-Couchoud P, Bordas FD, Garcia JRF, et al. Corneal disease in patients with chronic renal insufficiency undergoing hemodialysis. Cornea. 2001;20(7):695–702. doi:10.1097/00003226-200110000-00005
7. Hsiao C-H, Chao A, Chu S-Y, et al. Association of severity of conjunctival and corneal calcification with all-cause 1-year mortality in maintenance haemodialysis patients. Nephrol Dial Transplant. 2011;26(3):1016–1023. doi:10.1093/ndt/gfq485
8. Tokuyama T, Ikeda T, Sato K, et al. Conjunctival and corneal calcification and bone metabolism in hemodialysis patients. Am J Kidney Dis. 2002;39(2):291–296. doi:10.1053/ajkd.2002.30548
9. Lwanga SK, Lemeshow S; World Health Organization. Sample Size Determination in Health Studies: A Practical Manual/S. K. Lwanga and S. Lemeshow. Geneva: World Health Organization; 1991.
10. Levey AS, Eckardt K-U, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005;67(6):2089–2100. doi:10.1111/j.1523-1755.2005.00365.x
11. Verma SR, Singh A. Diagnosis of Dry Eye. IntechOpen; 2021.
12. Aktaş S, Sağdık HM, Aktaş H, et al. Tear function in patients with chronic renal failure undergoing hemodialysis. Ren Fail. 2015;37(2):245–248. doi:10.3109/0886022X.2014.982487
13. de Paiva CS. Effects of aging in dry eye. Int Ophthalmol Clin. 2017;57(2):47–64. doi:10.1097/IIO.0000000000000170
14. Sharma A, Hindman HB. Aging: a predisposition to dry eyes. J Ophthalmol. 2014;2014:781683. doi:10.1155/2014/781683
15. Ding J, Sullivan DA. Aging and dry eye disease. Exp Gerontol. 2012;47(7):483–490. doi:10.1016/j.exger.2012.03.020
16. Charlton JF, Schwab IR, Stuchell R. Tear hyperosmolarity in renal dialysis patients asymptomatic for dry eye. Cornea. 1996;15(4):335–339. doi:10.1097/00003226-199607000-00001
17. Grzybowski A. Tobacco smoking influences on eye diseases and vision. Br J Ophthalmol. 2009;93(4):559–560. doi:10.1136/bjo.2008.151902
18. Xu L, Zhang W, Zhu XY, et al. Smoking and the risk of dry eye: a meta-analysis. Int J Ophthalmol. 2016;9(10):1480–1486.
19. Ozdemir M, Bakaris S, Özdemir G, et al. Ocular surface disorders and tear function changes in patients with chronic renal failure. Can J Ophthalmol. 2004;39(5):526–532. doi:10.1016/S0008-4182(04)80143-1
20. Szczotka-Flynn LB, Maguire MG, Ying G-S, et al. Impact of dry eye on visual acuity and contrast sensitivity: Dry Eye Assessment and Management Study. Optom Vis Sci. 2019;96(6):387–396. doi:10.1097/OPX.0000000000001387
21. Liu Z, Pflugfelder SC. Corneal thickness is reduced in dry eye. Cornea. 1999;18(4):403–407. doi:10.1097/00003226-199907000-00002
22. Patil M. Dry eye and its relationship with status of serum calcium in the body at a tertiary care institute: a Case Control Study. Patil M, Balwir D, Khune A, Dhewale S. Dry eye and its relationship with status of serum calcium in the body at a tertiary care institute: a Case Control Study. MVP J Med Sci. 2018;5(1):82–86.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
