Back to Journals » Patient Preference and Adherence » Volume 15
The Relationship Between COVID-19 Related Stress and Medication Adherence Among High-Risk Adults During the Acceleration Phase of the US Outbreak
Authors Zhao C, Batio S, Lovett R, Pack AP , Wolf MS, Bailey SC
Received 16 March 2021
Accepted for publication 24 April 2021
Published 31 August 2021 Volume 2021:15 Pages 1895—1902
DOI https://doi.org/10.2147/PPA.S310613
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Caroline Zhao, Stephanie Batio, Rebecca Lovett, Allison P Pack, Michael S Wolf, Stacy C Bailey
Division of General Internal Medicine & Geriatrics, Feinberg School of Medicine at Northwestern University, Chicago, IL, USA
Correspondence: Stacy C Bailey
Division of General Internal Medicine & Geriatrics, Feinberg School of Medicine, Northwestern University, 750 N. Lake Shore Drive, 10th Floor, Chicago, IL, 60611, USA
Tel +1 312-503-5595
Fax +1 312-503-2777
Email [email protected]
Purpose: To assess the relationship between stress regarding COVID-19 and medication adherence.
Patients and Methods: Older adults with ≥ 1 chronic condition(s) were recruited from 4 active, federally funded studies in Chicago to participate in a longitudinal telephone survey. Participants self-reported stress regarding COVID-19 in the last week. Adherence was measured via the ASK-12 survey.
Results: Most participants reported feeling stressed “some of the time” (54.0%), while 18.2% felt stressed “most” or “all of the time” and 27.8% “never” felt stressed. In bivariate analyses, participants who reported being stressed “most” or “all of the time” had worse medication adherence than participants who reported being stressed “some of the time” or “never” (p < 0.001). In multivariable analyses, participants who reported feeling stressed “most” or “all of the time” had worse adherence than those who “never” felt stressed (Adjusted Least Square Mean (Standard Error): 21.3 (0.6) vs 19.7 (0.6), p=0.01).
Conclusion: Stress due to COVID-19 has significantly impacted medication adherence, which has negative implications for the course of both COVID-19 and comorbid conditions. Healthcare providers should be aware of the potential impact of COVID-19 on patients’ mental and physical well-being and consider ways to routinely assess patient experiences.
Keywords: COVID-19, stress, medication adherence, comorbidity
Introduction
Coronavirus-19 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in December 2019 and has rapidly evolved into a worldwide pandemic.1 The United States alone has amassed over 28 million cases and more than 500,000 deaths to date—a scope of infection not seen in nearly a century.2,3 The population most at risk for severe disease or death from COVID-19 is older adults with underlying comorbidities such as hypertension, diabetes, or kidney disease.4,5 Early evidence and clinical guidelines suggest that effective chronic disease self-management in this population is key to reducing COVID-19 related morbidity and mortality.
Medication adherence is often a cornerstone of chronic disease self-management. In the midst of COVID-19, supporting safe and consistent medication use among patients with chronic conditions has therefore become paramount. Yet, COVID-19 has disrupted adults’ daily lives, introducing barriers to medication access and use and inducing stress and anxiety.6 Studies conducted prior to the pandemic have shown that stress and other strong emotional responses—such as anger, anxiety, or depression—have a negative influence on adherence to prescribed medications; those who are more stressed have a higher likelihood of being non-adherent to their medication regimens than those who have lower or no stress.7,8 However, little is known about patients’ experiences with stress due to the COVID-19 outbreak and how this may impact medication use.
We took advantage of a unique opportunity to examine this relationship among a cohort of high-risk patients enrolled in the Chicago COVID-19 Comorbidities (C3) Survey. The purpose of this analysis is to explore the relationship between feelings of stress and nervousness regarding COVID-19 and adherence to prescribed medications among a cohort of adults living with chronic disease.
Methods
Parent Study Participants and Data Collection Procedures
The Chicago COVID-19 Comorbidities (C3) Survey is an on-going, telephone-based cohort study among predominantly older adults with at least one chronic condition in Chicago, IL.9 To date, it has consisted of five waves of surveys conducted at different stages of the pandemic. Primary objectives of the C3 Survey are to longitudinally assess pandemic-related knowledge, beliefs and behaviors among a diverse higher risk population.
The participants in the C3 Survey were active enrollees in four ongoing, federally funded studies; details of these clinical trials and cohort studies have previously been described.10−13 Participants were recruited to these parent studies after obtaining care from one of five academic practices or two community health centers in Chicago, IL.
Specific eligibility criteria differed between the participants’ parent studies; however, study populations generally consisted of middle-aged or older patients with at least one chronic condition. One trial included adults who were Spanish-speakers, while the rest only enrolled English-speaking patients.12 In order to participate in the C3 survey, participants had to have completed an interview for one of the parent studies between 2018 and 2020. They also had to have previously consented to being approached for future research studies. All participants who completed a Wave 1 interview were eligible to participate in subsequent waves.
The process of data collection was standardized across the existing five waves of the C3 Survey. Participants were called by research staff and invited to participate in a 30-minute survey related to COVID-19. All participant responses were recorded by trained research staff using REDCap software.14 Participants were given a $15 gift certificate for participation. The Northwestern University Institutional Review Board (IRB) approved all study procedures in accordance with the Declaration of Helsinki.
Sub-Study Participants and Data Collection
For this sub-study, we utilized data from Wave 3 of the C3 Survey. Wave 3 was conducted May 1–May 20, 2020 and included a total of 565 adult participants out of the 630 who were eligible. Of those who did not participate, 47 could not be reached for the follow-up interview and 18 declined to participate, for an overall cooperation rate of 89.7%. Our aim was to examine levels of patient stress and nervousness from COVID-19 and its relationship to self-reported barriers to appropriate medication use in May 2020, a period of time during which COVID-19 cases in Chicago reached over 47,000 and deaths exceeded 2200.9
Measures
As part of the NIH-funded parent studies, participants completed a number of standardized assessments measuring personal and health-related characteristics. This included sociodemographic information (eg, age, sex, race/ethnicity, educational attainment, income) and health status (chronic conditions, overall self-reported health). Health literacy was assessed via The Newest Vital Sign (NVS), a commonly used, validated measure that asks participants to interpret information found on a nutrition label.15 Summed scores of 0–1 reflect a high likelihood of limited literacy, while scores of 2–3 reflect a possibility of limited literacy; scores of 4–6 nearly always represent adequate literacy. Patient activation, or the degree to which an individual is actively engaged in their personal health, was measured with the Consumer Health Activation Index (CHAI).16 The CHAI is a validated measure that can be utilized among diverse individuals, including those who have low health literacy; furthermore, it can be administered across varying research and healthcare settings.
During Wave 3, stress and nervousness due to COVID-19 was measured by asking participants to self-report how often they felt stressed or nervous due to COVID-19 during the past week. Response options included: all of the time, most of the time, some of the time, or never. Unlike other measures of stress, this measure was specific to COVID-19. To measure medication adherence, the Adherence Starts with Knowledge (ASK-12) questionnaire was utilized. ASK-12 is a shortened, validated version of the 20-item ASK-20. For the ASK-12, participants rate their level of agreement (strongly agree, agree, neutral, disagree, strongly disagree) with twelve statements pertaining to medication adherence. Domains include adherence behavior, health beliefs, and inconvenience/forgetfulness. Scores range from 12 to 60, with higher scores signifying greater barriers to adherence.17
Analyses
Descriptive statistics, such as means and percentage frequencies, were calculated for the overall sample. Associations between stress and patient characteristics were assessed using χ2 tests. Bivariate analyses were used to determine differences between adherence, patient-level characteristics, and stress levels using t-tests or analysis of covariance, as appropriate. A multivariate general linear regression model was used to further examine the association of ASK-12 adherence and stress. The final model included stress levels as a primary covariate, as well as other socio-demographics variables (gender, race, age, poverty, insurance type), health-related outcomes (number of chronic diseases, self-reported health status), and parent study. We also included patient health activation and health literacy as control variables, as previous studies have demonstrated associations between these factors and medication adherence.18 We reported least-square means (LSM) and standard errors of covariates. Statistical analyses were performed using SAS, version 9.4.
Results
Table 1 displays the study sample characteristics. Participants were racially diverse; most were female (61.4%) and the average age of respondents was 62.3 years old. Almost half of the sample (46.6%) had a “high likelihood of limited literacy” or “possibility of limited literacy” according to the NVS (hereafter referred to as “low” or “marginal” health literacy, respectively), and 59.3% had three or more chronic conditions.
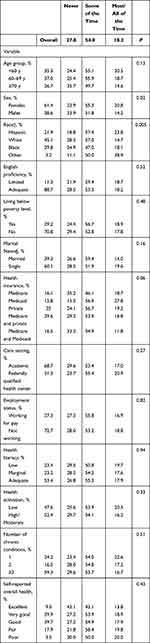 |
Table 1 Patient Characteristics and Reported Stress and Nervousness Due to COVID-19 (n = 565) |
When asked if they had felt stressed or nervous because of COVID in the last week, 27.8% of participants answered “never.” More than half (54.0%) reported feeling stressed “some of the time” and 18.2% said they felt stressed “most” or “all of the time” (Table 1). Women were significantly more likely to be stressed than men (p=0.02), with 20.8% of women reporting that they felt stressed “most” or “all of the time” compared to 14.2% of men (Table 1). Additionally, participants differed in their level of stress by race; participants identifying as Hispanic, Black, or Other reported feeling stressed “most” or “all of the time” more than participants identifying as White (p=0.005) (Table 1). The mean ASK-12 medication adherence score for our sample was 20.2 (standard deviation (SD) 5.2). Participants who were female, non-white, living below the poverty line, and those with limited English proficiency, multiple chronic conditions, poor overall health, and low patient health activation were more likely to have worse medication adherence (Table 2).
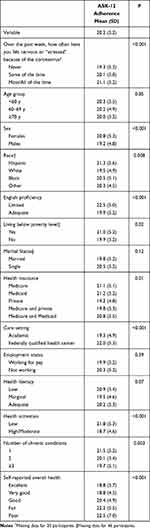 |
Table 2 ASK-12 Adherence Across Patient Characteristics (n = 565) |
In bivariate analyses, participants who reported being stressed “most” or “all of the time” were more likely to report more barriers to medication adherence than those who were “never” stressed or who were stressed only “some of the time” (ASK-12 score (SD): 19.3 (5.3) vs 20.1 (5.0), respectively, p < 0.001; Table 2). There was also a significant relationship between stress and adherence in multivariable analyses, adjusting for relevant covariates (p=0.04; Table 3). In particular, participants who reported feeling stressed “most” or “all of the time” had significantly poorer adherence than those who reported “never” feeling stressed (Adjusted LSM (SE): 21.3 (0.6) vs 19.7 (0.6), p=0.01). In adjusted analyses, participants with marginal health literacy, those who were older and those with private insurance were also independently less likely to report barriers to adherence, while those with low health activation and who reported poor health had worse adherence (Table 3).
 |
Table 3 Multivariate Models Examining Patient Characteristics, Stress Levels and Adherence (n = 546) * |
Discussion
Within our sample of primarily older adults with one or more comorbid medical conditions surveyed during the acceleration stage of the COVID-19 crisis in the US, rates of self-reported stress were high. Nearly three-quarters of participants endorsed experiencing at least some degree of stress due to the pandemic, with almost 20% reporting feeling stressed “most” or “all of the time.” In particular, women reported feeling more stressed than men, as did participants who identified as non-white compared to those who identified as white. These disparities by gender and race are consistent with other population-based surveys examining COVID-related stress.19,20 This is likely due to the disproportionate burden these groups have faced in regard to the economic and caregiving consequences of the pandemic.
Our results also suggest that increased stress and nervousness due to COVID-19 may have a negative impact on patient adherence to prescribed medications, although it should be noted that the magnitude of these differences was relatively small, making the clinical significance of this finding unclear. Specifically, when participants reported feeling stressed “most” or “all of the time” they tended to have more barriers to adherence than participants who reported feeling stressed “some of the time” or “never.” Furthermore, while participants who reported feeling stressed “some of the time” did have better adherence than participants who reported feeling stressed “most” or “all of the time,” they still had worse adherence than participants reporting “never” feeling stressed with regard to COVID-19. This indicates a possible gradient effect of related stress on adherence, with increasing levels of stress due to the virus leading to more barriers.
Medication adherence is a complex behavior influenced by multi-level factors.21 Before the COVID-19 pandemic, medication adherence was often noted as being negatively impacted by factors such as polypharmacy, interference with the patient’s daily schedule, poor physician-patient communication, access to care, or costs.22,23 However, researchers had also previously assessed the negative relationship between perceived stress and medication adherence across chronic disease contexts.6,24–28 Our results contribute to this broader literature by investigating how an intense stressor, such as COVID-19, further exacerbates poor medication adherence.
The Multidimensional Coping Inventory (MCI) offers insight into the potential mechanisms through which stress affects medication adherence. According to the MCI, there are three primary types of strategies for coping with stress: task-oriented coping, emotion-oriented and avoidance-oriented coping.29 Emotion-oriented coping was found to be one of the most significant predictors of poor medication adherence in a study conducted among older adults living with chronic disease; the more that participants focused on their emotions during stressful situations, the less likely they were to be adherent to their medications.26 Similarly, the stress and coping model of medication adherence and viral load24 suggests that negative mood (conceptualized as anger, depression and anxiety) leads to avoidant coping strategies that, in turn, result in poor medication adherence. With deaths in the United States topping 500,000, the COVID-19 pandemic is both stressful and emotional.6 While we did not assess coping specifically, other research has suggested that lockdown policies have diminished the supportive systems and positive coping strategies on which many older adults living with chronic conditions rely.30
Results from this analysis raise concerns about the less visible impact that COVID-19 has had, and may continue to have, on the management of other non-communicable diseases that require ongoing adherence to prescribed medications. Based on our analysis, this impact may disproportionately affect older patients, as well as those with low health literacy or those without private insurance. This is in line with data from previous studies examining medication adherence prior to the pandemic, which have shown lower medication adherence in patients who are older, those who have lower education levels, as well as those who grapple with high treatment costs.23,31
As COVID-19 cases in the United States continue, stress may persist, or perhaps increase, and continue to affect patient adherence to medication. As a result, other pre-existing conditions may worsen, which subsequently can possibly increase risk for COVID-19 morbidity and mortality.32,33 In light of this, physicians should be made aware of these new barriers their patients may be facing in taking their medications. Many patients may not share their feelings of stress with their provider, or feel open to discussing suboptimal medication use due to feelings of shame, embarrassment, or social desirability.34 Thus, it is vital for physicians to ask their patients at each visit about stressors they may be experiencing and the degree to which those stressors may be affecting their ability to take their medications as prescribed. Furthermore, it is important for providers to remain non-judgmental and be understanding of any obstacles that arise regarding their patient’s medication use during the pandemic.
This study has limitations. Participants were generally older, had at least one chronic condition, and all participants resided in the greater Chicago metropolitan area. Because of this, the study’s conclusions may not be generalizable to other populations. Furthermore, because of the self-report nature of this survey, social desirability bias may have affected how participants reported their adherence to medication, possibly resulting in overestimation of adherence. The relatively high rates of adherence reported by our sample, all of whom had at least one chronic medical condition, support this possibility. There was also no baseline measure of adherence measured before COVID-19 to which current ASK-12 scores can be compared. Finally, a single item was used to measure for stress and nervousness due to COVID-19; however brief, validated measures of stress specific to the pandemic were not widely available at the time this study was conducted.
Conclusion
Our assessment of the C3 Survey data pertaining to stress and medication adherence revealed that participants who have experienced more stress due to COVID-19 report more adherence barriers to their prescribed medications. These results raise concerns regarding the progression of non-communicable diseases, which have been shown to increase risk for COVID-19 morbidity and mortality, especially when uncontrolled, during this unprecedented time. Physicians should continue to emphasize the importance of medication adherence to their patients, but also make sure to work with them to understand their barriers and stressors so as to help them better engage in appropriate mental and physical self-care.
Acknowledgments
We are grateful for the support of this work by grants: R01AG030611, R01AG046352, R01DK110172, and R01NR01544 of the National Institutes of Health (NIH). Research reported in this publication was also supported, in part, by the National Institutes of Health’s National Institute on Aging, Grant Number P30AG059988. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure
Dr. Bailey reports grants from the NIH, Merck, Pfizer, Gordon and Betty Moore Foundation, Lundbeck and Eli Lilly and personal fees from the Sanofi, Pfizer, University of Westminster and Luto outside the submitted work. Dr. Pack reports grants from the NIH, Pfizer, Gordon and Betty Moore Foundation, Lundbeck and Eli Lilly. Dr. Wolf reports grants from the NIH, Amgen, Lundbeck, Merck, Pfizer, Gordon and Betty Moore Foundation, and Eli Lilly during the conduct of the study and personal fees from Sanofi, Pfizer, University of Westminster and Luto outside the submitted work. Miss Zhao reports grants from NIH during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. World Health Organization. Pneumonia of Unknown Cause-China; 2020.
2. Cipriano PF. 100 years on: the Spanish Flu, pandemics and keeping nurses safe. Int Nurs Rev. 2018;65(3):305–306. doi:10.1111/inr.12483
3. Worldometer. COVID-19 Coronavirus Outbreak; 2021.
4. Kretchy IA, Asiedu-Danso M, Kretchy JP. Medication management and adherence during the COVID-19 pandemic: perspectives and experiences from low-and middle-income countries. Res Social Adm Pharm. 2021;17(1):2023–2026. doi:10.1016/j.sapharm.2020.04.007
5. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi:10.1016/j.ijid.2020.03.017
6. Ballivian J, Alcaide ML, Cecchini D, Jones DL, Abbamonte JM, Cassetti I. Impact of COVID-19-related stress and lockdown on mental health among people living with HIV in Argentina. J Acquir Immune Def Syndr. 2020;85(4):475–482. doi:10.1097/QAI.0000000000002493
7. Kretchy IA, Owusu-Daaku FT, Danquah SA. Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int J Ment Health Syst. 2014;8:25. doi:10.1186/1752-4458-8-25
8. Miyazaki M, Nakashima A, Nakamura Y, et al. Association between medication adherence and illness perceptions in atrial fibrillation patients treated with direct oral anticoagulants: an observational cross-sectional pilot study. PLoS One. 2018;13(9):e0204814. doi:10.1371/journal.pone.0204814
9. Chicago Department of Public Health. 2021.COVID Dashboard. [online] Available from: https://www.chicago.gov/city/en/sites/covid-19/home/covid-dashboard.html. Accessed August 5 2021.
10. Wolf MS, Serper M, Opsasnick L, et al. Awareness, attitudes, and actions related to COVID-19 among adults with chronic conditions at the onset of the U.S. outbreak: a cross-sectional survey. Ann Intern Med. 2020;173(2):100–109. doi:10.7326/M20-1239
11. Bailey SC, Wismer GA, Parker RM, et al. Development and rationale for a multifactorial, randomized controlled trial to test strategies to promote adherence to complex drug regimens among older adults. Contemp Clin Trials. 2017;62:21–26. doi:10.1016/j.cct.2017.08.013
12. O’Conor R, Arvanitis M, Wismer G, et al. Rationale and design of the regimen education and messaging in diabetes (REMinD) trial. Contemp Clin Trials. 2019;83:46–52. doi:10.1016/j.cct.2019.06.016
13. Wolf MS, Curtis LM, Wilson EA, et al. Literacy, cognitive function, and health: results of the LitCog study. J Gen Intern Med. 2012;27(10):1300–1307. doi:10.1007/s11606-012-2079-4
14. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010
15. Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522. doi:10.1370/afm.405
16. Wolf MS, Smith SG, Pandit AU, et al. Development and validation of the consumer health activation index. Med Decis Making. 2018;38(3):334–343. doi:10.1177/0272989X17753392
17. Matza LS, Park J, Coyne KS, Skinner EP, Malley KG, Wolever RQ. Derivation and validation of the ASK-12 adherence barrier survey. Ann Pharmacother. 2009;43(10):1621–1630. doi:10.1345/aph.1M174
18. Smith SG, Curtis LM, Wardle J, von Wagner C, Wolf MS. Skill set or mind set? Associations between health literacy, patient activation and health. PLoS One. 2013;8(9):e74373. doi:10.1371/journal.pone.0074373
19. McKnight-Eily LR, Okoro CA, Strine TW, et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic - United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2021;70(5):162–166. doi:10.15585/mmwr.mm7005a3
20. Wang Y, Kala MP, Jafar TH. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS One. 2020;15(12):e0244630. doi:10.1371/journal.pone.0244630
21. Salmoirago-Blotcher E, Carey MP. Can Mindfulness training improve medication adherence? Integrative review of the current evidence and proposed conceptual model. Explore (NY). 2018;14(1):59–65. doi:10.1016/j.explore.2017.09.010
22. Poulter NR, Borghi C, Parati G, et al. Medication adherence in hypertension. J Hypertens. 2020;38(4):579–587. doi:10.1097/HJH.0000000000002294
23. Yeam CT, Chia S, Tan HCC, Kwan YH, Fong W, Seng JJB. A systematic review of factors affecting medication adherence among patients with osteoporosis. Osteoporos Int. 2018;29(12):2623–2637. doi:10.1007/s00198-018-4759-3
24. Weaver KE, Llabre MM, Durán RE, et al. A stress and coping model of medication adherence and viral load in HIV-positive men and women on highly active antiretroviral therapy (HAART). Health Psychol. 2005;24(4):385–392. doi:10.1037/0278-6133.24.4.385
25. Kalichman SC, Kalichman MO. HIV-related stress and life chaos mediate the association between poverty and medication adherence among people living with HIV/AIDS. J Clin Psychol Med Settings. 2016;23(4):420–430. doi:10.1007/s10880-016-9481-8
26. Gruszczyńska M, Wyszomirska J, Daniel-Sielańczyk A, Bąk-Sosnowska M. Selected psychological predictors of medication adherence in the older adults with chronic diseases. Nurs Open. 2021;8(1):317–326. doi:10.1002/nop2.632
27. Fan Y, Shen BJ, Tay HY. Depression, anxiety, perceived stress, and their changes predicted medical adherence over 9 months among patients with coronary heart disease. Br J Health Psychol. Epub 2020 Dec 31.
28. Baucom KJ, Queen TL, Wiebe DJ, et al. Depressive symptoms, daily stress, and adherence in late adolescents with type 1 diabetes. Health Psychol. 2015;34(5):522–530. doi:10.1037/hea0000219
29. Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990;58(5):844–854. doi:10.1037/0022-3514.58.5.844
30. O’Conor R, Opsasnick L, Pack AP, et al. Perceived adequacy of tangible support during stay-at-home orders in Chicago and New York. Prim Care Commun Health. 2021;12:21501327.
31. Uchmanowicz B, Chudiak A, Uchmanowicz I, Rosińczuk J, Froelicher ES. Factors influencing adherence to treatment in older adults with hypertension. Clin Interv Aging. 2018;13:2425–2441. doi:10.2147/CIA.S182881
32. Palmer K, Monaco A, Kivipelto M, et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res. 2020;32(7):1189–1194. doi:10.1007/s40520-020-01601-4
33. Yap AF, Thirumoorthy T, Kwan YH. Systematic review of the barriers affecting medication adherence in older adults. Geriatr Gerontol Int. 2016;16(10):1093–1101. doi:10.1111/ggi.12616
34. Brown MT, Bussell J, Dutta S, Davis K, Strong S, Mathew S. Medication adherence: truth and consequences. Am J Med Sci. 2016;351(4):387–399. doi:10.1016/j.amjms.2016.01.010
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
