Back to Journals » Psychology Research and Behavior Management » Volume 15
The Psychological Impact of Quarantine During the COVID-19 Pandemic on Quarantined Non-Healthcare Workers, Quarantined Healthcare Workers, and Medical Staff at the Quarantine Facility in Saudi Arabia
Authors Alfaifi A , Darraj A , El-Setouhy M
Received 21 February 2022
Accepted for publication 11 May 2022
Published 17 May 2022 Volume 2022:15 Pages 1259—1270
DOI https://doi.org/10.2147/PRBM.S362712
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Igor Elman
Abdulrahman Alfaifi,1 Abdulaziz Darraj,1 Maged El-Setouhy2,3
1Jazan Health Affairs, Ministry of Health, Jazan, Saudi Arabia; 2Department of Family and Community Medicine, Faculty of Medicine, Jazan University, Jazan, Saudi Arabia; 3Department of Community, Environmental and Occupational Medicine, Faculty of Medicine, Ain Shams University, Cairo, Egypt
Correspondence: Abdulrahman Alfaifi, Jazan Health Affairs, Ministry of Health, PO 96, Jazan, 45142, Saudi Arabia, Tel +966 56 887 3773, Email [email protected]
Background: COVID-19 is a viral infectious disease that spreads quickly through droplets. It is highly contagious and could overwhelm the health system. Because of that, many governments established health quarantines for suspected infected people to minimize the spread of this disease.
Objective: This study aimed to assess the prevalence of depression, anxiety, and stress symptoms and to address the associated risk factors among quarantined non-healthcare workers, quarantined healthcare workers, and medical staff in the Ministry of Health quarantine facility.
Patients and Methods: We conducted an analytical cross-sectional study at the health quarantine in Jazan, Saudi Arabia. The total number of participants was 301 individuals. Furthermore, the study questionnaire was composed of three sections, the first two were the background and clinical characteristics, and the last one was DASS 21 scale. Also, we used SPSS software to analyze the data. Lastly, we implemented logistic regression to assess the predictors of depression, anxiety, and stress symptoms.
Results: The prevalence of depression, anxiety, and stress symptoms among quarantined non-healthcare workers were 51.9%, 60.2%, and 40.6%, respectively. These prevalences were 25.0%, 29.8%, and 16.9% among quarantined healthcare workers and 20.5%, 20.5%, and 27.3% among the medical staff. The predictors of depression, anxiety, and stress symptoms among the study participants were female gender, perceived COVID-19 stigma, presence of other relatives in quarantine, comorbidities, and abnormal sleep duration.
Conclusion and Recommendations: Health quarantine is an environment that could negatively affect people’s mental health. The quarantined non-healthcare workers were the most affected study participants inside this environment. Therefore, the availability of mental health services there could minimize their depression, anxiety, and stress symptoms. Moreover, a home quarantine would be better to reduce these negative symptoms whenever possible.
Keywords: depression, anxiety, stress, prevalence, risk factors
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is a traumatic event.1 People who experienced such an event are liable for post-traumatic stress disorders and harmful psychiatric illness.2–8 One systematic review and meta-analysis found an increase in mental health problems such as depression, anxiety, distress, and insomnia during the COVID-19 pandemic, and the prevalence of these symptoms was 31.4%, 31.9%, 41.1%, and 37.9%, respectively. Moreover, it revealed that the most affected populations during the pandemic were the quarantined persons, healthcare workers, patients with noninfectious chronic disease, and COVID-19 patients.9 Another longitudinal study among the UK population found a deterioration in mental health during the COVID-19 pandemic as compared to pre-pandemic. This deterioration was seen more in some sociodemographic groups than others. For example, female gender, younger age, Asian people, urban population, those living in a low-income house or living with no partners showed lower mental health than others.10 Moreover, one US study reported more than threefold increase in the prevalence of depression during the COVID-19 pandemic than before, and those with lower income and who lost their job had a greater burden of depression symptoms.8 Meanwhile, a Saudi Arabian study stated similar finding of having more depression and anxiety symptoms during the COVID-19 pandemic than before, and the rate of depression during COVID-19 in 2020 increased by 71.2% as compared to 2018, from 12.5% to 21.4%.11
Many studies to investigate the prevalence of mental health problems before the COVID-19 pandemic in Saudi Arabia were found. Of them, one study was done among Jazan University students and found that the prevalence of insomnia among university students was 19.3%.12 Another study among dermatology patients found that the prevalence of depression, anxiety, and stress symptoms were 12.6%, 22.1%, and 7.5%, respectively.13 Furthermore, a study among type 2 diabetic patients found that the prevalence of depression, anxiety, and stress symptoms was 33.8%, 38.3%, and 25.5%, respectively.14 Variability of results in different sittings were found, keeping in mind that no single study was found to measure the prevalence of these negative symptoms among the general population before the COVID-19 pandemic.
It is worth mentioning that Saudi Arabia’s population is 34,218,169 residents, 38.3% of them were immigrants, majority of the population is under the age of 65 years.15 As of 28 September 2020, the total number of COVID-19 cases in Saudi Arabia reached 336,004 cases.16 By that time, 11,752 were in the Jazan region.17 In Saudi Arabia, few studies to measure the depression, anxiety, and stress symptoms during the COVID-19 pandemic among the general population were found. One of them showed that the prevalence of moderate-to-severe depression, anxiety, and stress symptoms was 28.3%, 24%, and 22.3%, respectively.5 Another showed that 28.9% of the respondents were depressed, 16.4% anxious and 17.8% stressed.18 Both studies reported that the female gender and those working in the medical field were more liable to these negative symptoms. Interestingly, a study done in Jazan city found that 26% of the participants were depressed and the presence of chronic diseases and female gender were risk factors for this negative symptom.19
On the other hand, the quarantine environments that were used to separate people who were exposed to coronavirus disease to prevent further spread could affect their residents adversely. One review study by Brooks et al found that quarantine has a wide-ranging, substantial, and long-lasting psychological impact on the population.20
The kingdom of Saudi Arabia has implemented 10 strategies to control the pandemic. Implementation of quarantine and travel restrictions was one of them. The rest were expansion of screening, mask-wearing and social distancing, hospitals preparation to deal with the influx of COVID-19 cases, public assurance, artificial intelligence use, economic stimulus, removal of slum areas with rehousing of their inhabitants, and cancellation of hajj season.15 Many studies in different geographical areas showed a negative psychological impact of these environments.20–26 One study to investigate the negative mental health of quarantine during the COVID-19 pandemic in China found a significant difference between quarantined and non-quarantined populations. Post-traumatic stress disorders, sleep problems, and fear were seen more in the quarantined group than in the non-quarantined.27 Moreover, one case–control study showed a higher depression, anxiety, and insomnia symptoms in the quarantined individuals than in the general population; younger age, lower income, and non-married had a higher risk of mental health problems.28 Interestingly, the higher prevalence was seen in Saudi Arabia as well; three studies found that the prevalence of the depression, anxiety, and stress symptoms inside the quarantine facility were (32.7–63.6)%, (21.5–40.5)%, and (25.7–55.5)%, respectively.24–26 Among those studies, one stated that 42.1% of quarantined individuals had insomnia.24 All of these studies showed that the female gender was more affected by the negative psychological symptoms than the male.
Therefore, both COVID-19 disease and the quarantine environment have a negative psychological impact on the population. To our knowledge, no study was found in Saudi Arabia to compare the prevalence of depression, anxiety, and stress symptoms among the quarantined and non-quarantined individuals inside the quarantine facility. Our hypothesis assumed that COVID-19ʹs quarantine facility in Jazan city, Saudi Arabia has a negative psychological impact such as depression, anxiety, stress, and sleep problems on its population, and this negative impact varies between the quarantined individuals and the medical staff serving there. So, we aimed to investigate the psychological impact of the quarantine environment on the quarantined healthcare and non-healthcare workers as well as on the medical staff serving there. By studying these different populations in such an environment, we would be able to identify the associated risk factors of these negative symptoms inside the quarantine facility. And this will help us to understand and mitigate any similar situation in the future.
Materials and Methods
Design, Setting, and Participants
We created an analytical cross-sectional study between June and September 2020 at the Saudi Ministry of Health (MOH) COVID-19 main quarantine facility in Jazan city, the capital of Jazan region, southwest of Saudi Arabia. This quarantine was a 5-star hotel, which is composed of 150 rooms. It started in late May 2020 and ended in September 2020. Quarantine reasons ranged from traveler coming to Saudi Arabia to suspected/confirmed cases with mild disease. The quarantined individual stayed in a single room for 14 days.25 The medical staff was working inside this quarantine facility, and they were responsible for delivering the health need of the quarantined individuals. They were communicating with patients through telephones that were available in each room. Upon need, the medical staff has direct contact with the quarantined individuals after wearing proper personal protective equipment and taking full precautions. By the end of September 2020, many individuals were quarantined at home.
We included those aged 18 years and above as well as the medical staff working in this quarantine facility. We excluded those who could not speak English or Arabic and those under psychiatric treatment before being in the quarantine.
Sampling Procedure
The total number of quarantined individuals during the study period was 463; 374 were eligible for the study and 89 were not (62 children, 25 not Arabic or English speakers, and 2 quarantined female healthcare workers with psychiatric illness). Among the eligible individuals, 220 were quarantined non-healthcare workers and 154 were quarantined healthcare workers. We invited all those who were eligible to participate. However, only 257 individuals agreed to participate (133 quarantined non-healthcare workers and 124 quarantined healthcare workers). The medical staff working in the quarantine facility were 52; 44 of them agreed to participate (12 physicians, 12 nurses, 12 epidemiologists, 3 public health specialists, 2 health informatics, 1 public health registrar, 1 laboratory technician, 1 administrator) (Figure 1).
 |
Figure 1 Recruitment of study participants. |
Data Collection
We used an online Google Forms survey that was distributed to the study participants through a social network platform (WhatsApp) using the registered contact numbers at the health quarantine. This survey was built in Arabic and English to allow the participants to use their preferred languages. The questionnaire contained 3 sections. The first was to collect the sociodemographic data, including (sex, age, education, marital status, nationality, education level, occupation, monthly income, and the presence of other relatives in the quarantine). The second section collected related clinical variables, including (perceived COVID-19 stigma, comorbidities, sleep duration, and daily time spent following the COVID-19 news). We used the recommended sleep duration for adults (7 to 9 hours per day). The third section was the Depression, Anxiety, and Stress Scale-21 (DASS-21), a validated and standardized tool used to evaluate depression, anxiety, and stress symptoms.29 This scale contains 21 questions evaluating the depression, anxiety, and stress symptoms, with seven questions for each symptom. It rates the degree of each symptom on a 4-point severity scale (0–3), where (0) stands for not applicable at all to me, (1) for applied to me for some degree or some time, (2) for applied to me for a considerable degree or enough time, and (3) for applied to me for most of the time or applied very much.30 For calculating the score of each emotional state, we summed the scores of the relevant items and then multiplied them by 2 to get the final scores. After that, we compared the scores to the recommended DASS-21 cut-off scores for severity (normal, mild, moderate, severe, and extremely severe). Furthermore, binary classification of depression, anxiety, and stress symptoms was implemented to get binary yes/no outcomes to calculate logistic regression. In this study, those with mild, moderate, severe, or extremely severe DASS-21 scores were considered to have depression, anxiety, or stress symptoms.
Data Analysis
We used the Statistical Package for Social Sciences (SPSS) version 25 for Windows (IBM Corporation, Armonk, NY, USA) for data analysis. The data analysis included both descriptive and inferential statistics. DASS-21 scores were the dependent variables, while various sociodemographic and clinical variables were independent. The Kruskal–Wallis test was used to find the difference in depression, anxiety, and stress symptoms between quarantined non-healthcare workers, quarantined healthcare workers, and medical staff. P-value <0.05 was considered statistically significant. Moreover, we performed a multivariate logistic regression analysis to estimate the effect of explanatory variables on the level of depression, anxiety, and stress.
Ethical Consideration
The Jazan Research Ethics Committee approved this study (approval number No. 2001), which complied with the Declaration of Helsinki. All eligible individuals reviewed and accepted the informed consent of the study. All data were kept anonymous, and confidentiality was maintained.
Results
A total of 301 individuals participated in this study. The response rates of the quarantined non-healthcare workers, quarantined healthcare workers, and medical staff were 60.45%, 80.52%, and 84.62%, respectively. Table 1 shows the demographic and clinical-related data for study participants. Around 58% of them were males. The median age was 31 years (interquartile range, 19–43). Around a quarter of quarantined non-healthcare workers suffered from chronic diseases, which was higher than other study groups.
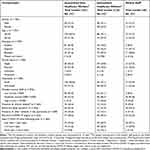 |
Table 1 Demographic and Clinical Characteristics of Study Participants During the COVID-19 Pandemic |
On the other hand, sleep disturbance was detected among 46.47% of study participants. Interestingly, one-third of quarantined non-healthcare workers reported the presence of other relatives in the quarantine. Nearly half of the study participants experienced perceived COVID-19 stigma. Moreover, 20% of the quarantined individuals and medical staff follow daily corona news for 1 to 3 hours, and around 10% follow them for more than 3 hours daily.
Figure 2 illustrates the prevalence of depression, anxiety, and stress symptoms among study groups.
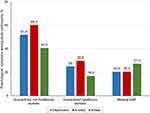 |
Figure 2 Percentage of depression, anxiety, and stress symptoms among study participants. |
Furthermore, the Kruskal–Wallis test showed that the quarantined non-healthcare workers experience higher depression and anxiety symptoms than the quarantined healthcare workers and medical staff. Regarding the stress symptoms, it was statistically significant that quarantined non-healthcare workers were higher than quarantined healthcare workers but not higher than the medical staff (Table 2).
 |
Table 2 The Difference in DASS-21 Scores of Depression, Anxiety, and Stress Symptoms Among Study Participants |
Among quarantined non-healthcare workers, the perceived COVID-19 stigma was a predictor of depression symptoms. Among the quarantined healthcare workers, the predictors of depression were the presence of other relatives in the quarantine. On the other hand, the predictors of anxiety among quarantined non-healthcare workers were the female gender and the perceived COVID-19 stigma, while among quarantined healthcare workers, they were the presence of other relatives in the quarantine and having chronic diseases. On the other hand, the predictors of stress among quarantined non-healthcare workers were female gender, perceived COVID-19 stigma, and abnormal sleep duration. And no predictor of stress among quarantined healthcare workers was found. The medical staff group had no single predictors for depression, anxiety, or stress symptoms (Table 3).
 |
Table 3 Multiple Logistic Regressiona of Depression, Anxiety, and Stress Symptoms Among Study Participants |
Discussion
The current study was conducted in Jazan city, Saudi Arabia, during the COVID-19 pandemic between June and September 2020. This research aimed to investigate the depression, anxiety, and stress symptoms among the quarantined individuals and the medical staff in the quarantine facility.
To our knowledge, this is the only study that compared the prevalence of depression, anxiety, and stress symptoms among different quarantine populations during the COVID-19 pandemic in Saudi Arabia using the Depression, Anxiety and Stress Scale – 21 (DASS-21). Although we have tried to involve all quarantined individuals and the medical staff working at the quarantine facility, a low response rate was seen. The other national and US studies reported a lower response rate as well.8,26,31 These could be attributed to the use of an online survey during the COVID-19 pandemic as a tool for collecting the data from study participants.32
In this work, we found that the prevalences of depression, anxiety, and stress symptoms among quarantined non-healthcare workers were 51.9%, 60.2%, and 40.6%, respectively. Interestingly, these prevalences were higher than quarantined healthcare workers and medical staff as well. One study found that the quarantined individuals had a higher prevalence of these symptoms than the medical staff.2 Moreover, we found that quarantined non-healthcare workers suffered more from severe and extremely severe depression, anxiety, and stress symptoms compared to other study groups. This higher prevalence could be due to being younger than other study groups.33 One study found that the psychological distress of the population was more among the younger, and peaked around the middle age.34 Also, the lower symptoms among the quarantined healthcare workers and medical staff could be attributed to the fact that healthcare workers are more prepared and knowledgeable about COVID-19 than non-healthcare workers,2 especially after the previous experience of coronavirus epidemics like SARS and MERS, keeping in mind that MERS struck Saudi Arabia in 2012.35,36
In the current study, the most reported symptoms among quarantined individuals were anxiety, with 45% (60% among quarantined non-healthcare workers and 30% among quarantined healthcare workers). However, this percentage was slightly more than another Saudi study in which it was 40.5%.26 This increase is not that much and could be attributed to the usage of different measurement scales. Although the current study showed a higher prevalence of negative psychological symptoms among the quarantined individuals than the general population results, a different pattern was seen where the anxiety symptoms were reported more.18 Other Saudi studies reported more depression than anxiety.5,18,25 Also, a similar pattern was seen in other international studies.4,37 However, one Canadian study reported an almost exact prevalence of anxiety and depression symptoms at 46.7% and 41.4%, respectively.38 Moreover, one study in Wuhan reported anxiety symptoms in 70.78% of the study sample, and it was like our quarantined non-healthcare workers’ result.3 This higher prevalence in the quarantined non-healthcare worker’s group might be attributed to being younger than other study groups, and the younger population is known to be affected by psychological problems more.2,33,34
One systematic review was done during the COVID-19 pandemic to assess the prevalence of depression, anxiety, and insomnia among healthcare workers showed results similar to those of our study.7 The similarity between the quarantined healthcare workers’ results and the general population results could be attributed to the fact that the healthcare workers’ negative symptoms were lower because they were more prepared and knowledgeable about the COVID-19 pandemic.2,35
During the COVID-19 pandemic, many studies around the world reported a higher prevalence of psychological problems among quarantined individuals.2–4,8,20,25–28,38–44 This was consistent with the result of the current study. On the other hand, 2 Saudi studies implemented among the general population during the COVID-19 pandemic showed a lower prevalence of psychological symptoms than our results.5,18 This was consistent with the literature, many studies showed a lower prevalence of psychological problems among the general population than the quarantined population.2,27,28 These findings could be because of the quarantine environment itself. It was shown to affect the restricted people there negatively, and this effect may last years after the quarantine ended.20,43,44 Moreover, it was noticeable that the stress symptoms were more prominent among the medical staff group; many studies found similar findings. It could be due to the increase in everyday work during the COVID-19 pandemic.45–48 Also, the isolation itself is a major risk factor. It significantly increases occupational stress in healthcare workers, as demonstrated in a longitudinal study.49
Interestingly, the prevalence of depression in our study was higher than that in the German, Chinese, and Indian populations with 31.1%, 26.47%, and 14.1%, respectively, keeping in mind that those people were quarantined at home.3,40,41 This higher prevalence of depression in our study could be due to the type of quarantine itself. One study in Jordan stated a high prevalence of depression in hospital quarantine, and their result was close to ours.39 In one review, Brook et al concluded that involuntary quarantine has more long-term complications and negative effects than the voluntary and less restricted one.20 Another review found that being in the centralized quarantine may lead to stigma from the community.50 On the other hand, a study among those quarantined at home found that a high percentage of participants were psychologically stable This was linked to the closeness of family members to each other, the more attention of people to their health, and being interested in self-development.51 Also, home quarantine was found to reduce the stress on the health system compared to the institutional qurantine.52
This study showed that half of the study participants had perceived COVID-19 stigma, and the quarantined non-healthcare workers who had it were almost 2 to 3 times more prone to depression, anxiety, and stress symptoms than those who had not. A similar finding was found in the quarantined community in the USA.53 Many studies showed that stigma harms mental health.54,55 Current study and many previous ones found that healthcare workers feel stigma secondary to COVID-19 infection as well.56,57 One more review reported stigmatization as one of the stressors of COVID-19.20 These results were constant with our study findings. Interestingly, we did not see an association between COVID-19 stigma and depression, anxiety, and stress symptoms among the quarantined healthcare workers and medical staff in our work. This could be due to the small sample size of the medical staff group. Therefore, merging of the quarantined healthcare workers and medical staff groups was done and a significant association between COVID-19 stigma and the stress symptoms was detected. One article found that healthcare workers involved in COVID-19 management are prone to psychological disorders and post-traumatic stress disorder because of the stressful work condition and perceived COVID-19 stigma.58
The quarantined healthcare workers who reported the presence of other relatives in the quarantine were almost 6 and 8 times more depressed and anxious respectively than those who did not. Moreover, after merging the quarantined healthcare workers and the medical staff groups 4 times more stress was seen. These increases might be due to the fear and blame among healthcare workers that they might be responsible for transmitting the infection to their relatives as compared to the quarantined non-healthcare workers.59
Interestingly, we found that female non-healthcare workers were more anxious and stressed than males. Many other studies showed similar findings.26,37,42 On the other hand, the quarantined female healthcare workers were not significantly depressed, anxious, or stressed. This could be because healthcare workers were more prepared for the COVID-19 pandemic.35
The odds of having anxiety among quarantined healthcare workers suffering from comorbidities was 5 times more than those who was not. An association between comorbidities and anxiety was seen in another study.18,60 The non-healthcare workers did not show similar findings. This higher odds might be because healthcare workers are more aware of their comorbidities than non-healthcare workers.61
Finally, the quarantined non-healthcare workers with abnormal sleep were almost 3 times more stressed than those who were not. One article reported close interaction between stress and sleep disorders.62 The other study groups did not report an association. These negative issues among quarantined non-healthcare workers could be due to their less knowledge about the COVID-19 pandemic than the others.35
Limitation
The response rate was not high because we had to use an online survey.
Conclusion and Recommendations
The quarantined individuals during the COVID-19 pandemic were affected by depression, anxiety, and stress symptoms more than the general population. Those quarantined non-healthcare workers were the most affected study group. Therefore, the availability of mental health services, such as screening, counseling, and treatment at the health quarantine facility could lower these negative symptoms. Moreover, it would be better to use home quarantine whenever possible.
Acknowledgments
The authors would like to thank all the staff who worked at the health quarantine for their patience and support during the study period.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhou Y-G, Shang Z-L, Zhang F, et al. PTSD: past, present and future implications for China. Chin J Traumatol. 2021;24(4):187–208. doi:10.1016/j.cjtee.2021.04.011
2. Li X, Yu H, Yang W, et al. Depression and anxiety among quarantined people, community workers, medical staff, and general population in the early stage of COVID-19 epidemic. Front Psychol. 2021;12:897.
3. Tang F, Liang J, Zhang H, Kelifa MM, He Q, Wang P. COVID-19 related depression and anxiety among quarantined respondents. Psychol Health. 2021;36(2):164–178. doi:10.1080/08870446.2020.1782410
4. Khan AH, Sultana MS, Hossain S, Hasan MT, Ahmed HU, Sikder MT. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. J Affect Disord. 2020;277:121–128. doi:10.1016/j.jad.2020.07.135
5. Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. 2020;102:152192. doi:10.1016/j.comppsych.2020.152192
6. Al sulais E, Mosli M, AlAmeel T. The psychological impact of COVID-19 pandemic on physicians in Saudi Arabia: a cross-sectional study. Saudi J Gastroenterol. 2020;26(5):249–255. doi:10.4103/sjg.SJG_174_20
7. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi:10.1016/j.bbi.2020.05.026
8. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686–e2019686. doi:10.1001/jamanetworkopen.2020.19686
9. Wu T, Jia X, Shi H, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;281:91–98. doi:10.1016/j.jad.2020.11.117
10. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi:10.1016/S2215-0366(20)30308-4
11. BinDhim NF, Althumiri NA, Basyouni MH, et al. Saudi Arabia Mental Health Surveillance System (MHSS): mental health trends amid COVID-19 and comparison with pre-COVID-19 trends. Eur J Psychotraumatol. 2021;12(1):1875642. doi:10.1080/20008198.2021.1875642
12. Albasheer OB, Al Bahhawi T, Ryani M, et al. Prevalence of insomnia and relationship with depression, anxiety and stress among Jazan University students: a cross-sectional study. Cogent Psychol. 2020;7(1):1789424. doi:10.1080/23311908.2020.1789424
13. Ahmed AE, Al-Dahmash AM, Al-Boqami QT, Al-Tebainawi YF. Depression, anxiety and stress among Saudi Arabian dermatology patients: cross-sectional study. Sultan Qaboos Univ Med J. 2016;16(2):e217. doi:10.18295/squmj.2016.16.02.013
14. Alzahrani A, Alghamdi A, Alqarni T, Alshareef R, Alzahrani A. Prevalence and predictors of depression, anxiety, and stress symptoms among patients with type II diabetes attending primary healthcare centers in the western region of Saudi Arabia: a cross-sectional study. Int J Ment Health Syst. 2019;13(1):1–7. doi:10.1186/s13033-019-0307-6
15. AlFattani A, AlMeharish A, Nasim M, AlQahtani K, AlMudraa S. Ten public health strategies to control the Covid-19 pandemic: the Saudi experience. IJID Regions. 2021;1:12–19. doi:10.1016/j.ijregi.2021.09.003
16. WHO. Coronavirus disease (COVID-19) dashboard. Available from: https://covid19.who.int/.
17. Sahli S, Nafisah SB. The prevalence of COVID-19 in Jizan Region-Saudi Arabia: a demographic analysis. J Med Law Public Health. 2021;1(2):15–18. doi:10.52609/jmlph.v1i2.4
18. Alamri HS, Algarni A, Shehata SF, et al. Prevalence of depression, anxiety, and stress among the general population in Saudi Arabia during Covid-19 pandemic. Int J Environ Res Public Health. 2020;17(24):9183. doi:10.3390/ijerph17249183
19. Alharbi A. The prevalence of depression and related factors during the COVID-19 pandemic among the general population of the Jazan Region of Saudi Arabia. Cureus. 2022;14(2):e21965. doi:10.7759/cureus.21965
20. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/S0140-6736(20)30460-8
21. Rothstein MA, Alcalde MG, Elster NR, et al.; Center for Disease Control. Quarantine and Isolation: Lessons Learned from SARS. University of Louisville School of Medicine, Institute for Bioethics, Health Policy and Law; 2003.
22. Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi:10.1016/S0140-6736(20)30567-5
23. WHO. Coronavirus disease 2019 (COVID-19). Situation report–91; 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200420-sitrep-91-covid-19.pdf?sfvrsn=fcf0670b_4.
24. Alodhayani AA, Almutairi KM, Alshobaili FA, et al. Predictors of mental health status among quarantined COVID-19 patients in Saudi Arabia.
25. Alkhamees AA, Aljohani MS, Alghesen MA, Alhabib AT. Psychological distress in quarantine designated facility during COVID-19 pandemic in Saudi Arabia. Risk Manag Healthc Policy. 2020;13:3103–3120. doi:10.2147/RMHP.S284102
26. El Keshky MES, Alsabban AM, Basyouni SS. The psychological and social impacts on personal stress for residents quarantined for COVID-19 in Saudi Arabia. Arch Psychiatr Nurs. 2021;35(3):311–316. doi:10.1016/j.apnu.2020.09.008
27. Wu L, Guo X, Shang Z, et al. China experience from COVID-19: mental health in mandatory quarantine zones urgently requires intervention. Psychol Trauma. 2020;12:S3–S5. doi:10.1037/tra0000609
28. Wang C, Song W, Hu X, et al. Depressive, anxiety, and insomnia symptoms between population in quarantine and general population during the COVID-19 pandemic: a case-controlled study. BMC Psychiatry. 2021;21(1):1–9. doi:10.1186/s12888-021-03108-2
29. Ali AM, Green J. Factor structure of the depression anxiety stress Scale-21 (DASS-21): unidimensionality of the Arabic version among Egyptian drug users. Subst Abuse Treat Prev Policy. 2019;14(1):1–8. doi:10.1186/s13011-019-0226-1
30. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343. doi:10.1016/0005-7967(94)00075-U
31. Evanoff BA, Strickland JR, Dale AM, et al. Correction: work-related and personal factors associated with mental well-being during the COVID-19 response: survey of health care and other workers. J Med Internet Res. 2021;23(4):e29069. doi:10.2196/29069
32. Ebert JF, Huibers L, Christensen B, Christensen MB. Or web-based questionnaire invitations as a method for data collection: cross-sectional comparative study of differences in response rate, completeness of data, and financial cost. J Med Internet Res. 2018;20(1):e24. doi:10.2196/jmir.8353
33. NIH. Mental illness. Available from: https://www.nimh.nih.gov/health/statistics/mental-illness.
34. Taylor MR, Agho KE, Stevens GJ, Raphael B. Factors influencing psychological distress during a disease epidemic: data from Australia’s first outbreak of equine influenza. BMC Public Health. 2008;8:347. doi:10.1186/1471-2458-8-347
35. Tan BY, Chew NW, Lee GK, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317–320. doi:10.7326/M20-1083
36. Temsah M-H, Al-Sohime F, Alamro N, et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health. 2020;13(6):877–882. doi:10.1016/j.jiph.2020.05.021
37. Shah SMA, Mohammad D, Qureshi MFH, Abbas MZ, Aleem S. Prevalence, psychological responses and associated correlates of depression, anxiety and stress in a global population, during the coronavirus disease (COVID-19) pandemic. Community Ment Health J. 2021;57(1):101–110. doi:10.1007/s10597-020-00728-y
38. Nkire N, Mrklas K, Hrabok M, et al. COVID-19 pandemic: demographic predictors of self-isolation or self-quarantine and impact of isolation and quarantine on perceived stress, anxiety, and depression. Front Psychiatry. 2021;12. doi:10.3389/fpsyt.2021.553468
39. Samrah SM, Al-Mistarehi A-H, Aleshawi AJ, et al. Depression and coping among covid-19-infected individuals after 10 days of mandatory in-hospital quarantine, Irbid, Jordan. Psychol Res Behav Manag. 2020;13:823. doi:10.2147/PRBM.S267459
40. Benke C, Autenrieth LK, Asselmann E, Pané-Farré CA. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020;293:113462. doi:10.1016/j.psychres.2020.113462
41. Singh SP, Khokhar A. Prevalence of posttraumatic stress disorder and depression in general population in India during COVID-19 pandemic home quarantine. Asia Pac J Public Health. 2021;33(1):154–156. doi:10.1177/1010539520968455
42. Pandey D, Bansal S, Goyal S, et al. Psychological impact of mass quarantine on population during pandemics—the COVID-19 Lock-Down (COLD) study. PLoS One. 2020;15(10):e0240501. doi:10.1371/journal.pone.0240501
43. Jurblum M, Ng CH, Castle DJ. Psychological consequences of social isolation and quarantine: issues related to COVID-19 restrictions. Austral J Gen Pract. 2020;49(12):778–783. doi:10.31128/AJGP-06-20-5481
44. Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol Health. 2020;42. doi:10.4178/epih.e2020038
45. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976–e203976. doi:10.1001/jamanetworkopen.2020.3976
46. Ma Y, Rosenheck R, He H. Psychological stress among health care professionals during the 2019 novel coronavirus disease outbreak: cases from online consulting customers. Intensive Crit Care Nurs. 2020;61:102905. doi:10.1016/j.iccn.2020.102905
47. Magnavita N, Soave PM, Antonelli M. Prolonged stress causes depression in frontline workers facing the COVID-19 pandemic—a repeated cross-sectional study in a COVID-19 Hub-hospital in central Italy. Int J Environ Res Public Health. 2021;18(14):7316. doi:10.3390/ijerph18147316
48. Magnavita N, Soave PM, Ricciardi W, Antonelli M. Occupational stress and mental health among anesthetists during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(21):8245. doi:10.3390/ijerph17218245
49. Magnavita N, Soave PM, Antonelli M. A one-year prospective study of work-related mental health in the intensivists of a COVID-19 hub hospital. Int J Environ Res Public Health. 2021;18(18):9888. doi:10.3390/ijerph18189888
50. Nada Q, Saryono S, Anggraeni MD. The impact of centralized quarantine on mental health of people affected by Covid-19: a systematic review. Jurnal Ilmu Kesehatan. 2021;6(1):45–52.
51. Jawa TM. Logistic regression analysis for studying the impact of home quarantine on psychological health during COVID-19 in Saudi Arabia. Alexandria Eng J. 2022;61(10):7995–8005. doi:10.1016/j.aej.2022.01.047
52. Ebrahim SH, Ahmed QA, Gozzer E, Schlagenhauf P, Memish ZA. Covid-19 and Community Mitigation Strategies in a Pandemic. Vol. 368. British Medical Journal Publishing Group; 2020.
53. Weinberger-Litman SL, Litman L, Rosen Z, Rosmarin DH, Rosenzweig C. A look at the first quarantined community in the USA: response of religious communal organizations and implications for public health during the COVID-19 pandemic. J Relig Health. 2020;59(5):2269–2282. doi:10.1007/s10943-020-01064-x
54. Lipai T. The COVID-19 pandemic: depression, anxiety, stigma and impact on mental health. Проблемы социальной гигиены, здравоохранения и истории медицины. 2020;28(5):922–927.
55. Aruta JJ, Antazo BG, Paceño JL. Self-stigma is associated with depression and anxiety in a collectivistic context: the adaptive cultural function of self-criticism. J Psychol. 2021;155(2):238–256. doi:10.1080/00223980.2021.1876620
56. Ramaci T, Barattucci M, Ledda C, Rapisarda V. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability. 2020;12(9):3834. doi:10.3390/su12093834
57. Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. 2020;20(7):782. doi:10.1016/S1473-3099(20)30498-9
58. Sachdeva A, Nandini H, Kumar V, Chawla RK, Chopra K. From stress to stigma–Mental health considerations of health care workers involved in COVID19 management. Indian J Tubercul. 2021. doi:10.1016/j.ijtb.2021.09.007
59. Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi:10.1016/S2215-0366(20)30046-8
60. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi:10.3390/ijerph17051729
61. Simione L, Gnagnarella C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front Psychol. 2020;2020:2166.
62. Han KS, Kim L, Shim I. Stress and sleep disorder. Exp Neurobiol. 2012;21(4):141. doi:10.5607/en.2012.21.4.141
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
