Back to Journals » Clinical Ophthalmology » Volume 16
The Prevalence of Work-Related Musculoskeletal Disease Among Pediatric Ophthalmologists
Authors Fouzdar Jain S, Akhter S, Ishihara R, Siddicky S , High R, Suh DW
Received 12 October 2021
Accepted for publication 15 February 2022
Published 18 March 2022 Volume 2022:16 Pages 833—840
DOI https://doi.org/10.2147/OPTH.S343155
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Samiksha Fouzdar Jain,1,2 Sidra Akhter,3 Rhys Ishihara,3 Safeer Siddicky,4 Robin High,2 Donny W Suh3,4
1Department of Pediatric Ophthalmology & Adult Strabismus, Children’s Hospital, and Medical Center, Omaha, NE, USA; 2College of Medicine, University of Nebraska Medical Center, Omaha, NE, USA; 3Creighton University School of Medicine, Omaha, NE, USA; 4Department of Orthopaedic Surgery, University of Arkansas for Medical Sciences, Little Rock, AR, USA
Correspondence: Samiksha Fouzdar Jain, Ophthalmology Department, Children’s Hospital and Medical Center, 8400 Dodge Street, Omaha, NE, 68114, USA, Tel +1 402 955 8280, Email [email protected]
Introduction: Work-related musculoskeletal disease (MSD) is the second leading cause of disability globally. Ophthalmologists widely report MSDs in the neck (70%) and back pain (40– 80%). Our study intended to identify the prevalence of MSDs among pediatric ophthalmologists.
Methods: Pediatric ophthalmologists self-reported chronic pain, instrumentation used, years practiced, surgeries performed, work schedule/environment modifications due to MSD, and treatment for MSD via an anonymous online survey. Statistical analysis of responses included odds ratios, Pearson chi-square testing, and Spearman correlations.
Results: This study had 101 respondents, with 66% reporting chronic pain. Chronic neck pain (41%) and lower back pain (31%) followed by shoulder pain (30%) were the leading MSD complaints and significantly correlated with years of experience (p< 0.05). Participants often had multiple types of pain, including 13% of the sample who experienced all three types of pain. Those reporting shoulder and back pain also reported a greater incidence in work modification (68– 83%). Those suffering from chronic neck, shoulder, and lower back pain have sought treatment for their MSD (p< 0.05).
Discussion: With such wide reporting of chronic neck, back, and shoulder pain, the development of MSDs likely leads to disability. Ergonomic innovations in the workplace may reduce the healthcare burden and prolong pediatric ophthalmologists’ ability to provide services.
Conclusion: In our study, the reported prevalence of chronic neck and back pain was comparable to previous studies and published literature, with 2/3 of participants reporting pain. There is a tremendous need for ongoing innovations, especially surgical loupes, operating microscopes, and slit-lamp modifications to prevent musculoskeletal disease.
Keywords: musculoskeletal disease, ergonomics, neck pain, back pain
Introduction
Work-related musculoskeletal disorders (MSDs) are the leading cause of occupational absence and the second cause of disability globally.1,2 Among the MSDs; chronic lower back pain is the leading cause of disability.3 Worldwide, thirty-seven percent of lower back pain is attributed to occupation.4,5 While reporting the incidence of MSDs varies among population classifications, such as age group and work, as many as 33% of the global population currently live with a painful MSD. MSDs are also associated with a high economic cost, accounting for over 20 billion dollars of worker’s compensation in the United States.1
Over the last decade, many surveys concerning work-related MSDs in ophthalmologic professionals were conducted. These studies report an incidence of 30–70% for neck pain and 40–80% for back pain.6–9 Across multiple surveys, up to 8% of respondents require surgery, and as high as 9% are unable to operate due to chronic pain.4 These studies were conducted before 2015 and mainly looked at ophthalmologists primarily in the United Kingdom, and fewer studies were performed in the United States. No investigation was done, mainly looking at musculoskeletal disease among pediatric ophthalmologists. For ophthalmologists, a commonly cited source of neck and back pain is magnification loupes during surgery.4
Ergonomics is an applied science concerned with designing and arranging things people use to interact efficiently and safely (Merriam Webster). This study aimed to identify the prevalence of MSDs among pediatric ophthalmologists and find areas where significant ergonomic improvement can be made.
Methods
Study Design
A 15-question anonymous survey was sent to all members of Pediatric Ophthalmology Listservs. The study was conducted over one month, from June 2019 to July 2019. The pediatric ophthalmology Listservs comprised of approximately 1000 pediatric ophthalmologists worldwide at different stages in their career with varying years in clinical practice ranging from 1 year to more than 25 years in practice. The group comprised male and female pediatric ophthalmologists in university and private practice settings. We sent out a reminder email two weeks after the initial survey to increase the response rate.
Questionnaire
The Pediatric ophthalmologists on the listserv self-reported chronic pain, instrumentation used, years practiced, surgeries performed, work schedule/environment modifications due to MSD, and treatment for MSD. The list of survey questions is shown in Box 1.
 |
Box 1 Questionnaire |
Statistical Analysis
Statistical analysis of collected responses included odds ratios, Pearson Chi-Square exact tests (due to the small counts of some factor combinations), Spearman correlations, and a negative binomial count data model. Statistical analyses were generated with PROC FREQ and PROC LOGISTIC from SAS/STAT software, Version 9.4 (© 2002–2012) of the SAS System for Windows (Cary, NC). The Institutional review board approved this study from the University of Nebraska Medical Center. The study was limited to pediatric ophthalmologists to provide a more homogenous sampling group that can be meaningfully interpreted for ergonomic change and innovation.
Results
We had a 10% response rate (101/1000), with 66.3% of participants reporting chronic pain. Chronic neck pain (41%), lower back pain (31%), and shoulder pain (30%) were the three leading MSD complaints (Table 1). Participants often had multiple types of pain, including 13% of the sample who experienced all three types of pain.
 |
Table 1 Types of Reported Pain from n=101 Participants |
We calculated the odds ratios for associating chronic pain with various devices and methods to uncover the relationship between specific instruments and chronic pain. (an odds ratio>1 indicates pain is related to that device or method) It would present as the number of hours worked increases by increments of 5 hours per week. Table 2 indicates that shoulder and lower back pain increases with surgical loupe use during surgery (p=0.094 and p=0.078 respectively); also, elbow pain and upper back pain are likely to develop with increased slit lamp use (p=0.057 and p=0.060 respectively). Furthermore, as the number of years in practice increases by 5, the likelihood of ophthalmologists developing chronic neck and lower back increases (p=0.030 and p=0.003 respectively) (Table 2). Additionally, as the number of surgeries performed each week is increased by two, the likelihood of wrist pain also becomes significant (p=0.008). Additionally, neck pain (p=0.03) and lower back pain (p=0.003) are more likely to increase with years of experience.
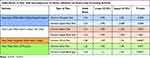 |
Table 2 Odds Ratios as for Pain More Likely to Occur as the Number of Hours Increases with the Use of Each Instrument |
Those suffering from chronic neck, shoulder, wrist, and lower back pain have sought treatment for their MSD (p<0.05 for all four types of pain). Some with pain actively participate in exercise programs specifically for these issues. Our results show chronic neck pain, shoulder pain, and lower back pain are associated with those who actively participate in an exercise program for pain relief (Table 3). Of the respondents, 45% have considered getting their posture evaluated. Corrective surgeries were more likely to occur with those reporting wrist pain (p=0.0015) and hip pain (p=0.0018).
 |
Table 3 Chronic Pain Associated with Those Actively Participating in and Exercise Program to Address with Chronic Pain |
Those reporting shoulder pain reported a greater incidence in making a change in the number of hours of their work (ie, alter, cut, modify, stop) (83% of those with pain vs 65% without pain, p =0.09) (Table 4). A Pearson-Chi square exact test demonstrated that chronic shoulder and chronic neck pain are not independent of each other and either occur simultaneously (25%) or do not occur at all (55%) (p<0.001). Thus, the presence of multiple types of pain may have contributed to a change in the number of hours worked.
 |
Table 4 Altered Work Activity with Shoulder Pain |
The Spearman correlation for the number of pain areas and years of experience is 0.36 (p=0.03) (Figure 1). A count data model based on the zero-inflated negative binomial distribution indicates that a person can have 1 area of pain within a year. Within 25 years, a person can have two areas of pain. Within 40 years, a person can have three areas of pain (Figure 1). The positive slope of the fitted curve to these data also indicates a possible increase in the number of pain areas with years of experience (p=0.30) (Figure 1). However, the small sample size for the study was unable to detect if this increase exists.
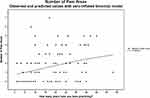 |
Figure 1 Count data model based on the negative binomial distribution. |
Additionally, among surgical loupe wearers, we noted a 4.27 times greater incidence of chronic upper back pain among those wearing 2.0x surgical loupes versus those wearing 4.0x surgical loupes.
Discussion
The field of Ergonomics in Ophthalmology is a growing area of interest. Our study results show that 2/3 of the participants have chronic pain.
Taken together, this data suggests that pediatric ophthalmologists will likely develop at least one MSD within 25 years of practice. Chronic MSDs lead pediatric ophthalmologists to modify their work behaviors and work fewer hours. The authors believe that the development of MSDs likely leads to disability and early retirement among pediatric ophthalmologists. As chronic pain increased, the number of hours worked decreased among ophthalmologists. Of note, there was a 5% increase in the number of pain areas reported among ophthalmologists with every five years practiced. Ergonomic innovations and interventions in the workplace may reduce the healthcare burden and prolong pediatric ophthalmologists’ ability to provide services.
MSD development in the operating room comes from standing or sitting in static positions for prolonged periods, placing stress and strain on muscles and tendons contributing to MSD development. There are many fine, precise, repetitive motor movements that must be made during procedures and high patient volumes that further contribute to MSD development. There are many recommendations to promote proper postures while performing operations. While these recommendations can reduce MSD development, there has been very little done to rethink or reinvent our surgical tools to encourage healthier postures.
The advent of surgical loupes impacted many surgical fields and subspecialties, and there was good evidence that loupe use increased Visual acuity operating ergonomics and provided greater surgical precision. However, other evidence suggested that despite some ergonomic improvement, loupes may increase neck and back strain and limit the depth of vision.4,10
Our previous work has shown that conventional surgical loupes are heavy, promote unhealthy postures and load inappropriate force onto the axial skeleton. By completely redesigning the loupe to be lighter, altering the angle of declination, and adding a novel Suh-Hermsen head strap, posture is corrected, and force on the axial skeleton decreased.11
A study in retinal surgeons demonstrated that indirect ophthalmoscope use during examinations and procedures promoted poor postures of spinal flexion, lateral bending, and rotation.4 Studies suggest that methods should be designed to facilitate neutral spine position during exams, such as raising operating tables to appropriate heights or bringing a patient’s eye to same height level as the examiner in a clinic.12
In a recently published article, the authors reported that pediatric ophthalmologists are prone to developing MSD because of the repetitive movements and awkward positioning required for strabismus surgery.13 Hyer et al performed an extensive survey on the United Kingdom ophthalmologists to determine the prevalence of MSD. Of their 518 replies, 50.6% reported back pain, 31.8% reported neck pain, and 62.4% reported having both. They further stratified their data into the prevalence of pain in each ophthalmic subspecialty. Oculoplastic and retina specialists had the highest reported prevalence of neck pain (~40% each), while pediatrics and strabismus reported the lowest prevalence (~20%). In terms of back pain, the prevalence for all subspecialties was around 50%.8 Other surveys performed on oculoplastic and retina specialists found a much higher prevalence of MSD than in the general population of ophthalmologists. A study conducted in 2004 depicted that only 15% of retina specialists were pain-free.12 In a 2011 survey of oculoplastic surgeons, 27.5% of respondents reported being pain-free when operating.14
When compared to our published work, it seems that pediatric ophthalmologists have a lower prevalence of MSD than that of other ophthalmic subspecialties, as 34% of our respondents were pain-free. Further classifying pain, 41% of respondents had neck pain, and 31% had lower back pain. From our data, pediatric ophthalmologists had a higher neck pain prevalence than the general ophthalmology population but reported a lower prevalence of back pain. The authors believe the primary source of neck pain is refraction exams that involve retinoscopy and indirect ophthalmoscopy and more surgical cases performed using surgical loops. The increased prevalence of neck pain could be due to the awkward neck positions assumed during eye examinations, especially in small children repetitively, thus straining their necks and back. In addition, pediatric ophthalmologists may spend less time operating with a microscope than other subspecialties, reducing lower back pain.
Other studies have suggested modifications for proper slit lamp use to prevent the development of MSD. These recommendations include positioning of the examiner closer to the patient as well as the slit lamp device to prevent forward flexion of the thoracic spine, and neck flexion to see through the ocular objectives; positioning the slit lamp at the proper height to avoid a slouched thoracic position and inferior translation of the head.15
To our knowledge, there are no published studies on redesigning these tools to promote neutral spine postures and beginning to reinvent our tools.
Limitations and Future Studies
Limitations to our study included a 10.1% response rate which is a common concern with survey articles. We sent out a reminder email two weeks after the initial survey was distributed to increase the response rate. Additionally, we did not inquire about the working distance of our participants, which could be an important factor in the development of MSD, especially neck problems due to leaning over the patient due to short working distance. We only examined the number of years they had been practicing. Furthermore, we did not investigate gender-specific differences in the reporting of chronic MSDs. Our survey should increase power by including oculoplastic, retinal, and general ophthalmologists.
Moreover, reaching out to retired ophthalmologists for a survey about their surgical loupe use in the past, the number of years in practice, the reason for retirement may be insightful. Lastly, the prevalence of MSDs in surveys may be over-reported, as physicians will be more likely to respond if they suffer from an MSD. Survey questions did not consider other coexisting conditions such as systemic diseases- health issues (overweight/ previous orthopedical surgery/sports habits etc. Therefore, the reported chronic pain in the manuscript cannot be attributed all to MSD. Additionally, the strength and endurance of muscles such as the neck, back, shoulder, and wrist muscles vary, and it may be one of the factors influencing pain in each region. Future studies need to consider this variable.
In conclusion, in our study, the reported prevalence of chronic neck pain and back pain was comparable to previous studies and published literature, with 2/3 of participants reporting pain. There is a tremendous need for ongoing innovations, especially surgical loupes, operating microscopes, and slit-lamp modifications to prevent musculoskeletal disease.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–656.
2. United States Bone and Joint Iniciative. The burden of musculoskeletal diseases in the United States (BMUS). 2014.
3. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi:10.1016/S0140-6736(17)32154-2
4. Shaw C, Bourkiza R, Wickham L, Mccarthy I, Mckechnie C. Mechanical exposure of ophthalmic surgeons: a quantitative ergonomic evaluation of indirect ophthalmoscopy and slit-lamp biomicroscopy. Can J Ophthalmol. 2017;52(3):302–307. doi:10.1016/j.jcjo.2016.09.011
5. Punnett L, Prüss-üstün A, Nelson DI, et al. Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind Med. 2005;48(6):459–469. doi:10.1002/ajim.20232
6. Chatterjee A, Ryan WG, Rosen I, Manchester ES. Back pain in ophthalmologists. 1994.
7. North C; The Departments of Research (P A M, Ophthalmology MP. Symptoms of musculoskeletal disorders in ophthalmologists. 2005.
8. Hyer JN, Lee RM, Chowdhury HR, Smith HB, Dhital A, Khandwala M. National survey of back & neck pain amongst consultant ophthalmologists in the United Kingdom. Int Ophthalmol. 2015;35(6):769–775. doi:10.1007/s10792-015-0036-z
9. Kitzmann AS, Fethke NB, Baratz KH, Zimmerman MB, Hackbarth DJ, Gehrs KM. A survey study of musculoskeletal disorders among eye care physicians compared with family Medicine physicians. Ophthalmology. 2012;119(2):213–220. doi:10.1016/j.ophtha.2011.06.034
10. Punnett L, Warren N, Henning R, Nobrega S, Cherniack M. Participatory ergonomics as a model for integrated programs to prevent chronic disease. J Occup Environ Med. 2013;55(12SUPPL):S19–S24. doi:10.1097/JOM.0000000000000040
11. Akhter S, Hermsen J, Kalaga P, et al. Surgical magnification loupe customization to prevent chronic back and neck pain in ophthalmic surgeons. Investig Ophthalmol Visual Sci. 2018;59(9):5214.
12. Desai UR, Abdulhak MM, Bhatti R. Occupational Back and Neck Problems in Vitreoretinal Surgeons. American Society of Retina Specialists Meeting; 2004.
13. Bonafede L, Kazmierczak L, Siddicky SF, Gunton KB. Ergonomics in strabismus surgery. Curr Opin Ophthalmol. 2019;30(5):331–336. doi:10.1097/ICU.0000000000000594
14. Sivak-Callcott JA, Diaz SR, Ducatman AM, Rosen CL, Nimbarte AD, Sedgeman JA. A survey study of occupational pain and injury in ophthalmic plastic surgeons. Ophthal Plast Reconstr Surg. 2011;27(1):28–32. doi:10.1097/IOP.0b013e3181e99cc8
15. Ratzlaff TD, Diesbourg TL, McAllister MJ, von Hacht M, Brissette AR, Bona MD. Evaluating the efficacy of an educational ergonomics module for improving slit lamp positioning in ophthalmology residents. Can J Ophthalmol. 2019;54(2):159–163. doi:10.1016/j.jcjo.2018.05.016
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
