Back to Journals » Clinical Ophthalmology » Volume 16
The Prevalence of Demodex Blepharitis in US Eye Care Clinic Patients as Determined by Collarettes: A Pathognomonic Sign
Authors Trattler W, Karpecki P , Rapoport Y, Sadri E, Schachter S, Whitley WO, Yeu E
Received 23 December 2021
Accepted for publication 9 March 2022
Published 15 April 2022 Volume 2022:16 Pages 1153—1164
DOI https://doi.org/10.2147/OPTH.S354692
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
William Trattler,1 Paul Karpecki,2 Yuna Rapoport,3 Ehsan Sadri,4 Scott Schachter,5 Walter O Whitley,6 Elizabeth Yeu6
1Center for Excellence in Eye Care, Miami, FL, USA; 2Kentucky Eye Institute, Lexington, KY, USA; 3Manhattan Eye, New York City, NY, USA; 4Visionary Eye Institute, Newport Beach, CA, USA; 5Advanced Eyecare, Pismo Beach, CA, USA; 6Virginia Eye Consultants, Norfolk, VA, USA
Correspondence: Elizabeth Yeu, Virginia Eye Consultants, 241 Corporate Boulevard, Suite 210, Norfolk, VA, 23502, Tel +1 757 793 4942, Fax +1 757 319 2493, Email [email protected]
Purpose: To evaluate the prevalence of Demodex blepharitis by its pathognomonic sign, collarettes, in patients presenting for any reason to eye care clinics in the United States.
Patients and Methods: In this retrospective study by 7 investigators at 6 eye care clinics, case records of consecutive patients who underwent a slit-lamp examination, regardless of chief complaint, were reviewed for Demodex blepharitis, as identified by the presence of collarettes. Patient characteristics, including age, gender, race, relevant ocular and systemic diagnoses, ocular medications, lid hygiene practices and contact lens wear, were also recorded.
Results: Of 1032 patients (mean age: 60.2 ± 17.8 years), 57.7% had Demodex blepharitis. While the prevalence of Demodex blepharitis in patients with dry eye disease (DED) (58.9%) and cataract (55.7%) was similar to the overall prevalence of Demodex blepharitis, it was higher in patients with blepharitis (69.1%) and glaucoma (64.8%). Among patients with collarettes, 44.0% had never been diagnosed with blepharitis. Among those on anti-inflammatory DED treatment, 60.0% had Demodex blepharitis. Demodex blepharitis prevalence was significantly higher among those using topical tea tree oil versus those who were not (74.5% versus 56.7% p = 0.014); prevalence was comparable among those using/not using lid wipes (56.9% versus 55.5%).
Conclusion: Demodex blepharitis, based on the pathognomonic finding of collarettes, is common and likely underdiagnosed among patients seeking eye care. These collarettes are still found in patients using over-the-counter treatments for blepharitis. The present study highlights the importance of screening patients for collarettes and Demodex blepharitis as part of every slit-lamp examination.
Keywords: prevalence of Demodex blepharitis, collarettes, cylindrical dandruff, Demodex mites, Demodex infestation, lid margin disease
Introduction
Blepharitis is a common ocular disease that is characterized by inflammation of the eyelid margin, redness and ocular irritation.1–5 It is typically diagnosed by an eye care professional; In a 2009 US survey, nearly one-third of the patients seen by an ophthalmologist and approximately half of patients seen by an optometrist had signs of blepharitis.6 Among other etiologies, blepharitis may be caused by an infestation of Demodex mites, the most common ectoparasite found in humans.6,7 Despite the frequent association between Demodex infestation and blepharitis,8–11 it is often overlooked in eye exams.12 In addition to lack of awareness, diagnosis may be limited by the lack of FDA-approved treatment options and/or challenges in diagnosis. Historically, definitive diagnosis of Demodex infestation has typically been accomplished by visualization of the mites during microscopic evaluation of epilated eyelashes.13 However, this technique is impractical as it is uncomfortable for patients, time consuming for the clinician, and not available to practices that lack access to light microscopy.
As Demodex mites have no method of internal digestion, they excrete proteases and lipases for external digestion of the eyelid’s healthy epithelial cells and sebum (or meibum of the meibomian glands, which is a modified sebum).14 Additionally, since the mites do not have excretory organs, regurgitated undigested material, combined with the epithelial cells, often pushes out of the follicle and accumulates around the base of the eyelashes to form collarettes, also referred to as cylindrical dandruff (CD).13 Demodex mites are the only organisms to create the lash-cuffing collarettes, and the deposits may include lipids, keratin, Demodex eggs and dead Demodex mites.14 Collarettes are a pathognomonic sign of Demodex blepharitis.3,4,8,15–22 In a study of eyelashes with and without collarettes, 100% of the lashes with collarettes were found to have Demodex mites.15 Additionally, when researchers in a recent study used PCR testing to identify mite DNA, all eyes with CD were positive for Demodex.23
The prevalence of Demodex blepharitis in community populations (ie, general populations, not necessarily those complaining of blepharitis symptoms) studied outside the US has been reported to range from 41% to 70%.23–29 There is a need to better understand the prevalence of Demodex mite infestation in patients encountered in routine clinical practice in the US. The purpose of this study was to evaluate the prevalence of Demodex blepharitis as confirmed by the presence of collarettes in patients presenting to US eye care clinics for any reason, including but not limited to annual examinations, contact lens exams, and medical eye exams for glaucoma, cataract evaluation, and dry eye disease (DED).
Materials and Methods
Six US optometry and ophthalmology clinics participated in this multicenter retrospective study: Advanced Eyecare in Pismo Beach, CA; Center for Excellence in Eye Care, Miami, FL; Kentucky Eye Institute, Lexington, KY; Manhattan Eye, New York City, NY; Virginia Eye Consultants, Norfolk, VA; and Visionary Eye Institute, Newport Beach, CA. Each clinic enrolled consecutive patients who visited for any purpose over a three-week period. The study was conducted in compliance with the study protocol and followed the tenets of the Declaration of Helsinki and its amendments. Salus Independent Review Board (Austin, USA) approved the study with waiver of informed consent as the data were recorded in patient charts as a part of routine clinical practice, and only de-identified patient data was analyzed.
Seven investigators at the 6 sites each reviewed case records for up to 180 consecutive patients who visited the eye clinic and who underwent a slit lamp examination including examination of the upper lid lashes and lash margin as part of routine practice protocols, regardless of chief complaint. Patients who had an active ocular infection (eg, acute conjunctivitis) or lid structural abnormalities that could have interfered with assessment of collarettes were excluded.
Besides the presence or absence of collarettes, additional patient characteristics, including age, gender, race/ethnicity, relevant ocular and systemic diagnoses, ocular medications, and lid hygiene practices, contact lens wear, and use of artificial eyelashes/eyelash extensions were also recorded.
Outcome Measures
The primary outcome measure was the prevalence of Demodex blepharitis, as confirmed by the presence of collarettes, in the overall dataset. The prevalence of Demodex blepharitis and its association with age, visit types, gender, and various comorbidities (blepharitis, meibomian gland dysfunction, DED, cataract, glaucoma, rosacea, diabetes, hypertension) was also evaluated. In addition, association with the use of concomitant medications or other home-based products (cyclosporine or lifitegrast for dry eye, prostaglandin analogues (PGA) for glaucoma, topical or oral steroids, oral medications, lid hygiene wipes, tea tree oil), contact lens wear and artificial eyelashes/eyelash extensions use was also evaluated.
Statistical Analysis
Continuous data were described using descriptive statistics (mean and standard deviation) and categorical data were described using the participant count and percentage in each category. The association between Demodex blepharitis and patient characteristics or risk factors was assessed using logistic regression. Odds ratios (OR) with 95% confidence intervals were reported. The independent t-test or its non-parametric counterpart, the Mann–Whitney U-test, was used as appropriate to compare the means (scale data) between the two groups. A p value of <0.05 was considered statistically significant.
Results
Investigators in this retrospective study reviewed 1032 case records that met the inclusion criteria. The mean age was 60.2 ± 17.8 years (range: 6 to 95 years) with a higher proportion of participants being female (61.9%) than male (38.0%). Table 1 presents the demographic details of the study participants. The prevalence of Demodex blepharitis in the overall study population was 57.7% (n=595/1032) (Figure 1). The mean age of participants with and without Demodex blepharitis was comparable (60.4±18.1 versus 60.0±17.5; p=0.568). While age was not a significant predictor of Demodex blepharitis (OR 1.001; 95% confidence interval (CI): 0.994 to 1.008; p=0.728) (Figure 2), males had a higher predisposition for Demodex blepharitis (62.9%) compared to females (54.5%) (OR: 1.414; 95% CI: 1.093 to 1.829; p=0.008).
 |
Table 1 Demographic Characteristics |
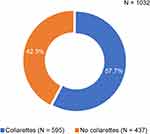 |
Figure 1 Prevalence of Demodex blepharitis, as confirmed by the presence of collarettes, in the overall dataset. |
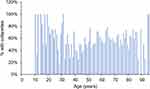 |
Figure 2 Prevalence of Demodex blepharitis by age of patients. |
The prevalence of Demodex blepharitis stratified by visit type is shown in Figure 3. The prevalence of Demodex blepharitis among the top four visit types was 64.8% of those presenting for a comprehensive/annual examination, 59.9% of those with cataract (whether preoperative workup or postoperative follow-up), 53.5% of those seen for a DED evaluation, and 60.8% of those seen for a glaucoma visit.
 |
Figure 3 Prevalence of Demodex blepharitis, by visit type. Orange horizontal bar indicates the overall prevalence. |
In addition to overall prevalence and prevalence by age and visit type, specific patient characteristics that might have been expected to influence the prevalence of Demodex blepharitis were also evaluated and OR for these characteristics were calculated. The prevalence of Demodex blepharitis and OR in patients with various ocular and systemic comorbidities are shown in Table 2. Patients diagnosed with blepharitis were more likely to have collarettes than those who were not (69.1%, n=327/473 versus 47.6%, n=258/542; OR=2.465; p<0.001). Likewise, glaucoma patients had significantly higher risk of having Demodex blepharitis than non-glaucoma patients (64.8%, n=153/236 versus 55.6%, n=442/795; OR=1.472, p=0.012). After controlling for age, the association between glaucoma and Demodex blepharitis was still significant.
 |
Table 2 Prevalence of Demodex Blepharitis, as Confirmed by the Presence of Collarettes, in Patients with Various Ocular or Systemic Comorbidities |
The prevalence of Demodex blepharitis and OR in patients receiving concomitant medications or products are shown in Table 3. There was no significant difference in the prevalence of Demodex blepharitis in participants who were using anti-inflammatory DED medications, compared to those who were not (60.0%, n=135/225 versus 57.0%, n=460/807, OR=1.132). The prevalence of Demodex blepharitis tended to be higher for patients on prostaglandin analogues versus those who were not (67.8%, n=59/87 versus 57.7%, n= 506/877, OR=1.545). Demodex blepharitis prevalence was significantly higher among those using topical tea tree oil versus those who were not (74.5%, n=38/51 versus 56.7%, n=556/980; OR=2.229, p=0.014). However, Demodex blepharitis was similarly prevalent among those using versus not using lid wipes (56.9%, n=58/102 versus 55.5%, n=456/822; OR=1.058).
 |
Table 3 Prevalence of Demodex Blepharitis in Patients Using Concomitant Medications, Products, Contact Lenses, or Artificial Eyelashes |
The prevalence of Demodex blepharitis was lower among contact lens wearers compared to those not using contact lenses; however, the difference was not statistically significant (50.6%, n= 44/87 versus 58.5%, n=501/856; OR=0.725) (Table 3). Patients with Demodex blepharitis were less likely to wear contact lenses than those without Demodex blepharitis (8.1%, n=44/545 versus 10.8%, n=43/398); this was also not statistically significant (Table 3).
The prevalence of Demodex blepharitis was comparable in patients diagnosed with DED whether they were receiving prescription DED treatment (cyclosporine or lifitegrast) or not (62.0% vs 58.0%; p=0.356) (Figure 4). Patients with both MGD and rosacea were more likely to have Demodex blepharitis (29/42, 69.0%) than those with MGD alone (89/162, 55.0%), although the difference was not statistically significant (p=0.099) (Figure 5). A lower percentage of patients using contact lenses had collarettes with concomitant blepharitis and DED compared to those not using contact lenses (15.0% vs 23.0%; p=0.070) (Figure 6).
 |
Figure 4 Prevalence of Demodex blepharitis in patients diagnosed with dry eye disease (DED) who were receiving or not receiving prescription DED therapy. |
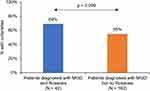 |
Figure 5 Prevalence of Demodex blepharitis in patients diagnosed with meibomian gland dysfunction (MGD), with or without concomitant rosacea. |
 |
Figure 6 Percentage of patients with concomitant blepharitis, dry eye disease (DED) and presence of collarettes in contact lens wearers versus those who were not using contact lenses. |
Discussion
The present study found the prevalence of Demodex blepharitis, as confirmed by the presence of collarettes, to be 57.7% among all patients visiting eye care clinics. This study presents a large, geographically diverse data set representing patients of all ages presenting to optometric and ophthalmology offices across the U.S for a wide variety of reasons. The top four reasons for eye care visits were annual exam, cataracts, dry eye, and glaucoma. Together, these types of visits accounted for ~77% of the overall dataset. These findings indicate a high prevalence of Demodex blepharitis regardless of the chief complaint when visiting an eye care provider.
The prevalence rate identified in the present study (57.7%) corroborates the findings of many studies conducted outside the US documenting prevalence between 41% and 70%23–29 and is consistent with the findings of a recent cross-sectional study in the US, in which the prevalence of Demodex infestation was 55.3%.30
Collarettes are a pathognomonic sign of Demodex blepharitis. They can be readily identified at the slit lamp by instructing patients to look down so that there is a clear view of the base of the upper lash margin.15,31 Incorporating this simple visual observation examination into the slit lamp exam in routine clinical practice may facilitate more timely diagnosis of Demodex blepharitis. The findings of this study may help quantify the prevalence of Demodex blepharitis in real-life clinical practice. The close correlation between the prevalence rate in the present study, based on collarette identification, and the prevalence rates reported in the literature based on mite counts suggests that collarettes may be a reasonable substitute for epilation and mite counts for diagnostic purposes.
Contrary to popular expectation, age was not a significant predictor of Demodex blepharitis; however, the study population was somewhat skewed toward an older age range; 75% of patients were over 50 years old. As such, the precise association between age and Demodex blepharitis prevalence cannot be determined from this study. Further prevalence studies with a more equally distributed age range are needed to better understand the relationship between age and Demodex infestation. The present study, however, did show that it is not uncommon to find signs of Demodex blepharitis in patients of all ages presenting for eye care visits.
Two-thirds of blepharitis patients in this study had collarettes, which is consistent with the literature reporting concomitant Demodex infestation in 45% to 90% of blepharitis patients.9,10,21,30,32–37 Of note, 44% of the patients with collarettes had not previously been diagnosed with blepharitis, suggesting considerable underdiagnosis of Demodex blepharitis.
The prevalence of Demodex blepharitis in the overall dataset was similar to the prevalence of DED (58.4%; n=593/1015), which indicates that Demodex blepharitis may be as common as DED. Almost 60% of the DED patients also had Demodex blepharitis, suggesting significant overlap of these two co-morbid diseases. These findings suggest that Demodex blepharitis may be a contributing or exacerbating factor to DED. Treatment for ocular surface disease may be unsuccessful and frustrate both patients and clinicians if a major underlying cause, Demodex mite infestation, is not addressed. Patients using lifitegrast and cyclosporine were just as likely to have collarettes as those not using these topical immunomodulators (60.0% vs 57.0%), suggesting that these agents do not affect, and are unlikely to mitigate, Demodex blepharitis. Effective medications to treat Demodex blepharitis may have the potential to provide better relief for dry eye patients.
In the present study, more than half the patients presenting for cataract surgery had Demodex blepharitis (55.7%). Clinical studies have found that more than 80% of patients presenting for cataract surgery have dry eye, and the majority of patients (62.9%) had a rapid tear break-up time of 5 seconds or less.38,39 Failure to identify and treat dry eye and MGD prior to performing preoperative testing for cataract surgery negatively impacts visual outcomes.40 It is also well known that the signs and symptoms of ocular surface disease (OSD) worsen after cataract surgery.41 Demodex blepharitis is a lid margin disease that is known to increase MMP-9, a marker of inflammation, and negatively affect tear break-up time,10,42 possibly affecting the ocular surface homeostasis and patient satisfaction following cataract surgery, particularly in patients undergoing premium intraocular lens (IOL) implantation. Untreated Demodex blepharitis has been reported to increase the risk of punctate keratitis, corneal melting, and postoperative infections (including endophthalmitis).41,43–45 Thus, in order to improve eyelid health and potentially reduce complications after cataract surgery, it is imperative to screen for Demodex blepharitis and initiate treatment in advance of surgical intervention.
In the present study, almost two-thirds of the glaucoma patients had Demodex blepharitis. There is a known association between topical therapy for glaucoma, particularly PGAs, and OSD.46–49 OSD-associated symptoms of burning, itching, and irritation may contribute to poor glaucoma medication compliance and glaucoma progression.50,51 The high prevalence of Demodex blepharitis seen in glaucoma patients in this study suggests that glaucoma patients should be screened for Demodex infestation to ensure that the disease is treated in a timely fashion so as to avoid contributing to ocular symptoms that affect medication compliance.
It is believed that contact lens use may provide a more favorable environment for Demodex mites to proliferate; in fact, contact lens wearers have been documented to harbor more Demodex mites than non-wearers.52 However, in the present study, we found the opposite, with a lower rate of Demodex blepharitis in contact lens wearers compared to non-wearers. Likewise, a higher percentage of patients with Demodex blepharitis were not using contact lenses compared to those who were (10.8% vs 8.1%). While these results were not statistically significant, this corroborates the findings of a prior study showing people who had discontinued contact lens use had significantly higher rate of Demodex infestation compared to contact lens wearers.53 This prior study suggests that Demodex blepharitis could be a significantly underdiagnosed contributor to contact lens intolerance. As such, it is important to always look for collarettes and screen for Demodex blepharitis in patients who wear contact lenses, especially those with contact lens intolerance. More research in current or former contact lens wearers is needed to fully understand the relationship between contact lens wear and Demodex blepharitis.
Tea tree oil (TTO) lid hygiene products are sometimes used for managing Demodex blepharitis despite poor tolerance, low efficacy and not being FDA-approved for this use. Participants using TTO products in the present study were a small percentage of the total population (51/1031, 4.9%) and were more likely to have Demodex blepharitis than those not using TTO (74.5% vs 56.7%; p=0.014). This finding may be interpreted in two ways. First, it is likely that Demodex blepharitis was diagnosed in these patients and the use of TTO products was recommended to manage their disease; consequently, a higher prevalence of collarettes was seen in these patients. Second, since previous studies using TTO products have shown limited levels of success,3,4,7,13,54–56 it may also be that TTO was ineffective in managing Demodex blepharitis, resulting in a continued high prevalence of collarettes among those using TTO products.
Despite the high prevalence of Demodex blepharitis, many clinicians do not routinely screen for it, particularly if the patient is not complaining of symptoms. The reasons for this may be multi-factorial but may be due to the lack of an FDA-approved prescription therapeutic, poor standardization and inconsistent levels of success with various over-the-counter management options, the potential toxicity of TTO to meibomian epithelial cells,57 and/or the discomfort and side effects. Although lash epilation and evaluation of mite density can be performed in Demodex blepharitis clinical trials, assessment of the lid margin for collarettes, the pathognomonic sign of Demodex blepharitis, is a more practical approach to diagnosing Demodex blepharitis in clinical practice, given that studies have previously demonstrated that 100% of patients with collarettes have Demodex.15 Collarettes have a very specific waxy, often translucent, cuff or plug-like appearance stuck to the base of the lash follicle that is easily identified by examining the upper lid margin and lash base while a patient looks down at the slit lamp. Participating investigators in the present study found that evaluating the lashes for collarettes was a straightforward, quick and comfortable method to confidently identify Demodex blepharitis patients.
This study is limited by its retrospective study design. A prospective study with patients equally distributed across all age groups could help to better understand the prevalence of Demodex blepharitis and collarettes in different age groups.
Conclusion
Demodex blepharitis is as common as dry eye in patients presenting for routine visits to ophthalmology and optometry practices. Of the four most common reasons for an eye care visit, we found that between 54% and 65% of patients making those visits had collarettes, the pathognomonic sign of Demodex blepharitis. Demodex blepharitis was common among people of all ages, race/ethnicity, and gender. Almost half the patients with collarettes had never been diagnosed with blepharitis, indicating substantial underdiagnosis either due to misdiagnosis or missed diagnosis. As such, the present study highlights the need to screen patients for collarettes and Demodex blepharitis in routine clinical practice.
Acknowledgments
Raman Bedi, MD (IrisARC - Analytics, Research & Consulting, Chandigarh, India) and Jan Beiting (Wordsmith Consulting, Cary, North Carolina) provided statistical and editorial assistance in the preparation of this manuscript.
Funding
This study was funded by research grants to the investigators from Tarsus Pharmaceuticals.
Disclosure
Dr William Trattler reports grants from Tarsus, during the conduct of the study; personal fees from Tarsus, personal fees from Allergan, personal fees from Sun Pharma, personal fees from Novartis, personal fees from Johnson & Johnson, outside the submitted work; Dr Paul Karpecki reports personal fees from Tarsus Pharmaceuticals, personal fees from Oasis Medical, personal fees from BioTissue, personal fees from OcuSoft, personal fees from Danelli Ocular Creations, personal fees from Alcon, personal fees from J&J, outside the submitted work; Dr Yuna Rapoport has nothing to disclose. Dr Ehsan Sadri reports being a consultant for Visionary Eye Institute, outside the submitted work; and Speaker Research Grant. Dr Scott Schachter reports working for Allergan.
Dr Walter Whitley reports personal fees from Tarsus Pharmaceuticals, during the conduct of the study; personal fees from Tissue Tech, personal fees from Alcon, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Amescua G, Akpek EK, Farid M, et al. Blepharitis Preferred Practice Pattern(R). Ophthalmology. 2019;126(1):56–93.
2. Dias MR, Guaresch BLV, Borges CR, Biazim DF, Casagrande D, Luz RA. Blefarite: epidemiologia, etiologia, apresentações clínicas, tratamento e evolução de nossos pacientes. Rev Bras Oftalmol. 2019;78(5):300–303.
3. Messaoud R, El Fekih L, Mahmoud A, et al. Improvement in ocular symptoms and signs in patients with Demodex anterior blepharitis using a novel terpinen-4-ol (2.5%) and hyaluronic acid (0.2%) cleansing wipe. Clin Ophthalmol. 2019;13:1043–1054.
4. Savla K, Le JT, Pucker AD. Tea tree oil for Demodex blepharitis. Cochrane Database Syst Rev. 2020;6:CD013333.
5. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15(3):539–574.
6. Eberhardt M, Rammohan G. Blepharitis. Treasure Island (FL): StatPearls; 2020.
7. Zhang AC, Muntz A, Wang MTM, Craig JP, Downie LE. Ocular Demodex: a systematic review of the clinical literature. Ophthalmic Physiol Opt. 2020;40(4):389–432.
8. Avila MY, Martinez-Pulgarin DF, Rizo Madrid C. Topical ivermectin-metronidazole gel therapy in the treatment of blepharitis caused by Demodex spp.: a randomized clinical trial. Cont Lens Anterior Eye. 2020;44(3):30084–30089.
9. Biernat MM, Rusiecka-Ziolkowska J, Piatkowska E, Helemejko I, Biernat P, Gosciniak G. Occurrence of Demodex species in patients with blepharitis and in healthy individuals: a 10-year observational study. Jpn J Ophthalmol. 2018;62(6):628–633.
10. Kabatas N, Dogan AS, Kabatas EU, Acar M, Bicer T, Gurdal C. The Effect of Demodex Infestation on Blepharitis and the Ocular Symptoms. Eye Contact Lens. 2017;43(1):64–67.
11. Suresha A, Sadhwini M. Role of demodex infestation in blepharitis and coconut oil as a treatment option. Indian J Clin Exp Ophthalmol. 2020;6(2):270–275.
12. Cheng AM, Sheha H, Tseng SC. Recent advances on ocular Demodex infestation. Curr Opin Ophthalmol. 2015;26(4):295–300.
13. Fromstein SR, Harthan JS, Patel J, Opitz DL. Demodex blepharitis: clinical perspectives. Clin Optom. 2018;10:57–63.
14. Nicholls SG, Oakley CL, Tan A, Vote BJ. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017;37(1):303–312.
15. Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089–3094.
16. Luo X, Li J, Chen C, Tseng S, Liang L. Ocular Demodicosis as a Potential Cause of Ocular Surface Inflammation. Cornea. 2017;36(Suppl 1):S9–S14.
17. Zhong J, Tan Y, Li S, et al. The Prevalence of Demodex folliculorum and Demodex brevis in Cylindrical Dandruff Patients. J Ophthalmol. 2019;2019:8949683.
18. Ziaja-Sołtys M, Kołodziejczyk M, Rymgayłło-Jankowska B, et al. Massive Demodicosis of the Eyes in a Patient with Sjögren Syndrome: a Case Report. Acta Parasitol. 2021;66(2):677–681.
19. Randon M, Liang H, El Hamdaoui M, et al. In vivo confocal microscopy as a novel and reliable tool for the diagnosis of Demodex eyelid infestation. Br J Ophthalmol. 2015;99(3):336–341.
20. Bitton E, Aumond S. Demodex and eye disease: a review. Clin Exp Optom. 2021;104(3):285–294.
21. Lopez-Ponce D, Zuazo F, Cartes C, et al. High prevalence of Demodex spp. infestation among patients with posterior blepharitis: correlation with age and cylindrical dandruff. Arch Soc Esp Oftalmol. 2017;92(9):412–418.
22. Rabensteiner DF, Aminfar H, Boldin I, et al. Demodex Mite Infestation and its Associations with Tear Film and Ocular Surface Parameters in Patients with Ocular Discomfort. Am J Ophthalmol. 2019;204:7–12.
23. Kasetsuwan N, Kositphipat K, Busayarat M, et al. Prevalence of ocular demodicosis among patients at Tertiary Care Center, Bangkok, Thailand. Int J Ophthalmol. 2017;10(1):122–127.
24. Murphy O, O’Dwyer V, Lloyd-McKernan A. Ocular Demodex folliculorum: prevalence and associated symptoms in an Irish population. Int Ophthalmol. 2019;39(2):405–417.
25. Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between demodex and ocular discomfort. Invest Ophthalmol Vis Sci. 2010;51(6):2906–2911.
26. Szkaradkiewicz A, Chudzicka-Strugala I, Karpinski TM, et al. Bacillus oleronius and Demodex mite infestation in patients with chronic blepharitis. Clin Microbiol Infect. 2012;18(10):1020–1025.
27. Sedzikowska A, Oseka M, Skopinski P. The impact of age, sex, blepharitis, rosacea and rheumatoid arthritis on Demodex mite infection. Arch Med Sci. 2018;14(2):353–356.
28. Sedzikowska A, Oseka M, Grytner-Ziecina B. Ocular symptoms reported by patients infested with Demodex mites. Acta Parasitol. 2016;61(4):808–814.
29. Wesolowska M, Knysz B, Reich A, et al. Prevalence of Demodex spp. in eyelash follicles in different populations. Arch Med Sci. 2014;10(2):319–324.
30. Teo A, Rosenberg E, Jacobson A. Prevalence of Demodex colonization in patients presenting to an outpatient clinic. Invest Ophthalmol Vis Sci. 2021;62(8):1236.
31. Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505–510.
32. Chanlalit W, Yodprom R, Arampinyokul P. Comparison of clinical manifestations between blepharitis patients with and without demodex infestation. J Med Assoc Thai. 2019;102(6):651–656.
33. Zeytun E, Karakurt Y. Prevalence and load of Demodex folliculorum and Demodex brevis (Acari: demodicidae) in patients with chronic blepharitis in the province of Erzincan, Turkey. J Med Entomol. 2019;56(1):2–9.
34. Zhu M, Cheng C, Yi H, Lin L, Wu K. Quantitative Analysis of the Bacteria in Blepharitis With Demodex Infestation. Front Microbiol. 2018;9:1719.
35. Bhandari V, Reddy JK. Blepharitis: always remember demodex. Middle East Afr J Ophthalmol. 2014;21(4):317–320.
36. Divani S, Barpakis K, Kapsalas D. Chronic blepharitis caused by Demodex folliculorum mites. Cytopathology. 2009;20(5):343–344.
37. Zhao YE, Wu LP, Hu L, Xu JR. Association of blepharitis with Demodex: a meta-analysis. Ophthalmic Epidemiol. 2012;19(2):95–102.
38. Gupta PK, Drinkwater OJ, VanDusen KW, Brissette AR, Starr CE. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refract Surg. 2018;44(9):1090–1096.
39. Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423–1430.
40. Matossian C. Impact of Thermal Pulsation Treatment on Astigmatism Management and Outcomes in Meibomian Gland Dysfunction Patients Undergoing Cataract Surgery. Clin Ophthalmol. 2020;14:2283–2289.
41. Afsharkhamseh N, Movahedan A, Motahari H, Djalilian AR. Cataract surgery in patients with ocular surface disease: an update in clinical diagnosis and treatment. Saudi J Ophthalmol. 2014;28(3):164–167.
42. Zhang XB, Ding YH, He W. The association between demodex infestation and ocular surface manifestations in meibomian gland dysfunction. Int J Ophthalmol. 2018;11(4):589–592.
43. Ubeid AMR. The Unsatisfied Patient after Cataract Surgery Ocular Surface Disease as a Major Contributor! Int J Ophthalmol Clin Res. 2018;5:095. doi:10.23937/2378-346X/1410095
44. Murthy R. Lid conditions affecting cataract surgery. J Clin Ophthalmol Res. 2017;5(1):65–66.
45. Speaker MG, Milch FA, Shah MK, Eisner W, Kreiswirth BN. Role of external bacterial flora in the pathogenesis of acute postoperative endophthalmitis. Ophthalmology. 1991;98(5):639–649.
46. Fechtner RD, Godfrey DG, Budenz D, Stewart JA, Stewart WC, Jasek MC. Prevalence of ocular surface complaints in patients with glaucoma using topical intraocular pressure-lowering medications. Cornea. 2010;29(6):618–621.
47. Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17(5):350–355.
48. Rossi GC, Pasinetti GM, Scudeller L, Raimondi M, Lanteri S, Bianchi PE. Risk factors to develop ocular surface disease in treated glaucoma or ocular hypertension patients. Eur J Ophthalmol. 2013;23(3):296–302.
49. Mocan MC, Uzunosmanoglu E, Kocabeyoglu S, Karakaya J, Irkec M. The Association of Chronic Topical Prostaglandin Analog Use With Meibomian Gland Dysfunction. J Glaucoma. 2016;25(9):770–774.
50. Zhang X, Vadoothker S, Munir WM, Saeedi O. Ocular Surface Disease and Glaucoma Medications: a Clinical Approach. Eye Contact Lens. 2019;45(1):11–18.
51. Denis P, Lafuma A, Berdeaux G. Medical outcomes of glaucoma therapy from a nationwide representative survey. Clin Drug Investig. 2004;24(6):343–352.
52. Jalbert I, Rejab S. Increased numbers of Demodex in contact lens wearers. Optom Vis Sci. 2015;92(6):671–678.
53. Tarkowski W, Moneta-Wielgos J, Mlocicki D. Demodex sp. as a Potential Cause of the Abandonment of Soft Contact Lenses by Their Existing Users. Biomed Res Int. 2015;2015:259109.
54. Karakurt Y, Zeytun E. Evaluation of the Efficacy of Tea Tree Oil On the Density of Demodex Mites (Acari: demodicidae) and Ocular Symptoms In Patients With Demodectic Blepharitis. J Parasitol. 2018;104(5):473–478.
55. Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular surface discomfort and Demodex: effect of tea tree oil eyelid scrub in Demodex blepharitis. J Korean Med Sci. 2012;27(12):1574–1579.
56. Navel V, Mulliez A, Benoist d’Azy C, et al. Efficacy of treatments for Demodex blepharitis: a systematic review and meta-analysis. Ocul Surf. 2019;17(4):655–669.
57. Chen D, Wang J, Sullivan DA, Kam WR, Liu Y. Effects of Terpinen-4-ol on Meibomian Gland Epithelial Cells In Vitro. Cornea. 2020;39(12):1541–1546.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
