Back to Journals » Clinical Ophthalmology » Volume 18
The Prevalence and Severity of Acquired Blepharoptosis in US Eye Care Clinic Patients and Their Receptivity to Treatment
Authors Matossian C
Received 21 September 2023
Accepted for publication 15 December 2023
Published 10 January 2024 Volume 2024:18 Pages 79—83
DOI https://doi.org/10.2147/OPTH.S441505
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Cynthia Matossian
Matossian Eye Associates, Doylestown, PA, USA
Correspondence: Cynthia Matossian, 3096 Comfort Road, New Hope, Doylestown, PA, 18938, USA, Tel +1 215-208-6944, Email [email protected]
Purpose: To assess the presence and severity of acquired blepharoptosis (ptosis) among patients visiting an eye care clinic and the receptivity of eligible patients to pharmacologic treatment with oxymetazoline 0.1% ophthalmic solution.
Patients and Methods: Patients aged 50 years or older who had a scheduled clinic appointment for any reason (eg, dry eye, cataract surgery consultation) were asked to respond to written questions about lid position and select whether their upper lid position most closely matched one of 4 images shown to them corresponding to no, mild, moderate, or severe ptosis. Patients selecting any of the mild, moderate, or severe ptosis were offered treatment with oxymetazoline 0.1% ophthalmic solution, barring any medical contraindications. The outcome measures were the proportion of patients with each self-reported lid position level (none to severe ptosis), the proportion of patients with asymmetric ptosis, and the proportion of patients willing to accept the treatment.
Results: Data for 188 eyes of 94 patients were analyzed. Overall, 73.4% of patients had ptosis in at least one eye, and 25.5% had an asymmetric upper eyelid presentation. The proportions of patients with self-reported mild, moderate, or severe ptosis in at least one eye were 41.5%, 25.5%, and 6.4%, respectively. Among those patients eligible for treatment, 19.7% were willing to accept the treatment.
Conclusion: Based on patients’ self-assessment of lid position, this study suggests a higher prevalence of ptosis than reported previously. Evaluation of the eyelids should be a standard part of the comprehensive eye examination.
Keywords: blepharoptosis, ptosis, severity of ptosis, oxymetazoline ophthalmic solution, lid position
A Letter to the Editor has been published for this article.
Introduction
Blepharoptosis, or ptosis, is a common disorder encountered in both optometric and ophthalmic practice. It is an abnormal drooping of the upper eyelid margin with the eye in primary gaze and can be unilateral or bilateral. Acquired ptosis, the predominant form of ptosis, typically appears later in life and is usually caused by aging, eye surgery, or disease affecting the levator muscle or its nerve.1 The reported prevalence of ptosis ranges from 4.7% to 13.5% in adults, but data on the incidence or prevalence of ptosis in a US older adult population is lacking.2–4
Drooping of the eyelids may create an aesthetically undesirable appearance, with patients stating that they look “sleepy” or their eyelids look asymmetrical. With increased severity, the obstruction of the pupil by the upper eyelid may lead to superior visual field deficits affecting vision.5 Despite its negative impact on patients’ vision as well as physical appearance, ptosis is likely underdiagnosed and underreported since treatments were historically limited to a surgical correction, with intervention only at more severe stages and for functional indications.6,7 Moreover, eyelid measurements for ptosis are not routinely performed as part of the comprehensive eye examination.
Literature on patient perceptions of acquired ptosis and awareness of treatment options is sparse. Patients with acquired ptosis may also lack awareness of what type of clinician (ophthalmologist, plastic surgeon, dermatologist, etc.) is best suited to address such concerns. The present study has been designed to assess the presence and severity of ptosis among patients visiting an eye care clinic and the receptivity of eligible patients to pharmacologic treatment with oxymetazoline 0.1% ophthalmic solution.
Materials and Methods
This retrospective, single-center, observational chart-review study was conducted in compliance with the study protocol and followed the tenets of the Declaration of Helsinki and its amendments. The study was approved by Salus Independent Review Board (Austin, TX) with a waiver of informed consent as the data were recorded in patient charts as a part of routine clinical practice, and only de-identified patient data were analyzed.
All consecutive clinic patients aged 50 years or older who had a scheduled clinic appointment during a 3-week period at Matossian Eye Associates for any reason (eg, dry eye, cataract surgery consultation) were included in the study, excluding those in the clinic for an ocular emergency, a scheduled appointment for any planned procedure (eg, thermal pulsation, intense pulsed light treatment, etc.), or for a Day 1 or Week 1 postoperative follow-up visit.
All eligible patients were asked to respond to written questions about lid position and select which of the 4 images shown to them (Figure 1), corresponding to no (A), mild (B), moderate (C) or severe (D) ptosis, most closely matched the position of their eyelids. The patient selected a lid position for each eye separately. Those selecting any option other than A were subsequently examined for ptosis by an experienced provider who checked all patients’ responses to confirm the presence of at least some level of ptosis when patients chose options B, C, or D, ruling out the possibility that ptosis was absent, when patients responded as having mild, moderate, or severe ptosis. Patients showing some degree of ptosis (mild, moderate or severe) were offered treatment with oxymetazoline 0.1% ophthalmic solution. Patients with Sjögren’s syndrome or active ocular infection, for whom the medication would be contraindicated, were not offered treatment. The medication dosing and out-of-pocket costs were clearly explained, and patients’ willingness to accept the treatment was recorded.
 |
Figure 1 Eyelid position by degree of ptosis: (A) no ptosis, (B) mild ptosis, (C) moderate ptosis, (D) severe ptosis. |
The outcome measures were assessment of the proportion of patients with each lid position level (A, B, C, D) in the right and the left eye, the proportion of patients with asymmetric ptosis (a difference in the self-reported level of ptosis for the two eyes), and the proportion of eligible patients willing to accept a prescription for the FDA-approved oxymetazoline hydrochloride ophthalmic solution 0.1%, for the temporary improvement of blepharoptosis.
Statistical Analysis
Data analyses were performed using SPSS software version 27 for windows (IBM SPSS Statistics 27, IBM Inc., Armonk, NY). For categorical/ordinal data, the results are presented as proportions.
Results
Data for 188 eyes of 94 patients were analyzed. Overall, 73.4% of patients had ptosis in at least one eye. Correspondingly, 26.6% of patients had no ptosis in either eye.
Figure 2 shows the proportion of patients reporting each level of ptosis in one or both eyes. Figure 3 shows the self-assessed severity of ptosis by eye. Figure 4 shows that asymmetric ptosis (different levels of severity between the two eyes) was present in 25.5% of patients.
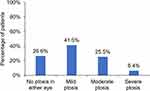 |
Figure 2 Highest severity of ptosis self-reported for one or both eyes. |
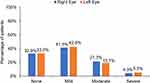 |
Figure 3 Summary of self-reported degree of ptosis for right and left eyes. |
 |
Figure 4 Proportion of patients with symmetric and asymmetric ptosis. |
Of the patients selecting any degree of ptosis (mild, moderate, or severe) who were offered treatment with oxymetazoline 0.1% ophthalmic solution, 19.7% were willing to accept the treatment.
Discussion
Acquired ptosis is a condition of the upper eyelid that has negative cosmetic and functional effects and may affect patient well-being, including increased appearance-related anxiety and depression;1 however, it is likely underdiagnosed and undertreated.1,6 Acquired ptosis is most commonly caused by a progressive, age-related stretching, dehiscence, or detachment of the levator muscle complex known as aponeurotic ptosis.6,8 The underlying etiology can also be myogenic, neurogenic, mechanical, or traumatic. Ocular surgery can also contribute to the development of transient or more persistent forms of ptosis.1
Patient self-assessment is the first step towards diagnosis of ptosis. The present study incorporated a questionnaire about lid position that included visual examples of ptosis, ranging from mild to severe, allowing for self-assessment of ptosis severity. Of note, none of the patients included in this study visited the clinic with ptosis as their chief complaint.
In the present study, we found more than 73% of patients with ptosis in at least one eye, which is much higher than previously reported prevalence rates of 11.5% to 13.4% in adult populations aged ≥40 years.2,4 In a community survey of 400 subjects aged ≥50 years old in the United Kingdom, 11.5% were determined to have ptosis.4 Another study of 17,296 Korean patients ≥40 years old reported an overall prevalence of ptosis of 13.4%.2 The large difference in the results of this study compared with other studies may be due to variations in how ptosis was defined. In the previous studies, ptosis was described as the descent of the upper eyelid margin below the normal anatomical position, and the upper eyelid droop was measured to classify ptosis as mild (1–2 mm), moderate (3–4 mm), and severe (>4 mm). In the present study, images of eyes corresponding to no, mild, moderate, and severe ptosis were shown to patients, but exact measurements of upper eyelid droop were not taken. Nevertheless, the provider did check all patients’ responses to confirm the presence of at least some level of ptosis when patients chose options B, C, or D, ruling out the possibility that ptosis was absent, when patients responded as having mild, moderate, or severe ptosis. This, however, does not rule out the possibility that patients might have under or overestimated the degree of ptosis.
In the present study, as high as 41.5% self-assessed their ptosis as mild. Mild ptosis is less likely to be diagnosed or treated when surgery is the only available intervention. The availability of a noninvasive topical pharmacologic treatment, topical oxymetazoline, 0.1%, offers the potential to treat a wider range of patients.9,10 Oxymetazoline 0.1% ophthalmic solution is a direct-acting α-adrenergic receptor agonist that increases activity of Müller’s muscle α-adrenergic receptors, leading to stronger contractions in Müller’s muscle, thereby keeping the upper eyelid elevated.11 In clinical trials, it significantly improved the superior visual field and upper eyelid elevation in patients with acquired ptosis and accompanying superior visual field deficit.11
Even ptosis patients without visual field deficit, however, may be bothered by their eyelid appearance, but they may not raise the issue with an eye care provider if not prompted. In the author’s personal experience, patients are well aware of the condition but do not realize it can be treated or that it can be treated by an eye care provider without surgery. We found that nearly 20% of eligible patients were receptive to treatment when offered, even with the understanding that the cost of treatment would be out of pocket.
Although acquired ptosis is generally related to aging, there can be other, more serious underlying causes that need to be identified. For example, in Horner syndrome, ptosis is typically mild but can be secondary to trauma, tumor, or carotid dissection.6 Increased patient awareness about ptosis is expected to enable early identification and subsequent treatment. As such, evaluation of the eyelid position should be a standard part of the comprehensive eye examination.6
This study is limited by its retrospective nature and real-world clinical setting. The data are based on patients’ self-assessment, and lid position was not quantitatively measured.
Conclusion
In conclusion, the present representative data based on patients’ self-assessment suggest a higher prevalence of ptosis than reported previously. Patients easily recognize ptosis and are bothered by their lid appearance, with or without functional deficits due to ptosis. Asymmetry may be more common than most clinicians realize. When appropriately counseled, patients are receptive to noninvasive topical treatment for ptosis.
Data Sharing Statement
The data used to support the findings of this study are included within the article. Clarifications or additional data used to support the findings of this study may be requested from the corresponding author.
Acknowledgments
Jan Beiting (Wordsmith Consulting) and Raman Bedi, MD (IrisARC-Analytics, Research & Consulting) provided assistance in preparing this manuscript.
Funding
Funding for this study was provided by RVL Pharmaceuticals.
Disclosure
Dr. Matossian has received consulting income from RVL Pharmaceuticals.
References
1. Bacharach J, Lee WW, Harrison AR, Freddo TF. A review of acquired blepharoptosis: prevalence, diagnosis, and current treatment options. Eye. 2021;35(9):2468–2481. doi:10.1038/s41433-021-01547-5
2. Kim MH, Cho J, Zhao D, et al. Prevalence and associated factors of blepharoptosis in Korean adult population: the Korea National Health and Nutrition Examination Survey 2008–2011. Eye. 2017;31(6):940–946. doi:10.1038/eye.2017.43
3. Hashemi H, Khabazkhoob M, Emamian MH, et al. The prevalence of ptosis in an Iranian adult population. J Curr Ophthalmol. 2016;28(3):142–145. doi:10.1016/j.joco.2016.04.005
4. Sridharan GV, Tallis RC, Leatherbarrow B, Forman WM. A community survey of ptosis of the eyelid and pupil size of elderly people. Age Ageing. 1995;24(1):21–24. doi:10.1093/ageing/24.1.21
5. Meyer DR, Stern JH, Jarvis JM, Lininger LL. Evaluating the visual field effects of blepharoptosis using automated static perimetry. Ophthalmology. 1993;100(5):651–658; discussion 658–659. doi:10.1016/S0161-6420(93)31593-9
6. Nichols KK, Malloy KA, Karpecki PM, et al. Topical review: an update of diagnostic and management algorithms for acquired blepharoptosis. Optom Vis Sci. 2022;99(3):230–240. doi:10.1097/OPX.0000000000001868
7. Cahill KV, Bradley EA, Meyer DR, et al. Functional indications for upper eyelid ptosis and blepharoplasty surgery: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(12):2510–2517. doi:10.1016/j.ophtha.2011.09.029
8. Lim JM, Hou JH, Singa RM, Aakalu VK, Setabutr P. Relative incidence of blepharoptosis subtypes in an oculoplastics practice at a tertiary care center. Orbit. 2013;32(4):231–234. doi:10.3109/01676830.2013.788673
9. Bacharach J, Wirta DL, Smyth-Medina R, et al. Rapid and sustained eyelid elevation in acquired blepharoptosis with oxymetazoline 0.1%: randomized Phase 3 trial results. Clin Ophthalmol. 2021;15:2743–2751. doi:10.2147/OPTH.S306155
10. Wirta DL, Korenfeld MS, Foster S, et al. Safety of once-daily oxymetazoline hcl ophthalmic solution, 0.1% in patients with acquired blepharoptosis: results from four randomized, double-masked clinical trials. Clin Ophthalmol. 2021;15:4035–4048. doi:10.2147/OPTH.S322326
11. Slonim CB, Foster S, Jaros M, et al. Association of oxymetazoline hydrochloride, 0.1%, solution administration with visual field in acquired ptosis: a pooled analysis of 2 randomized clinical trials. JAMA Ophthalmol. 2020;138(11):1168–1175. doi:10.1001/jamaophthalmol.2020.3812
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
