Back to Journals » International Journal of General Medicine » Volume 14
The Predictive Value of Soluble Urokinase-Type Plasminogen Activator Receptor in Contrast-Induced Acute Kidney Injury in Patients Undergoing Percutaneous Coronary Intervention
Authors Qin Y, Qiao Y, Wang D, Yan G, Tang C , Ma G
Received 13 September 2021
Accepted for publication 1 October 2021
Published 7 October 2021 Volume 2021:14 Pages 6497—6504
DOI https://doi.org/10.2147/IJGM.S339075
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yuhan Qin, Yong Qiao, Dong Wang, Gaoliang Yan, Chengchun Tang, Genshan Ma
Department of Cardiology, Zhongda Hospital, Medical School, Southeast University, Nanjing, Jiangsu, People’s Republic of China
Correspondence: Gaoliang Yan
Department of Cardiology, Zhongda Hospital, Medical School, Southeast University, Nanjing, Jiangsu, People’s Republic of China
Email [email protected]
Objective: Soluble urokinase-type plasminogen activator receptor (SuPAR) is a circulating protein and a novel identified promising biomarker for various renal diseases and kidney injury. However, it remains unknown on the predictive value of suPAR in contrast induced acute kidney injury (CI-AKI) in patients undergoing percutaneous coronary intervention (PCI).
Methods: A total of 399 patients undergoing PCI were enrolled in the research from June 2020 to June 2021 in Zhongda Hospital. Patients were divided into CI-AKI and non-CI-AKI groups according to the preoperative and postoperative serum creatinine levels. Plasma suPAR level was detected through enzyme-linked immunosorbent assay on admission. Demographic data, hematological parameters, coronary angiography data and medications were recorded and compared between CI-AKI and non-CI-AKI groups. Logistic regression analysis and receiver operator characteristic (ROC) curve analysis were performed for identifying the independent risk factors of CI-AKI and assessment of the predictive value of suPAR for CI-AKI.
Results: CI-AKI occurred in 65 (16.3%) patients undergoing PCI. The level of suPAR in CI-AKI group was significantly higher than that in the non-CI-AKI group. Multivariate logistic regression indicated diabetes, lower LVEF, lower hydration rate, lower baseline eGFR, higher plasma suPAR (OR = 2.875, 95% CI = 2.038– 3.672, P < 0.001) and volume of contrast media were all independent risk factors for CI-AKI after adjustment of the confounding factors. ROC analysis illustrated that the optimal area under the curve was 0.765, indicating plasma suPAR was a splendid predictor for CI-AKI. The corresponding cut-off value was 3.305 ng/mL, and the sensitivity and specificity were 63.1% and 82.3%, respectively.
Conclusion: Increased suPAR level is independently associated with elevated risk of suffering CI-AKI, and suPAR is a strong predictor for CI-AKI in patients undergoing PCI. SuPAR might act as a novel biomarker for CI-AKI in clinical practice.
Keywords: soluble urokinase-type plasminogen activator receptor, contrast media, acute kidney injury, percutaneous coronary intervention
Introduction
Iatrogenic renal impairment caused by contrast agents administration is the third leading cause of hospital-acquired acute renal injury after hypoperfusion- and drug-associated renal injury.1 The term “contrast induced acute kidney injury” (CI-AKI) is proposed by the Kidney Disease Improving Global Outcomes (KDIGO) working group.2 Multiple researches have demonstrated the relationship between CI-AKI, increased mortality rate,3 and accelerated progression of underlying renal disease. Long-term deterioration of kidney function was also reported correlated with CI-AKI.4
CI-AKI induced by percutaneous coronary intervention (PCI) remains a concern despite the raised awareness and improvements of prevention and risk stratification of CI-AKI.5 Emerging predictors for CI-AKI in patients subjected to PCI have been discovered recently, which might help the diagnosis and risk assessment of CI-AKI.6,7
Urokinase-type plasminogen activator receptor (uPAR) is a glycosylphosphatidylinositol-anchored protein, it is distributed on the cell membrane of a variety of bone marrow cells, immune cells, endothelial cells, fibroblasts and podocytes.8 Under inflammation and immune activation, the glycosyl phosphatidylinositol anchor of uPAR is cleaved by phospholipase C. uPAR Sheds from the activated immune and endothelial cell membrane, then circulating soluble uPAR (suPAR) is formed and released.9 It has been acknowledged that suPAR is correlated with immune activation and inflammation in patients with cardiovascular diseases10 and critically ill patients.11 Recent investigation has suggested Increased suPAR level contribute to deteriorated renal function and poor prognosis in patients with CKD.12 suPAR is involved in the pathogenesis of various kidney diseases, including diabetic nephropathy and focal segmental glomerulosclerosis.13 Elevated suPAR level contributes to endothelial dysfunction in inflammatory diseases, leading to subclinical organ damage and vascular complication in patients with CKD.14 In addition, suPAR has emerged as a promising biomarker in multiple chronic renal diseases as well as AKI.15,16 Furthermore, experimental study demonstrated suPAR overexpression resulted in severe AKI characterized by enhanced generation of mitochondrial superoxide and energetic demand.17
Considering the role of suPAR in oxidative damage and inflammation, we hypothesized whether high suPAR level is associated with high incidence of CI-AKI. The present research aims to evaluate the relationship between suPAR and CI-AKI in patients undergoing PCI and assess the predictive value of suPAR for CI-AKI induced by PCI.
Materials and Methods
Study Design and Protocol
The present study is a prospective study performed in Zhongda Hospital affiliated to Southeast University. Three hundred and ninety-nine patients underwent PCI were admitted from June 2020 to June 2021. The study was approved by the Ethics Committee of Zhongda Hospital and all participants provided written informed consent. Patients aged over 18 and underwent PCI procedure were enrolled in the research. The exclusion criteria were as follows: 1) patients with cardiogenic shock or hemodynamic instability; 2) allergy history of iodine contrast agent; 3) chronic renal insufficiency with eGFR < 15 mL/min/1.73 m2 or patients receiving maintenance hemodialysis; 4) received enhanced computed tomography, magnetic resonance imaging, or vascular angiography procedures within previous 2 weeks before admission; 5) suffered acute kidney insufficiency or history of taking nephrotoxic drugs during the past 2 weeks; 6) patients with autoimmune diseases, severe liver/kidney dysfunction, severe infectious disease; and malignant tumor. Patients with incomplete clinical data were also excluded. The clinical registration number is ChiCTR2100050487.
Coronary Angiography and Percutaneous Coronary Intervention
Seldinger puncture method was utilized to puncture the radial or right femoral artery. All included patients in the research were subjected to PCI by at least 2 experienced interventional operators. Use of standard hydration protocols and the type of stents were determined by the interventional physician, and a minimum required amount of nonionic, low-osmolality contrast agents were used during the procedure. The standard hydration protocol is as followed: 0.9% NaCl was administered intravenously in patients with according to guidelines (1.0 mL/kg/h during 12 h before and 12 h after contrast administration).18
Definition of CI-AKI
Serum creatinine (Scr) increased by 1.5 times or more over the baseline value within 7 days after contrast medium exposure; or serum creatinine level increased by at least 0.3 mg/dl (26.5 μmol/l) over the baseline value within 48 hours after contrast medium exposure; or a urinary volume of less than 0.5 mL/kg/h and persists for at least 6 hours after exposure.2
Measurement of suPAR and Serum Creatinine
Fasting venous blood samples for suPAR were collected on admission before the angiology procedure and stored at −80°C. Serum concentrations of suPAR were measured through a commercially enzyme-linked immunosorbent assay (ELISA) kit (suPARnostic® Elisa kit; ViroGates, Copenhagen, Denmark) according to the manufacturer’s protocol. Preoperative and postoperative Scr levels were measured within one week after exposure of contrast agent.
Statistical Analysis
Data were analyzed through SPSS 19.0 statistical software, normally and non-normally distributed numerical data were presented as mean±standard deviation and median [25–75% interquartile range], respectively. In addition, independent sample t-test or Mann–Whitney U-test was performed for comparison of normally and non-normally distributed data. Classification data were expressed as frequencies and percentages, and compared using the χ2 and Fisher exact tests. Univariate and multivariate logistic regression analysis were utilized for identification of independent risk factor of CI-AKI.
The predictive value of suPAR for CI-AKI and the optimal cut-off value were evaluated by receiver operator characteristic (ROC) curve. P < 0.05 was considered a statistically significant difference.
Results
Baseline Characteristics of CI-AKI and Non-CI-AKI Groups
Three hundred and ninety-nine patients who underwent PCI were enrolled consecutively. The research population included 258 male and 141 female patients with an average age of 65±13. CI-AKI was observed in 65 patients (16.3%). The baseline characteristics of included population are summarized in Table 1. Patients who developed CI-AKI are older, had higher incidence of diabetes, higher CKD, higher triple-vessel disease, higher volume of contrast media, higher baseline serum creatinine, lower hydration rates, lower eGFR level, lower left ventricular ejection fraction (LVEF) compared with those who do not developed CI-AKI (p < 0.05). Interestingly, suPAR level was significantly higher in subjects suffered CI-AKI compared with non-CI-AKI population (p < 0.001). No significantly statistical differences were found in other demographic data, hematological parameters, coronary angiography data and medications in patients with/without CI-AKI (p ≥ 0.05).
 |
Table 1 Baseline Characteristics Between CI-AKI Group and Non-CI-AKI Group |
SuPAR is an Independent Risk Factor for CI-AKI
Univariate logistic regression analysis identified the following factors independently associated with CI-AKI (Table 2): age, diabetes history, CKD history, LVEF, hydration, baseline serum creatinine, baseline eGFR, suPAR, triple vessel disease, volume of contrast media. Multivariate logistic analysis displayed the following independent risk factors for the development CI-AKI: diabetes (OR = 2.141, 95% CI = 1.491–2.679, p = 0.045), LVEF (OR = 0.866, 95% CI = 0.764–0.924 p = 0.039), hydration (OR = 0.703, 95% CI = 0.528–0.817, p = 0.035), baseline eGFR (OR = 0.692, 95% CI = 0.507–0.789, p = 0.014), suPAR (OR = 2.694, 95% CI = 2.379–2.928, p = 0.009), volume of contrast media (OR = 2.245, 95% CI = 1.683–2.294, p = 0.028) (Table 2). In addition, Figure 1 presents a forest plot of multivariate predictors for CI-AKI more intuitively.
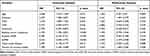 |
Table 2 Univariate and Multivariate Logistic Regression for the Independent Risk Factors of CI-AKI in Patients Undergoing PCI |
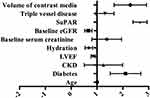 |
Figure 1 Forest plot of multivariate predictors for CI-AKI. |
ROC Curve Analysis of suPAR for CI-AKI
ROC curve analysis was utilized for evaluating the predictive value of suPAR in CI-AKI. Figure 2 shows the AUC (area under the curve) of suPAR is 0.765 (95% CI = 0.696–0.834, p = 0.035). The optimal cut-off value is 3.305 ng/mL, the corresponding sensitivity and specificity are 63.1% and 82.3%, respectively (Figure 2, Table 3). We explored the predictive value of the model incorporating all the independent risk factors selected through multivariate regression analysis (model 1), the results presented in Figure 2 and Table 3 indicate that model 1 significantly improved the predictive value for CI-AKI, the AUC reached 0.905 (95% CI = 0.848–0.952, p = 0.006). Interestingly, the model incorporating all the independent risk factors except for suPAR (model 2) had relatively lower predictive value for CI-AKI compared with model 1.
 |
Table 3 Risk Discrimination Metrics for CI-AKI |
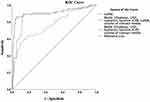 |
Figure 2 The ROC curve of suPAR and models for predicting CI-AKI in patients undergoing PCI. |
Discussion
The current prospective study for the first time to our knowledge demonstrated that higher suPAR level was associated with increased risk for developing CI-AKI and identified suPAR as an independent risk factor for CI-AKI in patients undergoing PCI. The ROC curve shows a fine predictive capacity of suPAR, and the prediction model included suPAR exerts as an outstanding predictor for CI-AKI in patients undergoing PCI.
Despite the advancements in the field of interventional cardiology and increased awareness of CI-AKI, iodinated contrast remains to pose a risk of CI-AKI, especially for patients at high risk. It was reported CI-AKI occurs in 7–18% of percutaneous cardiac procedures and it is closely related to poor prognosis.19 Multiple blood biomarkers and risk-stratification models have been proposed for evaluation of the risk of develop CI-AKI, and they might help evaluate the diagnosis of CI-AKI before the change of serum creatinine and eGFR. Incorporation of these new biomarkers could increase its prognostic capacity and lower the cost of trials.20 However, there is still a long way to go before clinical application due to limited research population and unknown crucial variables before the procedure, such as the volume of contrast media.21 The current investigation indicated increased suPAR level is closely associated with higher incidence of developing CI-AKI, and it might become a promising noninvasive biomarker for CI-AKI in the perioperative setting.
The exact pathophysiological mechanisms underlying CI-AKI have not been completely elucidated. Enhanced metabolic demand causes renal medulla susceptible to the vasoconstrictor effects of contrast media due to the low partial oxygen pressure. Contrast agents directly contribute to apoptosis and necrosis of tubular epithelial cells, leading to function loss. The release of vasoactive agents including endothelin, nitric oxide, and prostaglandins result in ischemic injury.22,23 More importantly, new findings have established the requisite role of epithelial inflammatory caspases24 and immune sensor NLRP325 in CI-AKI model, which might be related to the increased level of suPAR.
Previous reports have indicated suPAR levels are correlated with disease severity, readmission and mortality rate in patients admitted to acute care.26 Significant association has been found between increased plasma suPAR and various kinds of cardiovascular diseases, renal diseases and other pathologies.27 Salim reported elevated suPAR was independently associated with the incidence of chronic kidney disease.13 Emerging evidence has indicated suPAR is involved in the underlying mechanisms of diabetic nephropathy,28 lupus nephritis,29 and focal segmental glomerulosclerosis30 through a variety of molecular mechanisms, such as activation of αVβ3 integrin, modification of CD40 autoantibodies and acid sphingomyelinase-like phosphodiesterase 3b.31–33 In terms of AKI, our findings are largely consistent with the results from a clinical study enrolled 107 patients underwent cardiac surgery, indicating that preoperative suPAR level might become a predictive biomarker for AKI.15 Mechanistically, previous experimental evidence has shown suPAR exposure contributed to higher cellular energetic demand and oxidative stress, leading to injury of proximal tubules. SuPAR inhibitors remarkably alleviated the deterioration of kidney function caused by iohexol and reversed the bioenergetic changes in HK-2 cells.17
It was suggested that suPAR could be freely filtered by kidney and it is a biomarker beyond sensitive filtration marker. The association of suPAR with CI-AKI remained significant after adjustment for eGFR, indicating suPAR reflects more than reduced filtration but a characteristic of renal disease.34 In addition, increased suPAR concentration might be related to the potential tissue damage caused by systemic chronic inflammation. However, whether suPAR is involved in the pathogenesis of CI-AKI and the underlying mechanism remains unexplored.35 There are several crucial advantages for suPAR acting as a biomarker of CI-AKI. SuPAR is a highly stable biomarker and the serum concentration of suPAR is independent of diets, drugs, inflammation and the collection time throughout the day.36 Secondly, suPAR has a fine prognostic value for CI-AKI. Early monitoring of SuPAR could help risk stratification for patients undergoing PCI and guide clinical evaluations and treatment.
There are several limitations of the current research. Firstly, this is a single-center prospective study and the sample size is relatively small. Furthermore, the findings of the present study need to be validated through more large-scale prospective clinical research to ensure its consistency of observed associations. In addition, suPAR is not a commonly used detection indicator in clinical practice, and its clinical applicability is limited to some extent.
Conclusion
In conclusion, elevated suPAR in patients undergoing PCI was independently associated with higher risk for developing CI-AKI. suPAR might become a candidate plasma biomarker and included in the risk stratification model for CI-AKI in clinical application. Further experimental studies need to be carried out to investigate the underlying role of suPAR in CI-AKI and even explore potential novel therapeutic approaches for CI-AKI.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participant
This study was approved by the Ethics Committee of Zhongda Hospital, Medical School of Southeast University. All participants provided informed consent to participate in this research and that it was conducted in accordance with the Declaration of Helsinki.
Acknowledgment
This study was supported by grants from the National Natural Science Foundation of China (81600227, 81970237), Jiangsu Provincial Key Medical Discipline (Laboratory ZDXKA2016023) and Jiangsu Provincial Key Research and Development Program (No. BE2016785).
Disclosure
The authors declare that they have no competing interests concerning the paper.
References
1. Giacoppo D, Madhavan MV, Baber U, et al. Impact of contrast-induced acute kidney injury after percutaneous coronary intervention on short- and long-term outcomes: pooled analysis from the HORIZONS-AMI and ACUITY Trials. Circ Cardiovasc Interv. 2015;8(8):e002475. doi:10.1161/CIRCINTERVENTIONS.114.002475
2. Fliser D, Laville M, Covic A, et al. A European Renal Best Practice (ERBP) position statement on the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines on acute kidney injury: part 1: definitions, conservative management and contrast-induced nephropathy. Nephrol Dial Transplant. 2012;27:4263–4272.
3. Weisbord SD, Chen H, Stone RA, et al. Associations of increases in serum creatinine with mortality and length of hospital stay after coronary angiography. J Am Soc Nephrol. 2006;17:2871–2877.
4. James MT, Ghali WA, Tonelli M, et al. Acute kidney injury following coronary angiography is associated with a long-term decline in kidney function. Kidney Int. 2010;78:803–809.
5. Amin AP, Bach RG, Caruso ML, Kennedy KF, Spertus JA. Association of variation in contrast volume with acute kidney injury in patients undergoing percutaneous coronary intervention. JAMA Cardiol. 2017;2:1007–1012.
6. Jaroszyński A, Zaborowski T, Głuszek S, et al. Heat shock protein 27 is an emerging predictor of contrast-induced acute kidney injury on patients subjected to percutaneous coronary interventions. Cells. 2021;10:684.
7. Seibert FS, Heringhaus A, Pagonas N, et al. Dickkopf-3 in the prediction of contrast media induced acute kidney injury. J Nephrol. 2021;34:821–828.
8. Hahm E, Wei C, Fernandez I, et al. Bone marrow-derived immature myeloid cells are a main source of circulating suPAR contributing to proteinuric kidney disease. Nat Med. 2017;23:100–106.
9. Luo S, Coresh J, Tin A, et al. Soluble urokinase-type plasminogen activator receptor in black Americans with CKD. Clin J Am Soc Nephrol. 2018;13:1013–1021.
10. Hodges GW, Bang CN, Wachtell K, Eugen-Olsen J, Jeppesen JL. suPAR: a new biomarker for cardiovascular disease? Can J Cardiol. 2015;31:1293–1302.
11. Backes Y, van der Sluijs KF, Mackie DP, et al. Usefulness of suPAR as a biological marker in patients with systemic inflammation or infection: a systematic review. Intensive Care Med. 2012;38:1418–1428.
12. Jhee JH, Nam BY, Lee CJ, et al. Soluble urokinase-type plasminogen activator receptor, changes of 24-hour blood pressure, and progression of chronic kidney disease. J Am Heart Assoc. 2021;10:e017225.
13. Hayek SS, Sever S, Ko YA, et al. Soluble urokinase receptor and chronic kidney disease. N Engl J Med. 2015;373:1916–1925.
14. Sehestedt T, Lyngbæk S, Eugen-Olsen J, et al. Soluble urokinase plasminogen activator receptor is associated with subclinical organ damage and cardiovascular events. Atherosclerosis. 2011;216:237–243.
15. Mossanen JC, Pracht J, Jansen TU, et al. Elevated soluble urokinase plasminogen activator receptor and proenkephalin serum levels predict the development of acute kidney injury after cardiac surgery. Int J Mol Sci. 2017;18:1662.
16. Dande RR, Peev V, Altintas MM, Reiser J. Soluble urokinase receptor and the kidney response in diabetes mellitus. J Diabetes Res. 2017;2017:3232848.
17. Hayek SS, Leaf DE, Samman Tahhan A, et al. Soluble urokinase receptor and acute kidney injury. N Engl J Med. 2020;382:416–426.
18. Nijssen EC, Rennenberg RJ, Nelemans PJ, et al. Prophylactic hydration to protect renal function from intravascular iodinated contrast material in patients at high risk of contrast-induced nephropathy (AMACING): a prospective, randomised, Phase 3, controlled, open-label, non-inferiority trial. Lancet. 2017;389:1312–1322.
19. Ronco F, Tarantini G, McCullough PA. Contrast induced acute kidney injury in interventional cardiology: an update and key guidance for clinicians. Rev Cardiovasc Med. 2020;21:9–23.
20. Parikh CR, Liu C, Mor MK, et al. Kidney biomarkers of injury and repair as predictors of contrast-associated AKI: a substudy of the PRESERVE trial. Am J Kidney Dis. 2020;75:187–194.
21. Mehran R, Dangas GD, Weisbord SD. Contrast-associated acute kidney injury. N Engl J Med. 2019;380:2146–2155.
22. Mamoulakis C, Tsarouhas K, Fragkiadoulaki I, et al. Contrast-induced nephropathy: basic concepts, pathophysiological implications and prevention strategies. Pharmacol Ther. 2017;180:99–112.
23. Pistolesi V, Regolisti G, Morabito S, et al. Contrast medium induced acute kidney injury: a narrative review. J Nephrol. 2018;31:797–812.
24. Zhang Z, Shao X, Jiang N, et al. Caspase-11-mediated tubular epithelial pyroptosis underlies contrast-induced acute kidney injury. Cell Death Dis. 2018;9:983.
25. Lau A, Chung H, Komada T, et al. Renal immune surveillance and dipeptidase-1 contribute to contrast-induced acute kidney injury. J Clin Invest. 2018;128:2894–2913.
26. Rasmussen LJ, Ladelund S, Haupt TH, et al. Soluble urokinase plasminogen activator receptor (suPAR) in acute care: a strong marker of disease presence and severity, readmission and mortality. A retrospective cohort study. Emerg Med J. 2016;33:769–775.
27. Desmedt S, Desmedt V, Delanghe JR, Speeckaert R, Speeckaert MM. The intriguing role of soluble urokinase receptor in inflammatory diseases. Crit Rev Clin Lab Sci. 2017;54:117–133.
28. Theilade S, Lyngbaek S, Hansen TW, et al. Soluble urokinase plasminogen activator receptor levels are elevated and associated with complications in patients with type 1 diabetes. J Intern Med. 2015;277:362–371.
29. Hessol NA, Schneider M, Greenblatt RM, et al. Retention of women enrolled in a prospective study of human immunodeficiency virus infection: impact of race, unstable housing, and use of human immunodeficiency virus therapy. Am J Epidemiol. 2001;154:563–573.
30. Wei C, El Hindi S, Li J, et al. Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis. Nat Med. 2011;17:952–960.
31. Maile LA, Busby WH, Gollahon KA, et al. Blocking ligand occupancy of the αVβ3 integrin inhibits the development of nephropathy in diabetic pigs. Endocrinology. 2014;155:4665–4675.
32. Delville M, Sigdel TK, Wei C, et al. A circulating antibody panel for pretransplant prediction of FSGS recurrence after kidney transplantation. Sci Transl Med. 2014;6:256ra136.
33. Yoo TH, Pedigo CE, Guzman J, et al. Sphingomyelinase-like phosphodiesterase 3b expression levels determine podocyte injury phenotypes in glomerular disease. J Am Soc Nephrol. 2015;26:133–147.
34. Iversen E, Houlind MB, Kallemose T, et al. Elevated suPAR is an independent risk marker for incident kidney disease in acute medical patients. Front Cell Dev Biol. 2020;8:339.
35. Furman D, Campisi J, Verdin E, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019;25:1822–1832.
36. Andersen O, Eugen-Olsen J, Kofoed K, Iversen J, Haugaard SB. Soluble urokinase plasminogen activator receptor is a marker of dysmetabolism in HIV-infected patients receiving highly active antiretroviral therapy. J Med Virol. 2008;80:209–216.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
