Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
The Predictive Value of Endothelial Inflammatory Markers in the Onset of Schizophrenia
Authors Radu G , Luca C , Petrescu L, Bordejevic DA , Tomescu MC , Andor M , Cîtu I , Mavrea A , Buda V , Tomescu C, Borcan F , Dehelean L
Received 28 November 2019
Accepted for publication 29 January 2020
Published 24 February 2020 Volume 2020:16 Pages 545—555
DOI https://doi.org/10.2147/NDT.S240349
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Gabriela Radu,1,2,* Constantin Luca,3,* Lucian Petrescu,3,* Diana Aurora Bordejevic,2,3,* Mirela Cleopatra Tomescu,1,2 Minodora Andor,1,2 Ioana Cîtu,1,2 Adelina Mavrea,1,2 Valentina Buda,4 Cătălin Tomescu,1,2 Florin Borcan,4 Liana Dehelean5
1Department of Internal Medicine I, Cardiology Clinic, “Victor Babeş” University of Medicine and Pharmacy, Timişoara, Romania; 2City Emergency Hospital Timisoara, Timişoara, Romania; 3Department of Cardiology, “Victor Babeş” University of Medicine and Pharmacy, Timişoara, Romania; 4Department of Pharmacology and Clinical Pharmacy, “Victor Babeş” University of Medicine and Pharmacy, Timişoara, Romania; 5Department of Neurosciences and Psychiatry, “Victor Babeş” University of Medicine and Pharmacy, Timişoara, Romania
*These authors contributed equally to this work
Correspondence: Valentina Buda 2 nd E. Murgu Square, Timişoara 300041, Romania
Tel +40755100408
Email [email protected]
Purpose: This study aimed to assess the serum levels of intracellular adhesion molecule (sICAM-1), and vascular cell adhesion molecule (sVCAM-1), in the first psychotic episode schizophrenia (SZ) patients, before and after six months of antipsychotic treatment.
Patients and Methods: The study included 50 patients with a first hospitalization for SZ and 50 healthy control subjects that were patient-matched regarding age, gender, body mass index and smoking status. The evaluation included the presence of cardiovascular risk factors, measurements of systolic and diastolic blood pressure, body mass index, smoking status, ankle-brachial index, carotid intima-media thickness, and echocardiography. The Brief Psychiatric Rating Scale (BPRS) score was calculated for the patients. The plasma levels of fasting glucose, total cholesterol, LDL-cholesterol, HDL-cholesterol, triglycerides, sICAM-1 and sVCAM-1 were determined at baseline in all subjects and after six months of antipsychotic treatment. Thirty patients (60%) were treated with olanzapine and 20 (40%) with risperidone.
Results: The average age of patients experiencing their first episode of SZ was 29.7± 6.6 years, and 23 (46%) were men. The initial sICAM-1 levels of the patients were lower than those of the control group (P< 0.0001), and increased after treatment (P=0.02), but remained lower than in the healthy controls (P=0.026). The initial levels of sVCAM-1 levels were higher in the patients (P< 0.0001) and decreased after treatment (P< 0.0001) to values that were similar to those of the control group (P=0.39). The only independent predictor of a baseline BPRS over 120 was the baseline sVCAM-1 level (P< 0.0001). Antipsychotic treatment induced significant decreases in BPRS score (P< 0.0001), in systolic (P=0.005) and diastolic (P< 0.0001) blood pressure, in HDL-c (P=0.02), as well as significant increases in blood glucose (P< 0.01) and LDL-c (P< 0.001), with no differences between olanzapine and risperidone.
Conclusion: In the patients experiencing an FEP of SZ, the levels of sICAM-1 were lower, while the levels of sVCAM-1 were higher than in the healthy control subjects. The antipsychotics used in the treatment of schizophrenia increased sICAM-1 and decreased sVCAM. The baseline level of sVCAM-1 was an independent predictor of a BPRS score > 120 at baseline.
Keywords: sICAM-1, sVCAM-1, schizophrenia, inflammation, atherosclerosis, cardiac dysfunction
Introduction
Inflammation and endothelial dysfunction seem to be common pathways of atherosclerosis and schizophrenia (SZ) and a possible explanation of the increased cardiovascular risk of schizophrenia patients. Early intervention is known to improve outcomes in schizophrenia.1 Anti-psychotic naïve patients at the first episode of psychosis (FEP), usually at late adolescent or early adult years, are preferred when evaluating the prognostic factors of the disease, because, at this stage, the number of variables related to chronicity and medication is lower.2 The effects of antipsychotic drugs seem to be more pronounced in the first months of treatment.3 But, it is important to note that inflammatory, oxidative stress and metabolic disturbances may precede the FEP and initiation of antipsychotic treatment.4–6 There is also growing evidence regarding metabolic alterations induced by antipsychotic medication that increase the cardiovascular risk of the patients. Circulating Vascular Cell Adhesion molecule-1 (sVCAM-1) and Intercellular Adhesion Molecule-1 (sICAM-1) are well-known biomarkers of endothelial inflammation and dysfunction that are associated with an increased risk of atherosclerosis.7,8 Many studies have shown aberrant levels of a range of inflammatory markers in SZ patients.9–11 Decreased levels of sICAM-1 in SZ could represent the reduced activity of the type-1 immune system,12–14 but the role of inflammation and immune activation in severe mental disorders is still poorly understood.
Echocardiography, carotid ultrasonography, and ankle-brachial index (ABI) measurement are known to be accurate methods of detecting subclinical atherosclerosis and risk stratification.15
This exploratory study aimed to determine the best methods to detect the presence and progression of endothelial inflammation and subclinical atherosclerosis in antipsychotic-naïve SZ patients at first psychotic event and to determine the differences from healthy individuals, at baseline and after 6 months of antipsychotic treatment.
Materials and Methods
Subjects Selection
50 patients were selected between January 2018 and May 2019 among those who were hospitalized with a diagnosis of first-episode SZ.
A control group of 50 healthy volunteers without physical or psychiatric illness were selected. The healthy control group consisted of individuals selected to be gender-, ethnicity-, age-, smoking status- and body mass index (BMI)-matched with the subjects of the patient group, with no history of alcohol/drug abuse and without a diagnosis or treatment for any acute or chronic disease.
Clinical evaluation and blood samples were collected before any treatment was given, within the first 24 hrs after admission. Tests for pregnancy were done in all female patients.
The inclusion criteria of the SZ patients were: the first hospitalization for SZ, age ≥18 years, ability to give informed consent, no significant disease detected in the internal medicine examination, no former diagnosis or treatment for any chronic cardiovascular, digestive, respiratory, neurological, endocrinological, hematological or renal condition. Exclusion criteria were: pregnant women, alcohol/drug abuse, acute inflammatory diseases, neoplasms, inability to comply with study procedures, former diagnosis of any serious mental illness.
All subjects provided written informed consent to participate in the study. The study protocol, which was written according to the Helsinki Declaration, was approved by the Ethics Committee of the Emergency Clinical City Hospital Timisoara. Before obtaining the consent, the patients were given sufficient time and opportunity to inquire about the details of the study and decide to study participation or not.
Subjects Evaluation
The diagnosis of FEP SZ was established by expert clinicians according to the Diagnostic and Statistical Manual of Mental Disorders.16 The severity of symptoms was assessed using the BPRS-E scores (Brief Psychiatric Rating Scale – Expanded version 4.0)17
Clinical evaluation included the registration of data regarding age, gender, smoking status, calculation of body mass index, measurement of systolic and diastolic blood pressure. Blood pressure measurements were performed after 5 mins of rest at the right brachial artery with the subject in a supine position. Blood pressure was expressed as the mean value of three measurements over 30 mins. The ankle-brachial index (ABI) was ABI was measured by a single observer in both groups after a 15-mins rest in a supine position. Systolic pressures of brachial arteries of both arms and systolic pressures of both ankles were measured, using a contour-wrapped 12 cm cuff and an 8 MHz Doppler probe. The cuff was inflated to above the audible systolic pressure (for 20 mm Hg) in each artery. Then, the cuff was slowly deflated and the first audible sound by the Doppler probe was recorded as systolic pressure. Six systolic artery pressures (right arm brachial artery, left arm brachial artery, right dorsalis pedis artery, left dorsalis pedis artery, right tibialis posterior artery, left tibialis posterior artery) were measured. Of the same-side dorsalis pedis and tibial posterior artery pressures, the highest one was written on the numerator as the systolic ankle pressure. The highest arm systolic pressure was written on the denominator, and the ratio of ankle systolic pressure to brachial artery systolic pressure was calculated. The same calculation was performed for the other ankle. The lowest ratio was accepted as the ABI calculated as the ratio between systolic blood pressure measured at the brachial artery and the systolic blood pressure measured at the ankle.
Echocardiographic evaluation was done within the first 48 hrs of hospitalization, using a VIVID S5 echocardiograph. Mono- (M) and bidimensional (2D), pulsed and continuous Doppler measurements were done. Left ventricular ejection fraction (LVEF) was calculated using the Simpson method, by evaluating the end-diastolic volume and left ventricular end-systolic volume. After assessing antegrade mitral flow, we determined the ratio between early (E) and late (atrial-A) ventricular filling velocity (E/A ratio). The same echocardiographic device was used to determine carotid intima-media thickness (CIMT). To measure CIMT, patients were placed in a supine position and asked to turn their heads to the opposite direction of the carotid artery and to keep their necks extended. Measurements were performed at a distance of 1 cm from the bifurcation of the internal and external carotid artery branches. CIMT was measured in the anterior, posterior, and lateral projections. The mean wall thickness of the common carotid artery was used as the key variable for statistical analysis because of its strong association with cardiovascular risk factors.18
During the study, echocardiography, ABI, and CIMT were performed by the same certified cardiologist. Blood collection was performed in a fasting state and a temperature-controlled room. Venous blood samples were collected after 15 mins of rest following 12 or more hours of fasting. Samples were immediately placed on ice until analysis. Blood glucose, total cholesterol, high-density lipoprotein (HDL)-cholesterol, low-density lipoprotein (LDL)-cholesterol, and triglycerides were measured using routine laboratory methods at the hospital with standard enzymatic procedures.
The blood samples for sICAM-1 and sVCAM-1 determination were separated with an ultracentrifuge, and the serum samples were kept between –20 and –80°C until they were processed. The measurements were done at a central laboratory with a micro ELISA method, using the QuantikineELISA Human ICAM-1/CD54 Allele-specific Immunoassay for the quantitative determination of serum (s) ICAM-1 and Quantikine® ELISA Forty Assay. For the quantitative determination of sVCAM-1.
All patients were followed up for 6 months. After 6 months of antipsychotic treatment with either olanzapine or risperidone, all determinations were repeated in the patients. Standard doses of antipsychotic therapy were used (6 mg/day for risperidone, 10 mg/day for olanzapine). The patients` adherence to medication was checked using the pill counts method combined with the use of the Medication Adherence Rating Scale (MARS).19,20 The measurements for the control group were done only at the initiation of the study.
Statistical Analysis
The statistical analysis was performed using MedCalc Statistical Software version 12.7.7 (Ostend, Belgium). Continuous variables are presented as mean ± standard deviation (SD), and categorical as number (n) and percentage (%). The patient groups were compared using the chi-square test for the categorical variables and the t-test for the continuous ones. For the longitudinal follow-up paired comparison testing was used. Parameters with statistically significant risk in univariate analysis were included in the multivariate analysis by logistic regression. For the independent predictors identified by multivariate logistical regression, receiver operating characteristic (ROC) analysis was performed. Values of P <0.05 were considered statistically significant. The Bonferroni method was used to counteract the problem of multiple comparisons, according to the number of tests performed.
Results
The study group consisted of 100 subjects, 50 FEP antipsychotic–naïve SZ patients and 50 healthy controls that were selected to be age-, gender-, BMI- and smoking status-matched with the SZ patients.
Demographic and other relevant data are summarized in Table 1.
At baseline, we found that in the patient group the levels of sICAM-1 were significantly lower while those of sVCAM-1 were significantly higher than in the healthy control group (p<0.0001). SZ patients had echocardiographic evidence of left ventricular diastolic dysfunction, as evidenced by the significant lower E/A ratio at ante grade transmitral Doppler flow examination. This marker of subclinical cardiac dysfunction was not found in the healthy control group.
The frequency distribution of the BPRS score is presented in Figure 1 The mean total score was 120.2 ± 15 corresponding to a level of moderately severe symptoms. The median value of the BPRS score was 120.5. The percentage of cases with a BPRS-E score of over 140 was 8%.
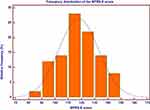 |
Figure 1 The frequency distribution of the BPRS score. Abbreviation: BPRS-E, the Brief Psychiatric Rating Scale-Expanded version. |
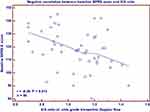
The BPRS score before antipsychotic treatment had a significantly negative correlation with the female sex (r= −0.48, 95% CI: −0.67 to −0.23, P<0.001) (Figure 2), and the E/A ratio at ante grade transmitral Doppler flow (Figure 3) (P=0.012), respectively, a significantly positive correlation with the baseline sVCAM-1 levels (P<0.01) (Figure 4).
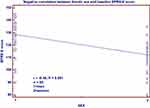 |
Figure 2 Negative correlation between the female sex baseline values of the BPRS-E score. Abbreviation: BPRS, the Brief Psychiatric Rating Scale-Expanded version. |
We analyzed the predictive parameters for a baseline BPRS score over the median value of 120. The variables associated with a BPRS score > 120 were, in univariate analysis: the gender (r= –0.40, P=0.003. 95% CI: −0.6125 to −0.1402), the E/A ratio (r=–0.39, P=0.005, 95% CI: –0.6045 to –0.1262), and the baseline value of sVCAM-1 (r=0.60, P<0.0001, 95% CI: 0.3913 to 0.7553). In multivariate logistic regression, the only independent predictor for a BPRS score >120 at FEP of SZ was the baseline value of sVCAM-1. For this parameter, we performed the receiver operating characteristic (ROC) analysis and analyzed the area under the curve (AUC) (AUC=0.872, 95% CI 0.776 to 0.964, P< 0.001), as shown in Figure 5.
30 (60%) of the patients received antipsychotic treatment with olanzapine, while 20 (40%) received risperidone, at standard doses (6 mg/day for risperidone, 10 mg/day for olanzapine). The evaluation at 6 months after antipsychotic treatment (Table 2) showed a significant decrease in systolic (P=0.005) and diastolic (P=0.0001) blood pressure, in the BPRS score (P<0.0001), in sVCAM levels (P<0.0001), and in HDL-cholesterol levels (P=0.02). We also observed significant increases in blood glucose (P<0.01), in LDL-cholesterol (P<0.001), and in sICAM-1 levels (P=0.02).
 |
Table 2 Results at 6 Months Follow-Up in the Patient Group |
We compared the levels of sICAM-1 and sVCAM-1 in the control group at baseline and the patient group at baseline and after 6 months of antipsychotic treatment (Figure 6). We observed that sICAM-1 levels were significantly lower in the SZ patients compared with healthy controls, both at baseline (P<0.0001), and after 6 months of therapy (P=0.0.26). In contrast, the sVCAM-1 levels were at baseline significantly higher in SZ patients than in the healthy controls (P<0.0001), and decreased after six months of antipsychotic therapy (P<0.0001), reaching the baseline level of the healthy controls (P=0.39).
We also analyzed the differences in the parameters that changed significantly at 6 months according to the type of antipsychotic therapy (olanzapine or risperidone) but we found no significant differences among the two antipsychotic therapy groups, neither before nor after the 6 months therapy, as shown in Table 3.
 |
Table 3 Comparison Between the Olanzapine and Risperidone Treated Patients |
Discussion
SZ is a complex disorder, with an etiology that involves multiple genes and a variety of environmental risk factors. Despite a high heritability rate, very little is known about the underlying biological mechanisms. Probably, several molecular pathways are involved. The current treatment options only offer symptom relief and are often accompanied by adverse effects. The first-generation antipsychotics (FGA) act by antagonizing dopamine (D2) receptors and have several adverse effects such as dyskinesia, akinesia, and parkinsonism. The second-generation (SGA) antipsychotics have an antagonizing effect on serotonin receptors (5-HT2) in addition to dopamine receptors. They have less extrapyramidal side effects but are associated with dyslipidemia, hyperglycemia and, overweight which increase the incidence of cardiovascular disease. Endothelial inflammation and dysfunction promote atherosclerosis and cardiovascular disease. Interestingly, a state of mental stress has been found to induce endothelial dysfunction in otherwise healthy individuals.21 As we know, the blood-brain-barrier consists of endothelial cells. Increased inflammation and endothelial cell activations have been reported in SZ but the relationships between these factors are unknown.
In this study, we investigated the cellular adhesion molecules sICAM-1 and sVCAM-1 which are thought to be biological markers in the progression and prognosis of endothelial inflammation and atherosclerosis in humans, in patients with SZ at their first psychotic episode. They were measured before and after 6 months of antipsychotic treatment. We compared the baseline values with those found in healthy individuals matched for demographic characteristics, body mass index, and smoking habits and found that sICAM-1 was significantly lower while sVCAM-1 was significantly higher in SZ patients than in the healthy controls (P<0.0001).
Having a broad tissue distribution, sICAM-1 increase gives general information on the overall level of inflammation; on the other side, sVCAM-1 is more restricted to endothelium and dendritic cell populations, being of more particular use in estimating endothelial dysfunction.
sICAM-1 acts as an important costimulatory molecule for lymphocyte activation, especially for T cells and monocytes. While increased levels of sICAM-1 have been observed in inflammatory and cell-mediated autoimmune disorders, decreased levels of sICAM-1 have been described in migraine.22 In a study published by Schwarz,23 sICAM-1 levels of 36 patients with SZ were investigated before antipsychotic therapy was initiated, and at the end of the acute phase, to observe the possible effects of antipsychotic therapy. The serum levels of sICAM-1 in patients with SZ were significantly lower in patients with SZ before treatment, in comparison with the control group, and the increase after treatment was not significant. The authors have suggested that this may be related to the weak immunological systems of patients with SZ. In contrast to the findings of Schwarz, we detected a significant increase in sICAM-1 after six months of antipsychotic treatment (P=0.02). A possible explanation could be the short time interval between the two determinations of sICAM-1 in the study of Schwartz and collaborators, both determinations being done during the hospitalization for the same psychotic episode. The duration of hospitalization is not indicated. Our results showing a significant increase are concordant to those found by Meyer.24 In this randomized study comparing the effects of multiple antipsychotic therapies on systemic inflammatory changes, the authors found an increase in sICAM-1 levels at three months of antipsychotic treatment. In particular, olanzapine was found to induce a more important sICAM-1 increase when compared to risperidone, but after applying the Bonferroni correction, the difference was no more significant. In our study, we found no differences between olanzapine and risperidone on the increase of sICAM-1 after six months of treatment at standard doses (P=0.25).
While sICAM-1 plays a role in endothelial activation in the initiation of atherosclerosis, sVCAM-1 becomes more active during the formation of the atheroma plaque and smooth muscle proliferation. VCAM-1 also plays a role in the immune reactions of atherosclerosis.25 Thus, the level of VCAM is more important to be determined in SZ, being a biological marker of both immune reactions and the development of atherosclerosis. The increased values of sVCAM-1 in FEP SZ patients could be explained by at least two causality chains. First, the time leading up to the first hospitalization is generally filled with stressful experiences related to the prodromal symptoms, and finally emergent symptoms. Even the first hospitalization represents a stressful experience. Alternatively, the increased sVCAM-1 could be secondary to the changes in the endothelial cells of the blood-brain barrier in SZ.
Similarly, antipsychotic drugs could directly affect biological markers, or their action could affect the patient–environment interaction. These distinctions have different implications for mechanism and treatment. It could be suggested that second-generation antipsychotics, which have effects especially on the serotonin 5-HT2a receptors, might cause a change in the levels of sVCAM because 5-HT2a receptors are predominantly present on platelets and smooth muscle cells. The significant decrease in levels of initially high sVCAM-1 at the 6th month of treatment might be a result of the second-generation antipsychotics (especially 5-HT2a antagonism).26
Regarding the effects of antipsychotic medication on other biological cardiovascular risk factors, we found that both olanzapine and risperidone significantly increased the levels of blood glucose (P<0.01) and of LDL-cholesterol (P<0.001), and decreased the levels of HDL-cholesterol (P=0.02) after 6 months of therapy, with no significant differences among them. We found no significant changes in triglycerides level (P=0.96).
The effects of antipsychotics on blood glucose and lipid levels were previously reported.27,28
In a study published by Attux and collaborators,29 blood lipids were measured initially and after 6 months in 44 patients with a diagnosis of first-episode SZ. LDL-cholesterol showed an increase while the HDL cholesterol levels showed a decrease after 6 months. These results are concordant with those found in our study, after 6 months of SGA therapy.
The markers of subclinical atherosclerosis, such as CIMT, ABI and echocardiographic parameters of left ventricular systolic function (LVEF) had no different values in SZ at baseline, compared with those measured in healthy subjects, and did not change significantly after 6 months of antipsychotic therapy. But, the echocardiographic examination showed significantly lower values of the E/A ratio in the SZ patients, suggesting the presence of subclinical left ventricular diastolic dysfunction. In a study published by Ünsal,15 patients with SZ had decreased ABI and increased CIMT when compared to healthy controls (P<0.01). The difference in the findings could be explained by the patients′ selection. Our study included SZ patients in the first psychotic episode, with a mean age of 29 years. In Ünsal′s study, the SZ patients head a mean age of 38 years and were not at the first psychotic episode, but the duration of the disease is not specified. Concordant to our results, Ünsal also observed the presence of significantly lower values of the echocardiographic determined E/A ratio in the SZ patients than in the control group (P<0.001). After 6 months of antipsychotic treatment, the E/A ratio increased in our study but remained significantly lower than in the healthy controls (P=0.03). No significant differences in the E/A increase were noted between the olanzapine and risperidone treated patients.
Patients with SZ have a higher risk for cardiovascular diseases and acute myocardial infarction compared with the nonschizophrenic population; therefore, they have an increased risk for mortality resulting from these diseases.30,31 Early diagnosis of patients with SZ with subclinical atherosclerosis or subclinical left ventricular dysfunction is of great importance in terms of reducing cardiovascular morbidity and mortality. Patients with SZ should be followed-up closely for cardiovascular risk factors, starting with the first psychotic episode. Our results underline the importance of early initiation of antipsychotic treatment in order to stabilize inflammation and to decrease the risk of atherosclerosis and cardiac dysfunction development and progression. Knowing that the SGA may induce dyslipidemia, hyperglycemia, and overweight, efforts have to be made to early detect and correct these additional cardiovascular risk factors in SZ patients.
Study Limitations
The limitations of this study include the small sample sizes of groups, the short follow-up period and the fact that only the SZ patients were hospitalized, the stress of hospital admission being a factor that might induce a supplementary endothelial dysfunction. Further, the antipsychotic medication could have independent effects on atherosclerosis and cardiac dysfunction. Larger studies are needed for highlighting the effects of antipsychotic treatment on the cardiovascular risk of SZ patients.
Conclusion
The present study shows that it is important to evaluate endothelial inflammation and subclinical cardiac diastolic dysfunction at the onset of SZ. The increased values of baseline sVCAM-1 were correlated with the severity of SZ symptoms at FEP. Antipsychotic treatment with SGA reduced significantly both the severity of SZ symptoms and the endothelial inflammation as evidenced by sVCAM-1 levels. But, the antipsychotic treatment also increased several markers of cardiovascular risk. These must be carefully monitored and immediately corrected, to reduce cardiovascular morbidity and mortality in this high-risk population. Increasing understanding of the role of inflammation in SZ will enable new therapeutic approaches and will provide new methods to reduce the cardiovascular risk in SZ patients.
Disclosure
Liana Dehelean reports personal fees from Angelini, Johnson & Johnson, Lundbek, Eli Lilly, and Gedeon Richter outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Leboyer M, Oliveira J, Tamouza R, Groc L. Is it time for immunopsychiatry in psychotic disorders? Psychopharmacology (Berlin). 2016;233:1651–1660. doi:10.1007/s00213-016-4266-1
2. Cheng SC, Schepp KG. Early intervention in schizophrenia: a literature review. Arch Psychiatr Nurs. 2016;30:774–781. doi:10.1016/j.apnu.2016.02.009
3. Fond G, d’Albis MA, Jamain S, et al. The promise of biological markers for treatment response in first-episode psychosis: a systematic review. Schizophr Bull. 2015;41:559–573. doi:10.1093/schbul/sbv002
4. Pillinger T, Osimo EF, Brugger S, et al. A meta-analysis of immune parameters, variability, and assessment of modal distribution in psychosis and test of the immune subgroup hypothesis. Schizophr Bull. 2019;45(5):1120–1133. doi:10.1093/schbul/sby160
5. Fraguas D, Diaz-Caneja CM, Ayora M, et al. Oxidative stress and inflammation in first-episode psychosis: a systematic review and meta-analysis. Schizophr Bull. 2017;45(4):742–751. doi:10.1093/schbul/sby125
6. Upthegrove R, Manzanares-Teson N, Barnes NM. Cytokine function in medication-naive first episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2014;155(1–3):101–108. doi:10.1016/j.schres.2014.03.005
7. Pramyothin P, Khaodhiar L. Metabolic syndrome with the atypical antipsychotics. Curr Opin Endocrinol Diabetes Obes. 2010;17:460–466. doi:10.1097/MED.0b013e32833de61c
8. Nguyen TT, Dev SI, Chen G, et al. Abnormal levels of vascular endothelial biomarkers in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2017. doi:10.1007/s00406-017-0842-6
9. Mulvihill NT, Foley JB, Crean P, Walsh M. Prediction of cardiovascular risk using soluble cell adhesion molecules. Eur Heart J. 2002;23:1569–1574. doi:10.1053/euhj.2002.3188
10. Muller WA, Weigl SA, Deng X, Phillips DM. PECAM-1 is required for transendothelial migration of leukocytes. J Exp Med. 1993;178:449–460. doi:10.1084/jem.178.2.449
11. Andor M, Dehelean LM, Romosan AM, et al. A novel approach to cardiovascular disturbances in patients with schizophrenia spectrum disorders treated with long-acting injectable medication. Neuropsychiatr Dis Treat. 2019;15:349–355. doi:10.2147/NDT.S186892
12. Khandaker GM, Cousins L, Deakin J, et al. Inflammation and immunity in schizophrenia: implications for pathophysiology and treatment. Lancet Psychiatry. 2015;2:258–270. doi:10.1016/S2215-0366(14)00122-9
13. Goldsmith DR, Rapaport MH, Miller BJ. A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder, and depression. Mol Psychiatry. 2016;21:1696–1709. doi:10.1038/mp.2016.3
14. Aboul-Fotouh S, Elgayar N. Atypical antipsychotics such as risperidone, but not paliperidone, worsen vascular endothelial function via upregulation of adhesion molecules VCAM-1, ICAM-1, and E-selectin in diabetic rats. Can J Physiol Pharmacol. 2013;91:1119–1126. doi:10.1139/cjpp-2013-0185
15. Unsal C, Oran M, Tureli HO, et al. Detection of subclinical atherosclerosis and diastolic dysfunction in patients with schizophrenia. Neuropsychiatr Dis Treat. 2013;9:1531–1537. doi:10.2147/NDT.S52030
16. DSM-5. Diagnostic and Statistical Manual of Mental Disorders.
17. Velligan D, Prihoda T, Dennehy E, et al. Brief psychiatric rating scale expanded version: how do new items affect factor structure? Psych Res. 2005;135(3):217–228. doi:10.1016/j.psychres.2005.05.001
18. Lang RM, Bierig M, Devereux RB, et al; Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendation for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 18;2005:1440–1463. doi:10.1016/j.echo.2005.10.005
19. Velligan DI, Lam YWF, Glahn DC, et al. Defining and assessing adherence to oral antipsychotics: a review of the literature. Schizophr Bull. 2006;32:724–742. doi:10.1093/schbul/sbj075
20. Fialko L, Garety PA, Kuipers E, et al. A large-scale validation study of the Medication Adherence Rating Scale (MARS). Schizophr Res. 2008;100:53–59. doi:10.1016/j.schres.2007.10.029
21. Spieker LE, Hurlimann D, Ruschitzka F, et al. Mental stress induces prolonged endothelial dysfunction via endothelin-A receptors. Circulation. 2002;105:2817–2820. doi:10.1161/01.CIR.0000021598.15895.34
22. Martelletti P, Stirparo G, Morrone S, et al. Inhibition of intercellular adhesion molecule-1 (ICAM-1), soluble ICAM-1 and interleukin-4 by nitric oxide expression in migraine patients. J Mol Med. 1997;75:448–453. doi:10.1007/s001090050130
23. Schwarz MJ, Riedel M, Ackenheil M, Muller N. Decreased levels of soluble intercellular adhesion molecule-1 (sICAM-1) in unmedicated and medicated schizophrenic patients. Biol Psychiatry. 2000;47(1):29–33. doi:10.1016/S0006-3223(99)00206-1
24. Meyer JM, McEvoy JP, Davis VG, et al. Inflammatory markers in schizophrenia: comparing antipsychotic effects in Phase 1 of the clinical antipsychotic trials of intervention effectiveness study. Biol Psychiatry. 2000;66:1013–1022. doi:10.1016/j.biopsych.2009.06.005
25. Habeas K, Shang L. Alterations in intercellular adhesion molecule 1 (ICAM-1) and vascular cell adhesion molecule 1 (VCAM-1) in human endothelial cells. Tissue Cell. 2018;54:139–143. doi:10.1016/j.tice.2018.09.002
26. Dehelean L, Andor M, Romosan AM, et al. Pharmacological and disorder associated with cardiovascular changes in patients with psychosis. A comparison between olanzapine and risperidone. Farmacia. 2018;66(1):129–134.
27. Chaggar PS, Shaw SM, Williams SG. Effect of antipsychotic medications on glucose and lipid levels. J Clin Pharmacol. 2011;51(5):631–638. doi:10.1177/0091270010368678
28. Perez-Iglesias R, Mata I, Pelago-Teron JM, et al. Glucose and lipid disturbances after 1 year of antipsychotic treatment in a drug-naïve population. Schizophr Res. 2009;107(2–3):115–121. doi:10.1016/j.schres.2008.09.028
29. Attux C, Quintana MI, Chanes AC. Weight gain, dyslipidemia and altered parameters for metabolic syndrome on first-episode psychosis patients after a six-month follow-up. Rev Bras Psiquiatr. 2007;29(4):346–349. doi:10.1590/S1516-44462006005000061
30. Lin HC, Chen YH, Lee HC, et al. Increased risk of acute myocardial infarction after acute episode of schizophrenia: 6 year follow-up study. Aust N Z J Psychiatry. 2010;44(3):273–279. doi:10.3109/00048670903487209
31. Lahti M, Tiihonen J, Wildgust H, et al. Cardiovascular morbidity, mortality and pharmacotherapy in patients with schizophrenia. Psychol Med. 2012;42:1–11.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.