Back to Journals » International Journal of General Medicine » Volume 15
The Predictive Value of Barthel Score, Sequential Organ Failure Assessment Score, and D-Dimer in the 28-Day Prognosis of Patients with Non-ST Elevation Myocardial Infarction: A Retrospective Study of 358 Patients
Authors Dai G, Wang J, Gao F, Liu W, Li P, Wei B, Yang J
Received 30 June 2022
Accepted for publication 7 September 2022
Published 13 September 2022 Volume 2022:15 Pages 7241—7248
DOI https://doi.org/10.2147/IJGM.S379628
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
GuiYing Dai,1,* JunYu Wang,1 FengLi Gao,2 WenHong Liu,1 Ping Li,1 Bing Wei,1 Jun Yang1,*
1Emergency Medicine Clinical Research Center, Beijing Chao-Yang Hospital, Capital Medical University, & Beijing Key Laboratory of Cardiopulmonary Cerebral Resuscitation, Beijing, People’s Republic of China; 2Nursing Department, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jun Yang, Emergency Medicine Clinical Research Center, Beijing Chao-Yang Hospital, Capital Medical University, & Beijing Key Laboratory of Cardiopulmonary Cerebral Resuscitation, Beijing, People’s Republic of China, Tel +86-13581846750, Fax +86-51718170, Email [email protected]
Purpose: To investigate the nursing prediction value of Barthel score, sequential organ failure assessment (SOFA) score and D-dimer on non-ST-elevation myocardial infarction (NSTEMI) inpatients.
Methods: The clinical data of 358 NSTEMI patients admitted to the emergency department were analyzed using logistic regression equation and a ROC curve was drawn. The area under ROC curve (AUC) of different indicators was compared. A COX regression model was created, and a survival curve was drawn.
Results: There were significant differences in age, D-dimer, WBC, NT-proBNP, EF (%), BI score, MEWS score, and SOFA score between the 28-day death group and the survival group (P < 0.05). The results showed that D-dimer (P = 0.002), SOFA score (P = 0.017), BI score (P < 0.001), and chest pain symptoms (P < 0.001) were independent predictors of 28-day death. When chest pain symptoms (AUC = 0.585), D-dimer (AUC = 0.945, Z = 8.00, P < 0.01), BI score (AUC = 0.145, Z = 5.36, P < 0.01), and SOFA score (AUC = 0.847, Z = 4.93, P < 0.01) were compared, the results showed that BI score (HR = 0.961, P < 0.01) and SOFA score (HR = 1.316, P < 0.001) had statistical significance on the 28-day survival time of the dead patients.
Conclusion: The Barthel score, SOFA score, and D-dimer are all essential in predicting the severity of NSTEMI patients, with a high nursing evaluation value. The Barthel and SOFA scores are associated with the risk of death within 28 days.
Keywords: Barthel score, NSTEMI, SOFA score, D-dimer, predictive value of nursing
Introduction
In recent years, the number of acute myocardial infarction (AMI) patients with non-ST-segment elevation myocardial infarction (NSTEMI) has been increasing.1–3 NSTEMI is characterized by acute onset, hidden disease, many complications, and high mortality rate. Research on related factors affecting the prognosis of the disease has always been a hot spot in this field.4–8 Nursing work, as an integral part of clinical diagnosis and treatment, is crucial to the implementation of overall diagnosis and treatment of patients, as well as disease prognosis. However, it remains unclear how nursing staff can use early clinical data to scientifically and comprehensively analyze and evaluate potentially high-risk critically ill patients in order to provide clinical nursing intervention measures. Evidence-based practice is still a challenge in the current nursing work. Therefore, we designed an experimental investigation using a retrospective analysis of related factors in NSTEMI patients who were admitted at the hospital. We identified and analyzed indicators with early warning value for the 28-day prognosis of NSTEMI patients. Indicators provide the basis for better clinical nursing management of critically ill patients by providing an early warning value of nursing grading and intervention measures.
Methods
Design
The research method adopted a cross-sectional study to retrospectively record the information of the non-ST elevation myocardial infarction patients from the emergency department of hospital. Patients were divided into two groups based on their 28-day prognosis: survival and death. A total of 311 (86.9%) patients survived, whereas 47 (13.1%) died. The patient’s symptoms, laboratory and disease-evaluation scoring scale were compared between the two groups. Furthermore, duration of hospitalization and the time from onset to death for patients who died 28 days after the onset of the disease were recorded.
Participants
Data from 358 non-ST elevation myocardial infarction patients, who were admitted to the emergency department of hospital, was continuously collected from January 1, 2020 to June 31, 2021. The data was obtained in accordance with the guidelines set by the European Society of Cardiology (ESC) in 2020 (Collet JP et al 2021).9
Data Collection
The data as follows: basic information including age, gender, past medical history, and admission complaints (eg, chest pain), among others; laboratory examinations at admission including blood routine, D-dimer, CK-MB, cTnI, and NT-proBNP, among others. The disease-evaluation scoring scale, which includes the BI score, MEWS score, and SOFA score, was used upon admission.
Ethical Consideration
This study complied with medical ethics standards, and the research plan was approved by Ethics Committee of Beijing Chao-Yang Hospital (review the batch number:2021-ke-474) and patients voluntarily signed an informed consent. This study complies with the Declaration of Helsinki.
Data Analyses
The data were analyzed using SPSS 24.0 software. The measurement data conforming to the normal distribution are expressed as mean ± standard deviation ( ). The comparison between two groups was conducted using an independent sample t-test. The count data is expressed as frequency or percentage. The χ2 test was used to compare frequencies between two groups, and the logistic regression equation was used to analyze the risk factor. We also generated a ROC working curve and calculated the odds ratio (OR) and 95% confidence interval (95% CI). The area under the ROC curve (AUC) was compared using the Z test. A multivariate COX regression model was used to analyze the death risk and generate a survival curve. The values were considered statistically significant when P < 0.05.
). The comparison between two groups was conducted using an independent sample t-test. The count data is expressed as frequency or percentage. The χ2 test was used to compare frequencies between two groups, and the logistic regression equation was used to analyze the risk factor. We also generated a ROC working curve and calculated the odds ratio (OR) and 95% confidence interval (95% CI). The area under the ROC curve (AUC) was compared using the Z test. A multivariate COX regression model was used to analyze the death risk and generate a survival curve. The values were considered statistically significant when P < 0.05.
Results
Comparison of Indicators Between the Survival and the Death Groups
Patients were divided into two groups based on their 28-day prognosis: survival and death. A total of 311 (86.9%) patients survived, whereas 47 (13.1%) died. When compared to the death group, males had a higher mortality rate (57.4%) than females (42.6%). The most prevalent complaint was chest pain with 144 (40.2%). The length of hospital stay was not statistically different between the two groups.
The survival group had significantly lower age (69.06 ± 13.24 vs 77.87 ± 8.99, P = 0.001), D-dimer (0.34 ± 0.71 vs 2.49 ± 3.06, P = 0.001), MEWS score (1.60 ± 1.53 vs 3.15 ± 2.10, P = 0.000), SOFA score (1.90 ± 2.08 vs 5.79 ± 3.11, P = 0.001), NT-proBNP (3871.38 ± 7331.09 vs 9876.83 ± 11,014.05, P = 0.001), and WBC (8.73 ± 3.55 vs 33.61 ± 52.28, P = 0.008), EF% (59.41± 12.32 vs 52.45 ± 13.31, P = 0.001), However, the Barthel score (44.13 ± 25.25 vs 7.45 ± 16.41, P = 0.000) was significantly higher in the survival group than in the death group, PCI was statistically significant between the two group. Other indices, such as creatine kinase isoenzyme (CK-MB), cardiac troponin I (cTnI), total cholesterol (TC), myoglobin (MYO), serum creatunine (SCR), blood sugar (BG), and hospital time were not significantly different (Table 1).
 |
Table 1 Comparison of Index Parameters Between the Survival Group and the Death Group |
Analysis of Risk Factors Correlated with Patient Death in 28 Days
The aforementioned variables were used in the logistic regression analysis equation, with prognosis as the dependent variable item to discriminately classify the prognostic outcome (death at 28 days). The predicted probability of 0.5 was used as the discriminant cut-off point. According to the results, the total discriminant rate of the equation was 92.8%. D-dimer [B = 0.696, Exp (B) = 2.006, P = 0.002] and SOFA score [B = 0.325, Exp (B) = 1.384, P = 0.17] were risk factors, whereas Barthel score [B = -0.068, Exp (B) = 0.934, P = 0.000] and chest pain symptoms [B = -2.842, Exp (B) = 0.058, P = 0.000] were independent predictors of 28-day death (Table 2).
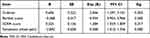 |
Table 2 Binary Logistic Regression Analysis Results |
The Predictive Value Analysis of the Barthel Score, SOFA Score, and D-Dimer
The above-mentioned parameters were used in the equation to draw the ROC working curve. The 28-day death was defined as a positive event. The D-dimer (AUC = 0.945, SE = 0.013) predicts 28-day death AUC significantly higher than SOFA score (AUC = 0.847, SE = 0.031, Z = 2.91, P < 0.01), Barthel score (AUC = 0.145, SE = 0.026, Z = 3.09, P < 0.01), and chief complaint of chest pain symptoms (AUC = 0.585, Z = 8.00, P < 0.01); SOFA score (AUC = 0.847, Z = 5.36, P < 0.01) and Barthel score (AUC = 0.145, Z = 4.93, P < 0.01). The AUC of 28-day death was significantly greater than the AUC of chest pain symptoms (AUC = 0.585). Furthermore, the SOFA and Barthel scores had the same predictive effect, indicating that the predictive value of D-dimer, SOFA score, and Barthel score for death was greater than that of chest pain symptoms (Figure 1 and Table 3).
 |
Table 3 ROC Curve Analysis of the Relationship Between the Three Indicators and the Death of Patients in the Hospital |
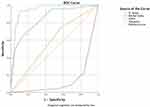 |
Figure 1 ROC curve of 28-day prognosis (death) in patients with NSTEMI. |
Multivariate Cox Regression Model Analysis
A total of 47 patients died within 28 days after the onset. The effects of D-dimer, SOFA score, and Barthel score of the dead patients on the time from onset to death of NSTEMI patients were analyzed using the Cox regression model. The results showed that the overall model test was significant (P = 0.000). The variables Barthel and SOFA scores were significant (P = 0.000), but D-dimer was excluded because it was not significant (P = 0.318). The results of the final selected model showed that the lower the Barthel score, the greater the risk of death; the higher the SOFA score, the greater the risk of death (Table 4). Lastly, the aforementioned settings were used to generate a survival curve (Figure 2).
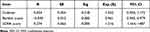 |
Table 4 Cox Regression Model Parameter Estimation |
 |
Figure 2 Survival curves of patients who died within 28 days. |
Discussion
Non-ST-segment elevation myocardial infarction (NSTEMI) is one of the most common cardiovascular emergencies and critical illnesses recorded in the emergency department. In recent years, the proportion of AMI patients with NSTEMI symptoms and signs has been increasing. Furthermore, the electrocardiogram changes are unusual, and the markers of myocardial injury appear during the late stages, making it is easy to overlook and misdiagnose, resulting in a poor prognosis. It is particularly difficult to classify the early risk of the disease and early recognition, which affects its short-term prognosis. The patients are prone to sudden death and other adverse events, posing significant risks in nursing work. Therefore, based on the existing diagnosis, treatment methods, and procedures, as well as in-depth analysis of the risk factors related to the prognosis of NSTEMI, it is critical to identify clinical indicators that can help early identification of high-risk patients with potential risks or poor prognosis in order to improve the quality of care and reduce risks.
The Barthel score scale is widely used in clinical nursing work in China. It provides a basis for guiding nursing classification and improving the quality of nursing services by accurately assessing the activities of daily living (ADL) of patients.10 In this study, we found that the Barthel score at admission was an independent predictor of death in 28 days in NSTEMI patients. The Barthel score was inversely proportional to the 28-day risk of death in patients. The forecast value was favorable, which could be attributed to various factors. Multiple organ functions may be involved due to the acute onset and severe illness of NSTEMI patients, leading to a decline in their self-care ability during admission, which is manifested as a decrease in the Barthel score. This obvious decline in the ability to take self-care is closely related to the severity of the patient’s illness at the time of onset. The death group had significantly lower Barthel score than the survival group. Poor self-care during at the time of admission to the hospital can easily lead to detection failure, poor diagnosis, and delayed treatment when the disease occurs or the condition changes, which affects the prognosis. The results of this study are similar to the conclusions made by Li F.11
A large number of studies have confirmed that D-dimer is an independent risk factor for the prognosis of cardiovascular patients.12,13 The higher the D-dimer level, the higher the long-term all-cause mortality and the higher the cardiogenic mortality rate. The number of patients with coronary artery disease has increased.14,15 This study found that D-dimer was a risk factor for death in 28 days for patients who had NSTEMI at the time of admission. The D-dimer level was inversely proportion to the probability of death within 28 days. D-dimer is a fibrinolysis-related marker, and its high level indicates thrombosis in the body, which is closely linked to endothelial damage caused by unstable systemic hemodynamics.13 Therefore, high D-dimer levels in patients with NSTEMI in the early stages often indicates that they are in a hemodynamically unstable state. If detection and correction are delayed, the prognosis of the patient becomes extremely poor. Although D-dimer is a risk factor for patient death and has a high predictive significance, its level is not correlated with the time of death of the patient. This could be due to early diagnosis of the abnormal physical signs of the patient via laboratory tests, as well as timely medication. Studies have shown that early identification and strengthening of nursing management have a positive impact on the prognosis of patients, and can effectively reduce the length of stay in NSTEMI patients and the occurrence of adverse events.16,17 Therefore, nursing staff should be more attentive to D-dimer changes in patients with NSTEMI in order identify the degree of criticality early, strengthen nursing interventions, improve the prognosis of patients, and reduce the occurrence of adverse events.
GRACE and TIMI scores are common tools for clinical risk stratification of patients with acute myocardial infarction.18 The GRACE score has a higher predictive value for the short-term mortality of NSTEMI patients than TIMI score.19 However, we found that SOFA score was more used in emergency patients, which was related to its applicability to multiple disease assessments and was more suitable for emergency room scenarios in. The SOFA score is a clinical scoring system for evaluating the severity of organ dysfunction in critically ill patients. The SOFA score is frequently used in the diagnosis and prognosis of sepsis patients.20,21 This study shows that the SOFA score at admission is an independent risk factor for 28-day death in NSTEMI patients, and it has a good predictive value for the prognosis. The higher the SOFA score at admission, the more severe the condition of the patient, and the greater the risk of death in the short term (28 days). The results of this study suggested that the SOFA score has great application value in the early stages of disease classification, prognosis judgment, and death risk assessment in NSTEMI patients. It is beneficial for nursing staff to identify patients in critical condition early in the management and implementation process, and accurately assessing patients with atypical clinical manifestations and potentially high-risk patients. Furthermore, nursing personnel should assist in accurate nursing grading and strengthen nursing intervention measures to reduce risk and improve patient prognosis.
This study indicated that chest pain symptoms were closely associated with prognosis of NSTEIM patients and were a protective factor for the 28-day death of patients. Patients with chest pain as the chief complaint had a lower mortality rate than patients with non-chest pain complaints, which may be more common in patients with typical chest pain symptoms. Early detection is correlated with early diagnosis and timely treatment. However, patients with poor self-care ability, especially when combined with language and other expression disorders, have a poor prognosis because the patient and family members cannot accurately describe the symptoms, or the clinical symptoms are not typical, and medical treatment is delayed. Previous studies have shown that patients with poor self-care ability have a worse prognosis and higher rates of adverse events after suffering from acute diseases than patients with good self-care ability.22 The current study confirmed the importance of Barthel score scale in NSTEMI patients. The prognosis is well-evaluated, with a good early-warning effect. The nursing staff should actively provide daily assistance to patients with low Barthel scores and pay attention to the changes in vital signs, particularly through details such as daily facial expressions, emotions, and emotional abnormalities of the patients. Moreover, the personnel should monitor changes in the condition of the patients over time. Furthermore, it is critical to appropriately strengthen the limb function training and cardiac rehabilitation training of the patients during the hospitalization period in order to improve the their ability of daily living and cardiac function and reduce the occurrence of adverse events.23
Because this was a retrospective study, and data was collected from patients who have completed their diagnosis and treatment. Therefore, it was impossible to adequately study the combination of Barthel score, D-dimer, SOFA score, and nursing grade due to the lack of continuous monitoring of relevant indicators. Furthermore, this was a single-center cross-sectional study with a small sample size and certain limitations. Therefore, the impacts of nursing interventions on changes in related indicators and the prognosis of patients may not have been thoroughly evaluated.
Conclusion
The D-dimer, SOFA score, and Barthel score are critical in early detection of the criticality of NSTEMI patients and have a high evaluation value. Barthel and SOFA scores are associated with the risk of death within 28 days. Monitoring the above indicators can assist clinical nurses to identify high-risk NSTEMI patients early, accurately implement nursing grading, and provide clinical evidence for improving the quality and safety of care and patient prognosis.
Author Contributions
All authors made a significant contribution to this work, whether that is in the conception, manuscript design, analysis, or in all these areas. All authors took part in drafting, revising, and critically reviewing the article. All authors gave final approval for the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for the contents of the article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cohen M, Visveswaran G. Defining and managing patients with non-ST-elevation myocardial infarction: sorting through type 1 vs other types. Clin Cardiol. 2020;43(3):242–250. doi:10.1002/clc.23308
2. Harrington DH, Stueben F, Lenahan CM. ST-elevation myocardial infarction and non-ST-elevation myocardial infarction: medical and surgical interventions. Crit Care Nurs Clin North Am. 2019;31(1):49–64. doi:10.1016/j.cnc.2018.10.002
3. Karwowski J, Gierlotka M, Gasior M, et al. Relationship between infarct artery location, acute total coronary occlusion, and mortality in STEMI and NSTEMI patients. Pol Arch Intern Med. 2017;127(6):401–411. doi:10.20452/pamw.4018
4. Pollack CV, Amin A, Wang T, et al. Contemporary NSTEMI management: the role of the hospitalist. Hosp Pract. 2020;48(1):1–11. doi:10.1080/21548331.2020.1701329
5. Chinese Medical Association Cardiovascular Diseases Branch, Chinese Journal of Cardiovascular Diseases Editorial Committee. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes (2016). Chin J Cerebrovasc Dis. 2017;45(5):359–376.
6. Hedayati T, Yadav N, Khanagavi J. Non-ST-segment acute coronary syndromes. Cardiol Clin. 2018;36(1):37–52. doi:10.1016/j.ccl.2017.08.003
7. Gilutz H, Shindel S, Shoham-Vardi I. Adherence to NSTEMI guidelines in the emergency department: regression to reality. Crit Pathw Cardiol. 2019;18(1):40–46. doi:10.1097/HPC.0000000000000165
8. Nishi FA, de Motta Maia FO, de Lopes Monteiro da Cruz DA. Assessing sensitivity and specificity of the Manchester Triage system in the evaluation of acute coronary syndrome in adult patients in emergency care: a systematic review protocol. JBI Database Syst Rev Implement Rep. 2015;13(11):64–73. doi:10.11124/jbisrir-2015-2213
9. Collet JP, Thiele H, Barbato E, et al.; ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289–1367. doi:10.1093/eurheartj/ehaa575
10. Ruoqiong S, Huang S, Hu M. Application research of Barthel index rating scale in guiding nursing staff to perform nursing grading[J]. Evid Based Nurs. 2017;3(1):82–84.
11. Li F, Li D, Yu J, et al. Barthel index as a predictor of mortality in patients with acute coronary syndrome: better activities of daily living. Clin Interv Aging. 2020;15:1951–1961. doi:10.2147/CIA.S270101
12. Choi S, Jang WJ, Song YB, et al. D-dimer levels predict myocardial injury in ST-segment elevation myocardial infarction: a cardiac magnetic resonance imaging study. PLoS One. 2016;11(8):e0160955. doi:10.1371/journal.pone.0160955
13. Wen Z, Yu T, Wu J, et al. The prognostic value of D-dimer in patients with acute non-ST-segment elevation myocardial infarction. China J Mod Med. 2019;29(7):86–91.
14. Charoensri N, Pornratanarangsi S. D-dimer plasma levels in NSTE-ACS patient. J Med Assoc Thai. 2011;94(Suppl 1):S39–45.
15. Schutte T, Thijs A, Smulders YM. Never ignore extremely elevated D-dimer levels: they are specific for serious illness. Neth J Med. 2016;74(10):443–448.
16. Chen YH, Huang SS, Lin SJ. TIMI and GRACE risk scores predict both short-term and long-term outcomes in Chinese patients with acute myocardial infarction. Acta Cardiol Sin. 2018;34(1):4–12. doi:10.6515/ACS.201801_34(1).20170730B
17. Ding X, Bai H, Ju Z. A comparative study of early invasive intervention and conventional delayed invasive intervention in elderly patients with acute non-ST-segment elevation myocardial infarction[J]. Chin Med Clin. 2020;20(18):3034–3036.
18. D’Ascenzo F, Biondi-Zoccai G, Moretti C, et al. TIMI, GRACE and alternative risk scores in acute coronary syndromes: a meta-analysis of 40 derivation studies on 216,552 patients and of 42 validation studies on 31,625 patients. Contemp Clin Trials. 2012;33(3):507–514. doi:10.1016/j.cct.2012.01.001
19. Wu C, Gao XJ, Zhao YY, et al. China Acute Myocardial Infarction (CAMI) Registry Research Group. [Prognostic value of TIMI and GRACE risk scores for in-hospital mortality in Chinese patients with non-ST-segment elevation myocardial infarction]. Zhonghua Xin Xue Guan Bing Za Zhi. 2019;47(4):297–304. Chinese. doi:10.3760/cma.j.issn.0253-3758.2019.04.007
20. The Emergency Physician Branch of the Chinese Medical Doctor Association. the shock and sepsis professional committee of the Chinese Research Hospital Association. Guidelines for the emergency treatment of sepsis/septic shock in China (2018). Infect Inflammat Repair. 2019;20(1):3–22.
21. Raith EP, Udy AA, Bailey M, et al.; Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE). Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in -hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017;317(3):290–300. doi:10.1001/jama.2016.20328
22. Zhuang-Sheng W, Yu-Sen C, Ying W, et al. Limitations in activities of daily living increase the risk of stroke in older Chinese adults: a population-based longitudinal study. China Nerve Regen Res. 2022;17(3):643–648. doi:10.4103/1673-5374.320994
23. Taylor JL, Bonikowske AR, Olson TP. Optimizing outcomes in cardiac rehabilitation: the importance of exercise intensity. Front Cardiovasc Med. 2021;8:7342. doi:10.3389/fcvm.2021.734278
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
