Back to Journals » Clinical Epidemiology » Volume 12
The Positive Predictive Value of Hip Fracture Diagnoses and Surgical Procedure Codes in the Danish Multidisciplinary Hip Fracture Registry and the Danish National Patient Registry
Authors Hjelholt TJ , Edwards NM , Vesterager JD , Kristensen PK , Pedersen AB
Received 15 November 2019
Accepted for publication 13 January 2020
Published 4 February 2020 Volume 2020:12 Pages 123—131
DOI https://doi.org/10.2147/CLEP.S238722
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Irene Petersen
Thomas J Hjelholt,1 Nina M Edwards,1 Jeppe D Vesterager,1 Pia K Kristensen,1,2 Alma B Pedersen1
1Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus N, Denmark; 2Department of Orthopedic Surgery, Horsens Regional Hospital, Horsens 8700, Denmark
Correspondence: Thomas J Hjelholt
Department of Clinical Epidemiology, Aarhus University Hospital, Olof Palmes Alle 43-45, Aarhus N 8200, Denmark
Tel +45 871 68219
Email [email protected]
Aim: The health-care databases may be a valuable source for epidemiological research in hip fracture surgery, if the diagnoses are valid. We examined the validity of hip fracture diagnoses and surgical procedure codes in the Danish Multidisciplinary Hip Fracture Registry (DMHFR) and the Danish National Patient Registry (DNPR) by calculating the positive predictive value (PPV).
Methods: We identified a random sample of 750 hip fracture patients registered in the DMHFR between 2014 and 2017. Diagnoses have been coded by the 10th revision of the International Classification of Diseases, while procedures have been coded by the Nordic Medico-Statistical Committee classification in the DNPR and directly transferred to the DMHFR. Using the surgical procedure description from the medical record as gold standard, we estimated the PPV of the hip fracture diagnoses and surgical procedure codes in the DMHFR and the DNPR with 95% confidence interval (CIs).
Results: The PPV was 90% (95% CI: 86%-93%) for fracture of the neck of femur, 92% (95% CI: 87%-95%) for trochanteric fracture, and 83% (95% CI: 78%-88%) for subtrochanteric fracture. Joining trochanteric and subtrochanteric fracture resulted in a PPV of 97% (95% CI: 95%-98%). Procedure codes had a PPV of 100% for primary prosthetic replacement and internal fixation with intramedullary nail, 96% (95% CI: 85%-99%) for internal fixation using screws alone, 91% (95% CI: 84%-96%) for internal fixation using plates and screws, and 89% (95% CI: 83%-94%) for internal fixation with other or combined methods. Stratifying by age group, gender, hospital type and calendar year of surgery showed similar results as the overall PPV estimates.
Conclusion: Our findings indicate a high quality of the hip fracture diagnoses and corresponding procedure codes in the DMHFR and the DNPR, with a majority of PPVs above 90%. Thus, the DMHFR and the DNPR are a valuable data source on hip fracture for epidemiological research.
Keywords: epidemiology, hip fractures, validity
Introduction
Hip fracture is a common condition among the elderly with almost 7000 new hip fractures in Denmark each year.1 The incidence worldwide is expected to rise substantially in the coming decades due to the aging population in all western societies.2–4 Sustaining a hip fracture has major individual and public health implications,5,6 indicated by a mortality rate of almost 30% within 1 year,1 high risk of postoperative complications,7 and increased disability among the survivors.8
This has led to the establishment of clinical quality databases on hip fracture patients in many countries around the world.9,10 The nationwide clinical quality database The Danish Multidisciplinary Hip Fracture Registry (DMHFR) was established in 2003.11 Since 2010, data on diagnoses and procedures have been directly transferred from the Danish National Patient Registry (DNPR) to the DMHFR. Clinical data are prospectively and routinely collected, giving the opportunity to perform epidemiological studies on incidence, risk factors and prognosis of hip fracture patients, answering clinical questions that are not easily addressed by randomized clinical trials. However, knowledge about the validity of data is essential if databases are used for research purposes.12
Until now, no validation studies on hip fracture diagnoses have been conducted in Denmark. Few validation studies on hip fracture diagnosis have been published from abroad, based on local data in Scandinavia (Norway and Finland)13,14 and administrative insurance claims in USA and Canada.15,16 The insurance claims databases are not comparable with the clinical quality databases due to the risk of selection bias. The Scandinavian studies represent health-care systems that share some common traits with the Danish, but there are also great differences in administrative systems and coding practices. Only the Finnish study subdivide the hip fracture diagnosis into neck of femur, trochanteric and subtrochanteric fractures and it was also the only study that validated the International Classification of Diseases 10th revision (ICD-10) codes rather than ICD-9. However, this study was challenged by different classification systems in their audit data and their registry, as pointed out by the authors themselves. Furthermore, since the publication of these studies, the Danish system has undergone a massive computerization, which may impact the registration. Since the DMHFR is being increasingly used for research purposes, the data quality needs to be determined.
Thus, we aimed to investigate the positive predictive value (PPV) of the diagnosis codes and the procedure codes in the DMHFR and the DNPR.
Materials and Methods
Health care in Denmark is fully tax-supported for all citizens, allowing equal access for all inhabitants to both general practitioners and hospitals.
Data Sources
The DMHFR is a nationwide clinical-quality database on hip fracture patients aged 65 years or above.11 The DMHFR was established in 2003 with the aim of monitoring and improving the treatment and care of hip fracture patients. All Danish hospitals treating hip fracture patients report data to the DMHFR on a number of selected quality indicators, as well as pre-, peri- and postoperative clinical data. During the first years of the DMHFR, data were collected using an independent web-platform. Since 2010, data are prospectively collected from the DNPR. Reporting is obligatory, and consequently, all hip fracture patients operated in Denmark should be registered in the DMHFR.
The DNPR has documented all hospital admissions with dates of admission and discharge, performed surgical procedures and discharge diagnosis with one primary – and up to 20 secondary diagnoses since 1977.17 Diagnoses are coded after ICD-8 up to 1993, and thereafter ICD-10 are used.18 The surgical procedures are coded after the Nordic Medico-Statistical Committee (NOMESCO) classification.19
Hip fracture diagnoses and all other DMHFR variables originate from the DNPR, from where ICD-10 and NOMESCO procedure codes are directly transferred to the DMHFR.
Study Population
From the DMHFR we identified all patients over 65 years of age, surgically treated for a hip fracture in the period January 1, 2014, until December 31, 2017. From this cohort, we collected a random sample of 150 patients from each of the following hospitals in the Central Denmark Region: Aarhus University Hospital, Horsens Regional Hospital, and Holstebro Regional Hospital. Likewise, from the Northern Denmark Region, we sampled 150 patients from Aalborg University Hospital and another 150 from Hjorring Regional Hospital. Thus, the total sample size included 750 hip fracture patients. This size was based on a balance between ensuring a good precision in our estimates within an acceptable use of resources.20 The sampling was conducted with equal weights on each diagnosis, to ensure 50 patients with each of the discharge diagnoses fracture of the neck of femur (DS720), trochanteric fracture (DS721) and subtrochanteric fracture (DS722) from each hospital.
In Denmark, each citizen is provided a 10-digit civil registration number, which is registered upon all health-care contacts, and encoded in health-care databases.21,22 We were able to use this civil registration number to find the patients in the hospitals’ electronic medical record.
Medical Record Review
Patient medical records were used as a gold standard. Trained health-care professionals, blinded from the information in the DMHFR, entered all information from the medical record in a standardized form, specifically developed for this purpose. Each review was initiated by confirming the civil registration number and the date of operation. The extracted information was based on the description of the performed procedure. The operating surgeon wrote the description, including the indication for the procedure, the diagnosis code, and the procedure code, on the day of operation. We were thus able to confirm or reject the hip fracture diagnosis and the surgical procedure recorded in the DMHFR.
We collected and managed all information from the medical journals using Research Electronic Data Capture (REDCap), an electronic data capture tools hosted at Aarhus University.23,24 REDCap is a secure, web-based software platform designed to support data capture for research studies.
Statistical Analysis
For each hip fracture diagnosis and surgical procedure we calculated, PPV with 95% confidence intervals (CI) as the proportion of diagnoses or procedures in the DMHFR, confirmed by the medical records. We calculated PPVs for each diagnosis and procedure individually in the overall cohort and stratified by age group, gender, hospital type and year of diagnosis. Furthermore, as many studies combine trochanteric and subtrochanteric fractures as lateral fractures, we mimicked this approach and computed PPVs for lateral fractures also. Analyses were performed in STATA version 15.1 (StataCorp) and R version 3.5.1 (R Foundation for Statistical Computing), package epiR.25 The content of this paper follows The Strengthening the Reporting of Observational Studies in Epidemiology.26
The Danish Data Protection Agency approved the study (journal number 2015-57-0002). As there was no contact with patients or interventions performed, permission from the Danish Scientific Ethical committee was not necessary.
Medical record review was approved by the Danish Patient Safety Authority (reference number: 3-3013-2739/1) and by the Head of each of the involved departments at the included hospitals.
Results
Figure 1 shows a flowchart of the selection and sampling process. We identified 26,920 patients in the DMHFR in the study period of which 6097 were treated at the five selected hospitals. All 750 records were eligible for analysis. The mean age among the sampled patients was 82.7 years (standard deviation: 8.3) and 514 (69%) were women. The overall PPV for all diagnoses was 100%; i.e. all patients had indeed sustained a hip fracture and had surgery performed on the date listed in the registry.
 |
Figure 1 Flowchart showing the selection of the study population. |
For patients operated for a fracture of the femoral neck, the most common procedure performed was a prosthetic replacement; either partial or total (Table 1). Patients with a trochanteric fracture were most frequently operated using a sliding compression screw with a side plate or an intramedullary nail, but different surgical codes were used for this operation. Most surgeons at the university hospitals used KNFJ6* whereas most surgeons at the regional hospitals used KNFJ8*, however even within the same hospital, the variation was substantial. Finally, patients with a subtrochanteric fracture were primarily treated with an intramedullary nail.
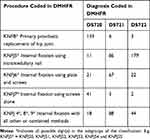 |
Table 1 Summary of Diagnosis Codes and Performed Procedures Coded in the Danish Multidisciplinary Hip Fracture Registry (DMHFR) |
PPV of Diagnosis Codes
Overall, we were able to verify the fracture of the neck of femur in 225 out of 250 cases, giving a PPV of 90% (95% CI: 86–93) (Table 2). A PPV of 92% (95% CI: 87–95) was found for trochanteric fracture whereas the result was 83% (95% CI: 78–88) for subtrochanteric fracture. When going through the surgery descriptions, we found many descriptions of a combined trochanteric and subtrochanteric fracture. However, only one of the diagnoses was registered in DMHFR since it was not possible to simultaneously record two. In the group of lateral fractures (trochanteric and subtrochanteric fractures combined), we found a substantially improved PPV of 97% (95–98).
 |
Table 2 Positive Predictive Value (PPV) of Diagnoses and Procedures Coded in the Danish Multidisciplinary Hip Fracture Registry (DMHFR) |
Stratifying the analysis into age group, gender, hospital type or by calendar year (Table 3–5) showed similar results as the overall analysis - the PPVs were robust for all stratifications. As for the overall analyses, we saw, with few exceptions, a general pattern with subtrochanteric fractures having the lowest PPV of 75–89% and trochanteric the highest PPV of 90–94%.
 |
Table 3 Positive Predictive Value (PPV) of Diagnoses and Procedures, by Age Group, Coded in the Danish Multidisciplinary Hip Fracture Registry (DMHFR) |
 |
Table 4 Positive Predictive Value (PPV) of Diagnoses and Procedures, by Gender and Hospital Type, Coded in the Danish Multidisciplinary Hip Fracture Registry (DMHFR) |
 |
Table 5 Positive Predictive Value (PPV) of Diagnoses Procedures, by Calendar Year, Coded in the Danish Multidisciplinary Hip Fracture Registry (DMHFR) |
PPV of Procedure Codes
In the overall analysis, we confirmed all 167 records of prosthetic joint replacements, giving a PPV of 100%. We also found a PPV of 100% for “internal fixations using intramedullary nail” with only one erroneous registration out of 276 entries (Table 2). For “internal fixation with screws alone”, the PPV was 96% (95% CI: 85–99), ‘internal fixation with plate and screws’ had a PPV of 91% (95% CI: 84–96) and the lowest PPV of 89% (95% CI: 83–94) was found for “internal fixation with other or combined methods”.
When stratifying the analysis according to age group, gender, hospital type or calendar year (Table 3–5) we again saw a slight variation, but generally PPVs with in the same range as for the overall analysis and with overlapping CIs. The lowest PPV for any analysis was observed for “internal fixation with other or combined methods” of 79% (95% CI: 63–90).
Discussion
Review of 750 patient records showed that the PPVs of hip fracture diagnoses and surgery codes in the DMHFR and the DNPR was high, in most cases above 90%. Our results suggest that these registries are indeed a valuable resource for epidemiologic hip fracture research. The PPV of 83% was found for subtrochanteric fracture, however, if we combined trochanteric and subtrochanteric fracture, the PPV increased to 97%.
Previous comparable studies validating the hip fracture diagnoses,13,15,27,28 find up to 20% of the database entries to be incorrect, meaning that the patient had not sustained a hip fracture. Our 100% correct registration of hip fracture patients in the DMHFR is likely because the DMHFR only includes patients recorded with both ICD and NOMESCO code in the DNPR. A validation study of the Norwegian registry by Hoiberg et al27 uses the same criteria as ours, finding 99.4% correct classification overall. If only identified by ICD codes, Hoiberg and colleagues found 24.1% of patients missing a NOMESCO code by mistake, which would not be included in the registry. However, a previous study from Denmark showed that completeness of the registration in the DNPR increased with less than 1% by using only diagnosis codes compared with using diagnoses in addition to surgery codes.1
Only one previous study,13 validating the Finnish hip fracture registry, divide hip fractures into sub-diagnoses. The authors find a PPV of 88.1% for fracture of the neck of femur, 96.0% for trochanteric and 62.5% for subtrochanteric fractures, slightly lower than our findings on all diagnoses. They argue that the variation in PPV is due to anatomic location, finding misclassifications to occur when the fracture is located on the border of the trochanteric region. However, this study is challenged by different classification systems in the database and the gold standard, which magnifies the problem substantially. Despite a uniform classification system for comparison in our registry, we find 15–20% of subtrochanteric fractures to be misclassified, mainly due to a combined fracture involving both the trochanteric and subtrochanteric region. This is concerning if one needs to distinguish between the two diagnoses, and thus, we recommend to pool them together, if possible, into “lateral fractures”.
The surgical procedure coding was in our study highly correct, with PPVs ranging from 89% to 100%. Especially prosthetic hip replacements, internal fixation using intramedullary nail and internal fixation using screws alone were good, which is quite similar to the findings of Cundall-Curry et al,28 although different coding systems were used. The concern in our results was the varying traditions in coding practices of sliding compression screw with lateral plate fixation. To our knowledge has this not been observed previously. According to the NOMESCO classification,19 the procedure should be coded as ‘internal fixation using other or combined methods’ (KNFJ8*), however it is understandable why some surgeons use KNFJ6* “internal fixation using plates and screws” as this title very well describes the procedure being performed. This confusion is likely the cause of the lower PPVs observed in these two groups.
The DMHFR use a setup with electronic transfer of routinely and prospectively collected data from the hospital medical records to the clinical quality database. This is very similar to a long range of hip fracture registries around the world. Even though other and locally selected variables should be validated before they are used for scientific research, we find, based on this study, good reasons to believe that the hip fracture diagnoses and procedure codes can be trusted in these databases in general. This is supported by the comparable validation of procedure codes from the British database.28 It should be noted that in order to make a comparison we had to rearrange the British data, based on their published results, into groups comparable to our own. Furthermore, data from one other Scandinavian country show similar PPVs on the hip fracture diagnoses with the distinction between trochanteric and subtrochanteric fractures as the main exception, as previously mentioned.13
This study only includes patients from two out of Denmark´s five regions. However, the different regions in Denmark seem to be comparable in terms of socioeconomic characteristics.29 Furthermore, the choice of hospitals of different volumes and uptake areas, including both the regional capital but also rural areas in both regions, encapsulates a representative sample of the Danish population. In support of this, we find comparable distributions of age and gender in our sample and at the national level.1 We find the risk of information bias in our study low, even though we relied solely on the description from the operating surgeon and did not evaluate preoperative x-rays or CT-scans. The detailed descriptions from the operating surgeon were very clear as to fracture type and surgical procedure. We have not evaluated the completeness of the registries, specificity, and negative predictive value. However, hip fracture patients are only admitted at a public hospital, since no private, inpatient acute wards exist in Denmark. All departments report discharge diagnoses to the DNPR for economic purposes and data is directly transferred from the DNPR to the DMHFR. Even though all departments have a strong incentive to ensure very high completeness, a study on all patients admitted to an orthopedic ward suggests the opposite.30
Conclusion
The PPVs for hip fracture diagnoses and surgical procedure codes in the DMHFR and DNPR were high, above 90%. The main exception was subtrochanteric fracture with a PPV between 80% and 90%, which can be surpassed by grouping trochanteric and subtrochanteric fractures. We find the data to be valuable for scientific research on prognosis among this group of patients and strongly encourage future studies on this topic.
Acknowledgments
The authors wish to thank the surgeons, physicians and other health-care professionals for their cooperation in submitting high-quality clinical data to the national health registries. Thank you to the DMHFR steering committee for their continuous work on developing and maintaining the database. We are grateful to the involved departments for their involvement and cooperation with our project. A special thanks to Project Nurse Henriette Kristofferson for assisting in building the electronic questionnaire for data capture. This work was supported by a grant from the Novo Nordisk Foundation.
Author Contributions
ABP conceived the study idea. All authors contributed to the study design and acquisition of the data. TJH analyzed the data and wrote the initial draft. All authors contributed towards drafting and critically revised the paper for important intellectual content, gave final approval of the published version and agreed to be accountable for all aspects of the work.
Disclosure
Dr Thomas J. Hjelholt and Mr Jeppe D. Vesterager report grants from Novo Nordisk Foundation, during the conduct of the study.
The authors report no other conflicts of interest in this work.
References
1. Pedersen AB, Ehrenstein V, Szepligeti SK, et al. Thirty-five-year trends in first-time hospitalization for hip fracture, 1-year mortality, and the prognostic impact of comorbidity: a danish nationwide cohort study, 1980–2014. Epidemiology. 2017;28(6):898–905. doi:10.1097/EDE.0000000000000729
2. Cooper C, Campion G, Melton LJ
3. Chen IJ, Chiang CY, Li YH, et al. Nationwide cohort study of hip fractures: time trends in the incidence rates and projections up to 2035. Osteoporos Int. 2015;26(2):681–688. doi:10.1007/s00198-014-2930-z
4. Stephens AS, Toson B, Close JC. Current and future burden of incident hip fractures in New South Wales, Australia. Arch Osteoporos. 2014;9:200. doi:10.1007/s11657-014-0200-5
5. Lane JM, Russell L, Khan SN. Osteoporosis. Clin Orthop Relat Res. 2000;372:139–150. doi:10.1097/00003086-200003000-00016
6. Lin JT, Lane JM. Osteoporosis: a review. Clin Orthop Relat Res. 2004;425:126–134. doi:10.1097/01.blo.0000132404.30139.f2
7. Lawrence VA, Hilsenbeck SG, Noveck H, Poses RM, Carson JL. Medical complications and outcomes after hip fracture repair. Arch Intern Med. 2002;162(18):2053–2057. doi:10.1001/archinte.162.18.2053
8. Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ. 1993;307(6914):1248–1250. doi:10.1136/bmj.307.6914.1248
9. The National Hip Fracture Database [homepage on the Internet]. https://www.nhfd.co.uk/.
10. Nasjonalt hoftebruddregister [Homepage on the Internet]. https://www.kvalitetsregistre.no/registers/nasjonalt-hoftebruddregister.
11. Kristensen PK, Röck ND, Christensen HC, Pedersen AB. The Danish Multidisciplinary Hip Fracture Registry 13-Year Results from a Population-Based Cohort of Hip Fracture Patients. Clin Epidemiol. 2020;12:9–21. doi:10.2147/CLEP.S231578
12. Goldberg J, Gelfand HM, Levy PS. Registry evaluation methods: a review and case study. Epidemiol Rev. 1980;2:210–220. doi:10.1093/oxfordjournals.epirev.a036224
13. Sund R, Nurmi-Luthje I, Luthje P, Tanninen S, Narinen A, Keskimaki I. Comparing properties of audit data and routinely collected register data in case of performance assessment of hip fracture treatment in Finland. Methods Inf Med. 2007;46(5):558–566. doi:10.1160/ME0382
14. Lofthus CM, Cappelen I, Osnes EK, et al. Local and national electronic databases in Norway demonstrate a varying degree of validity. J Clin Epidemiol. 2005;58(3):280–285. doi:10.1016/j.jclinepi.2004.07.003
15. Hudson M, Avina-Zubieta A, Lacaille D, Bernatsky S, Lix L, Jean S. The validity of administrative data to identify hip fractures is high–a systematic review. J Clin Epidemiol. 2013;66(3):278–285. doi:10.1016/j.jclinepi.2012.10.004
16. Rigler SK, Ellerbeck E, Whittle J, Mahnken J, Cook-Wiens G, Shireman TI. Comparing methods to identify hip fracture in a nursing home population using medicare claims. Osteoporos Int. 2011;22(1):57–61. doi:10.1007/s00198-010-1264-8
17. Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi:10.2147/CLEP.S91125
18. WHO. ICD 10 - version: 2016 [Homepage on the Internet]. World Health Organisation. https://icd.who.int/browse10/2016/en. Published 2016.
19. NOMESECO Classification of Surgical Procedures (NCSP), Version 1.15. Nordic Medico-Statistical Committee. https://norden.diva-portal.org/smash/get/diva2:970547/FULLTEXT01.pdf. Published 2010.
20. Pedersen A, Johnsen S. Vejledning for validering af data fra kliniske kvalitetsdatabaser. https://www.rkkp.dk/siteassets/om-rkkp/drift-og-udvikling/diverse-projekter/valideringmanuel_rkkp_-final_06062017.pdf. Published 2017.
21. Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi:10.2147/CLEP.S179083
22. Schmidt M, Pedersen L, Sorensen HT. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
23. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
24. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010
25. Stevenson M. epiR: tools for the analysis of epidemiological data [Homepage on the Internet]. https://CRAN.R-project.org/package=epiR. Published 2019.
26. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. doi:10.1371/journal.pmed.0040296
27. Hoiberg MP, Gram J, Hermann P, Brixen K, Haugeberg G. The incidence of hip fractures in Norway -accuracy of the national Norwegian patient registry. BMC Musculoskelet Disord. 2014;15:372. doi:10.1186/1471-2474-15-372
28. C-CD J, LJ E, FD M, GC R. Data errors in the National Hip Fracture Database. Bone Joint J. 2016;98-B(10):1406–1409. doi:10.1302/0301-620X.98B10.37089
29. Henriksen DP, Rasmussen L, Hansen MR, Hallas J, Pottegard A. Comparison of the five Danish regions regarding demographic characteristics, healthcare utilization, and medication use–a descriptive cross-sectional study. PLoS One. 2015;10(10):e0140197. doi:10.1371/journal.pone.0140197
30. Nymark T, Thomsen K, Rock ND. Diagnosis and procedure coding in relation to the DRG system. Ugeskr Laeger. 2003;165(3):207–209.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
