Back to Journals » Patient Preference and Adherence » Volume 14
The Outcome of Salt Treatment for Umbilical Granuloma: A Systematic Review
Authors Haftu H , Bitew H , Gebrekidan A, Gebrearegay H
Received 20 September 2020
Accepted for publication 23 October 2020
Published 30 October 2020 Volume 2020:14 Pages 2085—2092
DOI https://doi.org/10.2147/PPA.S283011
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Hansa Haftu,1 Helen Bitew,2 Atsede Gebrekidan,1 Hailemariam Gebrearegay1
1Department of Pediatrics and Child Health, School of Medicine, College of Health Sciences, Mekelle University, Tigray, Ethiopia; 2Department of Pharmacognosy, School of Pharmacy, College of Health Sciences, Mekelle University, Tigray, Ethiopia
Correspondence: Hansa Haftu Tel +251 948487877
Email [email protected]
Background: An umbilical granuloma is one of the common umbilical masses in young children which appears after the cords fall off, mainly due to an inflammatory reaction to subclinical infections. Though there are different recommendations of treatment modalities, which management modality is the best is not clear yet.
Objective: This systematic review aimed to assess the effectiveness of salt treatment in terms of complete resolution of the granuloma, any adverse effect, and any recurrence risk in those patients treated as inpatient or outpatient care.
Methodology: The literature search was done using search engines including Google scholar, PubMed, and Medlin. Articles published since 1990 and written in the English language with a target population of young children (less than 24 months) were included. To retrieve the articles, umbilical granuloma, treatment of umbilical granuloma, salt treatment, and neonatal umbilical disorder were used as keywords.
Results: This systematic review indicated that the majority of the studies done on salt treatment for umbilical granuloma show excellent response (complete resolution of the granuloma/discharge) with no adverse effect and no recurrence in the subsequent follow-up of the patients in almost all cases of the treatment group. Salt inside the occluded hyperosmolar chamber causes shrinkage of granuloma by a desiccant effect.
Conclusion: Cooking salt treatment for umbilical granuloma is effective, cheap, available, and easy to apply by non-health professionals. No side effects have been reported yet and a recurrence of the granuloma after treatment seems to be null.
Keywords: umbilicus, salt, infants, granuloma
Introduction
An umbilical granuloma is a common problem in the infancy period, which is a small swelling, composed of granulation tissue at the base of the umbilicus.1–3 The umbilical cord stump usually dries and separates within 1–2 weeks after birth.4,5 When the fibromuscular ring of the umbilicus closes and the cord stump falloff, the ring is covered by skin in normal circumstances. After the cord separation, there may be incomplete epithelialization over the ring and an area of beefy red tissue or granulation tissues with or without discharge may be visible. Granulation tissue formation is a normal stage in wound healing process, but if it is overgrowth in the umbilicus, it can result in Umbilical granuloma. This may follow a fumigating infection with discharge.6,7 The granuloma is thought to develop in response to subclinical infection.8–10 The size of the mass of the granuloma varies from 1 to 10 mm in diameter and it is the most common neonatal anomaly. The main reason for the granuloma development is because of delayed and irregular separation of stump due to inflammation. This excessive granulation tissue results in failure of epithelialization of the normal process and and may result in drainage.11
This excessive granulation tissue with or without discharge may infect and result in omphalitis and necrotizing fasciitis, which are fatal complication and may lead to death. Because of this, granuloma is considered as a pathologic and needs treatment.12,13 An umbilical granuloma looks like a small piece of bright red, moist flesh that remains in the umbilicus after cord separation when normal healing should have occurred.3 Despite the spontaneous regression of the untreated granulomas is not well documented, some authors recommend clinical follow-up (dry care) without any medication or intervention.9,14,15
Conventional treatment of umbilical granulomas with silver nitrate is a worldwide practice despite its high cost. Although the antiseptic effects of silver nitrate are remarkable, it has astringent/caustic effects as well. These effects are responsible for its therapeutic role, but adjacent healthy tissues may be damaged if silver nitrate is contacted.1,12,16,17 When principal textbooks on pediatrics and Neonatology were reviewed, it is unfortunate that silver nitrate application is advocated as a first-line treatment option, and other non-invasive approaches almost are not mentioned.1 There are other modalities of treatment like surgical electrocauterization, cryocauterization and surgical excision. But all treatment modalities have advantages and disadvantages, especially the complication and recurrences.8,14,18,19 The idea of using common salt for umbilical granuloma was first reported by Schmitt in 1972 and further detailed by Kesaree in 1983. This clinical incident occurred when an infant with an umbilical granuloma was treated with silver nitrate and the surrounding skin developed widespread superficial burns.20,21 Some literature reports support the presence of different management options, including salt treatment, although evidence-based ones are limited.1
Despite the presence of various treatment options in the literature, there is no clear consensus. The issue of what is the best treatment option is still elusive.20 Although the silver nitrate application is the most common one among the actual treatment options, other therapeutic methods are also available. These include common salt application, topical antiseptics/steroids, ligation, and excision.1 Though local Midwives and Consultant Neonatologists have expressed reservations about the use of salt without prior reference to medical opinion, salt treatment in the majority of cases is likely to be effective and safe in the available literature.21 The reasons for seeking these alternative options of managements are some unresponsive cases for silver nitrate application, the necessity of medical professionals for its application, the risk of periumbilical burn with chemical cauterization, some of the adverse effects, due to the presence of contraindications for bilateral ligations and its complication of the procedure, the lack of availability of the silver nitrate and the cost.1,18 Despite its promising results, there are limited studies and recommendations on salt treatment for Umbilical granuloma. One of the reasons why medical reference books have not yet supported the use of common salt for the treatment of umbilical granuloma is the small number of studies conducted in this area.12 Our case report demonstrates a complete resolution of the granuloma after the salt was applied on the second day. There was no adverse effect and recurrence in the subsequent follow-up.22 This triggers us to look for more evidence of salt treatment of umbilical granuloma because; this is the cheapest and available, which may have great importance for developing countries. Hence, the main objective of the systematic review is to look for evidence of salt treatment and its effectiveness for umbilical granuloma which will provide us the consolidated and summarized results, so that recommendations will be made based on the available research. The finding may help the researchers to do further clinical trials on the easily accessible, less costly, and no/little adverse effect of salt treatment, especially for the resources limiting areas which may be the treatment option.
Methods
A literature search was made using Google scholar, PubMed, and Medline as a database with the following keywords; umbilical granuloma, treatment of umbilical granuloma, salt treatment, and umbilical disorder. The selection of the articles was made based on the inclusion and exclusion criteria.
Study Selection
Articles were screened by reading the title and abstract. A total of 107 articles were found. When the title and abstract did not offer enough information, the authors searched for the full article. The steps of study selection are depicted in Figure 1. The articles were filtered finally based on the title and abstracts, language, and year of publications, age of the patients, and the type of granuloma.
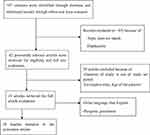 |
Figure 1 Systematic flowchart of article selection. |
Inclusion and Exclusion Criteria
Studies and case reports are written in English and conducted in young children (less than 24 months) treated as an outpatient or inpatient on salt treatment for umbilical granuloma was included. Studies and case reports without full text and those studies published before 1990, patients with the diagnosis of pyogenic granuloma and older children (above two years) were excluded.
The Outcomes of Interest
The major outcomes of interest of this systematic review were to collect and summarize salt treatment for umbilical granuloma. The authors documented the following data on the treatment in terms of complete resolution of granuloma/discharge, time of disappearance of the lesion, and adverse effects of salt. This will provide information for clinicians on the alternative options of treatment and for researchers to conduct further studies on salt treatment for its efficiency and any adverse effects.
Data Extraction
From each included study, the following data were extracted. The age range of the study population, type of the study design, sample size, year of publication of the study, diagnosis, country of the study, duration of treatment, the rate of response to treatment, any reported adverse effects, and area of treatment.
Result
Article selection was made by the PRISMA 2009 flow diagram shown in Figure 1. A total of 10 articles fulfilled all the eligibility criteria for the systematic review and all went through. The publication period ranges from 1990 to 2019. All studies assessed the diagnosis of umbilical granuloma in the outpatient department (OPD) and the outcome of the treatment. They also assessed the adverse effects and recurrences of the granuloma in the subsequent follow-up. All studies were done in young children (age range of 3 weeks to 24 months) in both genders who visited the outpatient department and diagnosed clinically with umbilical granuloma. In almost all of the studies, the design was a prospective observational and clinical trial of salt treatment effect on the granuloma except one which was a retrospective evaluation of the patient’s outcome for those who were treated with salt and assessed their outcome.
The treatment was made at home after mothers were counseled on details on how to apply the cooking (common) salt and appointed for the subsequent follow-ups for assessment of the outcome, any adverse effect, and recurrences. The cure rates of salt based on the different studies ranged from 53.33% to 100%. Except for one study which shows the cure rate of salt as 53.3%, the majority showed a higher cure rate (>90%) with no reported side effects and no recurrence rate (Table 1). Even in those patients who had no response to the initial 3–5 days of salt treatment, there was a misdiagnosis of granuloma for polyp and all patients went for surgery and responded well. But for those patients having the correct diagnosis with poor response to the salt treatment, the extension of the treatment to 5–10 days resulted in a good response without recurrence and adverse effect. The summary of all the data extracted from these studies is shown in Table 1.
 |  |  |
Table 1 The Summary of Research Data and Findings |
Discussions
An umbilical granuloma is a common umbilical abnormality of neonates and infants which develops in an umbilical stump after the cord falls off. The granuloma develops in about 1 out of 500 births.20 Most umbilical granuloma comes to attention after parent’s notice a persistent discharge or wet umbilicus or appearance of a pink beefy red tissue because of incomplete granulation tissue after the cord was dried and separated.21 If the granuloma is not treated, the discharge with or without the granulation tissue may persist and lead to irritation of surrounding skin, and the granuloma may be infected.21 There are different modalities of treatment for umbilical granuloma; such as silver nitrate, electro-cauterization, copper sulfate, and surgical excision. But each of the treatment modalities shows advantages and disadvantages.20,21 Standard texts and neonatologists continue to recommend silver as the first line of treatment, and no alternative methods for primary treatment have been discussed in the English texts and literature.20 But, silver nitrate causes burns in the surrounding skin and the recurrence rate is also there.20 The current treatment modalities for umbilical granuloma done via the health professional,like applied silver nitrate, and copper sulfate) and doing surgery unlike salt which can be done by the care giver or parents.20,23 Though there are limited recommendations of salt to treat granuloma in the literature, literature which showed how effective, easy to use and complete regression with no/reversible mild side effects of salt treatment are few in number.8,14,22,24
Haftu et al,22 and studies conducted by Farhat et al,5 Bagdad,25 Faranoush et al,24 and Saleh et al26 demonstrated a 100% cure rate of salt treatment with no adverse effect and no recurrence in the subsequent follow-up of the infants. Studies done by Hossain et al show excellent response in 91.7% of infants with a clinical diagnosis of umbilical granuloma and treated with cooking salt. There were no reported side effects and no recurrence. The remained 5% of infants unresponsive to this salt treatment was due to misdiagnosis of umbilical granuloma for a polyp. These patients were treated with surgery and the polyps were excised.9 This shows that the misdiagnosis of polyps for granuloma lowers the cure rate of salt treatment. We can conclude that the response rate in this study was higher than 91.7% if a corrected diagnosis of the umbilical granuloma was made.
Dhungel et al (2018) did a clinical trial of infants after they were grouped into salt and silver nitrate treatment categories. Patients in the salt group showed an excellent response rate (95%) than silver nitrate (87.6%) and they had no reported side effects and recurrence rates. But in silver nitrate groups, 19% of them had complications, and 9% of them had a recurrence of the umbilical granuloma. In this study, a total of 27 (8.3%) patients were unresponsive to common salt and silver nitrate for the treatment due to misdiagnosis of granuloma for polyp.23 Though the study did not put the exact numbers of patients who were misdiagnosed as granuloma for a polyp in the salt group, the response rate of salt treatment was above 95%.
Badebrarin et al also did a clinical trial of infants with umbilical granuloma comparing the response rate of patients who were treated with salt and surgical excision, which showed a 95% response rate after they were treated for five days. In this study, the unresponsive patients were treated for five additional days with salt and showed complete recovery except one who was misdiagnosed as a granuloma for a polyp and was treated surgically.12 So the response rate of salt in this study was almost 100% over the duration of treatment. This study showed an extension of treatment duration gained an additional response rate.
Fiaz et al2 and Annapurna et al27 did a clinical trial on the comparative effect of salt and copper sulfate. Both studies showed consistent results of copper sulfate as an excellent response which ranges from 95.5% to 100% with no side effects and recurrences. The overall cure rate of salt in the available literature ranges from 53.3%2 to 80%.27 Though there are reports on the recurrence rate and complications of the treatment in both studies, there are no clear reports on whether these patients had a misdiagnosis of polyps for granuloma or not, which were mentioned clearly in most of the other studies. And there was no extension, duration of treatment of salt beyond three days, which results in a higher cure rate.2,27 Badebrarin et al demonstrates the improvment of patients after they continue salt treatment for 5 additional days with total duration of treatment being 10 days..12 But, the shorter duration of salt treatment may not explain fully the low cure rate, as many patients responded well within three days of treatment.21
Conclusion
Despite the promising results of the few available pieces of the literature of salt treatment for umbilical granuloma, evidence in bigger sample size is still limited. Based on this systematic review, the majority of the studies showed that the application of common salt (cooking salt) to the umbilical granuloma is a simple, highly effective, and inexpensive form of treatment without any relapse or complications arising from the use of synthetic drugs or surgery. Above all salt can be applied by parents. So, salt treatment can be effective, safe, available, and cheap for the resource-limited countries where the medications may not be available and where health professionals are few in number to apply.
Data Sharing Statement
Please contact the Corresponding author for data requests.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
No specific funding was received.
Disclosure
The authors declare that they have no competing interests.
References
1. Karaguzel G, Aldemir H. Umbilical granuloma: modern understanding of etiopathogenesis, diagnosis, and management. J Pediatr Neonatal Care. 2016;4(3):1–5. doi:10.15406/jpnc.2016.04.00136
2. Fiaz M, Bhatti BA, Ahmed N, et al. A comparative study of the therapeutic effects of copper sulfate versus common salt (sodium chloride) in the treatment of infantile umbilical granuloma. Jmscr. 2017;5(11):31127–31132. doi:10.18535/jmscr/v5i11.226
3. Child Health Information. Umbilical granuloma in babies, royal united hospitals bath NHS. Foundation Trust. 2015;1–2.
4. Nathan TA. The umbilicus, granuloma. Nelson Pediatr. 2020;4175–4176.
5. Farhat A, Mohammadzadeh A. Comparison between two and twenty-four hours salt powder in treatment of infant umbilical granuloma. IRCMJ. 2008;10(4):267–269.
6. Donnell KA, Glick PL, Caty MG. Pediatric umbilical problems, pediatric surgery for primary care pediatrics part 1. Pediatr Clin North Am. 1998;45(4):791–799.
7. Block SL. Stumped’ by the newborn umbilical cord, practical advice for treating newborns and toddlers. Pediatr Ann. 2012;41(10):400–4004. doi:10.3928/00904481-20120924-05
8. Assi NA, Kadem KM, Alrubaee JR, et al. Management of umbilical granuloma. Thi-Qar Med J. 2010;4(4):82–87.
9. Hossain AZ, Hasan GZ, Islam KD. Therapeutic effect of common salt (table/cooking salt) on umbilical granuloma in infants. Bangladesh J Child Health. 2012;34(3):99–102. doi:10.3329/bjch.v34i3.10360
10. Kesaree N, Babu PS, Banapurmath CR, et al. Umbilical granuloma. Indian Pediatr. 1983;20(9):690–692.
11. Hegazy AA. Anatomy and embryology of umbilicus in newborns: a review and clinical correlations. Front Med. 2016;10(3):271–277. doi:10.1007/s11684-016-0457-8
12. Badebrarin D, Jamshidi M, Aabadi SA, et al. A comparison between the clinical results of salt therapy and surgery in the treatment of umbilical granuloma in infants. Iran J Pediatr Surg. 2018;4(1):1–13.
13. Wang H, Gao Y, Duan Y, et al. Dramatic response of topical, doxycycline in umbilical granuloma. Glob Pediatr Health. 2015;2:1–4. doi:10.1177/2333794X15607315
14. Lotan G, Klin B, Efrati Y. Double-ligature: a treatment for pedunculated umbilical granulomas in children. Am Fam Physician. 2002;65(10):2067–2068.
15. Whiston Hospital Children’s Community Nursing Team. Salt treatment for umbilical granuloma in babies, St Helens, and Knowsley a teaching hospital. Peadiatr Health Med Therap. 2018.
16. Poenaru D. Disorders of the umbilicus in infants and children: a consensus statement of the Canadian Association of Pediatric Surgeons. Pediatr Child Health. 2001;6(6):312–313.
17. Ogawa C, Sato Y, Suzuki C, et al. Treatment with silver nitrate versus topical steroid treatment for umbilical granuloma, A non-inferiority randomized control trial. PLoS One. 2018;1–10.
18. Brødsgaard A, Nielsen T, Mølgaard U, et al. Treating umbilical granuloma with topical clobetasol propionate cream at home is as effective as treating it with topical silver nitrate in the clinic. John Wiley Sons Ltd. 2015;104:174–177.
19. Abdullah O. Outcomes of local excision of the umbilical granuloma prior to silver nitrate cauterization. J Klagenfurt Austria. 2019;26(4):35–41.
20. Sanober B, Rachita S. A pinch of salt is all it takes! - The novel use of table salt for the effective treatment of pyogenic granuloma. J Am Acad Dermatol. 2019;1–7.
21. Bedfordshire and Luton Joint Prescribing Committee. Community health services bedfordshire, household salt for treatment of umbilical granuloma. Bedfordshire Health Commun Services. 2017;1–9.
22. Haftu H, Gebrehiwot T, Gidey A. Salt treatment for umbilical granuloma: effective, cheap and available alternative option of treatment. Case Rep Pediatr Health Med Therap. 2020;11:393–397. doi:10.2147/PHMT.S269114
23. Dhungel S, Pokhrel A, Acharya A. Outcomes and cost analysis of salt therapy versus silver nitrate for treatment of umbilical granuloma: 4-years’ experience in a private health centre; 4-years’ experience in a private health centre. EC Pediatr. 2018;7(7):653–659.
24. Faranoush M, Gohorbani R, Malek M, et al. Comparative study on therapeutic effect of sodium chloride and alcohol in infants with umbilical granuloma. J Kazvin Univ MED. 2006;10(2):65–68.
25. Bagadia J, Jaiswal S, Bhalala KB, et al. Pinch of salt: a modified technique to treat umbilical granuloma. Natl Inst Health. 2019;36(4):561–563.
26. Saleh AS. Therapeutic effect of common salt on umbilical granuloma in infants. Int J Med Sci Public Health. 2016;5(5):1–4. doi:10.5455/ijmsph.2016.07012016312
27. Annapurna D, Ramu P. Therapeutic effect of copper sulfate vs. common salt (table/cooking salt) on umbilical granuloma in infants, a comparative study. J Evol Med Dent Sci. 2015;4(10):1616–1621.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
