Back to Journals » Clinical Ophthalmology » Volume 17
The Outbreak of Acute Primary Angle-Closure Cases During the COVID-19 Omicron Variant Pandemic at a Tertiary Eye Center in Shanghai
Authors Huang H, Dai Y, Sun X , Fang Y
Received 18 September 2023
Accepted for publication 11 December 2023
Published 27 December 2023 Volume 2023:17 Pages 4009—4019
DOI https://doi.org/10.2147/OPTH.S440740
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Haili Huang,1 Yi Dai,1 Xinghuai Sun,1– 3,* Yuan Fang1,*
1Department of Ophthalmology & Visual Science, Eye & ENT Hospital, Shanghai Medical College, Fudan University, Shanghai, 200031, People’s Republic of China; 2State Key Laboratory of Medical Neurobiology and MOE Frontiers Center for Brain Science, Institutes of Brain Science, Fudan University, Shanghai, 200032, People’s Republic of China; 3NHC Key Laboratory of Myopia, Chinese Academy of Medical Sciences, Shanghai Key Laboratory of Visual Impairment and Restoration, Fudan University, Shanghai, 200031, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xinghuai Sun; Yuan Fang, Email [email protected]; [email protected]
Purpose: This study aimed to investigate the outbreak of acute primary angle-closure (APAC) during the COVID-19 Omicron variant pandemic in Shanghai.
Methods: This single-center retrospective observational study included all newly diagnosed patients with APAC in Eye, Ear, Nose, and Throat Hospital of Fudan University from December 15, 2022, to January 14, 2023 (pandemic group) during the COVID-19 pandemic of Omicron Variant, and from November 15, 2021, to February 14, 2022 (control group) when the infection rate of COVID-19 is very low in Shanghai. Demographic features, intraocular pressure, axial length, anterior chamber depth, lens thickness and pupil diameter were compared between the two groups.
Results: A total of 223 patients (261 eyes) were included in the pandemic group and 75 patients (82 eyes) in the control group. The number of APAC patients and eyes in the pandemic group is 8.92-fold and 9.55-fold of the monthly average number in the control group. The onset dates of acute angle-closure were mainly between December 17 and December 31, 2022. In the pandemic group, 72.65% of patients with APAC had a recent COVID-19 infection. Among the COVID-19-positive patients, 72% suffered APAC attacks within 24h of the occurrence of COVID-19 symptoms and 92% within 3 days. The pandemic group showed a longer time from symptoms to treatment and larger pupil diameter than the control group (7.92 ± 6.14 vs 3.63 ± 2.93 days, p = 0.006; 4.53 ± 1.17 vs 3.78 ± 1.24 mm, p = 0.003, respectively).
Conclusion: An outbreak of APAC attack was observed in our eye center during the COVID-19 Omicron variant pandemic in Shanghai. There may be a correlation between the onset of APAC and new COVID-19 Omicron variant infection, but the exact reason needs to be investigated further.
Keywords: acute primary angle-closure, COVID-19 pandemic, omicron variant, Shanghai
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It was first identified in December 2019 and has spread rapidly around the world.1–4 Due to the strict preventive measures implemented in Shanghai, the COVID-19 infection rate was very low until the preventive measures were lifted in early December 2022. From mid-December 2022 to mid-January 2023, the population of COVID-19 Omicron variant infection increased dramatically and dropped gradually in Shanghai.5
The infection can range from asymptomatic, mild to life-threatening respiratory distress. Due to the uncontrolled systematic inflammatory response resulting from the release of large amounts of chemokines and pro-inflammatory cytokines named “cytokine storm”, COVID-19 must be considered as a systemic disease involving multiple human systems.6–8 Ophthalmologists all over the world have reported various manifestations of the infection in the eye. As reported, about 31.6% COVID-19 affected patients had ocular manifestations consistent with conjunctivitis, including conjunctival hyperemia, chemosis, epiphora, or increased secretion.9 Besides conjunctivitis, viral keratoconjunctivitis, episcleritis, retinal vein occlusion, acute retinal necrosis, choroiditis, and some neuro-ophthalmic manifestations have been reported as COVID-19-related eye diseases.10–12 Some studies have reported that patients with COVID-19 suffered bilateral acute angle-closure attacks during hospitalization or after prone positioning.13–15 An Indian hospital reported a 62% increase in the proportion of visits that were true glaucoma emergencies during the COVID‑19 lockdown period in India in 2020.16 A Hong Kong’s hospital reported six cases of APAC, which was more than double of baseline in the second week of December 2022. All patients were newly COVID-19 affected.17 These reports indicated a relationship between COVID-19 and APAC attacks. Primary angle closure glaucoma (PACG) is an important reason for blindness in the Asian population.18 PACG is characterized by mechanical obstruction of the trabecular meshwork by apposition of the peripheral iris to the trabecular meshwork. APAC is usually due to a sudden occlusion of the trabecular network in the anterior chamber angle, resulting in a spike in intraocular pressure (IOP) and typical symptoms and clinical signs, such as ocular discomfort or pain, nausea or vomiting, or blurring of vision. Shallow anterior chamber, short axial length, elderly and female are considered as common risk factors for APAC.19 An outbreak of APAC attack was observed in our eye center from mid-December 2022 to late January 2023, which was the epidemic period of COVID-19 Omicron variant in Shanghai. After mid-January 2023, APAC cases decreased significantly. Thus, this study aimed to investigate the relationship between the onset of APAC and the COVID-19 Omicron variant infection and the clinical characteristics of APAC cases during the COVID-19 pandemic in Shanghai. In order to exclude the effect of season which was known as an influence factor for the onset of acute primary angle-closure20,21 and to make the sample size of two groups (the pandemic group and the control group) with good comparability, we collected and presented our hospital’s clinical data of APAC cases during the COVID-19 pandemic of Omicron Variant (December 15, 2022–January 14, 2023) which were compared to those during the similar season of the previous year (November 15, 2021– February 14, 2022) when the infection rate of COVID-19 is very low in Shanghai.
Materials and Methods
This retrospective observational study included consecutive cases diagnosed with APAC in the outpatient and emergency departments in our hospital from December 15, 2022, to January 14, 2023. Consecutive cases of APAC from November 15, 2021, to February 14, 2022, were included as the control group. This study was approved by the Institutional Ethics Committee of Eye, Ear, Nose, and Throat Hospital of Fudan University, Shanghai, China, and conducted in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from all subjects.
APAC was diagnosed based on the following criteria: (1) the presence of at least two of the following symptoms: ocular or periocular pain, nausea and/or vomiting, ipsilateral migraine, or antecedent history of intermittent blurring of vision with halos; (2) intraocular pressure (IOP) spike more than 40 mmHg; (3) the presence of shallow anterior chamber with at least three of the following signs: obvious conjunctival hyperemia, corneal epithelial edema, enlarged pupil, and direct disappearance of light reflex; and (4) detecting angle-closure in at least two quadrants of the chamber angle on gonioscopy.22 Only patients with newly diagnosed of APAC were included in the study. Participants with any of the following criteria were excluded: pre-diagnosed APAC, secondary angle-closure because of lens subluxation, uveitis, iris neovascularization, ocular trauma, intraocular tumor, and history of intraocular surgery.
Data, including age, gender, place of residence, systemic medical history, COVID-19 infection history, time from COVID-19 infection to APAC onset, and time from APAC onset to treatment, were collected. All patients underwent complete ophthalmologic examinations at presentation, including best-corrected visual acuity (BCVA) in logMAR and slit lamp biomicroscopy. IOP was measured using Goldmann applanation tonometry, and the mean of 3 IOP measurements recorded for each eye was used. Axial length (AL) and lens thickness (LT) were measured using IOL Master (Carl Zeiss, Inc., Jena, Germany). The anterior chamber angle, anterior chamber depth (ACD), and pupil diameter (PD) were determined using ultrasound biomicroscopy (UBM, MD-300L, MEDA Co., Ltd., Tianjin, China). All patients underwent UBM examinations in a supine position in the same room light.
All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 23.0) (IBM, Armonk, NY, USA). The Kolmogorov–Smirnov normality test was used to examine whether the variables were normally distributed. Continuous normally distributed data were summarized with a mean ± standard deviation (SD). Differences in the average between the two groups were evaluated using an independent sample t-test. To account for multiple testing, p values were adjusted using the Benjamini/Hochberg (B/H) method to control the false discovery rate (FDR). An association was considered statistically significant if the corresponding B/H-adjusted p value was less than 0.05, corresponding to an FDR of 5%. Categorical variables, such as sex, were assessed individually using Chi-squared test or Fisher’s exact test. p < 0.05 indicated statistical significance.
Results
Demographic Characteristics of Patients with APAC in Both Groups
A total of 298 cases were included in this study, all in Shanghai. Among them, 75 patients with APAC (82 eyes) were recruited from November 15, 2021, to February 14, 2022 (the control group), and 223 patients (261 eyes) were recruited during the COVID-19 pandemic from December 15, 2022, to January 14, 2023 (the pandemic group). The number of APAC patients in the pandemic group is 8.92-fold of the monthly average number of APAC patients in the control group. And the number of APAC eyes in the pandemic group is 9.55-fold of the monthly average number of APAC eyes in the control group. The mean ages (mean ± SD) of the patients in the control and pandemic groups were 67.05 ± 8.95 years and 65.34 ± 8.13 years, respectively. The control group included 16 (21.33%) males and 59 (78.67%) females, and the pandemic groups included 58 (26.01%) males and 165 (73.99%) females. The control group included 7 patients with APAC with bilateral onset (9.33%), and the pandemic group included 38 patients (17.04%). No significant differences in mean age, gender, left/right eyes, and laterality of the eyes were observed between patients in both groups (Table 1).
 |
Table 1 Demographic Characteristics of Patients with APAC in Both Groups |
Figure 1 showed the correlation between the number of APAC patients and date of their APAC onset. APAC patient numbers remained relatively stable in the same period of previous year (December 15, 2021–January 14, 2022; blue line). However, the number of APAC patients increased rapidly and spiked on December 23, 2022 and then dropped gradually during the COVID-19 pandemic of Omicron Variant (December 15, 2022–January 14, 2023; orange line). This trend was similar to the data of new COVID-19 infections in Shanghai.
 |
Figure 1 The onset date of patients with APAC recruited in the same period of different years with or without COVID-19 pandemic. |
Ocular Biometry of Patients with APAC in Both Groups
The peak IOP was 48.25 ± 7.23 mmHg in the control group and 46.01 ± 8.20 mmHg in the pandemic group, respectively (p = 0.122). The axial lengths (AL) were 22.36 ± 0.71 mm and 22.63 ± 2.28 mm, the anterior chamber depths (ACD) were 1.58 ± 0.29 mm and 1.62 ± 0.24 mm, and the lens thickness (LT) were 4.99 ± 0.44 mm and 5.02 ± 0.32 mm in the control and pandemic groups, respectively. No significant differences in AL, ACD, and LT were observed between the control and pandemic groups. However, the time from symptoms to treatment in the control group (3.63 ± 2.93 days) was significantly shorter than that in the pandemic group (7.92 ± 6.14 days, p = 0.006). Furthermore, the pupillary diameter was significantly larger in the pandemic group (4.53 ± 1.17 mm) than that in the control group (3.78 ± 1.24 mm, p = 0.003). All data are summarized in Table 2.
 |
Table 2 Ocular Biometry of Patients with APAC in Both Groups |
Characteristics of Patients with COVID-19 in the Pandemic Group
In the pandemic group, 72.65% (162/223) of the patients (192 eyes) were diagnosed with COVID-19 infection, identified by a nucleic acid or antigen test in previous 2 weeks, whereas 61 patients (69 eyes) showed no evidence of COVID-19 infection in previous 2 weeks. The mean ages (mean ± SD) were 65.25 ± 8.26 and 65.57 ± 7.83 years in the COVID-19-positive and COVID-19-negative groups, respectively. The COVID-19-positive group included 38 (23.46%) males and 124 (76.54%) females, and the COVID-19-negative group included 20 (32.79%) males and 41 (67.21%) females. In terms of bilateral onset, 30 patients with bilateral onset were in the COVID-19-positive group (18.52%) and 8 in the COVID-19-negative group (13.11%). No significant differences in mean age, gender, left/right eyes, and laterality of the eyes were observed between the COVID-19-positive and COVID-19-negative groups (Table 3).
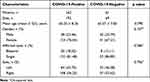 |
Table 3 Demographic Characteristics of Patients with APAC in the Pandemic Group |
The peak IOP was 45.97 ± 8.08 mmHg in the COVID-19-positive group and 46.10 ± 8.55 mmHg in the COVID-19-negative group. AL were 22.69 ± 2.58 mm and 22.41 ± 0.85 mm, ACD were 1.60 ± 0.25 mm and 1.63 ± 0.23 mm, and LT were 5.02 ± 0.32 mm and 5.04 ± 0.33 mm in the COVID-19-positive and COVID-19-negative groups, respectively. No significant differences in AL, ACD, LT and the time from symptoms to treatment were observed between the two groups. Furthermore, the pupillary diameter was significantly larger in the COVID-19-positive group (4.64 ± 1.19 mm) than that in the COVID-19-negative group (4.19 ± 1.05 mm). All data are summarized in Table 4.
 |
Table 4 Ocular Biometry of Patients with APAC in the Pandemic Group |
Additionally, most of COVID-19 infection patients presented systemic symptoms including fever, sore throat, nasal obstruction, tiredness and so on. The time from the occurrence of COVID-19 related systemic symptoms to APAC onset was statistically analyzed (Figure 2). Among all patients in the COVID-19-positive group, 149 (92%) experienced an APAC attack within three days of COVID-19 related systemic symptoms occurrence, whereas 117 (72%) of these patients experienced an attack within one day. These results indicate that APAC onset may be related to COVID-19 infection. Representative images obtained from single and bilateral eyes with APAC onset are shown in Figures 3 and 4, respectively.
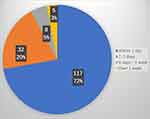 |
Figure 2 The days of APAC onset after COVID-19 related systemic symptoms in the COVID-19 positive patients. |
Discussion
This study showed an obvious increase in APAC onset in the Eye, Ear, Nose, and Throat Hospital of Fudan University, the biggest eye center in Shanghai, from December 15, 2022, to January 14, 2023. The number of patients newly diagnosed with APAC was 8.92-fold of the monthly average number of APAC patients in the control group, and the number of eyes that suffered APAC attack was 9.55-fold of the monthly average number of APAC eyes in the control group. The onset dates of APAC were mainly between December 17, 2022, and December 30, 2022, when COVID-19 rapidly spread in Shanghai.5 72.65% of patients newly diagnosed with APAC attack had a previous COVID-19 infection history. APAC symptoms started within 24h of fever caused by COVID-19 infection in 72% of patients with a COVID-19 infection history. The median onset time of APAC with a previous COVID-19 infection history was December 24, the same as when the COVID-19 infection reached its peak in Shanghai.5 These data suggest that there may be a correlation between the onset of APAC and new COVID-19 Omicron variant infection in the population.
COVID-19 has spread worldwide since 2019. Some APAC cases have been reported in COVID-19-positive patients or after vaccination against COVID-19 in Hong Kong, Korea, Italy, India, and Russia.11,13–15,17,23–25 An Indian hospital reported a 62% increase in the proportion of visits that were true glaucoma emergencies during the COVID-19 lockdown period. However, secondary open-angle glaucoma and neovascular glaucoma were the main emergency diagnoses. The number of APAC cases did not increase during the COVID-19 lockdown period.16 During Wuhan’s COVID-19 pandemic from the end of 2019 to the beginning of 2020, a mild increase in the number of APAC cases was observed compared to the next year.26 Our study showed an obvious outbreak of APAC cases in clinics during the COVID-19 Omicron variant pandemic, which is comparable with a recent report from other hospital in Shanghai and Guangdong.27,28 This may be due to the higher prevalence of PACG among Eskimos, Chinese, and Mongolians. Additionally, Asia accounts for about 77% of all worldwide PACG cases. Chinese ocular anatomic characteristics are a very important reason.29 Chinese have some ocular anatomic risk factors for angle-closure such as shadow anterior chamber, short AL, and narrow anterior angle.30–33 This can be explained why no outbreak of APAC in western countries during COVID-19 pandemic in last 3 years. Since December 2022, almost all epidemic strains in China were of the Omicron variant,5 with a higher infection rate than previous variants. The COVID-19 pandemic from the end of 2022 to the beginning of 2023 in China had a very fast speed of spread, and the COVID-19 infection ratio of the population reached 70–80% in about one month which is much faster and higher infection ratio than that in Wuhan 3 years’ ago. The outbreak of COVID-19 infection cases in such a short time in China is another important reason. Moreover, SARS-CoV-2 mutates all the time, and new strains are gradually generated. The main strains of SARS-CoV-2 in different countries were different. The China CDC analysis showed a predominance of Omicron lineages BA.5.2 and BF.7 among locally-acquired infections at the end of 2022. And in Shanghai, the main strains of the Omicron variant were BA.5.2 (accounting for 63%) and BF.7 (accounting for 37%).5 Different variants and strains have different pathogenic mechanisms. In Hong Kong, the main strains of the Omicron variant were BA.2 and BA. 4 in the 2022.34 The spread of different strains might be one of the reasons why there was no similar outbreak of APAC in Hong Kong and other Asian countries, which suffered the COVID-19 pandemic and had similar ocular anatomic risk factors for angle-closure.
The clinical characteristics of patients newly diagnosed with APAC in Shanghai during the COVID-19 pandemic were very similar to those reported in the previous year. Age, gender ratio, and bilateral acute attack ratio were very close in the two groups. Additionally, these data are very similar to those of previous reports in China or Korea in the non-pandemic period.26,35–37 However, the time from symptoms to treatment in the pandemic group was 7.92 ± 6.14 days, which was significantly longer than that in the control group (3.63 ± 2.93 days). In the pandemic group, the time from symptoms to treatment in COVID-19-positive patients was 8.42 ± 6.21 days, which was longer than that in COVID-19-negative patients (6.55 ± 5.76 days). Considering that APAC occurred at the same time of COVID-19 infection in most of the patients in the pandemic period, we proposed that, under severe systemic symptoms of COVID-19 such as fever and cough, many COVID-19-positive patients delayed APAC treatment. Besides that, the COVID-19 pandemic caused psychological panic to everyone.38 Even patients with a COVID-19-negative history are delaying their acute angle-closure attack treatment. As we known, rapid reduction of IOP is key to the treatment of APAC including antiglaucomatous drugs, laser treatment or surgery.39 Delayed treatment in the pandemic group might affect the final treatment results of APAC.
The anatomic parameters of eyeballs suffering APAC attacks were compared between the pandemic and control groups. Axial length, anterior chamber depth, and lens thickness were very close in both groups. However, the average pupil diameter of pandemic cases was 4.53 ± 1.17 mm, which was larger than that in the control group (3.78 ± 1.24 mm). In the pandemic group, the average pupil diameter in the COVID-19-positive group was 4.64 ± 1.19 mm, which was larger than that in the COVID-19-negative group. These findings are consistent with those of a previous study.26 Furthermore, the larger pupil diameter in the pandemic group, especially in the COVID-19-positive group, may be due to two reasons. First, the time from symptoms to treatment was longer in the pandemic group, especially in the COVID-19-positive group. Delayed treatment can lead to a longer time of high IOP, which causes more severe iris ischemia and pupillary sphincter damage, forming a larger pupil. Second, COVID-19 infection can cause direct damage, excessive inflammatory response, hypoxia, and other pathophysiological mechanisms, which may lead to more severe iris ischemia and a larger pupil.40–42
The reason why COVID-19 Omicron variant infection led to more APAC attacks is still unknown. COVID-19 is a systemic disease that can cause human respiratory infection and affect multiple organs. These organs include the kidney, liver, nervous system, spleen, etc. The coronavirus entry is through the angiotensin-converting enzyme 2 receptor (ACE-2 receptor).41 Coronavirus S protein binds to the cellular transmembrane protein, ACE-2 receptor, which promotes S protein activation by host protease and is responsible for viral entry.43,44 ACE-2 is not only expressed in the lungs, kidney, cardiovascular, but also highly expressed in ocular tissues, including conjunctiva, cornea, ciliary body, aqueous humor and retina.45–48 Conjunctivitis is most frequently reported as COVID-19 related eye disease. Besides ocular surface, the novel coronavirus may change the ciliary body shape or aqueous circulation through ACE-2 and lead to intraocular pressure elevation. A re-positive case of SARS-CoV-2 associated with glaucoma has been reported.49 However, this glaucoma case is not an angle-closure glaucoma case. It is well known that anatomy is the very important basis of acute angle-closure attacks. Acute angle-closure attacks are difficult to occur without a highly risky anatomic structure, even in eyeballs in COVID-19-positive patients.50,51 However, the onset of APAC requires a triggering factor in addition to these anatomic factors. Previous studies have reported that hantavirus infections cause bilateral acute angle-closure through non-pupillary blocking factors (ciliary body edema, anterolateral rotation of the iris-lens diaphragm).52 Similar to hantavirus, COVID-19 infection may be a very important trigger of acute angle-closure attacks. As shown in Figure 4, the initial presentation included subconjunctival hemorrhage and severe corneal stromal edema in some acute angle-closure cases with COVID-19 infection, which is hard to explain by APAC attacks only. COVID-19-affected conjunctivitis must occur, and COVID-19-affected uveitis might play a role in inducing acute angle-closure attacks. A case report showed that ciliary body swelling was observed in acute angle-closure cases after vaccination against COVID-19.11 The swollen ciliary body may lead to anterior shifting of the lens and trigger APAC attacks. Moreover, hypersecretion of aqueous humor may be a contributing risk factor in the eyes after vaccination against COVID-19.53 We proposed that COVID-19-affected eyes should have a similar ciliary body swelling and hypersecretion of aqueous humor as COVID-19-vaccinated eyes. The main strains of the Omicron variant of this COVID-19 pandemic in Shanghai might be more susceptible to the eyes, which needs further studies to identify. In Hong Kong’s cases reported that cough mixture or flu medication uses were detected in all these six APAC patients with newly COVID-19 affection.17 Commonly used cold medication including antitussive and nasal decongestants are common triggers to pupil dilation and can lead to APAC attack.54–57 In addition, some Chinese medicines containing ingredients such as pseudoephedrine and chlorpheniramine may also cause pupil dilation. Besides that, drinking a lot of water after fever,54 hyponatremia58 may also trigger APAC attacks during the COVID-19 pandemic period. Additionally, a high proportion of anxiety and depression was found in people during the COVID-19 pandemic.59,60 And it is increasingly acknowledged that APAC is highly associated with anxiety and depression.55,61,62 Moreover, lifestyle behaviors, including restricted physical activity and increased indoor and screen time caused by the COVID-19 pandemic, may play a role in APAC.63 All these factors may contribute to the outbreak of APAC attacks during the COVID-19 Omicron variant pandemic in Shanghai, but the exact reason remains to be further studied.
The present study has several limitations. First, this study was a single-center study based on the largest eye center in Shanghai, and we cannot exclude the influence of the patient choice preferences for Medical Care, the crowding of primary institution during the COVID-19 pandemic, and epidemic control policies. Therefore, the outbreak of APAC cases in this study is limited to our center and cannot represent all medical institutions nationwide. Long-term follow-up, multicenter and large sample clinical study are needed in the future research. Second, this study only used basic clinical characteristics for analysis, which indicate that there may be a correlation between the onset of APAC and new COVID-19 Omicron variant infection, but the exact reason remained unknown. Future work will include anterior aqueous humor analysis or animal studies. However, whether the virus has an effect on the prognosis of the APAC requires long-term observation.
Conclusion
An outbreak of APAC attack was observed in our eye center during the COVID-19 Omicron variant pandemic in Shanghai. Among COVID-19-positive patients, 92% suffered acute angle-closure attacks within 3 days of the occurrence of COVID-19 symptoms. Age, gender, bilateral ratio, and most of the anatomical characteristics during the COVID-19 pandemic were similar to those in the previous year. However, the time from symptoms to treatment of acute angle-closure attacks in this pandemic period was obviously longer, and the pupillary diameter was significantly larger than those in the previous year. There may be a correlation between the onset of APAC and new COVID-19 Omicron variant infection, but the exact reason needs to be investigated further.
Acknowledgments
We gratefully acknowledge the work of the past and present members of our department.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by Shanghai Clinical Research Key Project [grant number SHDC2020CR6029].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li T, Huang T, Guo C, et al. Genomic variation, origin tracing, and vaccine development of SARS-CoV-2: a systematic review. Innovation. 2021;2(2):100116. doi:10.1016/j.xinn.2021.100116
2. Rowe SL, Leder K, Dyson K, et al. Associations between COVID-19 and hospitalisation with respiratory and non-respiratory conditions: a record linkage study. Med J Aust. 2023;218(1):33–39. doi:10.5694/mja2.51778
3. Chan JYK, Wong EWY, Lam W. Practical aspects of otolaryngologic clinical services during the 2019 Novel Coronavirus Epidemic: an experience in Hong Kong. JAMA Otolaryngol Head Neck Surg. 2020;146(6):519–520. doi:10.1001/jamaoto.2020.0488
4. Grover S, Mehra A, Sahoo S, et al. Impact of COVID-19 pandemic and lockdown on the state of mental health services in the private sector in India. Indian J Psychiatry. 2020;62(5):488–493. doi:10.4103/psychiatry.IndianJPsychiatry_568_20
5. Chinese center for disease control and prevention. Available from: http://www.chinacdc.cn.
6. Long QX, Tang XJ, Shi QL, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020;26(8):1200–1204. doi:10.1038/s41591-020-0965-6
7. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
8. Rello J, Belliato M, Dimopoulos MA, et al. Update in COVID-19 in the intensive care unit from the 2020 HELLENIC Athens International symposium. Anaesth Crit Care Pain Med. 2020;39(6):723–730. doi:10.1016/j.accpm.2020.10.008
9. Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138(5):575–578. doi:10.1001/jamaophthalmol.2020.1291
10. Sen M, Honavar SG, Sharma N, Sachdev MS. COVID-19 and eye: a review of ophthalmic manifestations of COVID-19. Indian J Ophthalmol. 2021;69(3):488–509. doi:10.4103/ijo.IJO_297_21
11. Choi M, Seo MH, Choi KE, et al. Vision-threatening ocular adverse events after vaccination against coronavirus disease 2019. J Clin Med. 2022;11(12):3318. doi:10.3390/jcm11123318
12. Chen L, Deng C, Chen X, et al. Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: a cross-sectional study. Acta Ophthalmol. 2020;98(8):e951–e959. doi:10.1111/aos.14472
13. Barosco G, Morbio R, Chemello F, Tosi R, Marchini G. Bilateral angle-closure during hospitalization for coronavirus disease-19 (COVID-19): a case report. Eur J Ophthalmol. 2022;32(3):NP75–NP82. doi:10.1177/11206721211012197
14. Nerlikar RR, Palsule AC, Vadke S. Bilateral acute angle closure glaucoma after prone position ventilation for COVID-19 pneumonia. J Glaucoma. 2021;30(8):e364–e366. doi:10.1097/IJG.0000000000001864
15. Au SC. From acute angle-closure to COVID-19 during Omicron outbreak. Vis J Emerg Med. 2022;29:101514. doi:10.1016/j.visj.2022.101514
16. Rajendrababu S, Durai I, Mani I, Ramasamy KS, Shukla AG, Robin AL. Urgent and emergent glaucoma care during the COVID‑19 pandemic: an analysis at a tertiary care hospital in South India. Indian J Ophthalmol. 2021;69(8):2215–2221. doi:10.4103/ijo.IJO_635_21
17. Au SC. Cluster of ocular acute primary angle closure cases and increased antitussive or nasal decongestants usage following the surge in acute COVID-19 infection. QJM. 2023;116(7):601–602. doi:10.1093/qjmed/hcad023
18. Foster PJ, Oen FT, Machin D, et al. The prevalence of glaucoma in Chinese residents of Singapore: A cross-sectional population survey of the Tanjong Pagar District. Arch Ophthalmol. 2000;118(8):1105–1111. doi:10.1001/archopht.118.8.1105
19. Chen YY, Chen YY, Sheu SJ, Chou P. The biometric study in different stages of primary angle-closure glaucoma. Eye. 2013;27(9):1070–1076. doi:10.1038/eye.2013.127
20. Zhong X, Li Y, Huang C, et al. Seasonal variations and climatic factors on acute primary angle-closure admission in southern China: a 5-year hospital-based retrospective study. Acta Ophthalmologica. 2021;99(5):e761–e768. doi:10.1111/aos.14649
21. Zhu J, Xu Y, Wang H, Liu D, Zhu J, Wu H. The seasonality of acute attack of primary angle-closure glaucoma in Beijing, China. Sci Rep. 2018;8(1):4036. doi:10.1038/s41598-018-21074-w
22. Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86(2):238–242. doi:10.1136/bjo.86.2.238
23. Marchenko NR, Kasparova EA, Budnikova EA, Makarova MA. Anterior eye segment damage in coronavirus infection (COVID-19). Vestn Oftalmol. 2021;137(6):142–148. doi:10.17116/oftalma2021137061142
24. Krawitz BD, Sirinek P, Doobin D, et al. The challenge of managing bilateral acute angle-closure glaucoma in the presence of active SARS-CoV-2 Infection. J Glaucoma. 2021;30(3):e50–e53. doi:10.1097/IJG.0000000000001763
25. Sanghi P, Malik M, Hossain IT, Manzouri B. Ocular complications in the prone position in the critical care setting: the COVID-19 Pandemic. J Intensive Care Med. 2021;36(3):361–372. doi:10.1177/0885066620959031
26. Zhou L, Wu S, Wang Y, et al. Clinical presentation of acute primary angle closure during the COVID-19 epidemic lockdown. Front Med. 2022;9:1078237. doi:10.3389/fmed.2022.1078237
27. Zhu M, Yan Y. The surge of acute angle-closure glaucoma during the outbreak of Omicron in a tertiary hospital in Shanghai. Graefes Arch Clin Exp Ophthalmol. 2023;261(9):2709–2711. doi:10.1007/s00417-023-06077-2
28. Liu ZT, Chen ZD, Bing YC, et al. 新型冠状病毒Omicron变异株流行期间原发性闭角型青光眼就诊情况单中心研究 [Clinical presentation of acute primary angle-closure glaucoma during the 2019-nCoV epidemic of Omicron variants: a single-center retrospective study]. Zhonghua Yan Ke Za Zhi. 2023;59(10):838–845. Chinese. doi:10.3760/cma.j.cn112142-20230330-00129
29. Sun X, Dai Y, Chen Y, et al. Primary angle closure glaucoma: what we know and what we don’t know. Prog Retin Eye Res. 2017;57:26–45. doi:10.1016/j.preteyeres.2016.12.003
30. Lowe RF. Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Br J Ophthalmol. 1970;54:161–169. doi:10.1136/bjo.54.3.161
31. Lee DA, Brubaker RF, Ilstrup DM. Anterior chamber dimensions in patients with narrow angles and angle-closure glaucoma. Arch Ophthalmol. 1984;102(1):46–50. doi:10.1001/archopht.1984.01040030030029
32. Lee JR, Sung KR, Han S. Comparison of anterior segment parameters between the acute primary angle closure eye and the fellow eye. Invest Ophthalmol Vis Sci. 2014;55(6):3646–3650. doi:10.1167/iovs.13-13009
33. Marchini G, Pagliarusco A, Toscano A, Tosi R, Brunelli C, Bonomi L. Ultrasound biomicroscopic and conventional ultrasonographic study of ocular dimensions in primary angle-closure glaucoma. Ophthalmology. 1998;105(11):2091–2098. doi:10.1016/S0161-6420(98)91132-0
34. Center for health protection department of health the government of the hong kong special administration region. Available from: https://www.chp.gov.hk/sc/index.html.
35. Hong C, Hong SW, Park CK, Sung KR, Kim CS. Profiles and clinical characteristics of newly diagnosed glaucoma in Urban Korea: a multicenter study. Korean J Ophthalmol. 2020;34(5):353–360. doi:10.3341/kjo.2020.0033
36. Ha JY, Sung MS, Heo H, Park SW, Garza León M. Trends in the characteristics of acute primary angle closure in Korea over the past 10-years. PLoS One. 2019;14(10):e0223527. doi:10.1371/journal.pone.0223527
37. He M, Foster PJ, Ge J, et al. Prevalence and clinical characteristics of glaucoma in adult Chinese: a population-based study in Liwan District, Guangzhou. Invest Ophthalmol Vis Sci. 2006;47(7):2782–2788. doi:10.1167/iovs.06-0051
38. Zhou W, Lin H, Ren Y, et al. Mental health and self-management in glaucoma patients during the COVID-19 pandemic: a cross-sectional study in China. BMC Ophthalmol. 2022;22(1):474. doi:10.1186/s12886-022-02695-2
39. Napier ML, Azuara-Blanco A. Changing patterns in treatment of angle closure glaucoma. Curr Opin Ophthalmol. 2018;29(2):130–134. doi:10.1097/ICU.0000000000000453
40. Örnek K, Temel E, Kocamış Ö, et al. Anterior segment parameters in patients with coronavirus disease. Arq Bras Oftalmol. 2021;84(3):301–302. doi:10.5935/0004-2749.20210087
41. Machhi J, Herskovitz J, Senan AM, et al. The natural history, pathobiology, and clinical manifestations of SARS-CoV-2 infections. J Neuroimmune Pharmacol. 2020;15(3):359–386. doi:10.1007/s11481-020-09944-5
42. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi:10.1038/s41586-020-2012-7
43. Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280. doi:10.1016/j.cell.2020.02.052
44. Zhang W, Du RH, Li B, et al. Molecular and serological investigation of 2019-nCoVinfected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9(1):386–389. doi:10.1080/22221751.2020.1729071
45. Güemes-Villahoz N, Burgos-Blasco B, Vidal-Villegas B, et al. Novel insights into the transmission of SARS-CoV-2 through the ocular surface and its detection in tears and conjunctival secretions: a review. Adv Ther. 2020;37(10):4086–4095. doi:10.1007/s12325-020-01442-7
46. Holappa M, Valjakka J, Vaajanen A. Angiotensin(1–7) and ACE2, ”the hot spots” of renin-angiotensin system, detected in the human aqueous humor. Open Ophthalmol J. 2015;31(9):28–32. doi:10.2174/1874364101509010028
47. Luhtala S, Vaajanen A, Oksala O, Valjakka J, Vapaatalo H. Activities of angiotensin-converting enzymes ACE1 and ACE2 and inhibition by bioactive peptides in porcine ocular tissues. J Ocul Pharmacol Ther. 2009;25(1):23–28. doi:10.1089/jop.2008.0081
48. Deng W, Bao L, Gao H, et al. Ocular conjunctival inoculation of SARS-CoV-2 can cause mild COVID-19 in rhesus macaques. Nat Commun. 2020;11(1):4400. doi:10.1038/s41467-020-18149-6
49. Zhou X, Zhou YN, Ali A, et al. Case report: a re-positive case of SARS-CoV-2 associate with glaucoma. Front Immunol. 2021;12:701295. doi:10.3389/fimmu.2021.701295
50. Hada M, Khilnani K, Vyas N, et al. Evaluating the presence of SARS‑CoV‑2 in the intraocular fluid of COVID‑19 patients. Indian J Ophthalmol. 2021;69(9):2503–2506. doi:10.4103/ijo.IJO_820_21
51. Koo EH, Eghrari AO, Dzhaber D, et al. Presence of SARS-CoV-2 Viral RNA in aqueous humor of asymptomatic individuals. Am J Ophthalmol. 2021;230:151–155. doi:10.1016/j.ajo.2021.05.008
52. Zimmermann A, Lorenz B, Schmidt W. Beidseitiges akutes Engwinkelglaukom im Rahmen einer Hantavirus-Infektion [Bilateral acute angle-closure glaucoma due to an infection with Hantavirus]. Ophthalmologe. 2011;108(8):753–758. doi:10.1007/s00347-010-2311-8
53. Cullinane AB, Leung PS, Ortego J, Coca-Prados M, Harvey BJ. Renin-angiotensin system expression and secretory function in cultured human ciliary body non-pigmented epithelium. Br J Ophthalmol. 2002;86(6):676–683. doi:10.1136/bjo.86.6.676
54. Quigley HA. Angle-closure glaucoma-simpler answers to complex mechanisms: LXVI Edward Jackson memorial lecture. Am J Ophthalmol. 2009;148(5):657–669. doi:10.1016/j.ajo.2009.08.009
55. Wang BC, Tannenbaum CS, Robertazzi RW. Acute glaucoma after general surgery. JAMA. 1961;177(2):108–110. doi:10.1001/jama.1961.03040280012004
56. Lai JS, Gangwani RA. Medication-induced acute angle closure attack. Hong Kong Med J. 2012;18(2):139–145.
57. Au SC, Tsang A, Ko CK. Ocular events following the surge of cough and cold medications use during the Omicron outbreak in Hong Kong. QJM. 2023;116(3):259–260. doi:10.1093/qjmed/hcac096
58. Özmen S, Özkan Aksoy N, Çakır B, Alagöz G. Acute angle-closure glaucoma concurrent with COVID 19 infection; case report. Eur J Ophthalmol. 2022;11:11206721221113201.
59. Violant-Holz V, Gallego-Jiménez MG, González-González CS, et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2020;17(24):9419. doi:10.3390/ijerph17249419
60. Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):e0231924. doi:10.1371/journal.pone.0231924
61. Gillmann K, Hoskens K, Mansouri K. Acute emotional stress as a trigger for intraocular pressure elevation in Glaucoma. BMC Ophthalmol. 2019;19(1):69. doi:10.1186/s12886-019-1075-4
62. Zhang X, Olson DJ, Le P, Lin FC, Fleischman D, Davis RM. The association between glaucoma, anxiety, and depression in a large population. Am J Ophthalmol. 2017;183:37–41. doi:10.1016/j.ajo.2017.07.021
63. Balanzá-Martínez V, Atienza-Carbonell B, Kapczinski F, De Boni RB. Lifestyle behaviours during the COVID-19 - time to connect. Acta Psychiatr Scand. 2020;141(5):399–400. doi:10.1111/acps.13177
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


