Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
The Neutrophil/Lymphocyte Ratio Could Predict Noninvasive Mechanical Ventilation Failure in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease: A Retrospective Observational Study
Authors Sun W, Luo Z, Jin J, Cao Z, Ma Y
Received 19 May 2021
Accepted for publication 19 July 2021
Published 5 August 2021 Volume 2021:16 Pages 2267—2277
DOI https://doi.org/10.2147/COPD.S320529
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Wei Sun,1,* Zujin Luo,1,* Jiawei Jin,1 Zhixin Cao,1 Yingmin Ma2
1Department of Respiratory and Critical Care Medicine, Beijing Chaoyang Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Respiratory and Critical Care Medicine, Beijing Youan Hospital, Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yingmin Ma
Department of Respiratory and Critical Care Medicine, Beijing Youan Hospital, Capital Medical University, Beijing, People’s Republic of China
Tel +86-10-13501185982
Email [email protected]
Purpose: To determine the effectiveness of neutrophil/lymphocyte ratio (NLR), compared to traditional inflammatory markers, for predicting noninvasive mechanical ventilation (NIMV) failure in acute exacerbation of chronic obstructive pulmonary disease (AECOPD) patients.
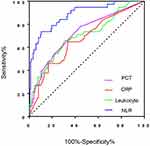
Patients and Methods: We conducted this retrospective observational study including 212 AECOPD patients who required NIMV during hospitalization from January 2015 to December 2020 in the department of respiratory and critical care medicine of Beijing Chao-Yang Hospital (west campus). We reviewed the medical record to determine if NIMV succeeded or failed for each patient, and compared NLR with traditional markers (leukocyte, C-reactive protein [CRP] and procalcitonin [PCT]) between NIMV failure and NIMV success group. Receiver-operating characteristic (ROC) curve and multivariate logistic regression analysis were used to assess the accuracy of these markers for predicting NIMV failure.
Results: A total of 38 (17.9%) patients experienced NIMV failure. NLR was a more sensitive biomarker to predict NIMV failure (AUC, 0.858; 95% CI 0.785– 0.931) than leukocyte counts (AUC, 0.723; 95% CI 0.623– 0.823), CRP (AUC, 0.670; 95% CI 0.567– 0.773) and PCT (AUC, 0.719; 95% CI 0.615– 0.823). There was statistically positive correlation between NLR and leukocytes count (r=0.35, p< 0.001), between NLR and CRP (r=0.258, p< 0.001), between NLR and PCT (r=0.306, p< 0.001). The cutoff value of NLR to predict NIMV failure was 8.9 with sensitivity 0.688, specificity 0.886 and diagnostic accuracy 0.868. NLR> 8.9 (odds ratio, 10.783; 95% CI, 2.069– 56.194; P=0.05) was an independent predictor of NIMV failure in the multivariate logistic regression model.
Conclusion: NLR may be an effective marker for predicting NIMV failure in AECOPD patients, and the patients with NLR> 8.9 should be handled with caution since they are at higher risk of NIMV failure and require intubation. Further study with a larger sample size and with more data is necessary to confirm our study.
Keywords: COPD, noninvasive mechanical ventilation, neutrophil/lymphocyte ratio, predictor, failure, NIMV, NLR, chronic obstructive pulmonary disease
Corrigendum for this paper has been published.
A Letter to the Editor has been published for this article.
Introduction
Noninvasive mechanical ventilation (NIMV) now has become the part of standard intervention for patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD).1,2 Compared with invasive mechanical ventilation (IMV), patients in NIMV success group exhibit several advantages including shorter duration of intensive care unit (ICU) and hospital stay, fewer complications.3,4 However, the NIMV failure rate is approximately 20% in AECOPD patients.5,6 Intubation following failed NIMV is associated with increased odds of a composite complication (desaturation, hypotension, or aspiration) and increased odds of mortality compared to patients intubated without a trial of NIMV.7 Delayed intubation for AECOPD patients can lead to a higher mortality rate (29.3%) compared with patients directly placed on IMV.8 On the contrary, early intubation was associated with decreased hospital mortality for AECOPD patients who were at the high-risk of NIMV failure.9 Hence, it is advisable to enhance the accuracy of early identification of AECOPD patients who may not benefit from NIMV.
The ratio of neutrophils to lymphocytes (NLR) in the peripheral blood is being increasingly studied as a systemic inflammatory marker considering it is easy to get and cost-effective. Several studies have demonstrated that an elevated NLR indicated a worse outcome in many clinical situations.10–13 Among patients with stable chronic obstructive pulmonary disease (COPD), clinical symptoms and quality of life significantly deteriorated with increasing NLR level, in addition, NLR values were inversely associated with the severity of airflow limitation determined by forced expiratory volume in 1 second (FEV1) predicted and absolute values.14 As for predicting AECOPD, NLR was a more sensitive indicator comparing with other traditional inflammatory markers.15,16
COPD is characterized with local chronic inflammation of the airways and lung parenchyma and systemic inflammation.17 Moreover, more than half of AECOPD are triggered by bacterial and/or viral infections, which can aggravate the chronic inflammatory responses.18,19 It was implied that among AECOPD patients, the NIMV failure group presented higher level of serum inflammatory markers (PCT and CRP) compared with patients of NIMV success.20,21 Thus, it is reasonable to speculate that the patients with higher level of inflammatory response are the candidates for NIMV failure.
We assumed that NLR would be higher in NIMV failure AECOPD patients than success ones. In addition, we elucidated the effectiveness of NLR for predicting NIMV failure in AECOPD patients, compared with the traditional inflammatory markers including leukocyte counts, CRP and PCT.
Methods
Study Design
We retrospectively collected 212 AECOPD patients admitted to Beijing Chao-Yang Hospital west campus from January 2015 to December 2020. The patients were followed in the ward, and if the patients needed intubation and they would be transferred to the ICU as needed. Patient selection is shown in Figure 1. Since the current study did not impose any diagnostic and therapeutic influence on patients, the Institutional Review Board for Beijing Chao-Yang Hospital approved the study with a waiver of informed consent (No. 2016-KE-95). We informed every patient by telephone regarding the study and obtained their consent, and we also keep patient clinical data confidential. The current study was conducted in accordance with the Declaration of Helsinki.
 |
Figure 1 Noninvasive mechanical ventilation outcome flow chart. Abbreviation: NIMV, noninvasive mechanical ventilation. |
Inclusion Criteria
Age≥18 years old; primary discharge diagnosis is COPD determined by spirometry data of airflow obstruction with bronchodilator (forced expiratory volume in 1 second [FEV1]/forced vital capacity [FVC]<0.70); Admission into hospital due to AECOPD (define as: a sustained worsening of the patient’s condition, that is acute in onset and necessitates a change in regular medication); NIMV use during hospitalization (NIMV indication: arterial blood pH<7.35 and/or PaCO2 more than 45mmHg, and/or presence of dyspnea at rest assessed using accessory respiratory muscles or paradoxical abdominal breathing).
Exclusion Criteria
Intubated before admission; incomplete data; presence of other severe pulmonary disease; end-stage of chronic disease (e.g., chronic kidney failure, chronic heart failure and malignancy) with<1 year of expected survival; less than 1 month from previous acute exacerbation; NIMV use time less than 48 hours; intubated due to other system fatal condition except AECOPD-related ones.
NIMV Failure Was Defined as Follow
Worsening of pH and PaCO2 in arterial blood (defined as arterial pH<7.25 with PaCO2 increased by>20% compared with the baseline or PaO2<60 mmHg despite maximum tolerated supplemental oxygen); clinical signs suggestive of severely decreased consciousness (eg, coma, delirium); excessive amount of respiratory secretions with weak cough; use of accessory respiratory muscles or thoracic-abdominal paradoxical movement; severe upper gastrointestinal bleeding with aspiration or vomiting; severe hemodynamic instability despite fluid repletion and use of vasoactive agents.22
The primary outcome of the current study was NIMV failure and the secondary outcome was length of stay in hospital (LOS).
Data Collection and Definition
Patients’ baseline characteristics were recorded, including gender, age, LOS in hospital, acute physiology and chronic health evaluation II (APACHE II) score, body mass index (BMI), smoking history, history of long-term oxygen therapy (LTOT), history of domestic noninvasive ventilation, and comorbidities (comorbidities including cor pulmonale, chronic heart disorders, pneumonia, diffuse parenchymal lung disease, severe bronchiectasis, severe old pulmonary tuberculosis, cerebrovascular disease, hypertension, diabetes mellitus, malignancy, chronic kidney disease and reflux esophagitis).
Vital signs (including heart rate, temperature, respiratory rate, systolic pressure, diastolic pressure) were recorded and arterial blood gas and peripheral venous blood were obtained at the time of admission. Use of antibiotic, inhaled bronchodilators and inhaled glucocorticoid were also recorded.
NLR was determined by dividing the total number of neutrophils by the total number of lymphocytes. Concentration of serum CRP were measured using immuno-scatter turbidimetry by Goldsite Aristo (Goldsite, Ltd., China), and the normal value of CRP ranges from 0 to 5mg/L. Concentration of serum PCT were measured using fluorescent enzyme immunoassays by BioMerieux VIDAS (BioMerieux Inc., France), and the normal value of PCT ranges from 0 to 0.5ng/mL.
Bi-level mode was applied for all patients. The inspiratory positive airway pressure (IPAP), expiratory positive airway pressure (EPAP) and backup frequency were set according to clinical practice and patients’ tolerance, and these parameters were also adjusted according to arterial blood gas. An oronasal mask (F1B Full Face Mask, BMC Medical) was used for all subjects. Supplemental oxygen was supplied for all subjects through a port in the mask, with the flow adjusted to maintain oxygen saturation above 90%.
Statistical Analyses
To compare qualitative or categorical variables (expressed as absolute values with percentages), the Chi-square test was used. For continuous variables, the Kolmogorov–Smirnov test was employed to assess the normality of the data, and Student’s t-test was utilized for normally distributed data (expressed as means ± standard deviations), and the Mann–Whitney U-test was used for non-normally distributed data (expressed as medians [25th–75th percentiles]). Spearman correlations were used for correlation analysis, and the results were displayed as correlation coefficients and P values. Receiver-operating characteristic (ROC) curves was used to evaluate the ability of inflammatory markers for predicting NIMV failure. For each ROC curve, the optimal cutoff values, sensitivity, specificity, positive/negative predictive value, diagnostic accuracy, likelihood ratio of positive/negative test, Youden’s index, area under curve (AUC), and 95% CI were calculated. Finally, to determine whether any of these markers were independently associated with NIMV failure, we conducted logistic regression analyses applying a conditional forward stepwise regression model, which resulted in adjusted odds ratios (OR, 95% CIs). All analyses were two-tailed, and differences were considered to be statistically significant at P<0.05. The SPSS software package (version 21.0) was utilized for all statistical analysis.
Results
Patients’ Characteristics and NIMV Outcome
Figure 1 showed the patients’ selection flow chart, a total of 1756 AECOPD patients were admitted to hospital from January 2015 to December 2020, and 495 patients were treated with NIMV, of them 283 patients were excluded, and the remaining 212 patients were included in the current study. Thirty-eight (17.9%) patients experienced NIMV failure. Among NIMV failure patients, 17 patients were intubated, and 21 patients were not intubated because of the patients’ will. All patients survived in the NIMV success group. One patient died in the NIMV failure intubated group and 16 patients died in the NIMV failure not-intubated group.
Table 1 shows the baseline characteristics of the study population. Compared to NIMV success patients, the NIMV failure group had longer LOS, higher APACHE II score, lower BMI, higher rates of domestic noninvasive ventilation use and lower rates of history of LTOT. As for complications, compared to NIMV success group, NIMV failure patients possessed lower rate of chronic heart disorders.
 |
Table 1 Baseline Characteristics of Patients |
Vital Signs, Arterial Blood Gas, Ventilation Parameters and Treatment at the Time of Admission
Based on Table 2, the patients in the NIMV failure group had faster heart rate (P<0.001) and worse arterial blood gas index, specifically, lower pH (P<0.001), higher PaCO2(P<0.001) and higher HCO3− value (P=0.001). Compared to NIMV success patients, NIMV failure patients IPAP (P<0.001) and EPAP (P=0.012) were statistically higher. There was no statistical difference between NIMV failure and success group in terms of treatment (including antibiotics, inhaled bronchodilator and inhaled glucocorticoid).
 |
Table 2 Patients Vital Signs, Laboratory Parameters, Ventilation Parameters and Treatment at Admission |
NLR, Leukocyte, CRP and PCT at the Time of Admission
As shown in Table 2 and Figure 2, NLR (P<0.001), leukocyte counts (P<0.001), CRP (P=0.001) and PCT (P<0.001) were statistically higher in the NIMV failure group than the NIMV success group. Specifically, NIMV failure patients had higher leukocyte and neutrophils counts than NIMV success patients did. The NIMV failure group had lower lymphocyte counts. Figure 3 had shown that there were positive correlations between NLR and leukocyte counts (r=0.35, P<0.001), between NLR and CRP (r=0.258, P<0.001), between NLR and PCT (r=0.306, P<0.001) respectively, and all the differences of correlations reached statistical significance.
 |
Figure 2 NLR (A), leukocyte counts (B), and CRP levels (C) at the time of admission in patients with NIMV success and failure. Abbreviations: NLR, neutrophil/lymphocyte ratio; CRP, C-reactive protein. |
 |
Figure 3 Correlations between NLR and leukocytes (A), NLR and CRP (B), NLR and PCT (C). Abbreviations: NLR, neutrophil/lymphocyte ratio; CRP, C-reactive protein; PCT, procalcitonin. |
Predictive Power of NLR, Leukocyte Counts, CRP and PCT Levels for NIMV Failure
The ROC curves of the NLR, leukocyte counts, CRP and PCT were displayed in Figure 4. Table 3 showed that the AUC of NLR (0.858; 95% CI, 0.785–0.931) was higher than that of leukocyte counts (0.723; 95% CI, 0.623–0.823), CRP (0.670; 95% CI, 0.567–0.773) and PCT (0.719; 95% CI, 0.615–0.823). The diagnostic accuracy of NLR, leukocyte counts, CRP and PCT were 0.868, 0.684, 0.660 and 0.742 respectively. The cutoff value for predicting NIMV failure was NLR>8.9, leukocyte>8.05, CRP>17 and PCT>0.11.
 |
Table 3 ROC Curve Data |
According to multivariate logistic regression analyses, both NLR >8.9 (OR, 10.783; 95% CI, 2.069–56.194; P=0.05) and leukocyte>8.05 (OR, 6.306; 95% CI, 1.062–37.427; P=0.043) were independent factors for predicting NIMV failure (Table 4). Multivariate logistic regression analyses was made with covariates including IPAP, EPAP, APACHE II score, BMI, history of LTOT, domestic noninvasive ventilation, heart rate, pH, PaCO2, HCO3−.
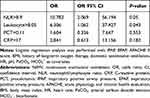 |
Table 4 Logistic Regression Analysis of Risk Factors for NIMV Failure |
Patients’ Outcome Grouped by the NLR Cutoff Value
Table 5 shows the baseline characteristics and NIMV outcomes of the patients grouped by the NLR cutoff value. Compared to patients with NLR ≤8.9, patients in the group of NLR>8.09 were older, had longer LOS, higher APACHE II score, less BMI and faster heart rates. Moreover, patients with higher NLR (>8.9) exhibited poorer arterial blood gas and inflammatory markers results, to be specific, lower pH, higher PaCO2 and HCO3−, and higher level of CRP and PCT value. The NIMV failure rate was significantly higher in patients with NLR >8.9 than in those with NLR ≤8.9 [28/46 (60.9%) vs. 10/166 (6.02%), P<0.001].
 |
Table 5 Patient Data Grouped Based on NLR Cutoff Value |
Patients’ Length of Days in Hospital (LOS)
Patients in the group of NLR>8.9 had longer LOS [12.5 (10–20) vs. 11 (9–14), P=0.012] (Table 5). There were positive correlations between LOS and NLR>8.9 (r=0.173, P=0.012), LOS and CRP>17 (r=0.136, P=0.055), LOS and APACHE II (r=0.148, P=0.032) (Table 6).
 |
Table 6 Correlations Between LOS and APACHE II, Inflammatory Markers |
Discussion
In this study, we found that NLR (OR, 10.783; 95% CI, 2.069–56.194; P=0.05) was a more sensitive marker to predict NIMV failure than traditional inflammatory markers in AECOPD patients, and NLR >8.9 was an independent predictor of NIMV failure. Moreover, the odds ratio of NLR to predict NIMV failure is 10.783, indicating that risk of NIMV failure of patients with NLR>8.9 is much higher than patients with NLR≤8.9.
The primary reason for NIMV failure of AECOPD patients is insufficient alveolar ventilation (could not be rectified by NIMV), which is mainly due to airway obstruction and remodeling and loss of elastic recoil, and this decrease in alveolar ventilation could be aggravated by mucus hypersecretion because of bacterial infection. Several studies had showed that NLR was positively correlated with airflow obstruction.15,23 According to Tanrıverdi and Geijn, AECOPD patients with bacterial infections had higher NLR values than those with non-bacterial infections.24,25 So patients with higher NLR tend to suffer from more serious airflow limitation and higher possibility of bacterial infection, and then it is reasonable to conclude that higher NLR AECOPD patients are prone to experience NIMV failure. Previous studies confirmed that NLR was a sensitive indicator of exacerbation, with cutoff value ranging from 3.3–7.3.15,26–28 The cutoff value of our study is 8.9, and this might because of the fact that patients included in this study were more serious since they all required NIMV and some of them even experienced NIMV failure and need intubation. To the best of our knowledge, our study is the first to report on the association between the NLR and NIMV failure in AECOPD patients.
Neutrophil inflammation is a prominent feature of COPD, both locally and systemically. Neutrophil numbers in bronchial biopsy specimens and induced sputum are associated with disease severity29 and the rate of decline in lung function,30 and neutrophils secrete serine proteases that contribute to alveolar destruction.31 Airway neutrophilia is linked to mucus hypersecretion because neutrophil elastase is a potent stimulant of mucus secretion.32,33 Blood neutrophils isolated from patients with COPD produced more reactive oxygen species under basal conditions as well as after stimulation in vitro.34 Thus, an increased NLR potentially provide information regarding airflow limitation or exacerbations.
Leukocyte counts was also an independent predictor of NIMV failure in this study, however, by comparing diagnostic accuracy and AUC between NLR and leukocyte counts, we concluded leukocyte counts was an inferior predictive marker of NIMV failure than NLR. Leukocytes are a big family, including several subtypes of cell, such as neutrophils, lymphocytes, eosinophils and so on, and fluctuation of leukocyte level is comprehensive result of all components, thus the counts of leukocyte is a less sensitive marker than the ratio of neutrophils and lymphocyte. Besides, neutrophils predominate the leukocyte family, and changes in leukocytes mainly represent neutrophils, while NLR can display changes both in neutrophils and in lymphocytes.35 In line with previous studies, NLR is a better marker than leukocyte in predicting perforated appendicitis in elderly patients of emergency department,36 and a better prognostic value in surgical renal cell carcinoma patients.37
This study demonstrated that NLR outmatch CRP and PCT in predicting NIMV failure. CRP is a sensitive acute-phase reactant and its serum levels increase with infection and chronic inflammatory diseases, and PCT levels increase in the presence of systemic, bacterial, fungal, and parasitic infections but remain normal or slightly increased in viral infections.38 Rammaert found that PCT (OR=1.024, 95% CI: 1.01–1.037, P=0.008) is independently associated with increased risk for ICU mortality for severe COPD patients who need intubation.39 Levels of CRP in combination with PCT is a reliable index for determining the existence of bacterial infection in AECOPD patients.40 A study by Marras showed that higher CRP levels could predict exacerbation in COPD.41 High serum PCT levels (OR= 2.0, 95% CI: 1.2–3.2, P= 0.006) and CRP levels (OR = 1.2, 95% CI: 1.1–1.3, P<0.001) could predicted NIMV failure for patients with AECOPD.20 Calderazzo found no differences of CRP and PCT between AECOPD subjects who had more severe clinical manifestation, lower FEV1 and those had less severe conditions.42 In the present study, both PCT and CRP were not independent predictors of NIMV failure. Possible explanation may be as follow. Firstly, the level of CRP and PCT can only reflect systemic inflammatory response induced by infection, but the impact of these two traditional markers in local airway and lung function remain elusive, it seems that elevation of them cannot be linked to significant airflow limitation or ventilation capacity decrease. Secondly, odds ratio of CRP and PCT to predict NIMV failure in the previous studies were quite low, indicating that these markers were not sensitive enough.
There was statistical difference in LOS between NLR>8.9 patients and NLR<8.9 patients. Also, there was positive correlations between LOS and NLR>8.9, but the correlation was weak (r=0.173). This was maybe because high level of inflammation reflected by high NLR can only partially influence LOS. LOS also depends on the rate at which the disease progresses, if the patient’s condition progresses quickly, LOS will be shorter, on the contrary, a slow progression will lead to a longer LOS.
Limitation
This study had certain limitations. Firstly, it is a single-center study and relatively small sample size, thus our results ought to be generalized with discreetness to other clinical settings. Secondly, we did not include the spirometry because the data is incomplete; especially lacking the data of severe patients whose condition is too weak to finish the lung function test. Thirdly, we cannot exclude the possibility that the need for intubation is due to poor obedience and/or mask intolerance instead of disease progression, and this could confound out study. Finally, certain data are absent such as the support level of ventilation since it is difficult to obtain all the data in the practical clinical settings.
Conclusion
This study indicates that NLR is a preferable marker for predicting NIMV failure than traditional inflammatory ones, and NLR>8.9 is an independent risk factor for NIMV failure. We suggested that patients with NLR>8.9 who need NIMV support due to AECOPD should be evaluated with caution to avoid delayed intubation. Nevertheless, further studies with a larger sample size are necessary to decide whether NLR as an inflammatory marker for screening out NIMV failure would improve NIMV outcomes in AECOPD patients. Because of the weak correlation between NLR and LOS, we concluded that NLR could not accurately predict LOS.
Abbreviations
NIMV, noninvasive mechanical ventilation; LOS, length of stay in hospital; APACHE, acute physiology and chronic health evaluation; LTOT, long-term oxygen therapy; BMI, body mass index; DPLD, diffuse parenchymal lung disease; Structural pulmonary disease include bronchiectasis and old pulmonary tuberculosis; HR, heart rate; RR, respiratory rate; PaCO2, arterial carbon dioxide tension; PaO2, arterial oxygen tension; HCO3−, bicarbonate; FiO2, fraction of inspired oxygen; NLR, neutrophil/lymphocyte ratio; CRP, C-reactive protein; PCT, procalcitonin; IPAP, inspiratory positive airway pressure; EPAP, expiratory positive airway pressure. SPD, structural pulmonary disease (including bronchiectasis and old pulmonary tuberculosis)
Acknowledgments
This study was supported by Beijing Yangfan Project (XMLX201709).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Davidson AC, Banham S, Elliott M, et al. BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax. 2016;71(Suppl 2):ii1–ii35. doi:10.1136/thoraxjnl-2015-208209
2. Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. doi:10.1183/13993003.02426-2016
3. Conti G, Antonelli M, Navalesi P, et al. Noninvasive vs. conventional mechanical ventilation in patients with chronic obstructive pulmonary disease after failure of medical treatment in the ward: a randomized trial. Intensive Care Med. 2002;28(12):1701–1707. doi:10.1007/s00134-002-1478-0
4. Jurjevic M, Matic I, Sakic-Zdravcevic K, Sakic S, Danic D, Bukovic D. Mechanical ventilation in chronic obstructive pulmonary disease patients, noninvasive vs. invasive method (randomized prospective study). Coll Antropol. 2009;33(3):791–797.
5. Contou D, Fragnoli C, Cordoba-Izquierdo A, Boissier F, Brun-Buisson C, Thille AW. Noninvasive ventilation for acute hypercapnic respiratory failure: intubation rate in an experienced unit. Respir Care. 2013;58(12):2045–2052. doi:10.4187/respcare.02456
6. Phua J, Kong K, Lee KH, Shen L, Lim TK. Noninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive pulmonary disease vs. other conditions: effectiveness and predictors of failure. Intensive Care Med. 2005;31(4):533–539. doi:10.1007/s00134-005-2582-8
7. Mosier JM, Sakles JC, Whitmore SP, et al. Failed noninvasive positive-pressure ventilation is associated with an increased risk of intubation-related complications. Ann Intensive Care. 2015;5:4. doi:10.1186/s13613-015-0044-1
8. Chandra D, Stamm JA, Taylor B, et al. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. Am J Respir Crit Care Med. 2012;185(2):152–159. doi:10.1164/rccm.201106-1094OC
9. Duan J, Wang S, Liu P, et al. Early prediction of noninvasive ventilation failure in COPD patients: derivation, internal validation, and external validation of a simple risk score. Ann Intensive Care. 2019;9(1):108. doi:10.1186/s13613-019-0585-9
10. Angkananard T, Anothaisintawee T, McEvoy M, Attia J, Thakkinstian A. Neutrophil lymphocyte ratio and cardiovascular disease risk: a systematic review and meta-analysis. Biomed Res Int. 2018;2018:2703518. doi:10.1155/2018/2703518
11. Ma A, Cheng J, Yang J, Dong M, Liao X, Kang Y. Neutrophil-to-lymphocyte ratio as a predictive biomarker for moderate-severe ARDS in severe COVID-19 patients. Crit Care. 2020;24(1):288. doi:10.1186/s13054-020-03007-0
12. Li W, Ai X, Ni Y, Ye Z, Liang Z. The association between the neutrophil-to-lymphocyte ratio and mortality in patients with acute respiratory distress syndrome: a Retrospective Cohort Study. Shock. 2019;51(2):161–167. doi:10.1097/shk.0000000000001136
13. Liu X, Shen Y, Wang H, Ge Q, Fei A, Pan S. Prognostic significance of neutrophil-to-lymphocyte ratio in patients with sepsis: a Prospective Observational Study. Mediators Inflamm. 2016;2016:8191254. doi:10.1155/2016/8191254
14. Lee H, Um SJ, Kim YS, et al. Association of the neutrophil-to-lymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2016;11(6):e0156511. doi:10.1371/journal.pone.0156511
15. Taylan M, Demir M, Kaya H, et al. Alterations of the neutrophil-lymphocyte ratio during the period of stable and acute exacerbation of chronic obstructive pulmonary disease patients. Clin Respir J. 2017;11(3):311–317. doi:10.1111/crj.12336
16. Farah R, Ibrahim R, Nassar M, Najib D, Zivony Y, Eshel E. The neutrophil/lymphocyte ratio is a better addition to C-reactive protein than CD64 index as a marker for infection in COPD. Panminerva Med. 2017;59(3):203–209. doi:10.23736/s0031-0808.17.03296-7
17. Barnes PJ. Cellular and molecular mechanisms of chronic obstructive pulmonary disease. Clin Chest Med. 2014;35(1):71–86. doi:10.1016/j.ccm.2013.10.004
18. Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359(22):2355–2365. doi:10.1056/NEJMra0800353
19. Nathan C. Points of control in inflammation. Nature. 2002;420(6917):846–852. doi:10.1038/nature01320
20. Wang J, Shang H, Yang X, Guo S, Cui Z. Procalcitonin, C-reactive protein, PaCO2, and noninvasive mechanical ventilation failure in chronic obstructive pulmonary disease exacerbation. Medicine. 2019;98(17):e15171. doi:10.1097/MD.0000000000015171
21. Zhu JJ, Liu LJ. Analysis of factors influenced by the effectiveness of non-invasive ventilation in the treatment of acute exacerbation of chronic obstructive pulmonary disease with different severities. Eur Rev Med Pharmacol Sci. 2016;20(22):4775–4781.
22. Cao Z, Luo Z, Hou A, et al. Volume-targeted versus pressure-limited noninvasive ventilation in subjects with acute hypercapnic respiratory failure: a multicenter randomized controlled trial. Respir Care. 2016;61(11):1440–1450. doi:10.4187/respcare.04619
23. Furutate R, Ishii T, Motegi T, et al. The neutrophil to lymphocyte ratio is related to disease severity and exacerbation in patients with chronic obstructive pulmonary disease. Int Med. 2016;55(3):223–229. doi:10.2169/internalmedicine.55.5772
24. Tanriverdi H, Ornek T, Erboy F, et al. Comparison of diagnostic values of procalcitonin, C-reactive protein and blood neutrophil/lymphocyte ratio levels in predicting bacterial infection in hospitalized patients with acute exacerbations of COPD. Wien Klin Wochenschr. 2015;127(19–20):756–763. doi:10.1007/s00508-014-0690-6
25. van de Geijn GM, Denker S, Meuleman-van Waning V, et al. Evaluation of new laboratory tests to discriminate bacterial from nonbacterial chronic obstructive pulmonary disease exacerbations. Int J Lab Hematol. 2016;38(6):616–628. doi:10.1111/ijlh.12550
26. Plant PK, Owen JL, Elliott MW. One year period prevalence study of respiratory acidosis in acute exacerbations of COPD: implications for the provision of non-invasive ventilation and oxygen administration. Thorax. 2000;55(7):550–554. doi:10.1136/thorax.55.7.550
27. Kurtipek E, Bekci TT, Kesli R, Sami SS, Terzi Y. The role of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in exacerbation of chronic obstructive pulmonary disease. J Pak Med Assoc. 2015;65(12):1283–1287.
28. In E, Kuluozturk M, Oner O, Deveci F. The importance of neutrophil-to-lymphocyte ratio in chronic obstructive pulmonary disease. Turk Thorac J. 2016;17(2):41–46. doi:10.5578/ttj.17.2.009
29. Di Stefano A, Capelli A, Lusuardi M, et al. Severity of airflow limitation is associated with severity of airway inflammation in smokers. Am J Respir Crit Care Med. 1998;158(4):1277–1285. doi:10.1164/ajrccm.158.4.9802078
30. Stănescu D, Sanna A, Veriter C, et al. Airways obstruction, chronic expectoration, and rapid decline of FEV1 in smokers are associated with increased levels of sputum neutrophils. Thorax. 1996;51(3):267–271. doi:10.1136/thx.51.3.267
31. Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27. doi:10.1016/j.jaci.2016.05.011
32. Fahy JV, Dickey BF. Airway mucus function and dysfunction. N Engl J Med. 2010;363(23):2233–2247. doi:10.1056/NEJMra0910061
33. Saetta M, Turato G, Facchini FM, et al. Inflammatory cells in the bronchial glands of smokers with chronic bronchitis. Am J Respir Crit Care Med. 1997;156(5):1633–1639. doi:10.1164/ajrccm.156.5.9701081
34. Noguera A, Batle S, Miralles C, et al. Enhanced neutrophil response in chronic obstructive pulmonary disease. Thorax. 2001;56(6):432–437. doi:10.1136/thorax.56.6.432
35. de Jager CP, Wever PC, Gemen EF, et al. The neutrophil-lymphocyte count ratio in patients with community-acquired pneumonia. PLoS One. 2012;7(10):e46561. doi:10.1371/journal.pone.0046561
36. Jung SK, Rhee DY, Lee WJ, et al. Neutrophil-to-lymphocyte count ratio is associated with perforated appendicitis in elderly patients of emergency department. Aging Clin Exp Res. 2017;29(3):529–536. doi:10.1007/s40520-016-0584-8
37. Hu H, Yao X, Xie X, et al. Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J Urol. 2017;35(2):261–270. doi:10.1007/s00345-016-1864-9
38. Polzin A, Pletz M, Erbes R, et al. Procalcitonin as a diagnostic tool in lower respiratory tract infections and tuberculosis. Eur Respir J. 2003;21(6):939–943. doi:10.1183/09031936.03.00055103
39. Rammaert B, Verdier N, Cavestri B, Nseir S. Procalcitonin as a prognostic factor in severe acute exacerbation of chronic obstructive pulmonary disease. Respirology. 2009;14(7):969–974. doi:10.1111/j.1440-1843.2009.01597.x
40. Li Y, Xie L, Xin S, Li K. Values of procalcitonin and C-reactive proteins in the diagnosis and treatment of chronic obstructive pulmonary disease having concomitant bacterial infection. Pak J Med Sci. 2017;33(3):566–569. doi:10.12669/pjms.333.12554
41. Nuñez A, Marras V. Association between routine blood biomarkers and clinical phenotypes and exacerbations in chronic. Obstruct Pulm Dis. 2020;15:681–690. doi:10.2147/copd.s240720
42. Calderazzo MA, Trujillo-Torralbo MB, Finney LJ, et al. Inflammation and infections in unreported chronic obstructive pulmonary disease exacerbations. Int J Chron Obstruct Pulmon Dis. 2019;14:823–832. doi:10.2147/COPD.S191946
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.