Back to Journals » Psychology Research and Behavior Management » Volume 16
The Mediating Role of Self-Perceived Burden Between Social Support and Fear of Progression in Renal Transplant Recipients: A Multicenter Cross-Sectional Study
Authors Liu S , Zhang Y , Miao Q, Zhang X, Jiang X, Chang T, Li X
Received 23 June 2023
Accepted for publication 17 August 2023
Published 4 September 2023 Volume 2023:16 Pages 3623—3633
DOI https://doi.org/10.2147/PRBM.S424844
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Sainan Liu,1,* Ying Zhang,1,* Qi Miao,1 Xu Zhang,1 Xiaoyu Jiang,1 Tiantian Chang,1 Xiaofei Li2
1The First Affiliated Hospital of China Medical University, Shenyang, 110000, People’s Republic of China; 2Transplantation and Hepatobiliary Department, The First Affiliated Hospital of China Medical University, Shenyang, 110000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaofei Li, Transplantation and Hepatobiliary Department, The First Affiliated Hospital of China Medical University, Shenyang, 110000, People’s Republic of China, Tel +86 15940564748, Email [email protected]
Purpose: To explore the mechanism of social support and fear of progression (FoP) in renal transplant recipients (RTRs) and the self-perceived burden that acts as a mediator between social support and FoP.
Patients and Methods: Sociodemographic and clinical characteristics, the Social Support Rating Scale (SSRS), the Self-Perceived Burden Scale (SPBS), and the Fear of Progression-Questionnaire-Short Form (FoP-Q-SF) were used. Structural equation modeling (SEM) was used to examine the mediating role of self-perceived burden.
Results: Our results showed that social support was negatively related to the self-perceived burden (r = − 0.28, p < 0.001) and FoP (r = − 0.37, p < 0.001). Moreover, we determined that self-perceived burden was positively related to FoP (r = 0.58, p < 0.001) and that the indirect effect of social support on FoP via self-perceived burden was significant (β = − 0.172, 95% CI: − 0.253, − 0.097), and with a mediating effect value of 36.9%.
Conclusion: The FoP in RTRs is a concern. Higher social support and lower self-perceived burden can reduce the risk of FoP. Healthcare professionals (HCPs) should assist RTRs in correctly evaluating an individual’s social support system, helping them optimize social support to reduce the self-perceived burden and the development of FoP.
Keywords: social support, self-perceived burden, fear of progression, renal transplantation
Introduction
For individuals suffering from end-stage renal disease, renal transplantation (RT) is the preferred and most cost-effective treatment choice.1 According to the China Scientific Registry of Kidney Transplantation, China will have performed 12,712 RTs by the end of 2022, ranking second in the world after the United States. The survival rate for renal transplant recipients (RTRs) is 95% in the first year and 88% by the fifth year.2 The low survival rate, chronic rejection,3 quality of the donor kidney,4 and various complications experienced by RTRs can result in heightened attention to disease progression, leading to serious emotional panic.5 Fear of progression (FoP) refers to a patient’s fear or concern about disease recurrence or progression.6 Patients with FoP may exhibit persistent concern regarding their physical symptoms,7 resulting in a psychological burden and increased susceptibility to fatigue.8,9 Importantly, studies have shown that FoP accounts for one-third of patient’ stressors, significantly impacting their quality of life.10 Moreover, patients with high FoP have reduced compliance with treatment and rehabilitation, prolonged hospital stays, escalated medical expenses, and heightened economic burden.11 In a study of 221 Chinese RTRs, FoP was moderate.12 Psychological intervention is one of the main interventions for patients with FoP.13 Consequently, healthcare professionals (HCPs) should recognize the mental elements affecting the development of FoP in RTRs and help them reduce this fear and improve living standards.
Social support is an available and effective external resource providing needed assistance for individuals when faced with pressure and difficulties.14 Transplant patients benefit from social support.15 Indeed, a study demonstrated that social support is the second largest factor in measuring whether patients can accept transplantation and greatly affects transplantation results.16 Patients undergoing RT face many psychological issues, including anxiety and fear. Drawing from the stress-buffering model, social support can improve the psychological status of RTRs.17 A meta-analysis demonstrated that social support is an important and effective coping mechanism for patients confronted with FoP.18 The absence of social support may increase the probability of FoP development. Nonetheless, there are few studies on social support and FoP in RTRs. Thus, the objective of this research was to examine how social support affects FoP in RTRs, thereby providing a more comprehensive theoretical foundation for alleviating FoP in RTRs.
The burden of disease and caregiving responsibilities frequently weighs heavily on caregivers, leading to a diminished sense of self-worth in RTRs. The social behavior-equity theory states that when an individual’s effort and feedback are not balanced, it is easy to induce bad emotions.19 Self-perceived burden encompasses adverse emotional experiences, such as self-blame, ennui, and apprehension, which are unfavorable for psychological adjustment.20 Moreover, serious patients are more prone to depression, and their lives may even be at risk.21 One study investigating 102 RTRs found that the patients had a severe burden of self-perception.22 Indeed, the more burden the patient perceives, the worse the patient’s ability to tolerate FoP.23 Previous studies demonstrated that illness uncertainty indirectly affects well-being via the self-perceived burden,24 which presents a unique viewpoint for examining the connection between social support, self-perceived burden, and FoP.
Previous research demonstrated the link between social support and FoP; however, little is known about the connection between social support, self-perceived burden, and FoP. The theoretical framework of this research was based on the Common-Sense Model of Self-Regulation (CSM)25 and the cognitive appraisal theory of stress.26 CSM posits that patients undergo activation of both cognitive and emotional stress response systems when exposed to external stimuli. After undergoing surgical stress, patients will strongly feel that their health is threatened, resulting in negative cognition and emotions, such as FoP. The cognitive appraisal theory of stress indicates that individuals will actively choose internal and external coping styles to regulate stress when encountering environmental stimuli. Social support and a cognitive assessment system will affect a person’s response to stressful events. The self-perceived burden is a psychological stressor for RTRs. Social support is a coping resource for RTRs to diseases and plays a vital role in FoP. The existing research on FoP is mostly in cancer patients. There needs to be more research on FoP in RTRs.
Taken together, the relationship between social support and FoP can be significantly impacted by the self-perceived burden. The following four assumptions were made: (1) social support is negatively associated with FoP; (2) social support is negatively associated with a self-perceived burden; (3) self-perceived burden is positively associated with FoP; (4) self-perceived burden is a mediator between social support and FoP.
Materials and Methods
Design and Participants
This study used a cross-sectional survey from November 2022 to March 2023. The research subjects were RTRs from three tertiary hospitals in Shenyang City, Liaoning Province, Changchun City, Jilin Province, and Hangzhou City, Zhejiang Province. Inclusion criteria: (1) patients with first RT; (2) ≥ 2 months since the transplantation; (3) age ≥ 18 years; (4) good communication and reading comprehension; (5) voluntary and informed consent for this study. Exclusion criteria: (1) subjects with severe physical diseases or mental disorders; (2) challenging to complete the questionnaire due to cognitive and audio-visual disorders. The sample size included 200–400 cases according to the requirements of the structural equation modeling (SEM).27 We issued 340 questionnaires; 11 questionnaires were not valid. Therefore, the number of valid completed questionnaires was 329, and the questionnaire recovery rate was 96.76%.
Data Collection Procedure
It used a questionnaire to collect information from the research subjects online. The research subjects were sent a two-dimensional code to gain access to the questionnaire through the WeChat group. Before commencing the questionnaire, the purpose, meaning, filling methods, and precautions of this study were explained to the subjects, and they provided informed consent. They could withdraw from filling out the questionnaire at any time. Before issuing the questionnaire, we selected 10 subjects for the pre-test. The answer time is 128 s to 453 s, taking into account the differences between patients, we will answer time of less than 100 s removed.
Measurements
Demographic and Clinical Characteristics
The sociodemographic and clinical characteristics of the patients were collected using a self-developed questionnaire based on the literature. The social demographics included gender, age, education level, marital status, residence, primary caregivers, working status, medical fee payment method, monthly income per capita, and economic burden. The clinical characteristics included transplantation time, dialysis method, dialysis time, number of complications, and recurrence of the primary disease.
Social Support
The Social Support Rating Scale (SSRS) reflecting the social support level was compiled by Xiao in 1986.28 The scale comprises ten items with three dimensions. The overall score of the scale is obtained by summing the scores of each item. The total score ranges from 12 to 66 points (≤ 22 points, poor social support; 23 to 44 points, moderate social support; ≥ 45 points, good social support). A higher score indicates an increased level of social support. The scale has been extensively utilized in China, with Cronbach’s alpha values for the ten items and the overall scale score falling between 0.825 and 0.896.29 In the current study, the Cronbach’s alpha value was 0.807.
Self-Perceived Burden
The Self-Perceived Burden Scale (SPBS) was originally developed by Cousineau in 2003 for chronic disease patients, and the scale has good reliability and validity.30 This study adopted the scale of Wu;31 the content validity of the questionnaire was 1, and the internal consistency reliability was 0.910. This scale consisted of ten items and three dimensions. A Likert five-point scale (1 to 5 points) was used to assess these items. A higher score indicates an increased level of self-perceived burden. The Cronbach’s alpha value for this scale in the current study was 0.961.
Fear of Progression
The Fear of Progression-Questionnaire-Short Form (FoP-Q-SF) is a simplified fear of disease progression scale developed by Mehnert in 2006 for breast cancer patients.32 This scale has good reliability (Cronbach’s alpha = 0.870). The Chinese version of the scale was sinicized by Wu for patients with primary liver cancer,33 and the Cronbach’s alpha value for the FoP-Q-SF to measure the FoP of Chinese is good. The scale included two arms: physical health (6 items) and social family (6 items); the Cronbach’s alpha values were 0.829 and 0.812, respectively. A Likert five-point scale (1 to 5 points) was used to evaluate each item in each arm. The score ranged from 12 to 60 points, with higher scores signifying elevated levels of FoP. A score ≥ 34 points implied that a patient experienced psychological impairment. The Cronbach’s alpha value for this study was 0.920.
Ethical Considerations
The Helsinki Declaration guidelines were adhered to in this study. Organ donation was voluntary and conducted according to the Declaration of Istanbul, with written informed consent obtained. This study was approved by the Ethics Review Committee of the First Affiliated Hospital of China Medical University (202372). The participants were informed that filling out the questionnaire was anonymous and voluntary.
Statistical Analysis
SPSS V.26.0 was used for data analysis. Charts (histograms and Q-Q plots) were used to evaluate the normality of the data. After testing, the three variables were subjected to a normal or approximate normal distribution. Continuous variables were expressed as the mean ± standard deviation (SD), and categorical variables were expressed as the frequency and percentage. Pearson correlation was used to test the correlation between the three variables. AMOS Statistics 26.0 was used to construct the SEM. The model was fitted with the SEM criteria (χ2/df < 3, GFI > 0.90, AGFI > 0.90, NFI > 0.90, IFI > 0.90, TLI > 0.90, CFI > 0.90, RMSEA < 0.08, and SRMR < 0.08), as previously described.34 The mediating effect was evaluated using a sample of 5000 cases through the utilization of bootstrapping. Effect estimates and bias-corrected 95% confidence intervals (CI) were derived. The mediating effect was considered statistically significant if the 95% CI did not include 0. All tests were two-sided, and p < 0.05 indicated statistical significance.
Results
Participant Characteristics
A sum of 329 RTRs participated in this study. Table 1 shows the general information for the RTRs. The proportion of males was 61.4% (n = 202), and 53.8% (n = 177) of the RTRs were ≤ 45 years old. The questionnaire revealed that 27.1% (n = 89) of the RTRs had a bachelor’s degree and above, 76.9% (n = 253) were married, and 80.9% (n = 266) lived in urban areas. For the working status of the RTRs, the proportions of the participants employed, unemployed, retired, and other (farmers, students) were 45.6%, 28.0%, 18.8%, and 7.6%, respectively. RTRs with complications ≥ 3 accounted for 25.2% (n = 83) of the research subjects, and 24.9% (n = 82) of the RTRs had heavy economic burdens.
 |
Table 1 Demographic and Clinical Characteristics of Participants (N=329) |
Correlations Between Social Support, Self-Perceived Burden, and FoP
The mean total scores for social support, self-perceived burden, and FoP among the RTRs were 39.20 ± 8.57, 29.09 ± 11.10, and 33.13 ± 10.32, respectively. The connections between social support, self-perceived burden, and FoP are depicted in Table 2. Social support was negatively related to FoP (r = −0.37, p < 0.001). The self-perceived burden was positively related to FoP (r = 0.58, p < 0.001). Social support was negatively related to the self-perceived burden (r = −0.28, p < 0.001).
 |
Table 2 Means, SDs, and Correlations of All Variables |
The Self-Perceived Burden is a Mediator Between Social Support and FoP
SEM was established with Amos 26.0 using social support (objective support, subjective support, and utilization of support) as an independent variable, self-perceived burden (physical burden, economic burden, and emotional burden) as an intermediary variable, and FoP (physical health and social family) as a dependent variable. The final best-fitting indexes are as follows (χ2/df = 2.897, GFI = 0.965, AGFI = 0.927, NFI = 0.970, IFI = 0.980, TLI = 0.967, CFI = 0.980, RMSEA = 0.076, and SRMR = 0.033). The mediating effect of self-perceived burden in social support and FoP is shown in Figure 1. Social support adversely impacted the self-perceived burden (β = −0.333, p < 0.001) and FoP (β = −0.294, p < 0.001) of the RTRs. Self-perceived burden beneficially impacted FoP (β = 0.516, p < 0.001) (Table 3). The results of the direct, indirect, and total effects in the mediation model are shown in Table 4. The total effect (β = −0.466, p < 0.001) and direct effect (β = −0.294, p < 0.001) of social support on FoP were significant. The indirect effect was significant after self-perceived burden had been incorporated (β = −0.172, 95% CI: −0.253, −0.097, p < 0.001), contributing to 36.9% of the total effect.
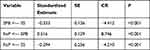 |
Table 3 The Path Coefficients of the Mediation Model |
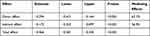 |
Table 4 Mediating Effect |
Discussion
This study explored the connection between social support, self-perceived burden, and FoP in RTRs and confirmed that social support indirectly affects FoP via self-perceived burden.
The mean FoP score (33.13 ± 10.32) for the RTRs was at a moderate level, and 52.6% (n = 173) of the patients had psychological dysfunction (FoP ≥ 34 points), which was consistent with a German study35 and a study of patients with hematological cancer.36 The high incidence of FoP in RTRs may be caused by the unpredictability of FoP, the ambiguity of the treatment outcome, concern about family burdens and adverse drug reactions, and fear of complications and death.37 Although RT can alleviate the psychological distress experienced by end-stage dialysis patients,38 the long-term use of medication and the survival time of the transplanted kidney are major factors that cause FoP in RTRs. Therefore, FoP is a common psychological issue in RTRs.
In the present study, the average social support score in RTRs was comparable to that in patients with liver stones, both at a medium level.39 However, it was lower than the social support reported by hemodialysis patients.38 This disparity may be attributed to the fact that most RTRs do not resume employment after undergoing RT and lack social support from colleagues and work units.40 In addition, social support was negatively correlated with FoP, confirming previous research findings.41 RTRs who receive greater social support are willing to develop an optimistic attitude towards the challenges posed by the disease, facilitating a quicker adjustment to postoperative life and ultimately reducing the occurrence of FoP.39 Good social support can also improve treatment compliance.15 Encouraging patients to increase their treatment knowledge by actively seeking relevant information can alleviate adverse emotions during treatment and reduce FoP. However, due to the different personalities and living environments of patients, the type of social support needed may differ. Korotkin’s research showed that people with anxiety need companionship support, whereas young people need mostly family support,42 implying that the HCPs should administer tailored interventions and diverse forms of social support to different patient cohorts while optimizing the availability and effectiveness of social support resources to effectively mitigate FoP.
The self-perceived burden score in this study was 29.09 ± 11.10, with 14.3% of RTRs reporting a severe self-perceived burden, similar to the results of Geng in 2017 for patients with amyotrophic lateral sclerosis.43 The high burden score may be attributed to the ongoing treatment requirements and complications that impose physical and psychological pressure on RTRs. The present study concluded that self-perceived burden was positively related to FoP, providing new ideas for studying the connection between these two variables. Patients with heavier self-perceived burdens have greater postoperative mental stress, lower tolerance for disease recurrence, and stronger fear.44 A quantitative systematic review study found that reducing the psychological burden and distress of patients can decrease the occurrence of FoP and enhance overall well-being.45 Patients with lower economic burdens have a low incidence of FoP.46 The cost of RT and post-maintenance treatment is expensive, which can heighten the concerns of some patients regarding the exorbitant expenses associated with disease progression, making them more afraid of disease changes. Thus, in addition to caring about the physical health of RTRs, the HCPs should emphasize the assessment of mental issues, encourage participation in social activities, promote the sharing of true feelings, and alleviate the self-perceived burden.
This study found that social support was negatively related to the self-perceived burden, suggesting that RTRs develop a self-perceived burden when faced with insufficient social support, similar to the results of Ren’s research.47 More importantly, the present study showed that self-perceived burden is a mediator between social support and FoP. Previous studies demonstrated that dysfunction indirectly affects depressive symptoms via self-perceived burden.48 A study conducted in 2023 on 386 patients with rheumatoid arthritis confirmed that social support indirectly affects kinesiophobia through self-perceived burden.49 Other studies have shown that high-quality time companionship, travel with family members and peers, and other ways to increase social support allow patients to share their emotional distress, eliminate negative emotions, and reduce emotional burdens.50,51 Consequently, patients can calmly confront disease changes, which is beneficial in mitigating FoP.52 Medical support provided by telemedicine can facilitate a patient’s comprehension of disease-related information,53 enabling them to promptly identify changes in their condition. This proactive approach can effectively minimize hospitalization and alleviate the physical and economic burdens associated with the condition and FoP.54 A study of foreign scholars showed that people with moderate to high levels of FoP do not receive needed social psychotherapy, and there needs to be a consensus on FoP management among social psychological workers.55 Therefore, this study identified a new direction for interventions that reduce FoP by increasing social support and reducing the self-perceived burden for RTRs.
Limitations
There are some constraints in this research. First, the study was cross-sectional and failed to exhibit a good causal connection between social support, self-perceived burden, and FoP. In the future, longitudinal research should be conducted around these three variables. Secondly, only the contribution of social support and self-perceived burden to FoP and the relationship between the three were discussed. Therefore, other potential contributions to FoP should also be considered. Third, the data were mainly collected through questionnaires, which could introduce recall and reporting bias. Fourth, only RTRs with good communication and reading comprehension were included in this study, which could cause selection bias and restrict the generalizability of our study results.
Conclusion
In summary, we found that the level of FoP in RTRs was moderate, and FoP among RTRs is a rising problem in China. Social support was negatively correlated with FoP. Social support also indirectly affected the FoP through self-perceived burden. Therefore, clinical nurses should always pay attention to patients’ social support and psychological status of self-perceived burden in the process of admission and discharge, and implement some interventions to enhance the social support of RTRs and decrease the occurrence and development of their self-perceived burden psychology. Enhanced social support may help promote a positive and stable psychological state, reducing FoP and, more importantly, improving quality of life.
Abbreviations
FoP, Fear of progression; RTRs, Renal transplant recipients; SSRS, Social Support Rating Scale; SPBS, Self-Perceived Burden Scale; FoP-Q-SF, Fear of Progression-Questionnaire-Short Form; HCPs, Healthcare professionals; RT, Renal transplantation; CSM, Common-Sense Model of Self-Regulation; SEM, Structural equation modeling.
Acknowledgments
We sincerely thank the teachers of each medical center for their help and support, and all the patients involved in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Axelrod DA, Schnitzler MA, Xiao H, et al. An economic assessment of contemporary kidney transplant practice. Am J Transplant. 2018;18(5):1168–1176. doi:10.1111/ajt.14702
2. Ayala-García MA, Díaz-Chávez E, Soel-Encalada JM, et al. Renal transplantation recipient patients survival. Gac Med Mex. 2020;156(1):34–39. doi:10.24875/GMM.19005434
3. Low JK, Crawford K, Manias E, Williams A. Stressors and coping resources of Australian kidney transplant recipients related to medication taking: a qualitative study. J Clin Nurs. 2017;26(11–12):1495–1507. doi:10.1111/jocn.13435
4. Sarier M, Duman I, Callioglu M, et al. Outcomes of conservative management of asymptomatic live donor kidney stones. Urology. 2018;118:43–46. doi:10.1016/j.urology.2018.04.035
5. De Pasquale C, Pistorio ML, Veroux M, et al. Psychological and psychopathological aspects of kidney transplantation: a systematic review. Front Psychiatry. 2020;11:106. doi:10.3389/fpsyt.2020.00106
6. Vickberg SM. The Concerns About Recurrence Scale (CARS): a systematic measure of women’s fears about the possibility of breast cancer recurrence. Ann Behav Med. 2003;25(1):16–24. doi:10.1207/S15324796ABM2501_03
7. Mutsaers B, Butow P, Dinkel A, et al. Identifying the key characteristics of clinical fear of cancer recurrence: an international Delphi study. Psychooncology. 2020;29(2):430–436. doi:10.1002/pon.5283
8. Kuang X, Long F, Chen H, et al. Correlation research between fear of disease progression and quality of life in patients with lung cancer. Ann Palliat Med. 2022;11(1):35–44. doi:10.21037/apm-21-2821
9. Meissner VH, Olze L, Schiele S, et al. Fear of cancer recurrence and disease progression in long-term prostate cancer survivors after radical prostatectomy: a longitudinal study. Cancer. 2021;127(22):4287–4295. doi:10.1002/cncr.33836
10. Hall DL, Lennes IT, Pirl WF, Friedman ER, Park ER. Fear of recurrence or progression as a link between somatic symptoms and perceived stress among cancer survivors. Support Care Cancer. 2017;25(5):1401–1407. doi:10.1007/s00520-016-3533-3
11. Guo J, Shen Y, Li B, et al. Does Tai Chi Chuan improve psychological well-being and quality of life in patients with breast cancer? Protocol for a systematic review of randomized controlled trials: a Protocol for Systematic Review and Meta-Analysis. Medicine. 2020;99(16):e19681. doi:10.1097/MD.0000000000019681
12. Lin W, Liu L, Wan J, Liu J, Yang M, Ma H. The status and factors associated with fear of progression in recipients of renal transplantation. Chin J Nurs. 2022;57(01):73–78.
13. Weis JB, Gschwendtner K, Giesler JM, Adams L, Wirtz MA. Psychoeducational group intervention for breast cancer survivors: a non-randomized multi-center pilot study. Support Care Cancer. 2020;28(7):3033–3040. doi:10.1007/s00520-019-05076-6
14. Xu C, Wang Y, Wang Z, et al. Social support and coping style of medical residents in china: the mediating role of psychological resilience. Front Psychiatry. 2022;13:888024. doi:10.3389/fpsyt.2022.888024
15. Bruschwein H, Chen G, Yost J. Social support and transplantation. Curr Opin Organ Transplant. 2022;27(6):508–513. doi:10.1097/MOT.0000000000001022
16. Ladin K, Emerson J, Berry K, et al. Excluding patients from transplant due to social support: results from a national survey of transplant providers. Am J Transplant. 2019;19(1):193–203. doi:10.1111/ajt.14962
17. Zheng W, Hu M, Liu Y. Social support can alleviate the fear of cancer recurrence in postoperative patients with lung carcinoma. Am J Transl Res. 2022;14(7):4804–4811.
18. Zhang X, Sun D, Qin N, Liu M, Jiang N, Li X. Factors correlated with fear of cancer recurrence in cancer survivors: a meta-analysis. Cancer Nurs. 2022;45(5):406–415. doi:10.1097/NCC.0000000000001020
19. Walster E, Berscheid E, Walster GW. New directions in equity research. J Pers Soc Psychol. 1973;25(2):151–176. doi:10.1037/h0033967
20. Liu B, Lee K, Sun C, Wu D, Lim PY. Systematic review on factors associated with self-perceived burden among cancer patients. Support Care Cancer. 2022;30(10):8417–8428. doi:10.1007/s00520-022-07129-9
21. Kowal J, Wilson KG, McWilliams LA, Péloquin K, Duong D. Self-perceived burden in chronic pain: relevance, prevalence, and predictors. Pain. 2012;153(8):1735–1741. doi:10.1016/j.pain.2012.05.009
22. Huang T, Liu Y, Shu Y. Analysis of the status quo and influencing factors of self-perceived burden in patients after kidney transplantation. Chin General Pract Nurs. 2021;19(10):1312–1315.
23. Hu X, Lu H, Lu Z, Zhang Y, Zhang X, Liang Y. A cross-sectional survey of the current situation and influencing factors of postoperative recurrence fear in young and middle-aged cancer patients. Fudan Univ J Med Sci. 2023;50(01):101–107.
24. Zhang N, Tang XQ, Lu K, et al. Illness uncertainty, self-perceived burden and quality of life in patients with chronic myeloid leukaemia: a cross-sectional study. J Clin Nurs. 2022;31(19–20):2935–2942. doi:10.1111/jocn.16123
25. Lee-Jones C, Humphris G, Dixon R, Hatcher MB. Fear of cancer recurrence--A literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology. 1997;6(2):95–105. doi:10.1002/(SICI)1099-1611(199706)6:2<95::AID-PON250>3.0.CO;2-B
26. Lazarus RS, Stress FS. Appraisal, and Coping. New York, NY: Springer; 1984.
27. Sim M, Kim SY, Suh Y. Sample size requirements for simple and complex mediation models. Educ Psychol Meas. 2022;82(1):76–106. doi:10.1177/00131644211003261
28. Xiao S. Theoretical Basis and Research Application of 《 Social Support Rating Scale》. J Clin Psychiatry. 1994;2:98–100.
29. Liu J, Li F, Lian Y. Investigation of reliability and validity of the social support scale. J Xinjiang Med Univ. 2008;1:1–3.
30. Cousineau N, McDowell I, Hotz S, Hébert P. Measuring chronic patients’ feelings of being a burden to their caregivers: development and preliminary validation of a scale. Med Care. 2003;41(1):110–118. doi:10.1097/00005650-200301000-00013
31. Wu Y, Jiang Y. Investigation and analysis of the self-perceived burden among cancer patients. J Nurs Admin. 2010;10(06):405–407.
32. Mehnert A, Herschbach P, Berg P, Henrich G, Koch U. [Fear of progression in breast cancer patients--validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF)]. Z Psychosom Med Psychother. 2006;52(3):274–288. German. doi:10.13109/zptm.2006.52.3.274
33. Wu Q, z Y, Li L, Liu P. Reliability and validity of Chinese version of fear of progression questionnaire-short form for cancer patients. Chin J Nurs. 2015;50(12):1515–1519.
34. Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–246. doi:10.1037/0033-2909.107.2.238
35. Goebel S, Mehdorn HM. Fear of disease progression in adult ambulatory patients with brain cancer: prevalence and clinical correlates. Support Care Cancer. 2019;27(9):3521–3529. doi:10.1007/s00520-019-04665-9
36. Borreani C, Alfieri S, Farina L, Bianchi E, Corradini P. Fear of cancer recurrence in haematological cancer patients: exploring socio-demographic, psychological, existential and disease-related factors. Support Care Cancer. 2020;28(12):5973–5982. doi:10.1007/s00520-020-05434-9
37. Dankert A, Duran G, Engst-Hastreiter U, et al. [Fear of progression in patients with cancer, diabetes mellitus and chronic arthritis]. Rehabilitation(Stuttg). 2003;42(3):155–163. German. doi:10.1055/s-2003-40094
38. Cui C, Wang K, An J, Jin C. Current status and influencing factors of post-traumatic growth in maintenance hemodialysis. Int J Nurs Sci. 2017;4(4):362–366. doi:10.1016/j.ijnss.2017.09.008
39. Wang Y, Huang C, Zhang H, et al. Correlation among psychological resilience, social support, and coping style in patients with complicated hepatolithiasis. Front Behav Neurosci. 2022;16:939512. doi:10.3389/fnbeh.2022.939512
40. De Pasquale C, Veroux M, Pistorio ML, et al. Return to work and quality of life: a psychosocial survey after kidney transplant. Transplant Proc. 2019;51(1):153–156. doi:10.1016/j.transproceed.2018.04.083
41. Thiele S, Goebel S, Kröger N, Pedersen A. Fear of disease progression and relevant correlates in acute leukemia patients prior to allogeneic hematopoietic stem cell transplantation. Psychooncology. 2020;29(8):1248–1254. doi:10.1002/pon.5397
42. Korotkin BD, Hoerger M, Voorhees S, Allen CO, Robinson WR, Duberstein PR. Social support in cancer: how do patients want us to help? J Psychosoc Oncol. 2019;37(6):699–712. doi:10.1080/07347332.2019.1580331
43. Geng D, Ou R, Miao X, et al. Patients’ self-perceived burden, caregivers’ burden and quality of life for amyotrophic lateral sclerosis patients: a cross-sectional study. J Clin Nurs. 2017;26(19–20):3188–3199. doi:10.1111/jocn.13667
44. Li Y, Yang Y, Zhang R, Yao K, Liu Z, Dang Y-H. The mediating role of mental adjustment in the relationship between perceived stress and depressive symptoms in hematological cancer patients: a cross-sectional study. PLoS One. 2015;10(11):e0142913. doi:10.1371/journal.pone.0142913
45. Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7(3):300–322. doi:10.1007/s11764-013-0272-z
46. Niu L, Liang Y, Niu M. Factors influencing fear of cancer recurrence in patients with breast cancer: evidence from a survey in Yancheng, China. J Obstet Gynaecol Res. 2019;45(7):1319–1327. doi:10.1111/jog.13978
47. Ren XR, Wei YY, Su XN, et al. Correlation between self-perceived burden and self-management behavior in elderly stroke survivors: a longitudinal observational study. Medicine. 2020;99(44):e22862. doi:10.1097/MD.0000000000022862
48. Dempsey LE, Karver MS, Labouliere C, Zesiewicz TA, De Nadai AS. Self-perceived burden as a mediator of depression symptoms amongst individuals living with a movement disorder. J Clin Psychol. 2012;68(10):1149–1160. doi:10.1002/jclp.21901
49. Tan M, Liu Y, Zhao R, Li H. The effect of pain social support on kinesiophobia in older patients with rheumatoid arthritis: the mediating role of self-perceived burden. Geriatr Nurs. 2023;50:52–57. doi:10.1016/j.gerinurse.2022.12.011
50. Roland KB, Rodriguez JL, Patterson JR, Trivers KF. A literature review of the social and psychological needs of ovarian cancer survivors. Psychooncology. 2013;22(11):2408–2418. doi:10.1002/pon.3322
51. Sawma T, Choueiri P. The influence of family functioning on the severity of fear of cancer recurrence: a cross-sectional study in a sample of breast cancer survivors of Lebanese women. Eur J Oncol Nurs. 2022;60:102169. doi:10.1016/j.ejon.2022.102169
52. Chang Y, Zhang XN, Yu F, et al. Influence of self-perceived burden on quality of life in patients with urostomy based on structural equation model: the mediating effects of resilience and social support. Biomed Res Int. 2022;2022:9724751. doi:10.1155/2022/9724751
53. Benson JJ, Oliver DP, Washington KT, et al. Online social support groups for informal caregivers of hospice patients with cancer. Eur J Oncol Nurs. 2020;44:101698. doi:10.1016/j.ejon.2019.101698
54. He L, Yu B, Yu J, et al. The impact of social capital and mental health on medication adherence among older people living with HIV (PLWH). BMC Public Health. 2021;21(1):2252. doi:10.1186/s12889-021-12251-0
55. Thewes B, Brebach R, Dzidowska M, Rhodes P, Sharpe L, Butow P. Current approaches to managing fear of cancer recurrence; a descriptive survey of psychosocial and clinical health professionals. Psychooncology. 2014;23(4):390–396. doi:10.1002/pon.3423
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

