Back to Journals » Clinical Ophthalmology » Volume 17
The Magnitude of Refractive Error and Its Associated Factors Among Patients Visiting Ophthalmology Clinics in Southern Ethiopia, 2022
Authors Worku S, Getachew T , Nagarchi K, Shewangizaw M
Received 24 February 2023
Accepted for publication 14 June 2023
Published 23 June 2023 Volume 2023:17 Pages 1801—1811
DOI https://doi.org/10.2147/OPTH.S408610
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Seid Worku,1 Tamiru Getachew,1 Khaleel Nagarchi,1 Misgun Shewangizaw2
1Department of Anatomy, Arba Minch University, Arba Minch, Ethiopia; 2School of Public Health, Arba Minch University, Arba Minch, Ethiopia
Correspondence: Tamiru Getachew, Email [email protected]
Introduction: Refractive error is a vision-impairing condition due to light rays not being able to focus on the retina, resulting in the visual outcome of a cloudy image. It is one of the main causes of central vision impairment globally and in Africa, including Ethiopia. This study was conducted to assess the magnitude of refractive error and its associated factors among patients attending ophthalmic clinics.
Methods: An institutional-based cross-sectional study design was utilized. A systematic random sampling technique was applied to select 356 participants. The data were gathered using an interview-structured questionnaire and check list. Then, the data were entered into Epi-data version 4.6 and transferred to SPSS version 25 for further clean up and analysis. Descriptive and analytical statistics were conducted. A binary logistic regression analysis was done, and variables with a p-value of less than 0.25 in univariate analysis were taken for bivariate analysis. Statistically significant was declared at a p-value of less than 0.05 with an adjusted odds ratio and 95% confidence interval.
Results: Among 356 participants, 96 (27.5%), with 95% CI (22.8, 32.1) had a refractive error, of which nearsighted is the most common type (15.8%). Regular use of electronic devices, near working distance (< 33cm), less or lack of outdoor activities, history of diabetes mellitus and family history of refractive error were factors significantly associated with refractive error.
Conclusion and Recommendations: The magnitude of refractive error was 27.5%, which is relatively elevated than the previous studies. Clients need to get screened regularly so that refractive defects can be detected and corrected early. Eye care professionals shall make a big concern for patients with a history of diabetes and other medical illnesses since they are related to ocular refractive defects.
Keywords: refractive errors, risk factors, magnitude, Southern Ethiopia
Introduction
Refraction is the ratio of the refractive power of the lens and cornea (the refractive media) to the axial length of the eyeball. It is characterized by changes in direction of light as it passes from one transparent medium into another with different optical densities. If there is a discrepancy between the eyeball’s axial length and the cornea’s and lens’s ability to focus light, then the condition is known as ametropia (refractive error).1,2 It occurs when the parallel light rays incoming through the eye (with accommodation at rest) do not focus on the retina in one or both meridians and result in the visual effect of a blurred image.3–5
The three main categories of refractive errors are astigmatism, hyperopia, and myopia.5,6 When one is nearsighted, items that are nearby appear clear while those that are far away appear hazy. With nearsightedness, light comes to focus in front of the retina instead of reaching the neural layer of the retina. When someone has farsightedness, they may be able to see distant objects more clearly than local ones. For individuals with significant farsightedness, vision can be cloudy for objects at any distance, nearby or far. Astigmatism is a disorder in which the eye does not focus the light ray frequently onto the retina (ie, the photo-sensitive tissue at the inner posterior aspect of the eyeball), and this results in the image to look blurry and stretched out.6
Generally, refractive error is caused by three reasons. Firstly, the abnormal length of the eyeball is the most common cause of the refractive error. The axial length of the eyeball is the distance between the cornea and retina pigment. When the length of the eyeball is too long, it causes myopia and when it is too short it causes hypermetropia. Secondly, abnormal curve of the cornea (if the curvature of the cornea is too steep, it results in myopia and too flat it leads to hypermetropia). Irregular curvature of the corneal surface also causes astigmatism. Thirdly, abnormality in the refractive index (light is passing through the major refracting aspects of the eyeball, ie, cornea and lens, before touching on the retina). A high refractive index causes myopia, while a low refractive index causes hypermetropia).7,8 Refraction errors are also accountable for a series of complications caused by different levels of damage to the visual function.9 It results in permanent vision loss (blindness) and amblyopia (in childhood) if it is not corrected early.10
Globally, more than 2.2 billion people are thought to have distance and nearsightedness, and approximately 1 billion are thought to have average or severe visual impairment or blindness due to uncorrected refractive error (88.4 million cases), cataract (94 million cases), glaucoma 66 (7.7 million cases), corneal opacities (4.2 million cases), diabetic retinopathy (3.9 million cases), and trachoma (2 million cases).11 The incidence of the visual disorder due to URE varied from 12.3% to 57.1%.12
In sub-Saharan Africa, about (48.5%) of moderate and severe visual impairment is because of undercorrected refractive error (URE).13 The numerous consequences that lead to eye impairment are a significant public health concern in sub-Saharan Africa.14 Refractive error is the commonest cause of low vision in Ethiopia, accounting for 33.4% of cases, and a primary cause of blindness, accounting for 7.8% of cases. Ethiopia is a developing nation in Africa, with relatively poor health service coverage, especially in eye health care, and is thought to have one of the highest rates of blindness in the world.15 The magnitude of refractive error in Ethiopia is varied in different areas, as in Debre markos 10.2%, in South Wollo 18.3% and in Hawassa 12.9%.16–18
Even though refraction management is relatively simple and low-priced with spectacles, millions of children and adults are giving up school and their efficiency and effectiveness are decreased. Refractive error is one of the most prevalent eye disorders related to regular absenteeism and poor productivity, based on the studies shown in Nigerian hospitals and industries.19
Up to the level of our knowledge, a refractive error among school-age children was conducted in a few different parts of Ethiopia. However, a refractive error was not done among all age groups of patients who attend the ophthalmic clinic, specifically in the study area. As a result, we intended in studying the burden of refractive errors and encouraging the stakeholders to work on it to reduce the problem. Therefore, this study focused to assess the magnitude of refractive errors and their associated factors among patients attending ophthalmology clinics in Southern Ethiopia.
Method and Materials
Study Settings, Design, and Population
An Institution-based cross-sectional study design was conducted among patients attending Arba Minch and Sawla general hospitals ophthalmology clinics in South Ethiopia from July to September 2022. Arba Minch and Sawla general hospitals are located in Arba Minch town, Gamo Zone and Sawla town, Gofa zone, Southern Ethiopia, respectively. In the two hospitals, there are 2 ophthalmologists, 6 optometrists, and 5 ophthalmic nurses. All patients who visited Arba Minch and Sawla general hospitals of ophthalmology clinics during the study period were involved in the study and those patients with a history of recent ocular trauma and surgery of both eyes (within three months of duration) were excluded from the study.
Sample Size Determination and Sampling Procedure
The sample size was calculated using single population proportion formula by considering the following assumptions: P (Prevalence of myopic refractive error) = 16.05% (taken from the study done in Hawasa), α (level of significance) = 5%, the Z value at 95% CI and 5% α = 1.96, margin of error (d) = 0.04 and “n” is the required sample size.
By including a 10% non-response rate, the required sample size was 356.
It was estimated that the two hospitals served approximately 528 patients in data collection period (ie, 286 from Arba Minch general hospital and 242 from Sawla general hospital). With this K value was calculated as (2*528)/356=1056/356 = 3 and systematic random sampling technique based on patient arrival was used to recruit the study participants with every 3rd participant by selecting the first respondent using the lottery method.
Study Variables
Dependent variable: Refractive error.
Independent variables: Socio-demographic, Health-related factors, behavioural and environmental factors were used as predictors.
Operational Definitions
Visual acuity: The ability to identify letters on the Snellen acuity chart at a distance of 6 meters.16
Refractive error: When the presenting visual acuity was less than 6/12 but improved to 6/12 or better with refraction.16
The refractive error was classified as:
Hyperopia: defined as ≥ +0.50 D (diopters) of the sphere on either of the eyes.20
Myopia: defined as a spherical equivalent refractive error (SER = sphere + 1/2 cylinder) of ≤−0.50 D on either eyes.20
Astigmatism: defined as greater than 0.50 D of the cylinder on either of the eyes.20
Family history of refractive errors: First-degree relatives (father, mother, brother and sister) anyone of refractive errors previously diagnosed by a professional.20
Outdoor activity: Considered as yes, if the patient spent more than 2 hours per day in outdoor activities such as walking, playing a game, football and other sports.21
Working distance: The typical distance range at which a person becomes accustomed to performing close-quarters jobs is thought to be 33 to 60 cm. A close working distance is any distance that is less than 33 cm.22
Regular use of electronic devices: Reading or watching computers or television or mobile phone video games and other digital devices at least once a day for not less than 2 hours.
Close-work – are occupations, like workmen, students and government workers (officers, technicians).
Non-close-work – occupational activities like farmers, housewives, waiters, daily labourers, unemployed and domestic workers.
Data Collection Procedure and Collection Instrument
The data was collected using a structured interviewer administered questionnaire combined with observational checklist. The questionnaire was sub-sectioned to include: Socio-demographic characteristics, environmental characteristics, behavioral and health-related characteristics.
Data collectors (BSc nurses) measured working distance using a ruler from the lateral canthus of the eye to the participant’s preferable distance reading after they have been provided with the reduced Snellen E chart. Snellen’s E chart was used to perform a visual acuity test at a distance of 6 meters on each eye. The client being tested must determine, at a distance of 6 meters, which way the capital letter “E” is facing. It could be facing upward, downward, left, or right. Using cards, care was made to make sure the unexamined eye was sufficiently closed.
Optometrists performed pinhole tests on patients with PVA of less than 6/12. If PVA improved to >6/12 with refraction, vision impairment was attributed to refractive error. To identify the types of refractive errors and power of refractive error (diopter), optometrists and/or ophthalmologists performed objective refraction (non-cycloplegic refraction for those >18 years and cycloplegic refraction for participants <18 years of age) using auto refractor and were cross-checked with subjective refraction by using standard refraction trial lenses set to determine the last prescription to the patients. Lastly, the data collectors (BSc nurses) recorded the results of the pinhole test and auto-refractor from the participant’s chart which was already documented by optometrists or ophthalmologists.
Data Processing and Analysis
Once we collected the data, each questionnaire was tested for its completeness, and the data were passed into Epi-data version 4.4 and then disseminated to SPSS version 25 for analysis. The magnitude of the refractive error was calculated. Descriptive statistics, frequency distribution, and percentage were calculated for categorical data and were displayed by a pie chart, bar graph and tables. Bi variant analysis employing binary logistic regression was done to see the candidate variables associated with refractive error. In a multi-variant analysis, the variables with P < 0.25 in the bi variant analysis were included and adjusted OR with 95% CI was computed. Variables which had p-value <0.05 were considered significantly associated with refractive error. Variance inflation factor (VIF) and tolerance were checked for multicollinearity, whose values were ≥0.1 and <10, respectively, to control confounders. Then the Hosmer and Lemeshow goodness-of-fit test was done to check for model fitness (it was 0.418).
Data Quality Assurance
To assure the reliability and validity of data, questionnaires were pretested on 5% of the sample size outside the study area. Two days of in-person training was given for data collectors and supervisors by the principal investigator on the purpose of study, skills of interview, data collection tools and ethical procedures. The supervisors were made onsite supervision during the data collection period and review all filled questionnaires so as to identify incomplete and incoherent responses. Incomplete data was not entered into the database prepared on Epi info. Data clean-up and crosschecking of missing data were done before analysis on SPSS.
Result
Socio-Demographic and Co-Morbidity Characteristics of the Participants
The study was administered to 356 patients with a response rate of 98% from the two general hospitals in South Ethiopia. The patient’s age range was from 8 to 79 years with the median and interquartile range of 35 and 50 years, respectively. More than half (194, 52.7%) of patients in this study were in the age group of 21–50 years and 189 (54.2%) of clients were females. The majority of the study participants 224 (64.2%) were urban dwellers and the remaining 35.8% were rural dwellers. More than half, 207 (59.3%), of the participants had non-close occupations. Concerning educational status, 119 (34.1%) of participants had at least an undergraduate/graduate level of education. Of the total participants, 49 (14%), 95 (27.2%) and 48 (13.8%) had a history of hypertension, diabetes mellitus, and family history of refractive errors, respectively (Table 1).
 |
Table 1 Socio-Demographic and Co-Morbidity Characteristics of Patients Visiting Ophthalmology Clinics in Southern Ethiopia, 2022 |
Personal and Environmental Related Factors
The majority of study participants 264 (75.6%) had no outdoor activities and 120 (34.4%) of patients had a history of regular use of computers or watching television. Regarding working distance, 66 (16.9%) study participants had a working distance of <33 cm. Among the total clients, 32 (9.2%) had smoked cigarettes and 68 (19.5%) participants had drunk alcohol.
The Magnitude of Refractive Error and Its Characteristics
Out of 349 patients, 96 were treated for refractive errors making the magnitude of 27.5%, with 95% CI (22.6, 32.1) (Figure 1). Of these, 55 patients (15.8%) had myopia, 25 (7.2%) had hyperopia and 16 (4.5%) had astigmatism, respectively (Figure 2). In this study, the degree of refractive error in myopic individuals (55 cases) was 8.6%, which was more than half of the total (30 cases) had >-3D, while nearly half of the remaining (10 cases) had <-3D. On the other hand, 16 out of 25 cases with hyperopia had >3D, and 9 out of 25 cases had <3D. Astigmatism accounted for 4.5% of all refractive cases (Table 2).
 |
Table 2 Distribution of Refractive Error Degree of Patients Visiting Ophthalmology Clinics in Southern Ethiopia |
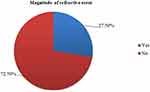 |
Figure 1 Magnitude of refractive error among patients visiting ophthalmology clinics in Southern Ethiopia, 2022. |
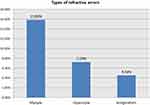 |
Figure 2 Types of refractive errors among patients visiting ophthalmology clinics in Southern Ethiopia, 2022. |
Concerning the age-wise distribution of types of refractory errors, 15 (15.6%) of participants aged greater than 60 developed all types of refractory errors and 10 (10.4%) of individuals aged 10 and above developed two types of refractory errors (Table 3).
 |
Table 3 Age-Wise Distribution of the Types of Refractive Errors in Patients Visiting Ophthalmology Clinics at AMGH and SGH, Southern Ethiopia, 2022 |
Factors Associated with Occurrences of Refractive Error
To select the candidate variables associated with refractive error bivariate analysis was performed and candidate variables at p < 0.25 were selected for multivariate analysis. In multivariate binary logistic regressions regular use of electronic devices (AOR=4.53,95% CI:2.46–8.33), the working distance at near (<33cm)(AOR=3.32,95% CI:1.32–8.33, less or lack of outdoor activities (AOR=3.87,95% CI:1.72–8.68), history of diabetes mellitus (AOR = 4.20, 95% CI:2.20–8.02), and family history of refractive errors (AOR=3.94,95% CI:1.85–8.42) were statistically significant variables (Table 4).
 |
Table 4 Bivariate and Multivariable Logistic Regression Analysis of Factors Associated with Refractive Error Among Patients Attending Ophthalmology Clinics in Southern Ethiopia, 2022 (n = 356) |
Discussion
This institution-based study investigated the magnitude of refractive error and associated risk factors at the two general hospitals, in South Ethiopia. The study shows the magnitude of refractive error among patients attending ophthalmology clinics of the two general hospitals (AMGH and SGH) is 27.5% with 95% CI (22.8, 32.1). This magnitude value is lower than the findings from the hospital-based study in India where the prevalence of refractive error is 55.56% and the findings from another study done in the same country, which is 54.62%.23,24 And this is also lower than the hospital-based studies in Nigeria which are 36.8%, 54.28% and 53.71%, respectively.25–27 The finding of the study is also much lower than the study done in Gondar which is 76.3% and another study in the same country, ie, 35.66%.25,28 But the finding of this study is higher than the study done in Addis Ababa and Borumeda hospital, South Wollo which is 4% and 18.34%, respectively.15,17 The discrepancy seen between the above result and the current study might be due to research methodology differences and cut-off points for defining the outcome of interest that is in a study done in Nigeria, the PVA 6/9 or worse was considered as visual impairment. This hospital-based study is also higher than several other community-based studies in Ethiopia, which have shown rates ranging from 4% to 12.9%.18,29,30 This difference might also be explained by because of the study participants and study setting (ie, school children and the site of the study school).
The commonest type of refractive error in this study was myopia, accounting for 57.3% of the cases. The overall rate of myopia was 15.8%, hyperopia 7.2% and astigmatism 4.5%. The prevalence of myopia is lower than the result reported from the USA 33.1% (95% CI, 31.5–34.7%), Taiwan (44.1%), and Bangladesh (22.1%),31–33 but it is higher than that of Western Nepal (8.3%)34 and South Wollo, Ethiopia (9.6%).17 This result is comparable to the finding in Gondar, Ethiopia (16.7%, 95% CI = 12.8–19.4%).20
The odds of having a history of consistent use of electronic devices were 4.53 times more likely to have RE than their counterparts (P < 0.001). This is in line with a study in Gondar, Ethiopia,35 Debre markos, Ethiopia16 Bangladesh36 and Haryana, India.37 The reason for this could be gazing at the computer, watching television and using other digital devices for a long time might induce prolonged accommodation and muscle fatigue (eyestrain) that may result in a myopic refractive error.38,39
The odds of those patients who underwent short working distances during close work activity had 3.32 times risk of developing refractive error than those using working distances greater than 60cm (p = 0.01). Similar findings have been reported in Singapore,40 China,41 India42 and Ethiopia.22 This could be explained by myopia being caused by high accommodating demand activities that increase pressure in the posterior part of the eye and increase the ocular length.22 Moreover, the positive correlation of this result may have been explained by the eyes’ reduced blink rate and insufficient blinks caused by prolonged eye contact with a computer or television. The tear film does not properly cover the entire cornea when the eyes are subjected to an incomplete and reduced frequency of blinking during prolonged use of digital instruments. Dry eye symptoms and changes to the cornea’s refractive power will result from this.39,43
Outdoor activity was significantly associated with refractive error, ie, not doing outdoor activities or having less outdoor activity increases the odds of having refractive error by 3.87-fold (p = 0.001). This finding is in line with the studies done in India,42 China,44 Almaty, Kazakhstan,45 Bahirdar, Ethiopia21 and Hawassa, Ethiopia.22 This might be explained by in nature most outside activities do not require close attention or accommodations and are carried out in the natural light as opposed to people who do not participate in outdoor sporting activities.46 Besides, inhibitor effects on ocular growth were observed and outdoor sports activities seemed to cause little change in choroidal blood flow.47
In this study, clients having a positive family history of refractive error increase the odds of having refractive errors by 3.94 times (p < 0.001). Studies done in India,37 Bangladesh,36 China48 and Hawassa, Ethiopia18 agree with this study finding. This could explain why, it might be, the parental history of refractive error was considered a marker for both genes and a shared family environmental exposure.
In this study, positive history of diabetes mellitus was found to increase the odds of having a refractive error. The patients with a positive history of diabetes mellitus were 4.20-fold more likely to have RE than were those with a negative history of diabetes (p < 0.001); this result is consistent with findings in a study of Yunnan, China,49 Shanghai, China50 and Ethiopia.17 The reason for this could be that as blood glucose levels rise, glucose from the aqueous humour diffuses into the lens. A portion of glucose is transformed into sorbitol, a sugar alcohol of glucose that is digested very slowly by the lens and builds up in the cytoplasm of lens cells. As a result, the osmotic pressure inside the lens rises, allowing water to enter the lens and causing swelling. The lens’s refractive power may be impacted by swelling.51
Strength and Limitation
As the strength,refractive error was diagnosed by an autorefractor which is the gold standard diagnostic modality and better experts (ophthalmologists and senior optometrists). However, this study is not without limitation. As it is a cross-sectional study, the cause-and-effect relationship cannot be determined. Also, the facilities were selected purposively and we cannot generalize for the population.
Conclusion and Recommendation
The magnitude of RE was 27.5%, which was relatively high compared to previous studies. Myopia was the most common type of refractive error. History of diabetes, family history of refractive errors, less/no outdoor activity, the working distance at near (<33cm) and regular use of electronic devices were factors significantly associated with RE.
Clients need to get screened regularly so that refractive disorders can be detected and corrected early. Eye care professionals shall make a big concern for patients with a history of diabetes and other medical illnesses since they are related to ocular refractive defects. Enhancing awareness of the clients on proper utilization of prescribed spectacles is recommended. Community-focused study in all age groups is recommended to determine the prevalence of refractive errors in the whole population.
Data Sharing Statement
The corresponding author will provide the datasets used and/or analyzed during the current work upon reasonable request.
Ethical Approval
Ethical clearance was obtained from the Research Ethics Review Board (RERB) of Arba Minch University with reference no, the Institutional Review Board (IRB) (IRB/1233/2022). Written consent was obtained from Arba Minch and Sawla General hospital. Oral consent was obtained from study participants and for participants under age of 18 years informed oral consent was taken from parents or legal guardians. Oral consent was approved by the Arba Minch University Institutional research Ethics Review Board. The participants’ involvement in the study was voluntary, and those who were not willing to participate in the study were not included. This study was conducted in accordance with the Declaration of Helsinki. The information concerning the nature, effects, management, and prevention of refractive errors was given to all study participants. Participants who were diagnosed with refractive errors were counselled about the importance and the necessity of taking appropriate prescriptions for spectacles.
Acknowledgments
We would like to extend our gratitude to Arba Minch University, College of Medicine and Health Science, for giving us this chance to write up this research project. We express our sincere gratitude and appreciation to data collectors and supervisors. Lastly, we would like to thank Arba Minch and Sawla general hospital health management information system, human resource management and ophthalmology clinics for their willingness to provide information on the three-month report and manpower of the hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Clarke B. Clinical optics third edition andrew. In: The society of society. Vol. 3. Herder México;2006:5–65.
2. Lang G. Ophthalmology a Pocket Textbook Atlas. Vol. 4. George Thieme Verlag; 2007:88–100.
3. Chuck RS, Jacobs S, Lee JK. Refractive errors and refractive surgery preferred practice pattern®. Ophthalmology. 2018;125(1):PP1–PP04. doi:10.1016/j.ophtha.2017.10.003
4. Khurana AK. Professor, ophthalmology RI of, Sciences PI of M, Rohtak- 124001 I. Compr Ophthalmol. 2017;2017:28.
5. Paul Johnstone NH. Synopsis of causation refractive error disclaimer; 2018.
6. Gel V, Nerve O. Refractive errors; 2014.
7. Center KE university of michigan. What is a refractive error? In: Refractive Errors. Center KE university of michigan; 2020:1–6.
8. Welfare F. Standard treatment guidelines ministry of health and family welfare; 2020.
9. Coroi M. [Complications of refraction disorders]. Ophthalmology. 2015;55(4):5–8. Romanian.
10. Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ. 2021;79:237–243.
11. Classification TI. Blindness and vision impairment; 2021.
12. Sherwin JC, Lewallen S, Courtright P. Blindness and visual impairment due to uncorrected refractive error in sub-Saharan Africa: review of recent population-based studies. J Ophthalmol. 2012;96(7):927–930.
13. Naidoo K, Kempen JH, Gichuhi S, et al. Prevalence and causes of vision loss in sub-Saharan Africa in 2015: magnitude, temporal trends and projections. Br J Ophthalmol. 2020;104(12):1658 LP–1668 . doi:10.1136/bjophthalmol-2019-315217
14. Dougnon A, Guirou N, Bakayoko S, et al. Situation analysis of uncorrected refractive errors in Sub-Saharan Francophone African Countries. J Ophthalmol Res. 2022;5(1):48–65.
15. Woldeyes A, Misganaw C. Prevalence and factors associated with refractive error among primary school children in Addis Ababa, Ethiopia. Int J Med Sci Public Health. 2014;1(9):92–104.
16. District M, Sewunet SA, Aredo KK, Gedefew M. Uncorrected refractive error and associated factors among primary school children in DebreMarkos District, Northwest Ethiopia. BMC Ophthalmol. 2014;14(1):1–6.
17. Besufikad B, Hailemichael W, Tilahun L, Yimam W, Anteneh S. Refractive errors and associated factors among patients visiting BoruMeda Hospital’ s secondary eye unit in Dessie Town, South Wollo Zone, Ethiopia. BMC Ophthalmol. 2022;1–5. doi:10.1186/s12886-022-02539-z
18. Alem KD, Gebru EA. A cross-sectional analysis of refractive error prevalence and associated factors among elementary school children in Hawassa, Ethiopia. J Int Med Res. 2021;49(3):300060521998894. doi:10.1177/0300060521998894
19. Berhane Y, Worku A, Bejiga A, et al. National survey on blindness, low vision and trachoma in Ethiopia: methods and cluster profiles. Ethiop J Health Dev. 2014;21(3):185–203.
20. Berhane MA, Demilew KZ, Assem AS. Myopia: an increasing problem for medical students at the University of Gondar. Clin Ophthalmol. 2022;16:1529–1539. doi:10.2147/OPTH.S365618
21. Sinshaw A, Id A, Tegegne MM, Fekadu SA. Prevalence and associated factors of myopia among school children in Bahir Dar city, Northwest Ethiopia, 2019. PLoS One. 2021;51:14–18.
22. Gebru EA, Mekonnen KA. Prevalence and factors associated with myopia among high school students in Hawassa City, South Ethiopia, 2019. Clin Optom. 2022;14(March):35–43. doi:10.2147/OPTO.S308617
23. Natung T, Taye T, Lyngdoh LA, Dkhar B, Hajong R. Refractive errors among patients attending the ophthalmology department of a medical college in North-East India. J Family Med Prim Care. 2017;6(3):543–548. doi:10.4103/2249-4863.222023
24. Rohul J, Maqbool A, Hussain SA, Shamila H, Anjum F, Hamdani ZA. Prevalence of refractive errors in adolescents in out- patient attendees of the preventive ophthalmology clinic of community medicine, S K I M S, Kashmir, India. J Health Allied Sci NU. 2020;3(1):17–20.
25. Malu K, Ojabo C. Refractive errors in patients attending a private hospital in Jos, Nigeria. Niger J Clin Pract. 2014;17(1):106.
26. Adio AO. Refractive Error Status in Bayelsa State, Nigeria. Niger J Ophthalmol. 2010;18(2):57–61.
27. Adeoti CO, Egbewale BE. Refractive errors in Mercyland Specialist Hospital, Osogbo, Western Nigeria. Niger Postgrad Med J. 2008;15(2):116–119. doi:10.4103/1117-1936.181025
28. Optometry C. Prevalence and degrees of myopia and hyperopia at Gondar university hospital tertiary eye care and training center, Northwest Ethiopia. Clin Optom. 2016;2016:85–91.
29. Kedir J, Girma A. Prevalence of refractive error and visual impairment among rural school-age children of Goro District, Gurage Zone, Ethiopia. Ethiop J Health Sci. 2014;24(4):353–358. doi:10.4314/ejhs.v24i4.11
30. Sume BW, Seyoum G. Prevalence of refractive errors among school students in Ethiopia: a systematic review and meta-analysis. SAGE Open Med. 2022;10:205031212211270. doi:10.1177/20503121221127096
31. Vitale S, Ellwein L, Cotch MF, Ferris FL, Sperduto R. Prevalence of refractive error in the United States, 1999 – 2004. Arch Ophthalmol. 2009;126(8):1111–1119. doi:10.1121/1.3183376
32. Chen S, Tung T, Liu J, et al. Prevalence and associated factors of refractive errors among type 2 diabetics in Kinmen, Taiwan. Ophthalmic Epidemiol. 2008;15(1):2–9. doi:10.1080/09286580701585736
33. Survey LV. Prevalence of refractive error in; 2004.
34. Tuladhar S, Dhakal S. Refractive error profile in a tertiary centre in Western Nepal. Int J Infect Microbiol. 2013;2(2):59–63.
35. Id MD, Yeshaw Y, Bantihun M, Dagnew B. Refractive error and its associated factors among pregnant women attending antenatal care unit at the University of Gondar comprehensive specialized hospital. PLoS One. 2021;27:1–13.
36. Rahman T, Science N, Chowdhury AI, et al. Determinants of early refractive error on school-going children (10–12 years) in Dhaka City, Bangladesh. Indian J Public Health Res Dev. 2021;12(2):381–388.
37. Kumar N, Jangra B, Jangra MS, Pawar N. Risk factors associated with refractive error among medical students. Int J Community Med Public Health. 2018;5(2):634–638.
38. Kim S, Suh Y, Choi Y, et al. Effect of watching 3-dimensional television on refractive error in children. Korean J Ophthalmol. 2015;29(1):53–57. doi:10.3341/kjo.2015.29.1.53
39. Kokab S, Khan MI. Computer vision syndrome: a short review. J Evol Med Dent Sci. 2012;1(6):1223–1226.
40. Pan C, Ramamurthy D, Saw S. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32(1):3–16. doi:10.1111/j.1475-1313.2011.00884.x
41. Lin Z, Vasudevan B, Mao GY, Ciuffreda KJ. The influence of near work on myopic refractive change in urban students in Beijing: a three-year follow-up report. Graefes Arch Clin Exp Ophthalmol. 2016;254(11):2247–2255. doi:10.1007/s00417-016-3440-9
42. Prema N. Causing factors of refractive error in children: heredity or environment ? Indian J Sci Technol. 2011;4(12):1773–1774. doi:10.1002/cssc.201100211
43. Alemayehu AM, Alemayehu MM. Pathophysiologic mechanisms of computer vision syndrome and its prevention: review. World J Ophthalmol Vis Res. 2019;2(5):1–7.
44. Guo Y, Liu LJ, Xu L, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2012;120(2):277–283.
45. Mukazhanova A, Aldasheva N, Iskakbayeva J, et al. Prevalence of refractive errors and risk factors for myopia among schoolchildren of Almaty, Kazakhstan: a cross-sectional study. PLoS One. 2022;17(6):e0269474. doi:10.1371/journal.pone.0269474
46. Saw S, Gazzard G, Shih-yen EC, Chua W. Myopia and associated pathological complications. Myopia Assoc Pathol Complicat. 2015;2015:381–391.
47. Lee Y, Lo C, Sheu S, Lin JL. What factors are associated with myopia in young adults ? A survey study in Taiwan military conscripts. Invest Ophthalmol Vis Sci. 2013;54(2):1026–1033.
48. Huo L, Qi Y, Zhao S. Refractive errors and risk factors for myopia in infants aged 1 – 18 months in Tianjin, China. BMC Ophthalmol. 2021;1–10. doi:10.1186/s12886-021-02172-2
49. Wang M, Cui J, Shan G, et al. Prevalence and risk factors of refractive error: a cross-sectional study in Han and Yi adults in Yunnan, China. BMC Ophthalmol. 2019;2019:1–12.
50. Zhu M, Tong X, Zhao R, He X, Zhao H, Zhu J. Prevalence and associated risk factors of undercorrected refractive errors among people with diabetes in Shanghai. BMC Ophthalmol. 2017;2017:1–11.
51. Sinha M. Refractive errors, blood group and diabetes mellitus: -a correlative study in South Indian population. Ann Rom Soc Cell Biol. 2021;25(6):13847–13856.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.